Abstract
Background
Sweden has one of the highest numbers of COVID-19 deaths per inhabitant globally. However, absolute death counts can be misleading. Estimating age- and sex-specific mortality rates is necessary in order to account for the underlying population structure. Furthermore, given the difficulty of assigning causes of death, excess all-cause mortality should be estimated to assess the overall burden of the pandemic.
Methods
By estimating weekly age- and sex-specific death rates during 2020 and during the preceding 5 years, our aim is to get more accurate estimates of the excess mortality attributed to COVID-19 in Sweden, and in the most affected region Stockholm.
Results
Eight weeks after Sweden’s first confirmed case, the death rates at all ages above 60 were higher than for previous years. Persons above age 80 were disproportionally more affected, and men suffered greater excess mortality than women in ages up to 75 years. At older ages, the excess mortality was similar for men and women, with up to 1.5 times higher death rates for Sweden and up to 3 times higher for Stockholm. Life expectancy at age 50 declined by <1 year for Sweden and 1.5 years for Stockholm compared to 2019.
Conclusions
The excess mortality has been high in older ages during the pandemic, but it remains to be answered if this is because of age itself being a prognostic factor or a proxy for comorbidity. Only monitoring deaths at a national level may hide the effect of the pandemic on the regional level.
Introduction
According to a recent report by WHO, Sweden is sharing the 12th place with the USA on the list of countries with most COVID-19 deaths per million inhabitants.1 However, absolute death counts can be misleading and age- and sex-specific death rates should be used when comparing countries in order to account for differences in underlying age structure of both cases and the total population. Even though the phrase ‘death rate from COVID-19’2 is often seen, most studies only present death counts without its relation to the underlying population at risk. Some studies have published estimates of age- and sex-specific rates,3 but not for Sweden, which has been hit hard by the pandemic.
Moreover, COVID-19 death counts are inherently uncertain and unappropriated to compare between countries because they depend on the testing strategy in the population, on the principles for assigning cause of death, on whether only hospitalized deaths are considered or all deaths, etc.4 Even when COVID-19 tests are in place and all deaths can be counted, the difficulty of attributing COVID-19 as a cause remains. Therefore, in Sweden, COVID-19 deaths are counted as all deaths occurring among individuals ‘with’ (and not from) confirmed COVID-19. A study from one region in Sweden that evaluated all death certificates of COVID-19 deaths found that around 15% of the deaths were directly attributed to COVID-19, 15% not attributed at all and the remaining 70% were partly attributed.5 Even if such distinctions of causes of deaths for old individuals with multiple chronic disease remain difficult, and the exact percentages should be interpreted with caution, it highlights the complexity of attributing deaths to COVID-19 and that comorbidities play an important role. It is therefore argued that excess mortality for all causes combined provides the most objective and comparable way of assessing the scale of the pandemic.6 With relative certainty, any excess mortality in 2020 can be assumed to be directly or indirectly attributed to the COVID-19 pandemic. Moreover, while COVID-19 has increased mortality, some deaths may have been saved due to the strategies of fighting the virus, e.g. improved hygiene, less traffic, etc.7 Therefore, the net effect of the pandemic may be a balance between these.
In Sweden, the governmental restrictions to fight the virus have mainly consisted of a recommendation to work from home and not to use public transport, to restrict meetings or events to 50 people, to digital teaching at high schools and universities, and to keep a distance of 2 m to other people. However, many restaurants, gyms and similar institutions closed temporarily. Thus, the Swedish ‘lockdown’ was less strict than in many other countries and the proportion of avoided deaths from other causes than COVID-19 may be smaller.
Age is another important issue to consider when comparing the burden of the pandemic between countries. Fatality from COVID-19 varies greatly over age, and the spread of the virus has affected age groups differently between countries. Therefore, age-specific death rates are a step toward a more comprehensive understanding of the pandemic’s impact on the mortality of the total population.4
Regional outbreaks add another layer to the assessment of excess mortality since the extent of the pandemic varies largely within countries. Nationwide estimates may thus hide excess mortality in the most affected regions.3 In Sweden, the region Stockholm was affected first and stood for the majority of all confirmed cases and deaths. With time, the virus has also affected other regions. However, in September 2020, 27% of the confirmed cases and 41% of COVID-19 deaths are still from the Stockholm region.
All-cause age- and sex-specific death rates provide valuable insights into how the pandemic affects specific ages and population subgroups, such as men and women. Already early during the COVID-19 outbreak in China, it was observed that more men than women died from the virus. This sex difference was seen both when estimated as a proportion of infected, and when counting the number of deaths. The same pattern has since then been observed in all countries affected by COVID-19.8 However, one must account for age differences before any conclusions can be drawn because populations have usually older women than men.
