Abstract
Background
While individual countries have gained considerable knowledge and experience in coronavirus disease of 2019 (COVID-19) management, an international, comparative perspective is lacking, particularly regarding the measures taken by different countries to tackle the pandemic. This paper elicits the views of health system staff, tapping into their personal expertise on how the pandemic was initially handled.
Methods
From May to July 2020, we conducted a cross-sectional, online, purpose-designed survey comprising 70 items. Email lists of contacts provided by the International Society for Quality in Health Care, the Italian Network for Safety in Health Care and the Australian Institute of Health Innovation were used to access healthcare professionals and managers across the world. We snowballed the survey to individuals and groups connected to these organizations. Key outcome measures were attitudes and information about institutional approaches taken; media communication; how acute hospitals were re-organized; primary health organization; personal protective equipment; and staffing and training.
Results
A total of 1131 survey participants from 97 countries across the World Health Organization (WHO) regions responded to the survey. Responses were from all six WHO regions; 57.9% were female and the majority had 10 or more years of experience in healthcare; almost half (46.5%) were physicians; and all other major clinical professional groups participated. As the pandemic progressed, most countries established an emergency task force, developed communication channels to citizens, organized health services to cope and put in place appropriate measures (e.g. pathways for COVID-19 patients, and testing, screening and tracing procedures). Some countries did this better than others. We found several significant differences between the WHO regions in how they are tackling the pandemic. For instance, while overall most respondents (71.4%) believed that there was an effective plan prior to the outbreak, this was only the case for 31.9% of respondents from the Pan American Health Organization compared with 90.7% of respondents from the South-East Asia Region (SEARO). Issues with swab testing (e.g. delay in communicating the swab outcome) were less frequently reported by respondents from SEARO and the Western Pacific Region compared with other regions.
Conclusion
The world has progressed in its knowledge and sophistication in tackling the pandemic after early and often substantial obstacles were encountered. Most WHO regions have or are in the process of responding well, although some countries have not yet instituted widespread measures known to support mitigation, for example, effective swab testing and social control measures.
Keywords: COVID-19, pandemic management, international survey, health systems, WHO regions, management control
Introduction
Coronavirus disease of 2019 (COVID-19) is a respiratory infectious illness caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. COVID-19 was first reported in Wuhan, China, in December 2019 [2, 3] and has resulted in a global pandemic. As of 26 October 2020, there were 43 328 034 reported confirmed cases and 1 159 006 associated deaths [1].
The COVID-19 pandemic has challenged societies and health systems with issues such as ventilator shortages, unavailability of personal protective equipment (PPE), lack of oxygen supplies and extreme pressures on healthcare workers to manage infected patients [4]. As the pandemic continues to test healthcare systems, recommendations for management and infection control have proliferated. Common strategies to prevent nosocomial transmission include outlining a clear plan for providing essential services during the pandemic, with dedicated COVID-19 beds and units [5]; separation of healthcare facilities for the treatment of infected COVID-19 patients and non-COVID-19 patients and increasing intensive care bed capacity [6]. Internationally, there has been considerable interest in determining the effectiveness of infection prevention strategies and control measures. For instance, early in the pandemic in China, there was rapid implementation of isolation, quarantine, social distancing and community containment measures [2]. Analyses revealed that these multifaceted public health interventions were associated with temporary improved control of the outbreak [7], indicating that it is possible to contain the virus with the rapid implementation of management strategies.
While there have been similarities across countries in adopting known control strategies, the timeliness and effectiveness of national pandemic responses has led to different experiences for healthcare workers in different countries, with some systems being overwhelmed by high rates of COVID-19 morbidity and mortality [8, 9]. Selection and deployment of management strategies have been dependent on multiple factors including national resource levels, healthcare system and public health capabilities, and the timing of the first COVID-19 reports in each country [10–13]. With national resources being a key determinant of how a country can respond and manage the pandemic, we are witnessing disproportionate harm among vulnerable and economically disadvantaged societies [4, 14], with the burden of the pandemic falling heavily on the most disadvantaged groups worldwide [15].
There is considerable uncertainty surrounding this pandemic, given the likelihood of continued waves of disease in the absence of effective vaccines or treatments. An analysis of the experiences and opinions of key stakeholders related to the effectiveness of their country’s COVID-19 control strategies is timely to support further refinement of pandemic readiness planning. It is essential that we capture international experiences and perspectives of pandemic preparedness and management strategies beyond publicized plans [10]. The aim of this study was to survey staff to canvass their experiences of national responses to, and management of, the COVID-19 outbreak and examine differences in responses by World Health Organization (WHO) region. We sought the views of frontline healthcare professionals, quality and safety professionals and other major stakeholders.
