Abstract
Background
Although attention is focused on addressing the acute situation created by the COVID-19 illness, it is imperative to continue our efforts to prevent cardiovascular morbidity and mortality, particularly during a period of prolonged social isolation which may limit physical activity, adversely affect mental health and reduce access to usual care. One option may be to deliver healthcare interventions remotely through digital healthcare solutions. Therefore, the aim of this paper is to bring together the evidence for remote healthcare during a quarantine situation period to support people living with cardiovascular disease during COVID-19 isolation.
Methods
The PubMed, CINAHL and Google Scholar were searched using telehealth OR digital health OR mHealth OR eHealth OR mobile apps AND COVID-19 OR quarantine search terms. We also searched for literature relating to cardiovascular disease AND quarantine.
Results
The literature search identified 45 potentially relevant publications, out of which nine articles were included. Three overarching themes emerged from this review: (1) preparing the workforce and ensuring reimbursement for remote healthcare, (2) supporting mental and physical health and (3) supporting usual care.
Conclusion
To support people living with cardiovascular disease during COVID-19 isolation and to mitigate the effects of quarantine and adverse effect on mental and physical well-being, we should offer remote healthcare and provide access to their usual care.
Keywords: Cardiovascular disease, COVID-19, remote healthcare, digital health, telehealth, quarantine, isolation
Background
Cardiovascular disease (CVD) is estimated to be responsible for almost 18 million deaths per year globally.1 Although attention is focused on addressing the acute situation created by the COVID-19 illness, it is imperative to continue our efforts to prevent cardiovascular morbidity and mortality, particularly during a period of prolonged social isolation which may limit physical activity and adversely affect mental health. The virus, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), first emerged in December 2019. By early April 2020 there were over a million confirmed cases of COVID-19 reported worldwide, with 46,891 deaths.2 Worryingly, complications and deaths appear to be higher in those with known CVD.3 While preparations for management of acute cases and field hospitals being established dominate our news, another alarming trend is appearing: people with chest pain or other cardiac symptoms that need acute care are delaying presentation at hospital, potentially with catastrophic effects.4–6 It is suggested that the causes of delays for chest pain presentation are likely multifactorial, but may include a fear of attending hospital due to perceived risk of contracting an infection, or because of limited emergency medical services due to staff who are ill or self-isolating, or systemic overload.6 Furthermore, patients observe how overstretched the healthcare system is and fear creating an additional burden, so minimize symptoms.6
In addition to delaying presentation, people with CVD are facing the largest quarantine that the world has ever known. Approximately one-third of the world is now in some form of quarantine.7 The word ‘quarantine’ originates from the Italian word for 40, ‘quaranta’, since people with illness that were feared to be contagious were isolated from others for 40 days.8 During this current crisis people may face much longer in quarantine. For example, in the UK during COVID-19, several groups of people who are considered to be at very high risk have been advised to remain in isolation for 12 weeks.9 This form of isolation is being described as ‘shielding’ and includes staying at home, avoiding situations where you come into contact with other people, such as in a supermarket queue or on public transport, asking others if they can shop for basic essentials, collect prescriptions or do anything that can help you to avoid going out. Even in the moderate risk group, which most people living with CVD will be in, the request is to practise ‘stringent social distancing’.9
Consequently, it is unsurprising that global physical activity levels are falling. A study in the USA has shown that physical activity, measured objectively by Fitbit trackers, has fallen by 39% in the month of March since social distancing measures were implemented.10 This is of great concern, as physical activity has well-established benefits for primary11 and secondary prevention of CVD. In patients with CVD12,13 physical activity can lead to a reduction in cardiovascular mortality and the risk of hospital admissions and improvement of quality of life.14 Indeed, one in four adults in the world and approximately half of CVD patients were already insufficiently active,15 and this will be adversely affected by any form of prolonged isolation.
