Abstract
Background
Since late 2019, the outbreak of COVID-19 has rapidly spread worldwide. As it is a newly emerged disease, many of its manifestations and complications are unknown to us. Cardiac involvement and arrhythmias are another aspect of the disease about which very little is known.
Case summary
A 71-year-old male patient presented at the Emergency Department complaining of fever, a dry cough, and dyspneoa. He was admitted due to these symptoms suggestive of COVID-19, and a chest CT and PCR test confirmed the diagnosis. During admission, cardiac involvement was detected, i.e. second-degree atrioventricular block with intermittent left bundle branch block (LBBB) which progressed to fixed LBBB and eventually developed into atrial fibrillation/flutter with bradycardia. Both cardiac troponin and echocardiographic findings for detecting myocarditis were negative. We waited 14 days for resolution of atrioventricular block before permanent pacemaker implantation, but the condition still did not improve after the waiting period.
Discussion
COVID-19 is mainly a respiratory infection but cardiac involvement is not uncommon in the course of the disease. Arrhythmia, during this infection, seems to be caused by an inflammatory response in the myocardium, electrolyte disturbances, and hypoxia; the course of the disease in our case study shows that the virus can preferentially and irreversibly involve the cardiac conduction system.
Keywords: Case report, COVID-19, Atrioventricular block, Myocarditis
Learning points
Conduction system disturbances in COVID-19 are mainly caused by an inflammatory response, and all types of arrhythmias are associated with this process.
COVID-19 can involve the conduction system preferentially, without myocardial involvement.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), like the previous strains of coronavirus, MERS-CoV and SARS-CoV, is mainly a respiratory virus. In our evolving knowledge of this novel virus, many aspects of the disease are unknown. Still, reports are suggesting that SARS-CoV-2 can affect many organs and systems similar to the other virulent coronaviruses.
In addition to the main presentation of the novel coronavirus disease 2019 (COVID-19), which is pneumonia and respiratory system impairment, cardiovascular complications are another important aspect of the disease that might cause serious and irreversible damage. Herein, we report a case of COVID-19 with cardiac damage which preferentially involved the conduction system.