Methods
The survey
A cross-sectional online survey was distributed between May and July 2020. Survey participants were listed email recipients of the International Society for Quality in Health Care (ISQua), the Italian Network for Safety in Health Care (INSH) and the Australian Institute of Health Innovation (AIHI). Snowballing techniques were applied whereby participants were asked to distribute the survey invitation to their colleagues working in healthcare organizations during the COVID-19 pandemic.
Sample
This purposive sample represented an ideal group of participants to provide insights from a range of countries. ISQua is an open society involving a wide range of domain experts, healthcare professionals, quality and safety professionals, policy-makers, managers, patients and associated personnel interested in quality and safety in healthcare. Approximately 17 000 invitees on ISQua’s circulation list were sent the email invitation. The INSH and AIHI circulated the survey to their distribution lists, and links to the questionnaire were tweeted widely.
Procedures
The survey took approximately 10 minutes to complete and included 70 items about country-specific experiences of the COVID-19 outbreak. The survey was designed to obtain information about participants’ (1) socio-demographic information, (2) professional information and (3) management of COVID-19 in the participants’ country of work. Participants were asked about their institutions’ approaches to COVID management and media communication, organization of acute hospitals, public health/primary health organization, PPE, staffing and training, and systems of intensive care available during the COVID-19 outbreak. Most questions were closed-ended with four response options (Yes, No, Don’t Know and Other). The response option ‘Other’ was followed by an open-text box for participants to expand on their answers. This qualitative data were analysed based on sentiment using inductive coding, considering differences in responses across states and WHO regions. The four response options (Yes, No, Don’t Know and Other) were recoded dichotomously (Yes/No) to examine differences between responses by region using chi-square analyses. The six WHO regions were used for comparisons: European region (EURO), Western Pacific region (WPRO), Eastern Mediterranean region (EMRO), Region of the Americas (Pan American Health Organization [PAHO]), South-East Asia region (SEARO) and African region (AFRO) (Figure 1). Cumulative cases and cumulative deaths per WHO region as of 4 October 2020 are displayed in Table 1 [1].
Figure 1.
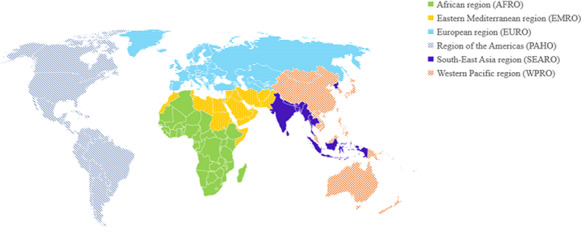
WHO regions.
Table 1.
Cumulative COVID-19 confirmed cases and deaths by WHO region, as of 4 October 2020
| WHO region | Cumulative cases (%) | Cumulative deaths (%) |
|---|---|---|
| AFRO | 1 198 550 (3%) | 26 264 (3%) |
| EMRO | 2 466 722 (7%) | 63 156 (6%) |
| EURO | 6 187 384 (18%) | 240 148 (23%) |
| PAHO | 16 990 036 (46%) | 568 358 (55%) |
| SEARO | 7 335 273 (21%) | 119 167 (12%) |
| WPRO | 625 642 (2%) | 13 632 (1%) |
Results
There were 1434 responses to the online survey. Responses were excluded if only demographic information was supplied (i.e. participants did not answer questions regarding the management of the COVID-19 outbreak). This yielded a final sample of 1131 responses for analysis.
Demographic results
Participants spanned 97 countries and all six WHO regions, with over one-third from EURO (see Figure 2). Specifically, most responses were from Italy (n = 257, 27.3%), followed by Australia (n = 90, 9.6%) and India (n = 54, 5.7%). One hundred and eighty-nine respondents did not indicate their state of origin. A complete list of participants by state is presented in Appendix 1. Demographic and work characteristics of participants are detailed in Table 2. Most participants (n = 948, 86.1%) were healthcare professionals, specifically medical practitioners (n = 440, 46.5%). Almost half (n = 490, 44.9%) of the sample held an official leadership role in their healthcare environment, such as hospital, department or ward management (n = 276, 59.3%).
Figure 2.
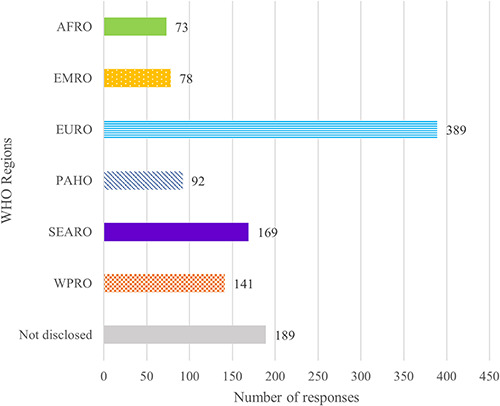
Number of responses by WHO region (N = 1131).