As well as adversely affecting physical health, it is clear that psychosocial health will be affected by social isolation and quarantine. A rapid review of the psychological impact of quarantine highlighted that frustration and boredom are common, and that many people experience anxiety and depression.16 Low mood and irritability are particularly noted, and the authors comment on the importance of minimizing the duration of quarantine, and of effective and rapid communication.16 One study showed that after the severe acute respiratory syndrome (SARS) quarantine, some people experienced depressive symptoms for at least three years following quarantine.17 Because anxiety and depression are well known predictors of poor outcome in CVD,18 it is essential that people with CVD are supported and have clear channels of communication that are relevant to their health during the current COVID-19 pandemic.
Although the importance of clear communication with people who can offer appropriate support would appear to be vital, many providers of health advice for people with CVD, such as cardiac rehabilitation staff, are being redeployed into acute care. One option may be to deliver healthcare interventions remotely through digital healthcare solutions. Therefore, the aim of this paper is to bring together the evidence for remote healthcare during a quarantine situation period to support people living with CVD during COVID-19 isolation.
Methods
A rapid review methodology was used to bring together the evidence.19 Searches were conducted between 27 March 2020 and 1 April 2020. We searched PubMed, CINAHL and Google Scholar. Search terms included telehealth OR digital health OR mHealth OR eHealth OR mobile apps AND COVID-19 OR quarantine. We also searched for literature relating to cardiovascular disease AND quarantine. We included papers published in English that focused on use of technology to support people with cardiovascular disease to manage their health during times of quarantine. We excluded papers that used technology to identify clusters of COVID-19 or to track or predict outbreaks of the virus. Our search was limited to the years 2000–2020 to ensure we captured information about quarantine in the digital age. A subsample of 20% of abstracts was reviewed by a second reviewer. Risk of bias was not assessed due to the limited literature available and the lack of trials in this area.
Results
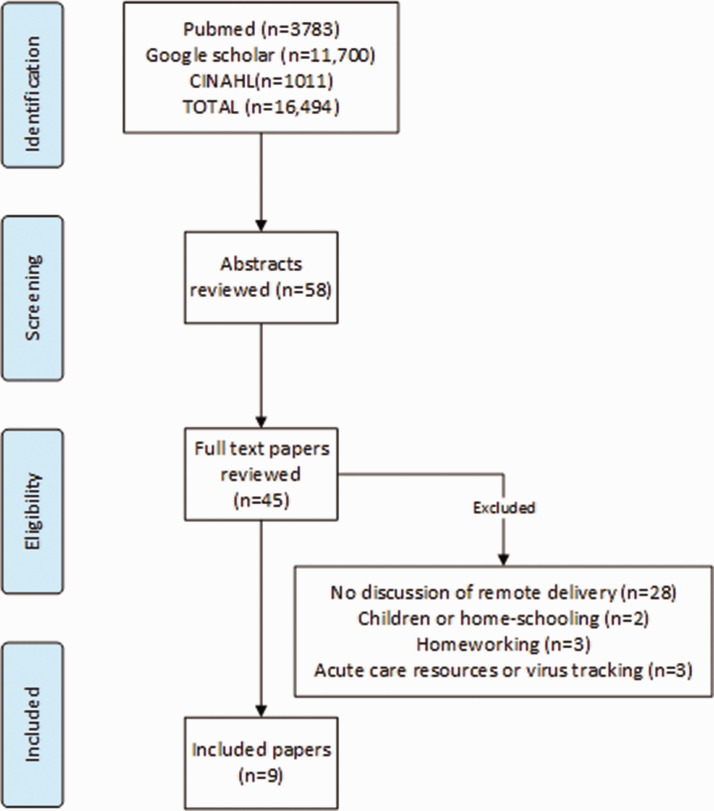
We reviewed over 16,000 titles (Figure 1). Fifty-eight abstracts were reviewed, 45 full text papers were considered and nine papers20–28 fitted the inclusion criteria for this review (Table 1). All included papers came from high income countries. All were ‘expert opinion’ papers, only one paper came from prior to 2020 and this was a book chapter. Quality of the evidence was therefore not assessed, as there were no trials included. Three overarching themes emerged from this review.
Figure 1.
Flowchart of included papers.
Table 1.
