Abstract
Objectives
Pulmonary platelet deposition and microangiopathy are increasingly recognized components of coronavirus disease 2019 (COVID-19) infection. Thrombosis is a known component of sepsis and disseminated intravascular coagulation. We sought to compare the level of platelet deposition in the pulmonary vasculature in cases of confirmed COVID-19 infection to other lung injuries and infections.
Methods
Immunohistochemistry was performed on 27 autopsy cases and 2 surgical pathology cases targeting CD61. Multiple cases of normal lung, diffuse alveolar damage, COVID-19, influenza, and bacterial and fungal infections, as well as one case of pulmonary emboli, were included. The levels of CD61 staining were compared quantitatively in the autopsy cases, and patterns of staining were described.
Results
Nearly all specimens exhibited an increase in CD61 staining relative to control lung tissue. The area of CD61 staining in COVID-19 infection was higher than influenza but still comparable to many other infectious diseases. Cases of aspiration pneumonia, Staphylococcus aureus infection, and blastomycosis exhibited the highest levels of CD61 staining.
Conclusions
Platelet deposition is a phenomenon common to many pulmonary insults. A spectrum of staining patterns was observed, suggestive of pathogen-specific mechanisms of platelet deposition. Further study into the mechanisms driving platelet deposition in pulmonary injuries and infections is warranted.
Keywords: Platelets, COVID-19, Pulmonary intravascular coagulopathy, CD61, Diffuse alveolar damage, Coronavirus
Key Points.
Coronavirus disease 2019 (COVID-19) infection results in increased platelet deposition as assessed by CD61 immunostaining when compared with control tissue and influenza infections.
A number of other infections (including both bacterial and fungal infections) also resulted in increased CD61 staining, with several cases exceeding the levels observed in COVID-19.
Different patterns of CD61 staining were apparent across different pathogens, suggesting pathogen-specific mechanisms of recruitment and interaction.
Coagulopathies and thrombotic complications associated with coronavirus disease 2019 (COVID-19) are increasingly described.1-5 Endothelial damage and/or activation by the influence of cytokines released during systematic infection is a possible mechanism of thrombosis in patients with COVID-19,3,5 but a number of different mechanisms have been proposed.6,7 The prototypical pathologic finding in COVID-19 infection in the lungs is diffuse alveolar damage (DAD),8-11 which can be associated with thrombosis.12 A number of emerging pathologic reports demonstrate increased numbers of platelets and megakaryocytes in the pulmonary capillaries of COVID-19 infections.13-17 The mechanistic link between the reported coagulopathies, the thrombotic complications (such as peripheral ischemia and stroke), and the increased presence of platelet aggregates in the lungs in COVID-19 infections remains unclear. The interplay between severe infections and coagulation is well described, with multiple pathophysiologic alterations contributing to thrombosis.18 Platelets themselves are known to have multiple interactions with the immune-inflammatory circuit, including modulating effector leukocyte functions19-21 and direct microbial interactions.22-39 Platelets appear primed to respond directly to microbial insults, as bacterial-derived products are capable of activating platelets via toll-like receptors.22-25 Platelets have also been demonstrated to react to these bacterial stimuli in ways that mediate antibacterial effects.29-33 Fungal-platelet interactions have been described with both yeasts34,35 and hyaline fungi.36-38 Viral infections, including influenza, have also been shown to increase platelet recruitment to the lungs.39 The cumulative evidence suggests that platelets respond to infections and participate in a number of nuanced and targeted interactions with both leukocytes and microorganisms, including viruses, bacteria, and fungi. We therefore sought to investigate the patterns of CD61 staining in the lungs of multiple infections, including several in-house COVID-19 autopsies. In doing so, we compared the amount of CD61 deposition in cases of COVID-19 with other infectious diseases, control tissues, and noninfectious lung injuries, giving context to the finding of increased platelet aggregates and megakaryocytes in the lungs of patients with COVID-19. Using quantitative analysis of CD61 staining, we observed a number of deposition patterns across different infections and clinical circumstances. Our results collectively demonstrate that platelets localize to the lungs in varying degrees and patterns across different pulmonary injuries, implying an intrinsic role for platelets in infection, immunity, and response to lung injury.
Materials and Methods
Clinical information for each of the included cases was retrieved from the autopsy reports and electronic medical records in accordance with our institution’s research on decedents protocol. Pertinent clinical information gathered included medical history, final platelet count, venous duplex (or other thrombosis-related imaging studies), anticoagulation apart from prophylactic doses of subcutaneous heparin, and peak D-dimer. D-dimers were assayed by Liatest (Diagnostica Stago) and are expressed in µg/mL fibrinogen equivalent units (FEUs). The literature cutoff value for exclusion of deep vein thrombosis/pulmonary embolism for this assay is 0.5 µg/mL FEUs.