For these reasons, we make use of national Swedish register data about total weekly deaths and total population at risk to estimate weekly death rates for 2020, as well as rate ratios stratified by age and sex in comparison to the five previous years. We conduct these analyses for Sweden as a whole and for its most affected region—Stockholm. We focus on ages 50 and older because of the few deaths in ages below age 50 observed during the pandemic in Sweden. Through this, we aim to draw a more accurate picture of excess mortality attributable to the COVID-19 pandemic in Sweden. To quantify the overall health burden of the pandemic, we also assess remaining life expectancy at the age of 50, 65 and 80 for the first 33 calendar weeks of 2020.
Methods
Data
Our analysis rests on weekly death counts for all-cause mortality by 5-year age groups and sex from 2015 to the most recent weeks in 2020 for Sweden as a whole and for the region Stockholm. We used monthly population counts by single years of age to calculate the respective denominator. The data are provided by Statistics Sweden. Age is measured as ‘highest age attained’ during the respective year, and thus, death and population counts correspond to five consecutive birth cohorts. This data structure is a prerequisite to calculate death rates on a weekly basis. The single-year population counts have been aggregated to match the age grouping of the death counts.
By comparing the updated death counts across several weeks, we found a registration delay of around 3 weeks. After that time, the reported counts for the respective weeks change only marginally. Therefore, we focus our analysis on calendar weeks 1–33.
Disaggregating monthly population estimates
In order to calculate week-specific death rates, population counts were disaggregated from a monthly to a weekly basis by calculating a weighted average of the population at the beginning and the end of the respective month. The weights derive from the distance in days of the specific week start to the respective begin- or end-month population. End-week populations have been calculated accordingly. The corresponding person-years lived during the week are the average of the start-week and end-week population times the number of weekdays divided by the total number of days in the respective year.
Mortality measures
Several approaches for the calculation of baseline mortality or an expected number of deaths in absence of the pandemic are available (see for instance9). We opted for a simple approach to increase transparency and reproducibility of our findings. We defined our baseline as the average observed weekly death counts between 2015 and 19. Excess mortality is then estimated by subtracting the baseline from the weekly counts in 2020. A similar approach has for instance been used by Statistics Sweden, the Federal Statistical Office of Germany or the Our World in Data database.10–12
In a next step, we calculated age-specific death rates on a weekly basis and estimated rate ratios between the observed death rates in 2020 and the median of average age-specific death rates between 2015 and 19. The necessary statistical inference measures have been calculated using a bootstrap procedure assuming Poisson distributed death counts.10 This was done for total Sweden as well as for the Stockholm region.
We additionally calculated life expectancy separately for each year and for the weeks 1–33 of 2020 combined. We did this to summarize the current total effect of the pandemic on mortality across all ages. Life expectancy has been calculated using standard methods. Although the estimation of life expectancy based on small population numbers can be problematic, the total number of person-years under risk in our analysis is sufficient considering the recommended threshold of 5000 person-years.13
To gain more insights into how the life expectancy in 2020 compares to those of previous years, we additionally conducted a decomposition of the life expectancy difference by age and region. The decomposition allows us to break down the total differences into the contributions of changes in age-specific death rates and changes in composition of the home region of the deceased individuals. The estimation procedure rests on frequently used demographic decomposition techniques that are described elsewhere.14 For home regions, we distinguished between Stockholm and Sweden without Stockholm.
Results
Sweden reached 1000 officially confirmed COVID-19 cases during Week 11, 5000 confirmed cases during Week 14, 10 000 confirmed cases during Week 15 and more than 81 347 confirmed cases at the end of Week 33 (source: https://coronavirus.jhu.edu/map.html).
The difference in deaths between the first 33 weeks of 2020 and previous years for total Sweden, Stockholm and Sweden minus Stockholm can be seen in Supplementary Appendix figure S1. The figure reveals that death counts exceeded those of previous years both in Stockholm and the rest of Sweden for every week between 12 and 26. For both men and women, around 50% of the total number of excess deaths above age 50 comes from Stockholm county; a region with around 20% of the total Swedish population. The greatest excess of deaths has been observed during weeks 15 and 16.