Included papers.
| Author and date | Country | Type of paper | Focus | Recommendations |
|---|---|---|---|---|
| Bachireddy et al., 202021 | USA | Expert opinion | Reimbursement and redesign of services | Removing Medicaid restrictions on telehealth should alleviate healthcare burden and reduce COVID-19 transmission |
| Greenhalgh et al., 202024 | UK | Expert opinion | Preparing for adoption at scale | Staff need training to deliver telehealth. During COVID-19 this should ideally be delivered remotely. Guidance is needed to support optimal use of video consultation |
| Kun, 200720 | Book chapter | Preparing for isolation | Developing a connected home environment with access to a range of services including banking, health, shopping and entertainment on demand should minimize the effects of isolation during quarantine. Telehealth platforms should include electronic health records | |
| Lee et al., 202027 | USA | Expert opinion | Use of telehealth to maintain normal services | Telemedicine can maintain access and continuity of care for patients, support colleagues on the front-line, optimize in-person services and minimize infectious transmission of COVID-19 coronavirus |
| Smith et al., 202022 | Australia | Expert opinion | Preparation for delivery of telehealth at scale | Ensure that all health professionals receive appropriate education and trainingIntroduce telehealth accreditation for health professionalsProvide funding which adequately covers the cost of providing telehealthRedesign clinical models of careSupport all stakeholders with an effective communication and change management strategyEstablish systems to manage telehealth services on a routine basis |
| Ting et al., 202023 | Singapore | Expert opinion | Use of a range of digital technology | Healthcare systems should plan to use digital technology. This would ensure that patients continue to receive standard clinical care while reducing physical crowding of patients into hospital premises |
| Torous et al., 202028 | USA | Expert opinion | Mental health and digital technology | Digital health can be used to increase access and quality of mental health. There is a need for workforce training, high-quality evidence and digital equity |
| Yeo et al., 202026 | Singapore | Expert opinion | Providing cardiac rehabilitation remotely during COVID-19 | Cardiac rehabilitation (CR) providers should explore and implement methods to improve or supplement existing programmes. Utilizing technology for CR delivery can provide the much-needed boost to CR programmes during and beyond the COVID-19 outbreak |
| Zhou et al., 202025 | Australia | Expert opinion | Mental health support during isolation | Telehealth for mental health support is practically feasible and appropriate for the support of patients, family and healthcare workers. The psychological side effects of COVID-19 are likely to be high and will have long-term impacts beyond the duration of quarantine |
Theme 1. Preparing the workforce and ensuring reimbursement for remote healthcare
Overall, all papers commented on the importance of telehealth to improve access to services during any form of quarantine. Over 10 years ago, it was recognized that having a digitally connected home could mitigate the effects of quarantine.20 Despite that, it is clear that substantial work needs to be undertaken to prepare the health systems for delivering healthcare remotely. First, mechanisms need to be made available to reimburse healthcare providers for work done remotely.21–23 Second, staff may need upskilling and resources may need to be made available to provide suitable equipment and technology to ensure rapid deployment of remote health solutions.22,24 Staff who already have skills in remote delivery could not only be leveraged to provide support to people with CVD, but could also provide training and support to those who are new to it.24
Theme 2. Supporting mental and physical health
The adverse effects on mental and physical well-being in patients were noted.25 It is recommended that providers transition to providing remote resources to support people living with CVD.26 In particular, it was highlighted that patients are usually offered cardiac rehabilitation following on from a cardiac event, but this may have ceased as providers are called back to acute care roles to support immediate management of COVID-19.26 Therefore, given the well-known benefits of cardiac rehabilitation on cardiovascular risk factors, quality of life and the reduction of morbidity and mortality, transitioning existing cardiac rehabilitation programmes online seems to be critical in maintaining the health of people with CVD.26
Theme 3. Supporting usual care
For people with CVD, it is vital that they have access to their usual care. They need to be able to access their medications, and online pharmacies could provide a solution to enabling vulnerable people to obtain medications.20,27 Furthermore, access to healthy food and other essential supplies can be obtained remotely.20 It was noted that anxiety during the recent months has led to panic buying,28 and this is something that may make obtaining essential supplies remotely more challenging for those who have previously had limited access to technology and are having to rapidly upskill in use of digital technology.