Formalin-fixed, paraffin-embedded blocks obtained from each of the archived autopsy and surgical pathology cases were cut into 5-µm sections to be stained with H&E and our in-house routine CD61 immunohistochemical stain. The 27 assessed autopsy cases included the following: 3 cases of histologically normal lung, 4 cases of DAD (3 noninfectious, 1 related to polymicrobial sepsis), 9 cases of confirmed COVID-19 infection, 2 cases of influenza, 4 cases of bacterial pneumonia (1 methicillin-sensitive Staphylococcus aureus [MSSA] with an antecedent influenza infection, 1 Pseudomonas aeruginosa infection, and 2 cases of aspiration pneumonia), 4 cases of invasive fungal infections (candidiasis, cryptococcosis, aspergillosis, and blastomycosis), and 1 case of bilateral pulmonary thromboemboli (associated with eosinophilic myocarditis, included as a positive control for diffuse CD61 staining). Two surgical pathology cases were also assessed to ensure that platelet deposition was not a postmortem artifact. These cases consisted of lung specimens with Pneumocystis jirovecii infection and invasive zygomycosis. All COVID-19 autopsies demonstrated findings consistent with prior descriptions of the pathologic changes present in COVID-19 and severe acute respiratory syndrome infections (acute-to-organizing DAD, chronic inflammation, and reactive pneumocyte changes; Table 1 and Image 1).7-11 The other cases exhibited pathologic changes typical of the respective entities as well. Summaries of the histologic findings in each case can be found in Table 1.
Table 1.
Clinical History, Pertinent Laboratory and Imaging Findings, and Histology for the Studied Cases
| Case No. | Disease Group | History | PLT, × 103/μL (Normal, 150-400) | D-Dimer, μg/mL FEU | Thrombosis (Imaging) | Anticoagulation | Histology |
|---|---|---|---|---|---|---|---|
| A20-1 | Control lung | Metastatic carcinoma | 126 | NP | NP | None | Normal lung |
| A20-6 | Control lung | Heart failure | 190 | NP | None | Heparin drip | Normal lung with hemosiderin-laden macrophages |
| A18-84 | Control lung | Heart failure | 206 | NP | None | Heparin drip | Normal lung |
| A18-2 | DAD (MI) | Myocardial infarction | 70 | 10.42 | NP | Heparin drip | Early diffuse alveolar damage and intra-alveolar hemorrhage |
| A18-15 | DAD (AML) | Acute myeloid leukemia | 30 | 1.13 | None | None | Exudative phase diffuse alveolar damage and intravascular blasts |
| A18-32 | DAD (pulmonary hemorrhage) | Ruptured AAA | 95 | NP | NP | None | Alveolar hemorrhage and rare thrombi |
| A18-123 | DAD (polymicrobial sepsis) | CLL, factor VIII deficiency | 11 | 6.26 | Right cephalic vein thrombus | None | Alveolar damage and multifocal bronchopneumonia |
| A20-56 | COVID-19 | Diabetes, Morbid obesity | 344 | 1.49 | None | Heparin drip | Extensive bacterial pneumonia, rare microthrombi, and foci of diffuse alveolar damage |
| A20-59 | COVID-19 | Tetrology of Fallot following correction | 155 | 2.04 | Left axillary vein thrombus | Heparin drip | Organizing diffuse alveolar damage and mucus plugs |
| A20-62 | COVID-19 | Dementia | 254 | 3.59 | Right upper extremity thrombus | Heparin drip | Early diffuse alveolar damage, hemorrhage, aspiration pneumonia focally, and rare thrombi |
| A20-65 | COVID-19 | CVA, dementia | 362 | 2.13 | None | None | Early diffuse alveolar damage, hemorrhage, aspiration pneumonia focally, and rare thrombi |
| A20-73 | COVID-19 | CLL, anal cancer | 229 | 1.83 | None | None | Diffuse alveolar damage, hyaline membranes, and focal bronchopneumonia |
| A20-76 | COVID-19 | None | 169 | 3.4 | None | Heparin drip | Diffuse alveolar damage, hemorrhage, and reactive pneumocytes |
| A20-78 | COVID-19 | Morbid obesity | 405 | >20 | None | Heparin drip | Diffuse alveolar damage, infarction, and hemorrhage |
| A20-83 | COVID-19 | Diabetes | 394 | >20 | None | Heparin drip | Diffuse alveolar damage, infarction, and edema |