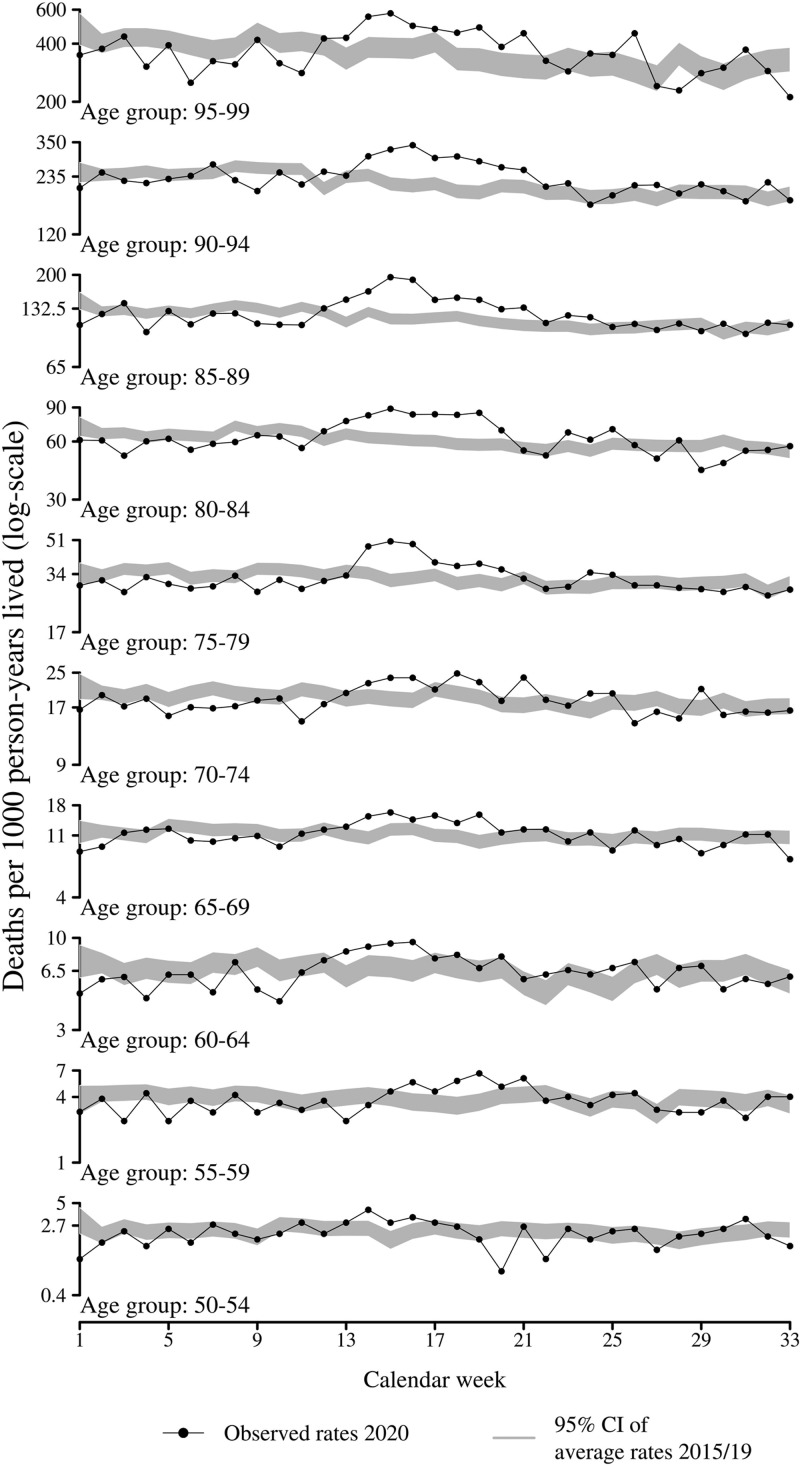
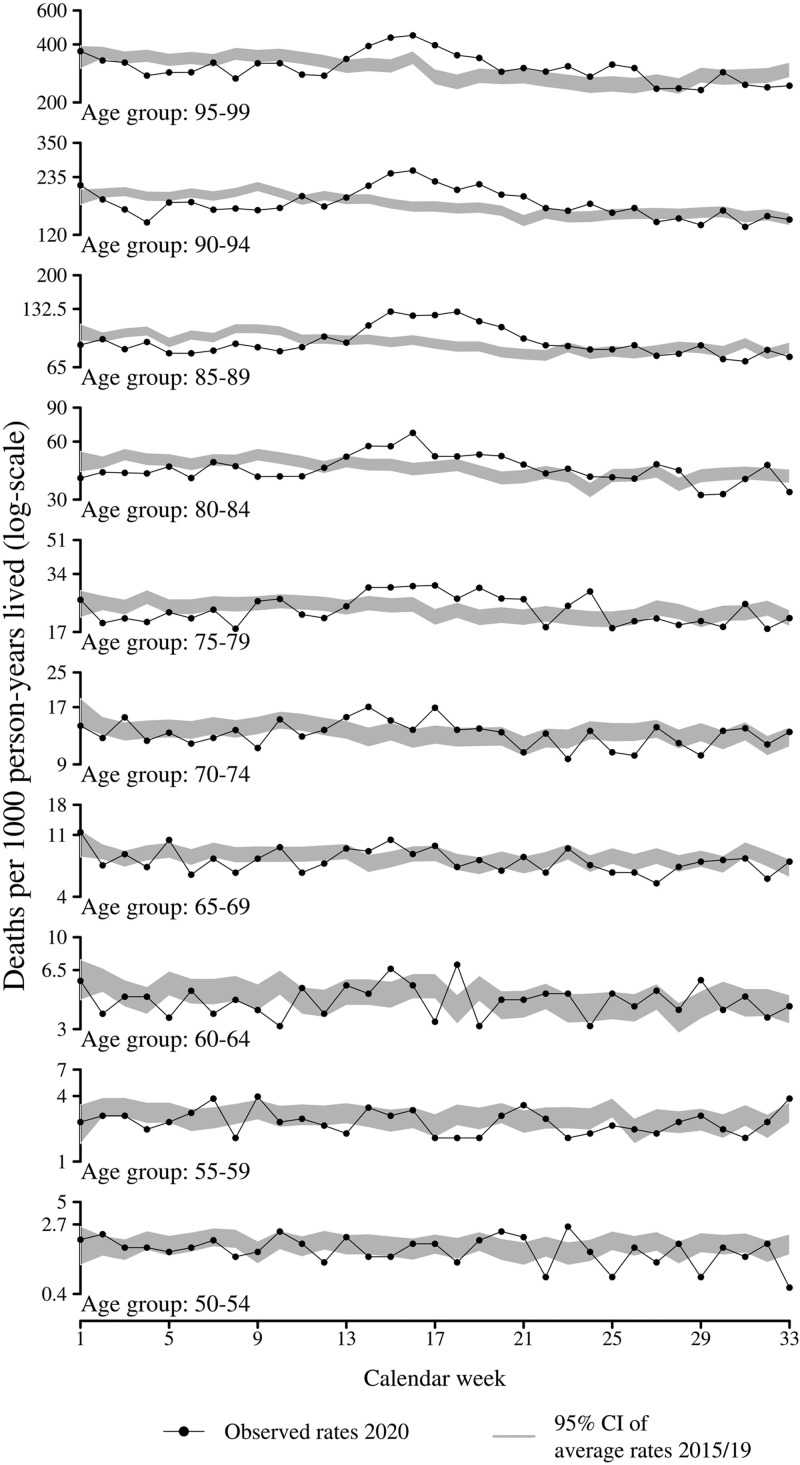
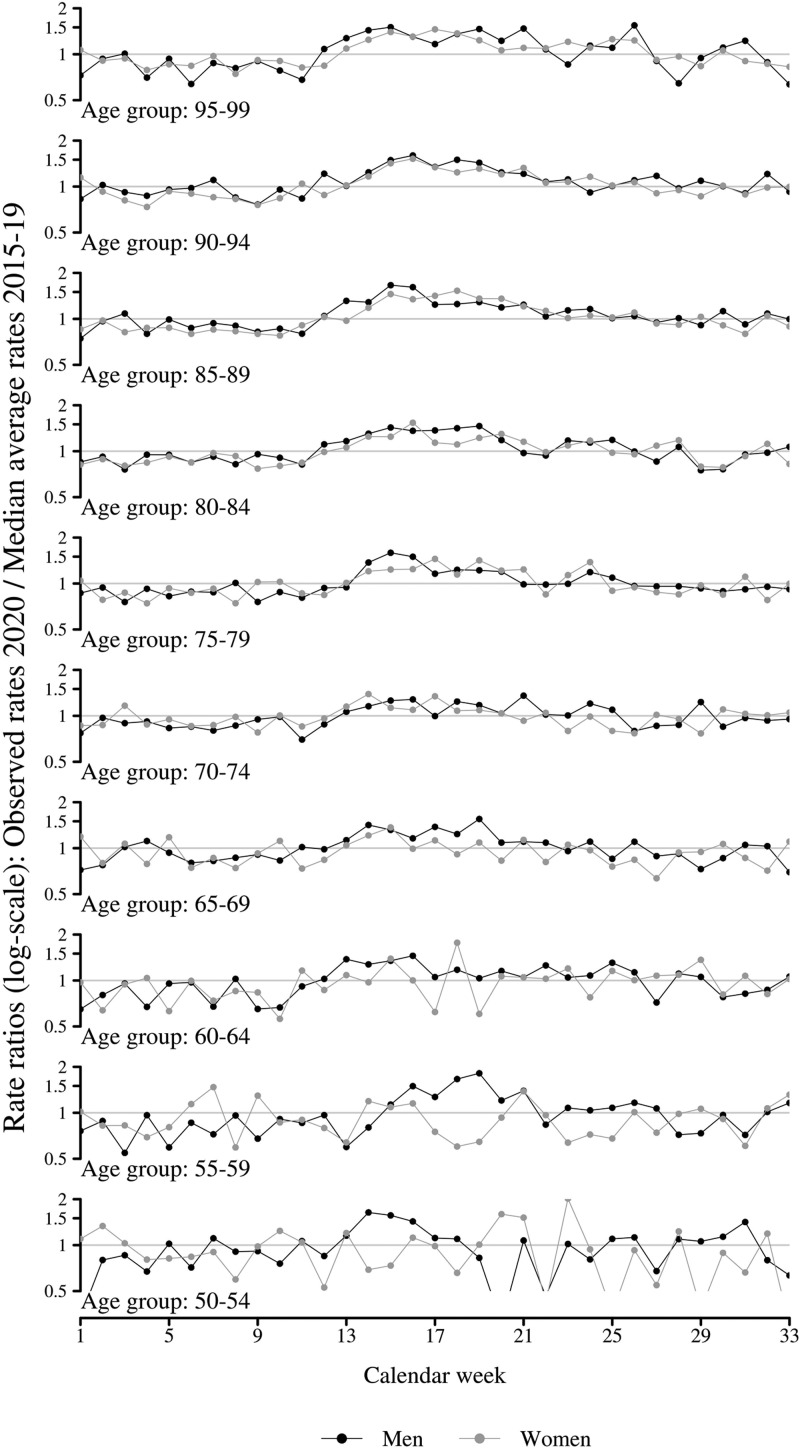
Figure 1 (men) and figure 2 (women) present age- and sex-specific weekly death rates in 2020 (points) compared to the 95% confidence interval of average death rates for the corresponding weeks from 2015 to 2019 (shaded area). Until week 12, mortality in 2020 was lower compared to the previous years for both men and women. However, from week 13 and onward, death rates in 2020 exceed the previous years. This pattern became more and more pronounced during the advancing pandemic and peaked during weeks 15–16. The highest age groups, i.e. ages 80 and above, were most strongly affected by the pandemic. For instance, in week 15, individuals at ages 85–99 were exposed to death rates 50–70% higher than the median of average death rates from 2015 