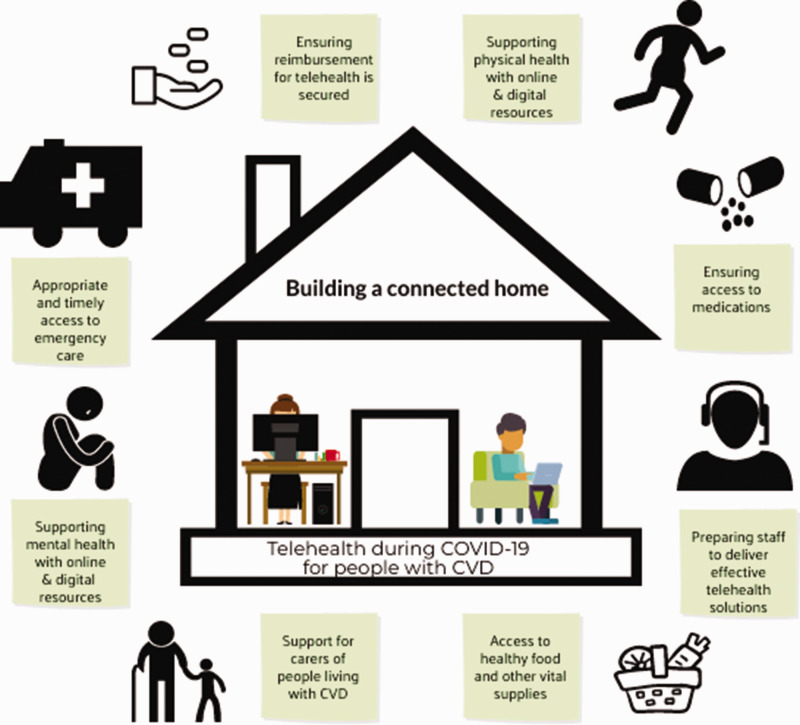
The findings of this review are synthesized into our ‘top 10 recommendations for remote delivery of healthcare to CVD patients’ (Table 2). These overarching themes, together with our own experience of looking after patients with CVD in the community, led us to develop a conceptual model for a CVD patient (Figure 2) which highlights the key findings of this review, with the addition of one essential point. People with CVD need to know that it is still vitally important that they seek appropriate healthcare if they experience sudden changes in their symptoms. For example, if a patient has chest pain, they should still call for an ambulance. Although the ‘stay at home’ message is vitally important, CVD emergencies will still occur, and if people with CVD do not seek help in a timely fashion the consequences could be grave.
Table 2.
Top 10 recommendations for remote delivery of healthcare to CVD patients.
| 1. Use existing systems and platforms (patient portals) to encourage patients to initiate remote healthcare when available. |
| 2. Create a system that allows some time for urgent consultations. Patients are frightened and they need to be able to ask questions about their health. |
| 3. Provide routine appointments to CVD patients either through telephone or online services. |
| 4. Work with colleagues to ensure that patients are not required to access multiple unconnected services. For example, a telehealth service providing prescriptions to CVD patients will not succeed if pharmacy is not included in the care pathway. |
| 5. Make sure patients know there is a clear line of communication to minimize emergency department overuse for non-critical issues. |
| 6. Ensure that patients with CVD know that sudden change in cardiac symptoms, including breathlessness, chest pain and oedema, still require urgent treatment. |
| 7. Consider use of connected technology. For example, digital trackers, blood pressure monitors, weighing scales to monitor and support. |
| 8. Ensure privacy, keep it simple, if people need support to start, consider creating a downloadable PDF ‘how-to’ guide. |
| 9. Resources can be delivered synchronously (i.e. in real time) or asynchronously. Each has a place in supporting people with CVD. |
| 10. Audit your data and report it so that best practice in remote delivery can be upscaled, and lessons learnt can be shared with colleagues around the world. |
CVD: cardiovascular disease.
Figure 2.
Conceptual model for telehealth during COVID-19 for people with cardiovascular disease (CVD).