| A20-90 | COVID-19 | Diabetes | 185 | 7.35 | None | Heparin drip | Organizing diffuse alveolar damage |
| A18-172 | Influenza | None | 98 | NP | NP | Heparin drip | Intra-alveolar hemorrhage, chronic inflammation, and mild emphysematous changes |
| A18-27 | Influenza | Glioblastoma multiforme | 46 | >20 | NP | None | Intra-alveolar hemorrhage, edema, chronic inflammation, and mild emphysematous changes |
| A17-30 | MSSA pneumonia + influenza | None | 70 | NP | NP | None | Necrotizing pneumonia with abundant bacterial organisms |
| A18-131 | Pseudomonas pneumonia | Necrotizing enterocolitis, prematurity | 43 | NP | None | Heparin drip | Hemorrhage, perivascular bacterial colonies, and minimal inflammation |
| A18-33 | Aspiration pneumonia | T-cell lymphoma | 118 | 3.83 | None | None | Extensive aspiration pneumonia with polymicrobial forms |
| A18-147 | Aspiration pneumonia | None | 290 | >20 | Multiple lower extremity thrombi | Heparin drip | Multifocal pneumonia with associated microorganisms |
| A18-58 | Candidiasis | Stage IV neuroblastoma, TA-TMA | 51 | 9.52 | Radial artery thrombus | Heparin drip | Diffuse alveolar damage and abundant yeast forms |
| A18-96 | Aspergillosis | T-ALL | 14 | 1.05 | Left subclavian/ distal axillary vein thrombus | None | Diffuse alveolar damage and abundant fungal hyphae |
| A20-79 | Cryptococcosis | Heart transplant | 124 | 2.02 | NP | Heparin drip | Diffuse cryptococcal pneumonia |
| A19-33 | Blastomycosis | Alcoholism | 151 | 13.74 | NP | None | Diffuse necrotizing fungal pneumonia |
| A18-155 | Multiple pulmonary thromboemboli | None | 262 | NP | Pulmonary emboli | Heparin drip | Multiple pulmonary emboli and bacterial overgrowth without inflammation |
AAA, abdominal aortic aneurysm; AML, acute myeloid leukemia; CLL, chronic lymphocytic lymphoma; COVID-19, coronavirus disease 2019; CVA, cerebrovascular accident; DAD, diffuse alveolar damage; FEU, fibrinogen equivalent unit; MI, myocardial infraction; MSSA, methicillin-sensitive Staphylococcus aureus; NP, not performed; PLT, platelet; T-ALL, T-cell acute lymphoblastic leukemia; TA-TMA, transfusion-associated thrombotic microangiopathy.
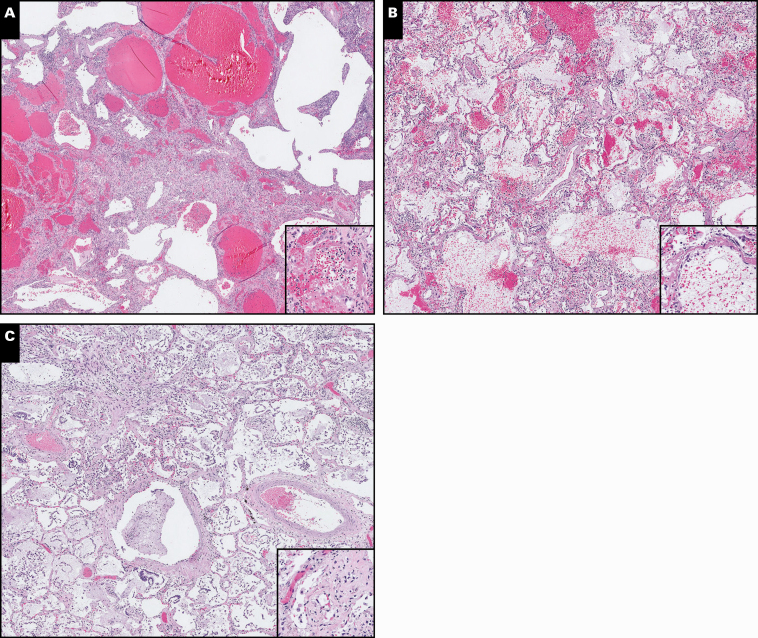
Image 1.
A-C, Representative H&E-stained slides of coronavirus disease 2019 infections demonstrating diffuse alveolar damage and hemorrhagic changes (H&E, ×5; inset, ×20).
Quantitative immunohistochemistry (IHC) was performed on all of the autopsy cases. The CD61-stained slides were scanned in the Philips digital pathology software and analyzed virtually. The most heavily staining areas were photographed at least in triplicate (an up to a maximum of six replicates) across unique regions at ×5, taking care not to sample the same area more than once. The raw ×5 still images obtained above were then analyzed in ImageJ (National Institutes of Health) using IHC Toolbox H-DAB color-based analysis. The DAB-corrected image was converted to 8-bit, and the thresholds were adjusted to provide crisp particles and eliminate background noise (all thresholds were from 150-175 brightness). The resulting image was then analyzed for total positive area. The raw data generated from this analysis were subsequently stored in Microsoft Excel and analyzed using GraphPad Prism (GraphPad Software). Statistical analysis was performed using one-way analysis of variance and Student unpaired t test. Results were considered significant if P < .05.
Results
Representative photos of the scanned H&E-stained slides of three COVID-19 infections demonstrating DAD, interstitial inflammation, and hemorrhagic changes are shown in Image 1. Representative images of IHC studies demonstrating CD61 staining across the different classes of disease are shown in Image 2 and Image 3. The raw data obtained from ImageJ for each autopsy case are included as Supplemental Data 1 (all supplemental materials can be found at American Journal of Clinical Pathology online).