to 2019 (see figure 3). Individuals between ages 60 and 79 were exposed to death rates around 25% higher than in previous years. The rate ratios in figure 3 also show that excess mortality is higher among men than women in ages up to 75 years. In ages above 75 years, men and women had about the same relative excess mortality with around 1.5 times higher rates compared to the average of previous years. In Supplementary Appendix figures S3–S5, corresponding results are found for Stockholm. These results show the same pattern as for total Sweden but with clearly higher excess mortality. For example, death rates among men in Stockholm were up to three times higher compared to previous years.
Figure 1.
Age- and sex-specific weekly death rates in 2020 compared to the 95% confidence interval of average death rates for the corresponding weeks in 2015–19, men, Sweden
Notes: The shaded parts are showing the 95% confidence intervals of average age-specific death rates for the period 2015–19. The interval has been calculated based on bootstrapping procedure.
Figure 2.
Age- and sex-specific weekly death rates in 2020 compared to the 95% confidence interval of average death rates for the corresponding weeks in 2015–19, women, Sweden
Notes: The shaded parts are showing the 95% confidence intervals of average age-specific death rates for the period 2015–19. The interval has been calculated based on bootstrapping procedure.
Figure 3.
Age- and sex-specific rate ratios comparing mortality in 2020 to the corresponding weeks in 2015–19, men and women, Sweden
Notes: The median of the average age-specific death rates for the period 2015–19 serves as reference. The median has been calculated based on a bootstrapping procedure.