Discussion
This review indicates that a large body of literature has been generated in a small amount of time, but there is very little work conducted to understand the effects of prolonged quarantine on cardiovascular health, or outcomes of remote delivery of advice and support to people living with CVD during quarantine. Consequently, recommendations to use telehealth during COVID-19 are written by experts in the field who have experience of remote delivery of healthcare solutions. The 2007 paper by Kun suggests that we could have been better prepared for a quarantine scenario, and emphasizes the need to proactively develop protocols and systems for rapid change to healthcare delivery.20 While our review highlighted the importance of reimbursement mechanisms, we contend that telehealth has now moved beyond an optional extra to become an essential service that must be funded.
Despite increased requirements for the patient to initiate and maintain self-care and self-management in the COVID-19 social distancing context, discussion on these points was very limited in the literature reviewed. As self-care tends to decline over time29 and support from health professionals is independently predictive of long-term adherence to cardiac treatment,30 strategies that promote independent self-care are urgently needed. Strategies that promote increased perceived control may be beneficial given the association with self-care in Liljeroos et al. (2020).29 In most non-invasive remote healthcare patients and/or family caregivers need to take an active role and be motivated to gather data of signs and symptoms (self-care monitoring) and to respond to changes if needed (self-care management). Some patients might experience challenges for remote healthcare since they suffer from sensory, cognitive and physical decline and this needs to be taken into account when offering telehealth.31
It is probable that people with CVD will experience lasting effects of social isolation and reduced physical activity beyond COVID-19. Overall, this review suggests that proactive use of telehealth could mitigate some of these effects. People living with CVD are frightened and have many questions about COVID-19 and what they should or should not do. A recent paper from the European Society of Cardiology patient forum highlights the many questions that patients are asking about their health during COVID-19 and offers answers to these,32 although it is likely that people will have many more concerns that could be effectively supported through remote services. Although the papers in our review did not highlight the importance of routine follow-up appointments, including with General Practitioners, cardiologists and specialist nursing or allied professional services, it is our contention that continued support and care will reduce some of the potential adverse effects people with CVD may experience following quarantine.
In addition, other sources of support are available, including patient forums. Cardiac patients are interested in other patients’ experiences33 and social media provides a useful tool for patients to meet and provide mutual support.34 There are many examples of patient forums, for example, PatientsLikeMe (https://www.patientslikeme.com/) or the Arrhythmia Alliance (https://www.heartrhythmalliance.org), but the benefits of such forums are poorly investigated. Referring patients to an appropriate website may be necessary to support at distance, but when doing so, healthcare professionals need to ensure that the content of the site is appropriate and user-friendly.35 The Heart Failure Matters website is an example of a user-friendly website with reliable information36 which offers updates on the consequences of the COVID-19 pandemic for heart failure patients in 10 languages and also gives the opportunity to discuss experiences via a dedicated Facebook forum (https://www.heartfailurematters.org).
Although online resources are not listed in standard academic databases, there is a range of available tools that are being made available at this time, and in Table 3 we have highlighted a few that are available. This list is not intended to be exhaustive, and should be used only as a guide. One exemplar from this list is TeleCheckAF – a programme that started in March 2020, and now has 13 sites enrolled across Europe. Scalability of services depends on cooperation, and pockets of excellence will only benefit a minority of people. Therefore, it is critical that we share best practice and ensure we collaborate to support people with CVD.
Table 3.
Examples of useful online resources for CVD patients or starting telehealth.