Timeline
| Admission | Admission due to symptoms suggestive of COVID-19 |
|---|---|
| Day 3 | 2:1 atrioventricular block with intermittent left bundle branch block (LBBB) |
| Day 4 | 2:1 atrioventricular block with fixed LBBB |
| Day 6 | Atrial fibrillation with bradycardia |
| Day 14 | Pacemaker implantation |
Case presentation
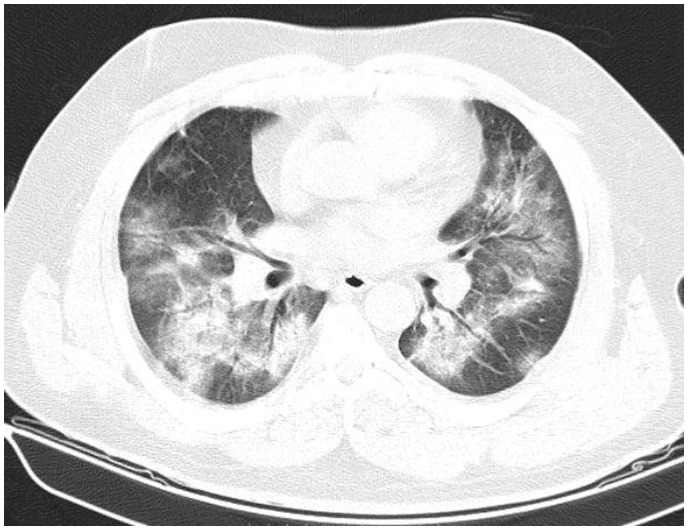
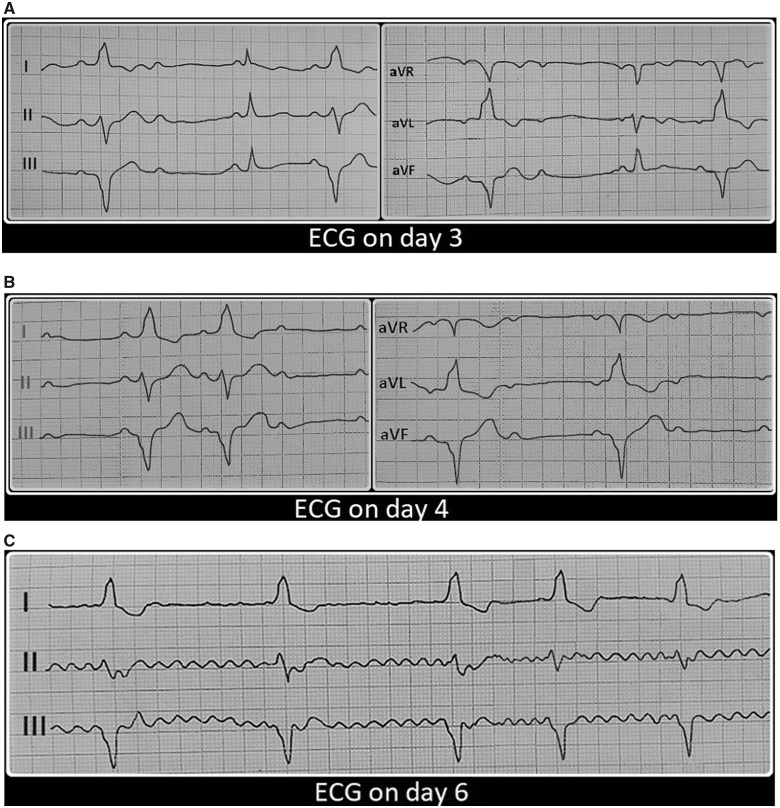
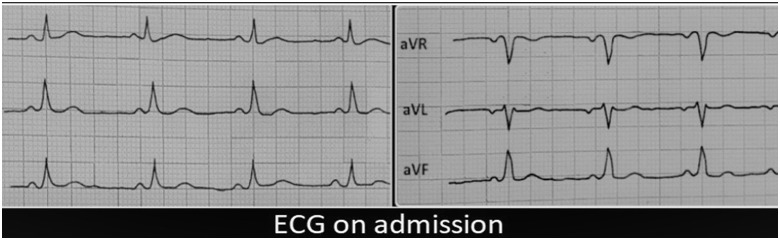
The patient was a 71-year-old man with no noteable past medical history who presented to the Emergency Department (ED) with weakness, fever, a dry cough, and dyspnoea. On physical exam, his temperature was 38.5°C, pulse rate 71 b.p.m., respiratory rate 26 breaths/min, O2 saturation 85% (on room air), and blood pressure 110/80 mmHg. Routine blood test showed a white blood cell count of 10.4 × 109/L, lymphocyte count of 1.3 × ×109/L, and C-reactive protein >3 mg/L. The patient was admitted due to symptoms suggestive of SARS-CoV-2 infection during the outbreak period and underwent double-drug therapy with hydroxychloroquine (400 mg as a single dose) and combination of lopinavir plus ritonavir (200/50 mg every 12 h). A chest CT (Figure 1) and PCR test for COVID-19 confirmed the diagnosis. The electrocardiogram (ECG) on the third day of admission displayed second-degree atrioventricular (AV) block with intermittent left bundle branch block (LBBB) (Figure 2and3A). Antiviral drugs were discontinued after 2 days because AV block due to drug side effects was suspected. Due to this complication, cardiac enzyme (troponin) was measured in two blood samples 9 h apart and both test results were negative. Echocardiography was performed and showed neither pericardial effusion nor reduction in ejection fraction. On the following day, there were changes in ECG readings, showing a 2:1 AV block (Mobitz II) with fixed LBBB (Figure 3B), and he eventually developed episodes of paroxysmal atrial fibrillation with bradycardia on the sixth day (Figure 3C) despite improvement in O2 saturation (90%). Since we had had experience of COVID-19 patients with reversible heart block, we waited for a couple of weeks for resolution of AV block but it was irreversible and did not improve after the waiting period. Hence, a dual-chamber permanent pacemaker was implanted through the left subclavian approach. During the 1 month follow-up, pacemaker analysis revealed the persistence of AV block.