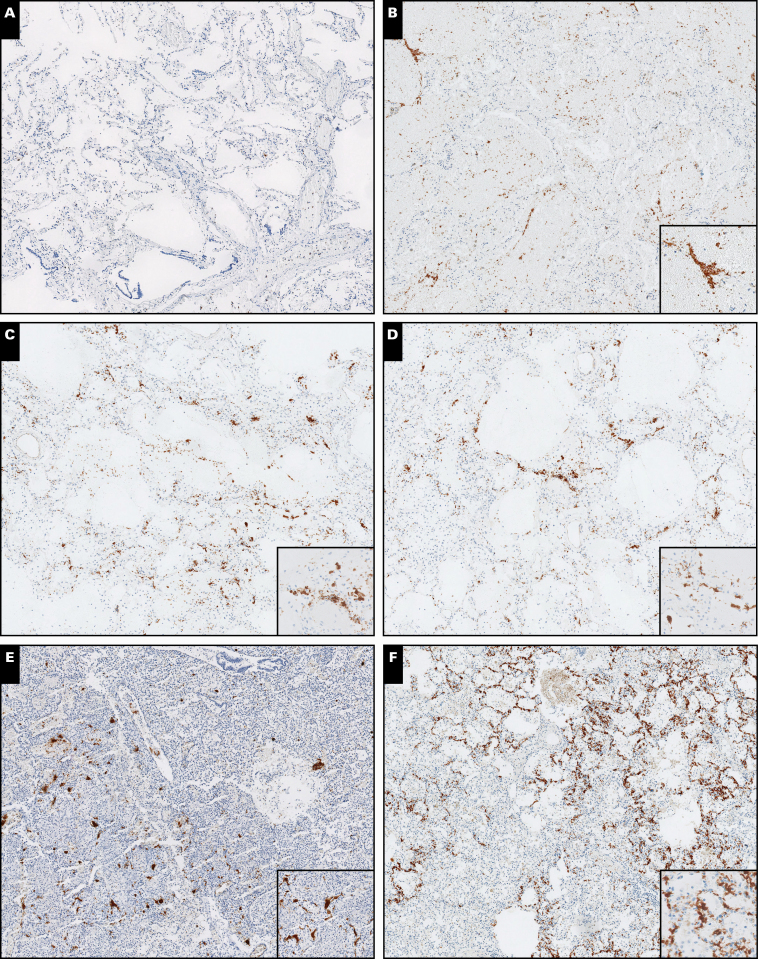
Image 2.
Representative scanned images of CD61-stained tissue from autopsy specimens. A, Control lung. B, Diffuse alveolar damage (noninfectious). C, Coronavirus disease 2019. D, Influenza. E, Pseudomonas pneumonia. F, Methicillin-sensitive Staphylococcus aureus pneumonia. All images were taken at ×5 magnification (insets, approximately ×20).
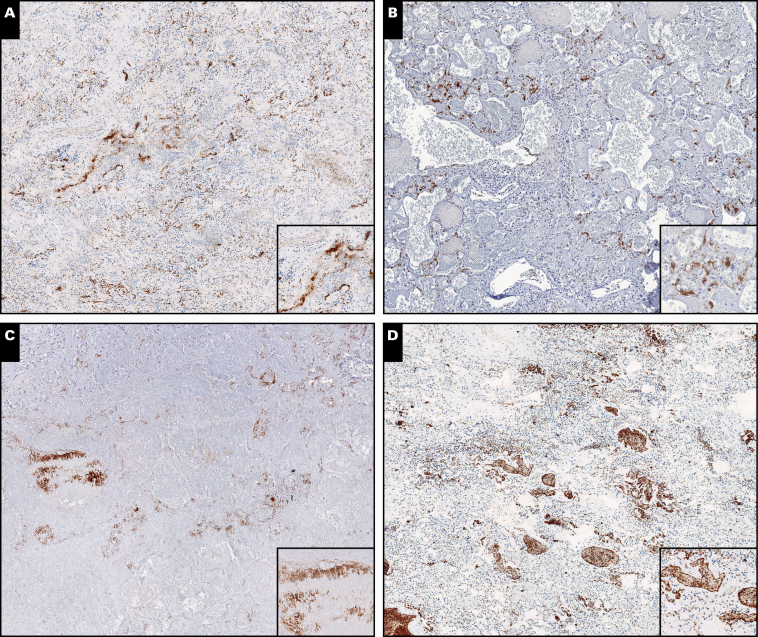
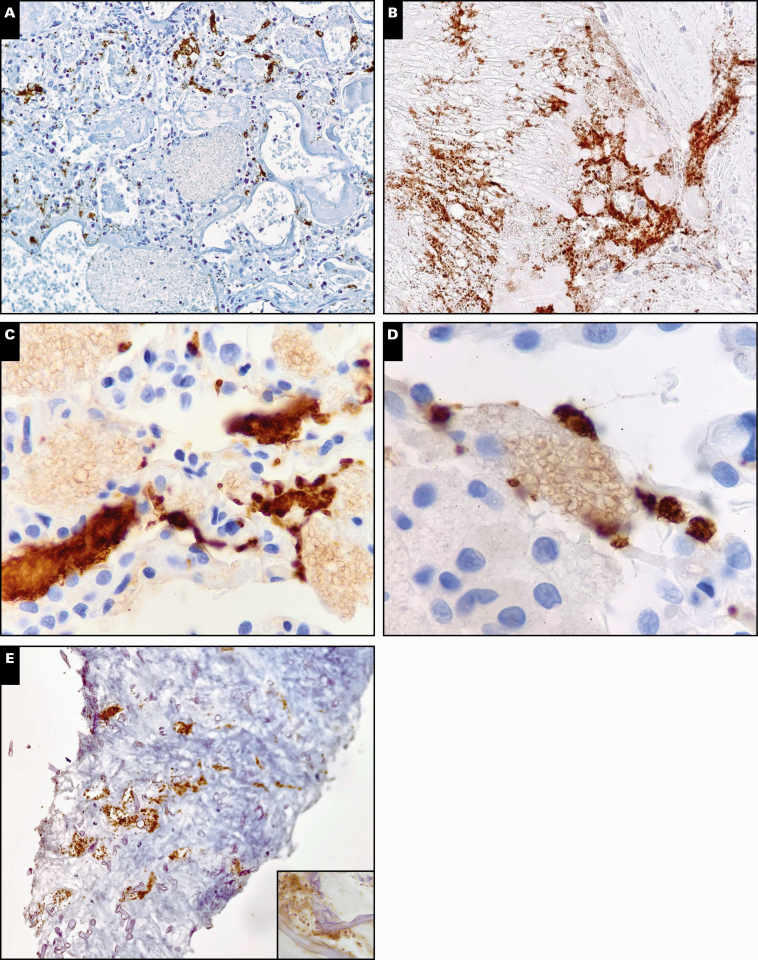
Image 3.