| Type of resource | Country of origin | Web address |
|---|---|---|
| Questions and answers about COVID-19 from ESC patient forum | Europe | https://www.escardio.org/Education/COVID-19-and-Cardiology/what-heart-patients-should-know-about-the-coronavirus-covid-19 |
| Online version of the Heart Manual – evidence based home cardiac rehabilitation programme | UK | https://www.heartmanual.scot.nhs.uk/ |
| Online cardiac rehabilitation sessions conducted via Zoom meetings | Canada | https://www.healtheuniversity.ca/en/cardiaccollege |
| Links to resources to keep health during COVID-19 | UK | https://www.bhf.org.uk/informationsupport/heart-matters-magazine/wellbeing/how-to-keep-healthy-while-you-cant-go-out |
| Video on how to establish online cardiac rehabilitation | USA | https://www.youtube.com/watch?v=MyZHL0zO5j8&feature=youtu.be |
| Tips for heart failure patients from Heart Failure Matters | Europe | https://www.heartfailurematters.org/en_GB/General/COVID-19-Virus-and-Heart-Failure-Information-and-Practical-Tips |
| TeleCheckAF– online programme for patients using FibriCheck to monitor atrial fibrillation and connect with cardiology services during COVID-19 | Netherlands | https://twitter.com/Dominik_Linz/status/1247203392532951045 |
ESC: European Society of Cardiology.
Of course, with any new service, there must be caveats: we do not know what the outcomes of deploying remote healthcare during quarantine will actually be. Although studies have shown favourable outcomes for people with CVD who access healthcare through remote technology, they have also noted that these are complex interventions, and the ‘active ingredient’ is always hard to determine.37 Indeed, no single intervention has been delivered without some form of face-to-face component, even if it is only to recruit participants into the study. Furthermore, the quality of communication delivered via remote technology is likely to be significant in ensuring appropriate healthcare access. In a recent study looking at the effects of telecare on presentation with myocardial infarction, skilled probing to elicit an accurate history was critical in timely use of emergency services.38 Similarly, the paper by Greenhalgh et al. emphasized the need for training to conduct remote healthcare delivery effectively.24 This is echoed by a study conducted to deploy telemedicine for stroke patients, in which nurses had a vital role to play in ensuring uptake, but also they may feel less prepared or willing to adopt telemedicine than non-nursing colleagues.39 One of the challenges we may face is preparing staff to provide remote care when training must also be conducted remotely.
One key obstacle that has not been addressed in this review is global access to digital technology. There is a potential that making services available through digital technology may exclude those who cannot afford access to digital devices, and it is likely that those who are most vulnerable will suffer most. All of the included literature came from high income countries, where access to the Internet is as high as 95%.40 Although rapid deployment of technology is possible, it needs to be matched by an effort to ensure that everyone who needs support can access it.
Finally, this review was conducted in a very short timeframe, and the literature has been evolving daily. Despite that, there are few papers that contain original research. Our findings from this review suggest that what is urgently needed is long-term monitoring of the effects of quarantine on cardiovascular health and evaluation of remote healthcare on the quality of life and healthcare outcomes for people with CVD. We strongly encourage our colleagues who are delivering care to CVD patients remotely to audit their programmes and to report these findings to inform future developments. It is likely that patients will suffer if all resources are diverted to acute care, so we call on healthcare policy makers and payers to ensure that routine care is not overlooked, and to support people with CVD during and beyond COVID-19.
Limitations
Due to the rapidly evolving literature on this topic, it is likely that more has been published even since the initial search was conducted. It is also possible that the search terms were not exhaustive, since we did not specifically look at the terms ‘social isolation’ or ‘social distancing’. The papers are predominantly calls to action to improve healthcare management with digital interventions and the extent of effect these interventions have on CVD is unclear. A large number of resources may not have been identified, as they are being deployed. Longer term outcomes of quarantine and CVD are not known.
Conclusions
There is very little literature on the effects of quarantine on people living with CVD, but experts agree that telehealth is likely to provide an opportunity to ensure that people living with CVD are supported during COVID-19. Urgent research is required during this crisis, and systems must be developed and supported that enable staff to upskill and allow long-term follow-up of people with CVD who have experienced quarantine, social isolation or social distancing.
Acknowledgement
We gratefully thank Inga Drossart from the European Society of Cardiology for her review of this paper from a patient perspective.
Declaration of conflicting interests
The authors have no conflicts of interest to declare.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1. World Health Organization. Cardiovascular diseases, https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (2017, accessed 30 March 2020).
- 2. European Centre for Disease Prevention and Control. COVID-19- Situation update worldwide, as of 2 April 2020, https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (2020, accessed 3 April 2020).