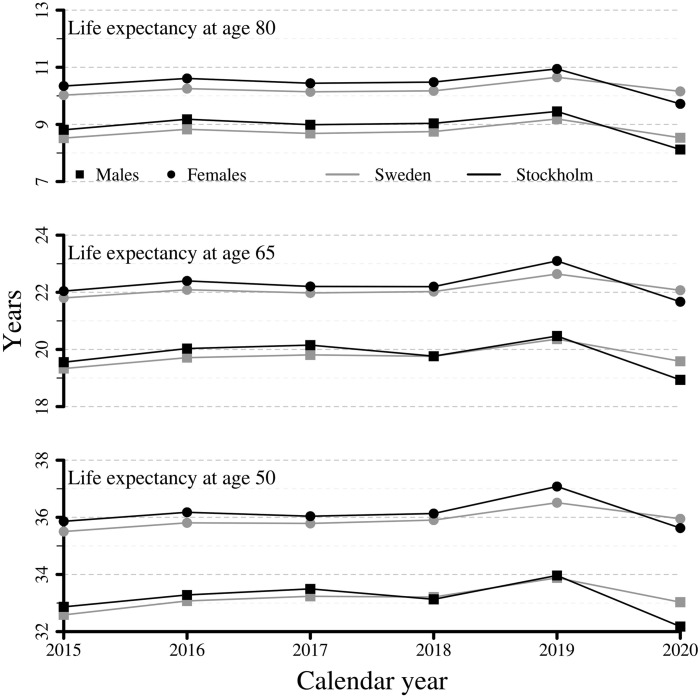
We also estimated the remaining life expectancy at age 50, 65 and 80 years for the years 2015–20, for total Sweden as well as for Stockholm, see figure 4. There was a positive trend in life expectancy over the years, with 2018 having the lowest and 2019 the highest life expectancy during 2015–19. However, the excess mortality in 2020 has caused a clear drop in life expectancy for 2020 compared to 2019 with about 1 year for Sweden and 1.5 for Stockholm. The drop in life expectancy is slightly larger for men than women at ages 50 and 65. It is important to note that the estimated life expectancy for 2020 is based on the 33 first weeks of the year. If mortality declined during the remainder of the year, the effect on life expectancy for the whole of 2020 will be reduced.
Figure 4.
Remaining life expectancy at age 50, 65 and 80 years for the years 2015–20 based on the age-specific death rates measured over the calendar weeks 1–33, men and women, Stockholm county and Sweden
Note that, we additionally conducted a decomposition of how Stockholm and the respective age groups contributed to the change in life expectancy (see Supplementary Appendix figure S2).
Discussion
The final consequences that the COVID-19 pandemic will have on mortality and life expectancy in Sweden and other countries cannot be known at this point in time. However, by analyzing weekly age- and sex-specific death rates for all-cause mortality during 2020 and previous years, we can get a perception of the mortality burden.
Our analysis shows that from week 13 (the last week of March) mortality in Sweden started to increase, peaked during weeks 15 and 16 and has since then slowly come down. It has been argued that the pandemic affected the frailest the most, and that many of them would have died regardless, just somewhat later. In such case, the effect on life expectancy would maybe not be substantial. However, so far (week 33), we do not see any compensation of mortality so that it has reached levels below previous years. The general pattern of excess mortality compared to previous years is clear and consistent. We also show that the excess mortality at the national level clearly differs from the effect of the pandemic on the most affected region, namely Stockholm, where the excess mortality is 2–3 times higher.
Excess mortality thus unfolded 13 weeks after Sweden’s first confirmed case of COVID-19 (31 January) and 2–3 weeks after community transmission was confirmed (9 March) in the Stockholm region. During week 11, Sweden surpassed the number of 1000 test confirmed COVID-19 cases and from week 13 and onwards, the death rates at all ages above 60 are higher than those in previous years.
Sweden has so far taken a somewhat different approach than most countries for the containment of the virus. The strategy is built on recommendations and emphasizes individuals’ own responsibility for social distancing, without enforcing a strict lockdown. It has been suggested that this strategy would indirectly result in herd immunity. However, together with Italy, Spain, France, the UK and Belgium, Sweden is among the European countries with highest reported excess mortality (source: https://euromomo.eu/), and the results from random serological testing presented 6 June showed a modest antibody prevalence of 7.3% for the Stockholm region. Moreover, a brief report about the situation in neighboring country Denmark concluded that measures against the pandemic offset more than COVID-19 deaths due to adverting deaths from other causes of death.7
Quantifying excess deaths and their impact on life expectancy at birth provides a picture of the COVID-19 burden on mortality.15 We found a reduction in life expectancy in 2020 of about 1 year for Sweden compared with 2019. However, one should consider that 2019 was an outlier with exceptionally high life expectancy, likely due to a very mild flu season. A comparison with 2018 instead showed a reduction in life expectancy by only 0.2 years for men and no decrease at all for women. This differs from findings from other countries. For example, Goldstein and Lee16 estimated the reduction in remaining life expectancy to be 3 years for the USA, and two other preprint articles from Italy and Spain estimated a similar impact on life expectancy for northern Italy and the most affected regions in Spain.17 However, the effect on life expectancy in 2020 will be very sensitive to the time period under study. Our measure is now taking in half of 2020. Ultimately, the full year of 2020 will serve as a better comparison between countries.