Representative scanned images of CD61-stained tissue from autopsy specimens. A, Aspiration pneumonia. B, Candidiasis. C, Aspergillosis. D, Multiple pulmonary emboli. All images were taken at ×5 magnification (insets, approximately ×20).
With regard to laboratory and clinical testing, D-dimer was performed in 19 (70.4%) of 27 cases and in all of the COVID-19 infections. D-dimers more than 20 were seen in COVID-19, influenza, and aspiration pneumonia. D-dimers more than 5 were seen in DAD secondary to myocardial infarction, DAD secondary to polymicrobial sepsis, COVID-19, influenza, aspiration pneumonia, candidiasis, and blastomyocosis. Imaging for thrombosis was performed in 19 (70.4%) of 27 cases, and thrombosis was present in 7 (36.8%) of these 19 cases. Thrombosis was present in two (22.2%) of nine COVID-19 cases, one (25%) case of DAD, one (25%) case of bacterial pneumonia, two (50%) cases of fungal pneumonia, and in the case of multiple pulmonary thromboemboli. Heparin infusions were common in our series, with 16 (59.3%) of all 27 patients having a heparin drip ordered at some point during their terminal admission. Seven (77.8%) of nine patients with COVID-19 received a heparin infusion (which was largely uncorrelated with D-dimer or imaging findings). This is compared with one (25%) of four DAD cases, one (50%) of two influenza cases, two (50%) of four bacterial pneumonias, and two (50%) of four fungal infections. Heparin infusion was also used in two (66.7%) of three control cases and in the case of multiple pulmonary thromboemboli.
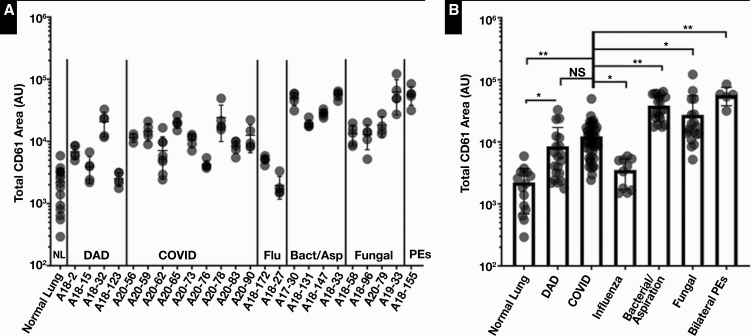
Nearly every condition assessed resulted in increased levels of CD61 staining compared with control tissue. While some of these deposits could be identified on the H&E-stained slides, definitive classification as platelet-rich or fibrin thrombi could not be accurately performed on H&E alone, and thus our quantitative assessment was limited to the CD61-stained slides. COVID-19–positive cases demonstrated a significant increase in CD61 staining compared with normal control lung (P < .0001) and influenza (P < .01; Image 2 and Figure 1). DAD resulted in a similar elevation in CD61 staining compared with COVID-19 infections, without a statistically significant difference. Among the fungal infections, DAD was present secondary to candidiasis and aspergillosis, and these two cases exhibited elevations in CD61 staining similar to both COVID-19 and other cases of DAD. MSSA pneumonia, aspiration pneumonia, and blastomycosis exhibited markedly higher rates of platelet deposition than influenza, COVID-19, and DAD (Images 2, 3 and Figure 1). Interestingly, the patient with MSSA pneumonia (A17-30) was originally admitted for influenza infection and subsequently developed bacterial pneumonia while admitted. This patient had significantly more CD61 staining than the other two influenza infections, neither of which exhibited superimposed processes. The level of staining in A17-30 was comparable to that seen in aspiration pneumonia and blastomycosis, suggesting that some superimposed processes may enhance platelet deposition.
Figure 1.
