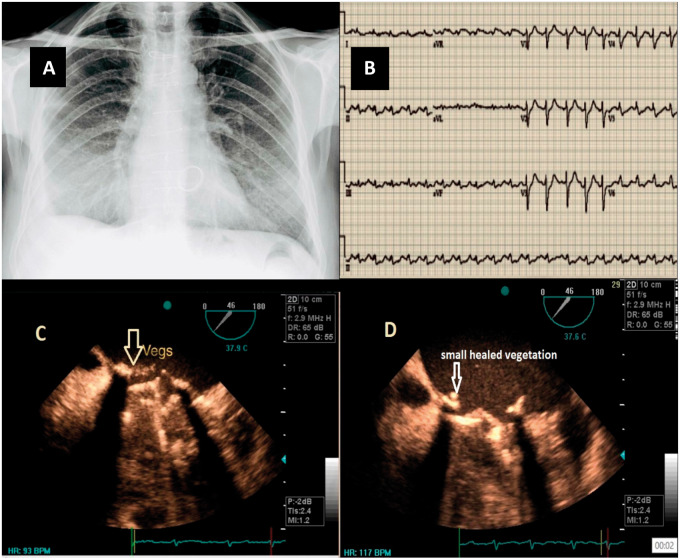
A 24-year-old male, known case of rheumatic heart disease, who had undergone mechanical mitral valve replacement 4 years ago, was referred to our echocardiography laboratory, due to fever, chills, and severe anorexia, 3 weeks after being discharged due to COVID-19 infection. He had been diagnosed due to a chest X-ray suggestive of viral pneumonia (Panel A) and a positive RT–PCR for SARS-COV-2. On admission, he was febrile (38°C), had tachycardia (heart rate: 100/min), and a normal oxygen saturation in room air and his electrocardiogram displayed sinus tachycardia (Panel B). Due to a high suspicion of infectious endocarditis (IE) on echocardiographic examination, a transoesophageal echocardiogram was performed, which revealed several typical vegetations on the posterior prosthetic mitral valve leaflet (Panel C). His previous echocardiogram had demonstrated normal functioning mitral valve prosthesis and a left ventricular ejection fraction of 45%. Blood culture results came back positive for Staphylococcus aureus. Other noticeable laboratory tests included leucocytosis and an elevated C-reactive protein (72 mg/L, normal level <3).
Patient was treated with Azithromycin, Hydroxychloroquine, and corticosteroids and was discharged 2 weeks later. After 6 weeks of antibiotic treatment, repeated trans-thoracic oesophageal echocardiogram (TEE) displayed healing of the vegetative lesions (Panel D).
Up till now, there has been limited evidence on COVID-19 and IE, but since the process of vegetation development begins through transient bacteraemia, followed by binding of bacteria to damaged endothelium, Coronavirus infection and the systemic inflammation caused by it can be a potential risk factor for IE, particularly in susceptible patients with underlying diseases. Furthermore, the administration of corticosteroids and its role in precipitating the condition is unknown.
Supplementary material is available at European Heart Journal online.
Conflict of interest: The authors have submitted their declaration which can be found in the article Supplementary Material online.
Supplementary Material
Contributor Information
Azin Alizadehasl, Cardio-Oncology Department and Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Hashemi Rafsanjani Blvd, Tehran 1996911101, Iran.
Pegah Salehi, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Hashemi Rafsanjani Blvd, Tehran 1996911101, Iran.
Soudeh Roudbari, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Hashemi Rafsanjani Blvd, Tehran 1996911101, Iran.
Mohammad Mehdi Peighambari, Cardiovascular Intervention Research Center, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Hashemi Rafsanjani Blvd, Tehran 1996911101, Iran.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.