Table 2.
Demographic and work characteristics of respondents (N = 1131)
| N | % | ||
|---|---|---|---|
| Gender | Male | 457 | 41.7 |
| Female | 635 | 57.9 | |
| Non-binary | 5 | 0.5 | |
| Age range | 18–24 years | 2 | 0.2 |
| 25–34 years | 144 | 13.1 | |
| 35–44 years | 297 | 27.0 | |
| 45–54 years | 295 | 26.8 | |
| 55–64 years | 269 | 24.4 | |
| 65–74 years | 83 | 7.5 | |
| 75 + years | 12 | 1.1 | |
| Experience in current role | 1–5 years | 276 | 25.2 |
| 6–10 years | 178 | 16.2 | |
| 10+ years | 642 | 58.6 | |
| Healthcare professional role | Physician/Medical practitioner | 440 | 46.5 |
| Nurse | 149 | 15.8 | |
| Midwife | 6 | 0.6 | |
| Technician | 31 | 3.3 | |
| Researcher | 54 | 5.7 | |
| Allied health professional | 58 | 6.1 | |
| Student | 4 | 0.4 | |
| Other (e.g. radiologist, dentist, public health) | 204 | 21.6 | |
| Professional role (non-healthcare professional) | National or state government policy-maker | 10 | 6.6 |
| Employer | 3 | 2.0 | |
| Employee | 25 | 16.4 | |
| Administrator | 14 | 9.2 | |
| Manager | 31 | 20.4 | |
| Executive | 26 | 17.1 | |
| Other (e.g. consumer) | 43 | 28.3 |
Numbers do not always add to total number of respondents due to missing data.
Institutional approach and media communication
Overall, most respondents (n = 573, 71.4%) reported that in their state, the national Ministry of Health or equivalent lead public institution had an effective national plan for prevention and control of pandemics prior to the COVID-19 outbreak. Significant differences in responses based on WHO region were found (χ2 [5, N = 693] = 117.41, P < 0.001). Only 31.9% of respondents from PAHO indicated that there was an effective national plan compared with 90.7% from SEARO and 88.1% from WPRO (other regions: AFRO = 61.5%, EMRO = 89.9%, EURO = 62.2%). For some, plans were considered old, not adequately updated at the inception of this outbreak, or not fit for purpose for the current context. For example, one participant from Australia indicated: ‘Pandemic plan in place but ineffective for this outbreak’; and another from the UK stated: ‘There was a national plan but it was not effectively put into action.’
In total, 78.6% of participants (n = 566) reported that in their healthcare organization an emergency taskforce was immediately or soon activated when the first case was identified in their country. This was most commonly reported by respondents from SEARO (92.1%) and significantly differed by region, (χ2 (5, N = 618) = 22.82, P < 0.001; AFRO = 84.4%, EMRO = 88.1%, EURO = 72.5%, PAHO = 76.4%, WPRO = 79.3%). According to participants, taskforces comprised a wide array of stakeholders, most of which included some combination of emergency medicine doctors, clinical risk managers, epidemiologists, hospital managers, infection prevention and control staff, intensivists, medical practitioners, microbiologists, nursing managers and respiratory disease experts. Those personnel most frequently involved in the taskforce were hospital managers (n = 532, 47.0%), infection prevention and control experts (n = 529, 46.8%) and emergency medical doctors (n = 482, 42.6%).
According to the majority of participants (n = 664, 79.0%), there was an official spokesperson to manage external communication to citizens regarding the COVID-19 outbreak in healthcare provider organizations. Participants reported that the frequent channels of communication used to deliver key messages included social media (e.g. Twitter, Facebook) (n = 655, 57.9%) and the World Wide Web (n = 593, 52.4%). Overall, communication channels were perceived to be effective (n = 694, 91.4%), with clear and unambiguous messages (n = 658, 78.1%), and relevant information (n = 673, 78.0%). Examining differences by WHO region, we found that there was a statistically significant difference in perceptions: of effectiveness of communication channels, (χ2 (5, N = 660) = 13.31, P < 0.001; AFRO = 86.0%, EMRO = 93.5%, EURO = 89.7%, PAHO = 86.6%, SEARO = 95.9%, WPRO = 97.2%); that messages were clear and unambiguous, (χ2 (5, N = 726) = 69.63, P < 0.001; AFRO = 88.9%, EMRO = 95.5%, EURO = 66.1%, PAHO = 72.2%, SEARO = 94.5%, WPRO = 87.4%); and that information was relevant, (χ2 (5, N = 746) = 31.72, P < 0.001; AFRO = 77.0%, EMRO = 88.4%, EURO = 69.6%, PAHO = 73.5%, SEARO = 91.0%, WPRO = 82.1%). Consistently, participants from SEARO, WPRO and EMRO were more positive than those from AFRO, EURO and PAHO.