We show that persons above age 80 are disproportionally more affected by the pandemic. We cannot say whether this is an effect of age itself or if it mirrors the comorbidity burden correlated with these ages. A recent clinical study from Sweden did, however, confirm that comorbidity and frailty seemed to matter more than age per se.18
Our results also confirm the sex difference in COVID-19 death counts that has been reported since the outbreak of COVID-19. Although subject to fluctuations, the rate ratios of the age-specific death rates in 2020 compared to the previous years show approximately similar general age patterns for men and women. However, the magnitude of excess mortality is higher for men at ages up to 75 years. We cannot draw any conclusions about whether the mortality difference truly stem from different chances of surviving COVID-19, or a difference in the risk of getting affected, neither can we explain the mechanisms that lead to the observed sex differences. The number of confirmed cases from COVID-19 is higher for women than men (by 23 September, there was 50 960 confirmed cases among women and 38 796 among men), which together with the higher mortality, and number requiring intensive care for men clearly indicates higher fatality for men than women with COVID-19. The similar excess mortality in the oldest ages despite higher case fatality among men would then be explained by a larger number of COVID-19 cases among women. It should, however, be noted that it is confirmed cases and not all cases. Since COVID-19 testing is not random, more frequent testing among women could explain the higher numbers of confirmed cases. A recent preprint article reports similar susceptibility to COVID-19 for men and women but that men seem to be more prone to develop severe symptoms and die independent of age.8 The finding that the excess mortality follows the same age-pattern for men and women but with higher levels for men at all ages may suggest biological explanations to a higher fatality among men. Similar estimates of age- and sex-specific death rates for other countries would enable proper comparisons of the impact of COVID-19 on total mortality, as well as provide insights into the sex differences.
Confirmed COVID-19 deaths account for about 85–90% of the excess mortality observed in our analyses. The remaining 10–15% could represent COVID-19 deaths occurring among individuals without having tested positive for the virus. They could also represent an increase in other causes of deaths as an indirect consequence of the pandemic, e.g. due to restriction of health care resources, treatments and/or surgeries, or a changed behavior of seeking medical care for severe conditions. Most hospitals in the Stockholm region cut down on all non-acute surgery and treatment, but it is likely that even acute treatments and medical care in the geriatric sector have been affected. At the same time some of the COVID-19 deaths could be due to other causes than COVID-19. Future analyses with access to information about other causes of death will be informative in this respect.
To what extent the pandemic will lead to increasing total mortality for the entire year 2020 will depend on the progression of the pandemic, the extent to which some of the deaths attributed to COVID-19 would have occurred regardless of the pandemic, the consequences for other health conditions, as well as the health care sector at large. With consequences, we mean e.g. potentially raised mortality due to changes in the utilization of emergency care, prolonged waiting times, or raised psychiatric illness and suicide due to for instance social isolation. It has been hypothesized that the effect of the pandemic will not have a huge impact on life expectancy since many deaths in old age and risk groups would have occurred even in the absence of COVID-19, only somewhat later. However, a recent study suggests the opposite and concludes that the virus can be harmful for individuals at all levels of frailty and that it has cut lifespans by at least a decade on average.19 This article has, however, met critique for overestimating the burden of the pandemic by not accounting for multimorbidity in the patients who died from COVID-19.20 The death toll we found suggests at least that the number of deaths in near future must come down to very low levels to offset the tragic losses observed until recently.
Conclusion
Sweden, and especially the Stockholm region, has suffered from excess mortality at all ages from 60 years and older. From June and onwards mortality has reached the level of previous years. Persons above age 80 have been disproportionally affected, and in ages up to 75 years men suffer higher excess levels than women. What consequences the pandemic will eventually have on life expectancy will be determined by a complex interplay of several factors. We welcome similar estimates of age-, sex- and region-specific death rates for other countries to enable proper comparisons of the impact of COVID-19 on total mortality.
Supplementary data
Supplementary data are available at EURPUB online.
Availability of data and material
The data underlying the results in this manuscript build on official data provided by Statistic Sweden. Any researcher can turn to them and ask for similar data.
Code availability
The authors are open to share their codes upon request.
Conflicts of interest: None declared.
Key points
Estimating excess mortality avoids miscounting deaths from COVID-19-related deaths and/or other health conditions left untreated.
Age-, sex- and region-specific death rates allow us to understand the impact of the pandemic in different populations segments and thus informs public health policy and its actions.
Since beginning of March, there has been a clear and consistent excess mortality in all ages above 60 years in Swede, and men experience higher levels of excess mortality than women in ages up to 75 years.
Among the very oldest, the mortality increase with age has been disproportional if this is a factor of age itself or comorbidity remains to be explored.
Result on the national level clearly hides the burden for the most affected regions, in our case the Stockholm region.
Supplementary Material
References
- 1.WHO. Coronavirus Disease (COVID-19). Weekly Epidemiological Update. September 14, 2020. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/20200914-weekly-epi-update-5.pdf (14 September 2020, date last accessed).