Figure 1.
Chest CT showed bilateral ground-glass opacities.
Figure 3.
(A) 2:1 atrioventricular block with intermittent left bundle branch block. (B) 2:1 atrioventricular block (Mobitz II) with fixed left bundle branch block. (C) Paroxysmal episodes of atrial fibrillation with bradycardia.
Figure 2.
ECG on admission.
Discussion
The recent outbreak caused by a newly emerged coronavirus has spread worldwide, and we are faced with lesser known features and complexities of the disease. It is well known that a wide spectrum of viruses can cause myocarditis. There are many reports that indicate that SARS-CoV-2 is one of these cardiotropic viruses, and myocardial injury can occur in 7–17% of patients.1 Myocardial injury and conduction system disturbances in viral infections are mainly caused by an inflammatory response, and all types of tachyarrhythmia and bradyarrhythmia are associated with this inflammatory process. Both innate and adaptive immune responses are involved in myocardial and conduction system injury.2 Clinically, this injury can manifest as conduction block in the AV node or in the infranodal system and reversibility is related to the severity of inflammation.3
Although SARS-CoV-2 seems to be mainly a respiratory virus, cardiac complications are not uncommon. Arrhythmia in these patients is reported in up to 16.7% of cases.1 It is known that some of these arrhythmias including conduction blocks are related to the side effects of medications such as hydroxychloroquine and combination of lopinavir plus ritonavir, and, if these arrhythmias occur, it is recommended that antiviral drugs be discontinued.4 In COVID-19 patients, as in patients infected with other cardiotropic viruses, inflammation is probably the main cause of arrhythmias but, in addition to this, hypoxia and electrolyte disturbances caused by renal impairment can also be involved.
It is noteworthy that it was first reported in this case study that despite the occurrence of conduction system impairment, both echocardiographic findings for diagnosing myocarditis and cardiac troponin were negative. These findings illustrate that irreversible cardiac damage in COVID-19 can occur preferentially in the conduction system without myocardial inflammation and injury. Nevertheless, isolated conduction system disturbances are not uncommon in infectious diseases; for example, Lyme disease can present with similar manifestations.5
Furthermore, an important issue to consider is that as the number of patients increases during the outbreak, the probability of detection of coincident disorders will also increase. Accordingly, in our case study, concurrent COVID-19 and AV block may be merely coincident, and a causal link between the two cannot be proved.
Conclusions
Notwithstanding the fact that COVID-19 can cause myocarditis and, consequently, conduction disturbances, it can involve conduction system preferentially without myocardial involvement.
Lead author biography

Dr Alireza Malekrah is a cardiac electrophysiologist at Mazandaran Heart Center Hospital. He received his Medical Degree from Tehran’s Shahid Beheshty University of Medical Science and then completed cardiology and electrophysiology fellowship training at Mazandaran and Tehran University of Medical Science. respectively.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Patient consent: The author/s confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Ethic code: IR.MASUMS..REC.1399.7884
Conflicts of interest: none declared.
Supplementary Material
References
- 1. Xiong TY, Redwood S, Prendergast B, Chen M.. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J 2020;41:1798–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yajima T, Knowlton KU.. Viral myocarditis: from the perspective of the virus. Circulation 2009;119:2615–2624. [DOI] [PubMed] [Google Scholar]
- 3. Caughey RW, Humphrey JM, Thomas PE.. High-degree atrioventricular block in a child with acute myocarditis. Ochsner J 2014;14:244–247. [PMC free article] [PubMed] [Google Scholar]
- 4. Chong VH, Chong PL, Metussin D, Asli R, Momin RN, Mani BI, Abdullah MS.. Conduction abnormalities in hydroxychloroquine add on therapy to lopinavir/ritonavir in COVID-19. J Med Virol 2020;doi: 10.1002/jmv.26004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kannangara DW, Sidra S, Pritiben P.. First case report of inducible heart block in Lyme disease and an update of Lyme carditis. BMC Infect Dis 2019;19:428. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.