- 3. Madjid M, Safavi-Naeini P, Solomon SD, et al. Potential effects of coronaviruses on the cardiovascular system: A Review. JAMA Cardiol. Epub ahead of print 27 March 2020. DOI: 10.1001/jamacardio.2020.1286. [DOI] [PubMed] [Google Scholar]
- 4.Jaarsma T, van der Wal M, Hinterbuchner L, et al. Flexibility and safety in times of coronavirus disease 2019 (COVID-19): Implications for nurses and allied professionals in cardiology. Eur J Cardiovasc Nurs. 2020; 19: 462–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tam C-CF, Cheung K-S, Lam S, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment -elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. Epub ahead of print 17 March 2020. DOI: 10.1161/CIRCOUTCOMES.120.006631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wood S. The mystery of the missing STEMIs during the COVID-19 pandemic, https://www.tctmd.com/news/mystery-missing-stemis-during-covid-19-pandemic (2020, accessed 3 April 2020).
- 7. Kaplan J, Frias L, McFall-Johnsen M A third of the global population is on coronavirus lockdown – here’s our constantly updated list of countries and restrictions, https://www.businessinsider.com/countries-on-lockdown-coronavirus-italy-2020-3?r=US&IR=T (2020, accessed 31 March 2020).
- 8. Centers for Disease Control and Prevention. History of quarantine, https://www.cdc.gov/quarantine/historyquarantine.html (2012, accessed 31 March 2020).
- 9. Public Health England. Guidance on shielding and protecting people defined on medical grounds as extremely vulnerable from COVID-19, https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 (2020, accessed 31 March 2020).
- 10. Evidation Health. COVID-19 Pulse: Delivering weekly insights on the pandemic from a 150,000+ person connected cohort, https://evidation.com/news/covid-19-pulse-first-data-evidation/ (2020, accessed 31 March 2020).
- 11. World Health Organization. Global action plan on physical activity 2018–2030: More active people for a healthier world. Geneva: World Health Organization, 2018.
- 12. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2015; 18: 891–975. [DOI] [PubMed] [Google Scholar]
- 13. Piepoli MF, Conraads V, Corrà U, et al. Exercise training in heart failure: from theory to practice. A consensus document of the Heart Failure Association and the European Association for Cardiovascular Prevention and Rehabilitation. Eur J Heart Fail 2011; 13: 347–357. [DOI] [PubMed] [Google Scholar]
- 14. Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J Am Coll Cardiol 2016; 67: 1–12. [DOI] [PubMed] [Google Scholar]
- 15. Dontje ML, van der Wal MH, Stolk RP, et al. Daily physical activity in stable heart failure patients. J Cardiovasc Nurs 2014; 29: 218–226. [DOI] [PubMed] [Google Scholar]
- 16. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020; 395: 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu X, Kakade M, Fuller CJ, et al. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatry 2012; 53: 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hare DL, Toukhsati SR, Johansson P, et al. Depression and cardiovascular disease: A clinical review. Eur Heart J 2014; 35: 1365–1372. [DOI] [PubMed] [Google Scholar]
- 19. Tricco AC, Langlois EV, Straus SE Rapid reviews to strengthen health policy and systems: A practical guide. Geneva: World Health Organization, 2017. [Google Scholar]
- 20. Kun L. The use of technology to transform the home into a safe-haven. Stud Health Technol Inform 2007; 127: 18–27. [PubMed] [Google Scholar]
- 21. Bachireddy C, Chen C, Dar M Securing the safety net and protecting public health during a pandemic: Medicaid’s response to COVID-19. JAMA. Epub ahead of print 19 March 2020. DOI: 10.1001/jama.2020.4272. [DOI] [PubMed] [Google Scholar]
- 22. Smith A, Thomas E, Snoswell C, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. Epub ahead of print 20 March 2020. DOI: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ting D, Carin L, Dzau V, et al. Digital technology and COVID-19. Nat Med 2020; 26: 459–461. [DOI] [PMC free article] [PubMed]