- 2.Statista. Coronavirus (COVID-19) Death Rate in Countries with Confirmed Deaths and over 1000 Reported Cases as of September 16, by country. 2020. Available at: https://www.statista.com/statistics/1105914/coronavirus-death-rates-worldwide/ (16 September 2020, date last accessed).
- 3. Sinnathamby MA, Whitaker H, Coughlan L, et al. All-cause excess mortality observed by age group and regions in the first wave of the COVID-19 pandemic in England. Euro Surveill 2020;25:2001239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dudel C, Riffe T, Acosta E, et al. Monitoring trends and differences in COVID-19 case-fatality rates using decomposition methods: contributions of age structure and age-specific fatality. PLoS One 2020;15:e0238904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Region Östergötland. Dödsfall med Covid-19 på särskilda boenden eller i eget hem i Östergötland. Rapport efter journalgranskning. 2020. Available at: https://www.regionostergotland.se/contentassets/621708f279b94b0e84fc3e4e2f5a337e/dodsfall-med-covid-19-pa-sarskilda-boenden-eller-i-eget-hem-i-ostergotland.pdf (10 September 2020, date last accessed).
- 6. SVea LD. COVID-19: a need for real-time monitoring of weekly excess deaths. Lancet 2020;395:e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Vaupel JWJMABoucher M-PB, et al. Danish Covid19 Policies Reduced Overall Mortality. Rockwool fonden. 2020. Available at: https://www.rockwoolfonden.dk/kommentarer/danish-covid19-policies-reduced-overall-mortality/ (10 September 2020, date last accessed).
- 8. Peckham HNdGRaine C, et al. Sex-Bias in COVID-19: a Meta-Analysis and Review of Sex Differences in Disease and Immunity, 20 April 2020, PREPRINT (Version 2) available at Research Square. 2020. Available at: + 10.21203/rs.3.rs-23651. [DOI]
- 9.European Monitoring of Excess Mortality for Public Health Action (EuroMOMO). Work Package 7 Report. A European Algorithm for a Common Monitoring of Mortality across Europe. Copenhagen: EuroMOMO. Available at: https://www.euromomo.eu/uploads/pdf/wp7_report.pdf. (20 August 2020, date last accessed).
- 10. Max Roser HR, Ortiz-Ospina E, Hasell J, et al. 2020. “Coronavirus Pandemic (COVID-19)”. Published online at OurWorldInData.org. Available at: https://ourworldindata.org/coronavirus [Online Resource] (17 September 2020, date last accessed).
- 11. Zur Nieden F, Sommer B, Lüken S.. Sonderauswertung der Sterbefallzahlen. Wirtsch Stat 2020;72:38–50. [Google Scholar]
- 12.SCB. Available at: https://www.scb.se/en/About-us/news-and-press-releases/highest-mortality-this-millennium-noted-in-sweden/ [press release] 2020 (20 September 2020, date last accessed).
- 13. Eayres D, Williams ES.. Evaluation of methodologies for small area life expectancy estimation. J Epidemiol Community Health 2004;58:243–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Preston SH, Heuveline P, Guillot M.. Demography: Measuring and Modeling Population Processes. London: Wiley-Blackwell, 2001. [Google Scholar]
- 15. Aburto JM, Kashyap R, Scholey J, et al. Estimating the burden of COVID-19 on mortality, life expectancy and lifespan inequality in England and Wales: A population-level study. medRxiv 10.1101/2020.07.16.201550772. [DOI] [PMC free article] [PubMed]
- 16. Goldstein JR, Lee RD.. Demographic perspectives on the mortality of COVID-19 and other epidemics. Proc Natl Acad Sci USA 2020;117:22035–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Trias-Llimos S, Riffe T, Bilal U. Monitoring life expectancy levels during the COVID-19 pandemic: Example of the unequal impact of the first wave on Spanish regions. PLOS ONE 15(11): e0241952. https://doi.org/10.1371/journal.pone.0241952. [DOI] [PMC free article] [PubMed]
- 18. Hägg S, Jylhävä J, Wang Y, et al. Age, frailty and comorbidity as prognostic factors for short-term outcomes in patients with COVID-19 in geriatric care. J Am Med Dir Assoc 2020;21:1555–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hanlon P, Chadwick F, Shah A, et al. COVID-19? Exploring the implications of long-term condition type and extent of multimorbidity on years of life lost: a modelling study [version 1; peer review: awaiting peer review]. Wellcome Open Res 2020;5:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rubo M, Czuppon P.. Years of life lost estimates cannot always be taken at face value: response to “COVID-19 – exploring the implications of long-term condition type and extent of multimorbidity on years of life lost: a modelling study”. Wellcome Open Res 2020;5:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.