Results of quantitative immunohistochemistry analysis of CD61-stained tissue sections across all cases (A) and groups (B). Points represent individual measurements obtained from still images, and error bars represent standard deviation. Statistical analysis was performed using a one-way analysis of variance (P < .0001) for comparison of all cases and unpaired Student t tests for individual comparisons. Statistical significance is abbreviated as follows: NS, not significant, *P < .01, **P < .0001. AU, arbitrary units; Bact/Asp, bacterial/aspiration; DAD, noninfectious causes of diffuse alveolar damage; Flu, influenza; NL, normal lung; PEs, pulmonary emboli.
Overall, the predominant pattern of CD61 staining observed in all cases was in the form of intravascular aggregates, which were primarily located in the interalveolar capillaries and smaller vessels. In the cases of candidiasis and pneumocystis infection, platelet aggregates were primarily located within capillaries around extravascular fungal colonies. Interestingly, the fungal colonies adjacent to these aggregates exhibited a peculiar acquisition of positive staining on the surface of fungal organisms in some areas Image 4A, Image 4C, and Image 4D. Large vessel involvement was rarely seen in our case series and was noted to be present in blastomycosis, aspergillosis, and the control case of multiple pulmonary thromboemboli. Direct fungal-platelet interactions were easily observed in aspergillosis and zygomycosis Image 4B and Image 4E. Blastomycosis also demonstrated a unique zonal pattern in the acute/active inflammatory and granulomatous components (Supplemental Figures 1A, and 1B). CD61-positive areas were identified primarily in the granulomatous regions, again primarily in capillaries. The areas of acute/neutrophilic inflammation were largely CD61 negative. Both blastomycosis and aspiration pneumonia also exhibited cytoplasmic staining of effector leukocytes in the vicinity of the platelet aggregates (Supplemental Figure 1C).
Image 4.
Examples of pathogen-specific staining patterns identified with CD61 immunostaining. A, Discrete staining of capillaries adjacent to yeast colony, with faint surface staining of yeast forms adjacent to platelets (×10). B, Large patch of positive staining likely representing angioinvasion in aspergillosis, with direct platelet-hyphal interactions observed (×20). C, D, Platelet aggregates adjacent to fungal colonies with surface staining of yeasts in pneumocystis infection (×40). E, Staining of vessels at the periphery of invasive zygomycosis and evidence of direct fungal-hyphae interactions (×20; inset, ×40).
Discussion
Our study is the first to our knowledge to use CD61 staining in a spectrum of lung injuries to contextualize the finding of platelet aggregates and megakaryocytes in the lungs of patients with COVID-19. The magnitude of CD61 staining for COVID-19 in our study was indeed higher than both control tissue and influenza but was overall comparable to many other infectious scenarios. Our results highlight a spectrum of platelet recruitment patterns for lung injury including infections, likely indicative of a common, underlying role for platelets in the described scenarios. This commonality comes with an apparent variation in the way platelets interact with different pathogens. For instance, the finding of intact platelet-fungal interactions (seen in aspergillosis and zygomycosis) and that of apparent thrombi-dependent transference of CD61 to the surface of yeasts (seen in candidiasis and pneumocystis infections) seems to indicate different mechanisms of interaction between platelets and different classes of organisms. In addition, in both blastomycosis and aspiration pneumonia, inflammatory cells near platelet-rich aggregates were seen exhibiting cytoplasmic staining for CD61 (Supplemental Figure 1), potentially indicating the uptake of platelet antigens by effector leukocytes for immunomodulatory purposes. This finding could alternatively suggest induced expression of a protein containing the CD61 antigen, such as CD41/CD61 or CD51/CD61.40 Immunomodulation is a well-described role of platelets in inflammation and infections,21,40-42 and thus the apparent acquisition of a CD61-containing protein by effector leukocytes in the vicinity of platelet aggregates is a finding of interest.
Our study is still somewhat limited—notably, the relatively small sample size of each infection and limited ability to control outside influencing factors in the autopsy cases used (including the time at which autopsy was performed relative to the onset of symptoms). Some patients had cofounding medical comorbidities (as summarized in Table 1), which could have conceivably influenced platelet function. While thrombocytopenia and anticoagulation could both conceivably influence platelet recruitment and deposition patterns, the thrombocytopenic patients in this study all exhibited levels of CD61 to a similar or higher degree than the COVID-19 cases, and heparin infusion did not appear to correlate with staining density. Our results cannot address whether unique platelet-pathogen interactions capable of inducing platelet activation or aggregation occur in COVID-19 infection, nor can our data implicate or refute specific platelet-viral interactions as a cause of the described thrombotic complications. Our results only demonstrate that the observed phenomenon of increased CD61 staining in the pulmonary capillaries of COVID-19 infections is a finding that is apparently shared across multiple domains of infectious pathogens and noninfectious lung injuries. While increased platelet deposition does not appear to be a unique facet of COVID-19 infection, the finding of varied platelet antigen deposition patterns in our study suggests pathogen-specific interactions can occur and may have significant pathophysiologic implications.
