Within weeks, the COVID-19 pandemic has transformed clinical cardiology practice completely. Patients with chronic cardiac diseases such as heart failure, congenital heart defects, and implantable cardiac devices are traditionally followed including face-to-face contacts during outpatient visits.1,2 Patients are assessed on signs or symptoms of clinical deterioration and are followed with an interactive consultation about treatment goals and strategy of care. Due to the COVID-19 pandemic, healthcare providers cancelled most outpatient visits of chronic patients with various cardiac diseases, to save hospital resources and limit disease transmission.3 However, in a recent article, it is strongly recommended to evaluate clinical warning indicators to explore for the early identification of COVID-19 patients.4 Healthcare providers may consider rapidly switching to the commonly unknown area of remote care.
Remote care consists of a variety of modalities such as telephone contact, video contact, medical apps on smartphones, and wearables.5 The large amount of possibilities hinders the medical professional unfamiliar with the topic of remote care to change swiftly their clinic practice. A joint decision with the patient (shared decision-making) to switch to remote care is recommended.
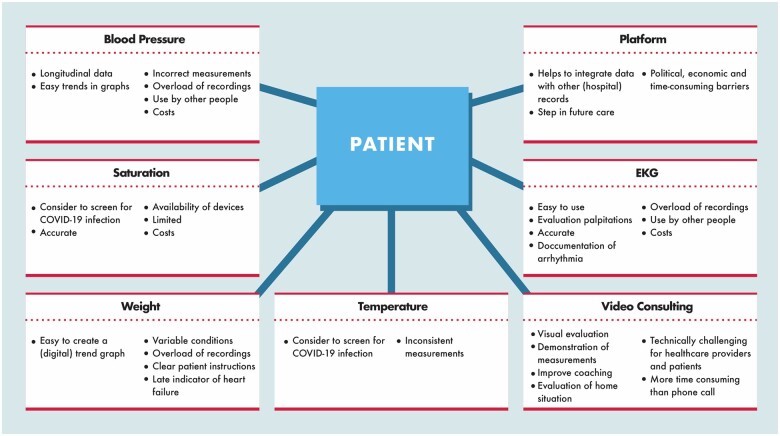
An overview of practical considerations to choose the best remote care for chronic cardiac patients is shown in Figure 1.5 An existing platform can help, particularly if it integrates remote care data with hospital data.5 Platforms with CE mark, ISO, and NEN certification provide good quality in data security. However, the many political, economic, and time-consuming barriers discourage a quick introduction. Video consulting has the advantage of visual evaluation of the clinical performance of a patient at home and visual evaluation of vital signs and symptoms of heart failure. It can also be used to evaluate how patients perform measurements of vital parameters. Video consulting can be used to provide clear patient instructions to avoid errors and facilitate a smooth startup of the measurements. It can also improve personalized coaching, which is one of the most effective remote care interventions.6 However, video consulting can be a technical challenge for both healthcare providers and patients and it can be more time consuming than a telephone call. These challenges are a result of disparities among patients' personal devices, disparities among patients' technical abilities, and disparities among patients' internet connections. In general, there is not one model that works for everyone, which means that extra guidance is needed. Furthermore, it is advised to strive to use validated and approved devices.
Figure 1.
Practical considerations to choose the best remote care for chronic cardiac patients. Left column: benefits, right column: risks.
Other considerations are secure storage facilities for patient data and digital communication channels between healthcare providers and patients. Also, clear protocols to handle contacts and incoming measurements should be considered, especially if tasks are reallocated to paramedical or administrative personnel. An intuitive user interface is recommended to make sure patients and healthcare providers not having to get lost, confused, guessing, or experimenting with software or devices. Otherwise consider also a helpdesk, website, or pocket card with clear instructions for technical handling for them. Scheduled remote contacts can help in the startup phase to monitor commitment closely, further, follow-up can be on the indication. Consider also the revenue model for free software and the risk of data breaches.
The impact of an increase in remote care will probably also be visible years after the COVID-19 pandemic. The rapid initiation could possibly lead to will and decisiveness to create sustainable tools, arrange for financial compensation, and perform more clinical outcome studies. It is, however, expected that there will always be a role for face-to-face contact during outpatient visits, because both healthcare providers and patients appreciate social contact and experience clinical value.
Chronic cardiac patients need regular care and are at increased risk of infection with SARS-CoV-2 with worse outcome.7 Therefore, remote care should be considered in these vulnerable patients to reduce the risk of transmission, to diagnose COVID-19 infection early, but also to continue regular care. Our practical considerations might be helpful to overcome the first barriers in the initiation of remote care, in order to optimize care in these tumultuous times.
References
- 1. Ponikowski P, Voors AA,, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola V-P, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 2. Schuuring MJ, Backx AP, Zwart R, Veelenturf AH, Robbers-Visser D, Groenink M, Abu-Hanna A, Bruining N, Schijven MP, Mulder BJ, Bouma BJ. Mobile health in adults with congenital heart disease: current use and future needs. Neth Heart J 2016;24:647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tan W, Aboulhosn J. The cardiovascular burden of coronavirus disease 2019 (COVID-19) with a focus on congenital heart disease. Int J Cardiol 2020;309:70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang C, Yang J, Zhang J, Yang J. More clinical warning indicators should be explored for monitoring COVID-19 patients’ condition. Int J Cardiol 2020;310:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kauw D, Koole MAC, Winter MM, Dohmen DAJ, Tulevski II, Blok S, Somsen GA, Schijven MP, Vriend JWJ, Robbers-Visser D, Mulder BJM, Bouma BJ, Schuuring MJ. Advantages of mobile health in the management of adult patients with congenital heart disease. Int J Med Inform 2019;132:104011. [DOI] [PubMed] [Google Scholar]
- 6. Noah B, Keller MS, Mosadeghi S, Stein L, Johl S, Delshad S, Tashjian VC, Lew D, Kwan JT, Jusufagic A, Spiegel BMR. Impact of remote patient monitoring on clinical outcomes: an updated meta-analysis of randomized controlled trials. Nature 2018;1:20172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Du Y, Tu L, Zhu P, Mu M, Wang R, Yang P, Wang X, Hu C, Ping R, Hu P, Li T, Cao F, Chang C, Hu Q, Jin Y, Xu G. Clinical features of 85 fatal cases of COVID-19 from Wuhan: a retrospective observational study. Am J Respir Crit Care Med 2020;201:1372–1379. [DOI] [PMC free article] [PubMed] [Google Scholar]