- 24. Greenhalgh T, Wherton J, Shaw S, et al. Video consultations for covid-19. BMJ 2020; 368: m998. [DOI] [PubMed] [Google Scholar]
- 25. Zhou X, Snoswell C, Harding L, et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed J E-Health 2020; 26: 377–379. [DOI] [PubMed]
- 26. Yeo TJ, Wang Y-TL, Low TT Have a heart during the COVID-19 crisis: Making the case for cardiac rehabilitation in the face of an ongoing pandemic. Eur J Prev Cardiol. Epub ahead of print 1 April 2020. DOI: 10.1177/2047487320915665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee I, Kovarik C, Tejasvi T, et al. Telehealth: Helping your patients and practice survive and thrive during the COVID-19 crisis with rapid quality implementation. J Am Acad Dermatol 2020; 82: 1213–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Torous J, Myrick K, Rauseo-Ricupero N, et al. Digital mental health and COVID-19: Using technology today to accelerate the curve on access and quality tomorrow. JMIR Mental Health 2020; 7: e18848. [DOI] [PMC free article] [PubMed]
- 29. Liljeroos M, Kato NP, van der Wal MH, et al. Trajectory of self-care behaviour in patients with heart failure: The impact on clinical outcomes and influencing factors. Eur J Cardiovasc Nurs. 2020; 19: 421–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kähkönen O, Kyngäs H, Saaranen T, et al. Support from next of kin and nurses are significant predictors of long-term adherence to treatment in post-PCI patients. Eur J Cardiovasc Nurs 2020; 19: 339–350. [DOI] [PubMed] [Google Scholar]
- 31. Allemann H, Poli A Designing and evaluating information and communication technology-based interventions? Be aware of the needs of older people. Eur J Cardiovasc Nurs. 2020; 19: 370–372. [DOI] [PubMed] [Google Scholar]
- 32. European Society of Cardiology Patient Forum. COVID-19 and heart patients (Q&A), https://www.escardio.org/Education/COVID-19-and-Cardiology/what-heart-patients-should-know-about-the-coronavirus-covid-19 (2020, accessed 2 April 2020).
- 33. Schweier R, Grande G, Richter C, et al. In-depth statistical analysis of the use of a website providing patients’ narratives on lifestyle change when living with chronic back pain or coronary heart disease. Patient Educ Couns 2018; 101: 1283–1290. [DOI] [PubMed] [Google Scholar]
- 34. Partridge SR, Grunseit AC, Gallagher P, et al. Cardiac patients’ experiences and perceptions of social media: Mixed-methods study. J Med Internet Res 2017; 19: e323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Klompstra L, Östbring MJ, Jaarsma T, et al. The appropriateness and presentation of commonly available cardiovascular web pages providing information about cardiovascular diseases. Comput Inform Nurs 2019; 37: 493–497. [DOI] [PubMed] [Google Scholar]
- 36. Wagenaar KP, Rutten FH, Klompstra L, et al. ‘heartfailurematters. org’, an educational website for patients and carers from the Heart Failure Association of the European Society of Cardiology: Objectives, use and future directions. Eur J Heart Fail 2017; 19: 1447–1454. [DOI] [PubMed] [Google Scholar]
- 37. Jin K, Khonsari S, Gallagher R, et al. Telehealth interventions for the secondary prevention of coronary heart disease: A systematic review and meta-analysis. Eur J Cardiovasc Nurs 2019; 18: 260–271. [DOI] [PubMed] [Google Scholar]
- 38. Ericsson M, Ängerud KH, Brännström M, et al. Interaction between tele-nurses and callers with an evolving myocardial infarction: Consequences for level of directed care. Eur J Cardiovasc Nurs 2019; 18: 545–553. [DOI] [PubMed] [Google Scholar]
- 39. Bagot K, Moloczij N, Arthurson L, et al. Nurses’ role in implementing and sustaining acute telemedicine: A mixed-methods, pre-post design using an extended technology acceptance model. J Nurs Scholarsh 2020; 52: 34–46. [DOI] [PubMed] [Google Scholar]
- 40. Internet World Stats. Internet world stats, https://www.internetworldstats.com/top20.htm (2020, accessed 2 April 2020).