In conclusion, the degree of platelet deposition was variable across different pathogens and patients. There are likely multiple factors influencing the deposition of platelets to sites of injury, many of which are already well described.18-21,43,44 Our results likely demonstrate portions of these varied phenomena. The finding of similar patterns in two surgical pathology cases taken from living patients supports this role for platelets in vivo and argues against the observed phenomena being attributable to an artifact related to autopsy. The mechanisms leading to platelet deposition are likely multifaceted and could include mechanisms outside the canonical thinking of “thrombus” or “embolus.” Some of these potential mechanisms may share some commonality in cytokine-induced or infection-related endothelial injury,18,41 which is a well-described process that results in recruitment of platelets, forming a network capable of honing leukocyte migration,21,41,42 modulating inflammation,41,42 and directly interacting with microorganisms.26-38 However, the lung has been known to be a site of thrombopoiesis since experiments dating back to Aschoff in the late 1800s.45,46 Thus, we cannot exclude that the platelet deposition and staining patterns observed across our series are the result of increased local production of platelets by pulmonary megakaryocytes, rather than the result of an influx of circulating platelets or thromboemboli. This is an area of future study for our group.
Pathogen-specific interactions with platelets could also conceivably play previously unrecognized roles in the pathogenesis of pulmonary infections, including COVID-19. Our work in the context of current publications demonstrates that increased CD61 staining in the vasculature of lung parenchyma is itself not a specific finding related to COVID-19 infection and is a phenomenon that can be found in multiple pathophysiologic settings, including noninfectious etiologies. The factors contributing to platelet recruitment in lung injury and in particular infectious diseases should therefore be studied further.
This study received funding from the Department of Pathology, University of Chicago.
Supplementary Material
References
- 1. Llitjos J-F, Leclerc M, Chochois C, et al. . High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients. J Thromb Haemost. 2020;18:1743-1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bikdeli B, Madhavan MV, Jimenez D, et al. . COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up. J Am Coll Cardiol. 2020;75:2950-2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Magro C, Mulvey JJ, Berlin D, et al. . Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: a report of five cases. Transl Res. 2020;220:1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Klok FA, Kruip MJHA, van der Meer NJM, et al. . Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Escher R, Breakey N, Lämmle B. Severe COVID-19 infection associated with endothelial activation. Thromb Res. 2020;190:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McGonagle D, O’Donnell J, Sharif K, et al. . Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet. 2020;2:E437-E445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hwang DM, Chamberlain DW, Poutanen SM, et al. . Pulmonary pathology of severe acute respiratory syndrome in Toronto. Mod Pathol. 2005;18:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fox SE, Akmatbekov A, Harbert JL, et al. . Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. 2020;8:681-686. doi: 10.1016/S2213-2600(20)30243-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Xu Z, Shi L, Wang Y. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8:420-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barton LM, Duval EJ, Stroberg E, et al. . COVID-19 autopsies, Oklahoma, USA. Am J Clin Pathol. 2020;153:725-733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tian S, Hu W, Niu L, et al. . Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J Thorac Oncol. 2020;15:700-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Deshpande C. Thromboembolic findings in COVID-19 autopsies: pulmonary thrombosis or embolism? Ann Intern Med. 2020;173:394-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rapkiewicz AV, Mai X, Carsons SE, et al. . Megakaryocytes and platelet-fibrin thrombi characterize multi-organ thrombosis at autopsy in COVID-19: a case series. E Clin Med. 2020;24:100434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carsana L, Sonzogni A, Nasr A, et al. . Pulmonary post-mortem findings in a series of COVID-19 cases from northern Italy: a two-centre descriptive study. Lancet. 2020;20:P1135-P1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Buja LM, Wolf DA, Zhao B, et al. . The emerging spectrum of cardiopulmonary pathology of the coronavirus disease 2019 (COVID-19): report of 3 autopsies from Houston, Texas and review of autopsy findings from other United States cities. Cardiovasc Pathol. 2020;48:107233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Levi M, Thachil J, Iba T, et al. . Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet. 2020;7:e438-e440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sauter JL, Baine MK, Butnor KJ, et al. . Insights into pathogenesis of fatal COVID-19 pneumonia from histopathology with immunohistochemical and viral RNA studies [published online July 2, 2020]. Histopathology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Simmons J, Pittet JF. The coagulopathy of acute sepsis. Curr Opin Anaesthesiol. 2015;28:227-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Italiano JE Jr, Mairuhu AT, Flaumenhaft R. Clinical relevance of microparticles from platelets and megakaryocytes. Curr Opin Hematol. 2010;17:578-584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reid VL, Webster NR. Role of microparticles in sepsis. Br J Anaesth. 2012;109:503-513. [DOI] [PubMed] [Google Scholar]
- 21. Cerletti C, Tamburrelli C, Izzi B, et al. . Platelet-leukocyte interactions in thrombosis. Thromb Res. 2012;129:263-266. [DOI] [PubMed] [Google Scholar]
- 22. Claushuis TAM, Van Der Veen AIP, Horn J, et al. . Platelet toll-like receptor expression and activation induced by lipopolysaccharide and sepsis. Platelets. 2019;30:296-304. [DOI] [PubMed] [Google Scholar]
- 23. Cognasse F, Hamzeh-Cognasse H, Lafarge S, et al. . Toll-like receptor 4 ligand can differentially modulate the release of cytokines by human platelets. Br J Haematol. 2008;141:84-91. [DOI] [PubMed] [Google Scholar]
- 24. Shiraki R, Inoue N, Kawasaki S, et al. . Expression of Toll-like receptors on human platelets. Thromb Res. 2004;113:379-385. [DOI] [PubMed] [Google Scholar]
- 25. Aslam R, Speck ER, Kim M, et al. . Platelet Toll-like receptor expression modulates lipopolysaccharide-induced thrombocytopenia and tumor necrosis factor-alpha production in vivo. Blood. 2006;107:637-641. [DOI] [PubMed] [Google Scholar]
- 26. Bryant AE, Bayer CR, Aldape MJ, et al. . Clostridium perfringens phospholipase C-induced platelet/leukocyte interactions impede neutrophil diapedesis. J Med Microbiol. 2006;55:495-504. [DOI] [PubMed] [Google Scholar]
- 27. Mirlashari MR, Hagberg IA, Lyberg T. Platelet-platelet and platelet-leukocyte interactions induced by outer membrane vesicles from N. meningitidis. Platelets. 2002;13:91-99. [DOI] [PubMed] [Google Scholar]
- 28. Shepel M, Boyd J, Luider J, et al. . Interaction of Yersinia enterocolitica and Y. pseudotuberculosis with platelets. J Med Microbiol. 2001;50:1030-1038. [DOI] [PubMed] [Google Scholar]
- 29. Dankert J, van der Werff J, Zaat SA, et al. . Involvement of bactericidal factors from thrombin-stimulated platelets in clearance of adherent viridans streptococci in experimental infective endocarditis. Infect Immun. 1995;63:663-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fitzgerald JR, Foster TJ, Cox D. The interaction of bacterial pathogens with platelets. Nat Rev Microbiol. 2006;4:445-457. [DOI] [PubMed] [Google Scholar]
- 31. Palankar R, Kohler TP, Krauel K, et al. . Platelets kill bacteria by bridging innate and adaptive immunity via platelet factor 4 and FcgRIIA. J Thromb Haemost. 2018;16:1187-1197. [DOI] [PubMed] [Google Scholar]
- 32. Tang YQ, Yeaman MR, Selsted ME. Microbicidal and synergistic activities of human platelet factor-4 (hPF-4) and connective tissue activating peptide-3 (CTAP-3). Blood. 1995;86:556a. [Google Scholar]
- 33. Yeaman MR. Platelets in defense against bacterial pathogens. Cell Mol Life Sci. 2010;67:524-544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Robert R, Nail S, Marot-Leblond A, et al. . Adherence of platelets to Candida species in vivo. Infect Immun. 2000;68:570-576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Eberl C, Speth C, Jacobsen ID, et al. . Candida: platelet interaction and platelet activity in vitro. J Innate Immun. 2019;11:52-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rødland EK, Ueland T, Pedersen TM, et al. . Activation of platelets by Aspergillus fumigatus and potential role of platelets in the immunopathogenesis of aspergillosis. Infect Immun. 2010;78:1269-1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smith NL, Bromley MJ, Denning DW, et al. . Elevated levels of the neutrophil chemoattractant pro-platelet basic protein in macrophages from individuals with chronic and allergic aspergillosis. J Infect Dis. 2015;211:651-660. [DOI] [PubMed] [Google Scholar]
- 38. Perkhofer S, Kainzer B, Kehrel BE, et al. . Potential antifungal effects of human platelets against zyogomycetes in vitro. J Infect Dis. 2009;200:1176-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sugiyama MG, Gamage A, Zyla R, et al. . Influenza virus infection induces platelet-endothelial adhesion which contributes to lung injury. J Virol. 2016;90:1812-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Antonov AS, Antonova GN, Munn DH, et al. . αVβ3 integrin regulates macrophage inflammatory responses via PI3 kinase/Akt-dependent NF-κB activation. J Cell Physiol. 2011;226:469-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Weyrich AS, Zimmerman GA. Platelets in lung biology. Annu Rev Physiol. 2013;75:569-591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Morrell CN, Aggrey AA, Chapman LM, et al. . Emerging roles for platelets as immune and inflammatory cells. Blood. 2014;123:2759-2767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ogura H, Kawasaki T, Tanaka H, et al. . Activated platelets enhance microparticle formation and platelet-leukocyte interaction in severe trauma and sepsis. J Trauma. 2001;50:801-809. [DOI] [PubMed] [Google Scholar]
- 44. Wang Y, Zhang S, Luo L, et al. . Platelet-derived microparticles regulate thrombin generation via phosphatidylserine in abdominal sepsis. J Cell Physiol. 2018;233:1051-1060. [DOI] [PubMed] [Google Scholar]
- 45. Lefrançais E, Ortiz-Muñoz G, Caudrillier A, et al. . The lung is a site of platelet biogenesis and a reservoir for haematopoietic progenitors. Nature. 2017;544:105-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Aschoff L. Uber capillare Embolie von riesenkemhaltigen Zellen. Arch Pathol Anat Phys. 1893;134:11-14. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.