In some instances, timeliness and confusion were identified as key issues by participants. Participants noted that messages could not always provide the information warranted given the many uncertainties faced. The main messages provided to inform the public emphasized health risks (n = 729, 64.5%) and focused on the importance of an individual’s contribution to make a difference for the community (n = 772, 68.3%). Messages were less frequently used to emphasize penalties for misbehaviour (n = 237, 21.1%).
Organization of health services
The most commonly reported strategies to organize health services in the face of the infection were limiting who could visit hospitals, using progressive care organization in COVID-19 dedicated areas (i.e. intensive, subintensive, ordinary and subacute care) and designing new clinical pathways for COVID-free patients. Table 3 presents aspects of health service organization in response to the COVID-19 outbreak by the six WHO regions. Significant differences are presented in bold font.
Table 3.
Participant perspectives: health service organization during COVID-19 (n = 942)
| In the healthcare organization where I work… | % Participants responding yes to statement | Response by regions | |||||
|---|---|---|---|---|---|---|---|
| AFRO (n = 73) |
EMRO (n = 78) |
EURO (n = 389) |
PAHO (n = 92) |
SEARO (n = 169) |
WPRO (n = 141) |
||
| Infection control measures included limiting hospital visits by relatives of patients** | n = 678, 97.1% | 95.8% | 86.5% | 98.8% | 98.2% | 98.1% | 97.7% |
| A progressive care organization (intensive, sub intensive, ordinary and subacute care) was created in a COVID-19 hospital or dedicated COVID-19 areas. | n = 597, 90.2% | 78.6% | 86.8% | 91.6% | 90.7% | 93.1% | 85.7% |
| Clinical pathways for COVID-free patients were designed (e.g. surgery, time-dependent diseases, pregnant women). | n = 582, 89.1% | 88.1% | 83.3% | 91.5% | 89.8% | 91.4% | 91.9% |
| We isolated patients under investigation.* | n = 576, 88.9% | 93.5% | 85.5% | 85.5% | 95.6% | 96.0% | 92.0% |
| Elective activities were temporarily suspended (e.g. hospitalizations, surgery, outpatient visit).** | n = 646, 87.7% | 65.2% | 89.8% | 97.1% | 90.2% | 65.7% | 93.2% |
| There is a care pathway for a suspected COVID-19 patient from home or nursing home to hospital.* | n = 494, 77.9% | 67.4% | 79.2% | 75.7% | 72.1% | 83.7% | 92.1% |
| Anyone with symptoms can have a swab taken for testing at home or by attending a specific testing site.** | n = 485, 72.1% | 79.6% | 82.4% | 66.5% | 64.0% | 70.2% | 88.0% |
| We increased single room capacity in order to isolate COVID-19 patients.* | n = 469, 76.1% | 57.5% | 72.3% | 74.6% | 67.4% | 85.0% | 77.4% |
| COVID-19 patients were admitted to dedicated wards within the same hospital as COVID-free patients.** | n = 479, 70.8% | 65.9% | 43.1% | 82.0% | 70.1% | 63.0% | 66.7% |
| COVID-19 patients were admitted to a dedicated hospital or building.** | n = 449, 66.7% | 73.3% | 86.0% | 56.4% | 52.9% | 86.3% | 63.9% |
| A clinical database and/or a bank of biological samples was shared in the hospital network | n = 268, 65.0% | 48.6% | 63.2% | 66.2% | 65.6% | 75.8% | 68.4% |
| Primary care doctors take care of the COVID-19 patients discharged from hospital for monitoring their health status at their home.* | n = 352, 63.2% | 40.0% | 70.5% | 67.2% | 56.8% | 63.2% | 64.5% |
| Nursing homes were immediately isolated to avoid possible infections of residents/patients from an external source.** | n = 359, 60.3% | 38.7% | 68.6% | 51.9% | 43.2% | 84.8% | 78.8% |
| There is an outpatient clinic managed by general practitioners.** | n = 409, 57.5% | 72.5% | 70.6% | 52.0% | 70.2% | 74.5% | 75.3% |
| The bed capacity was extended by means of mobile structures.* | n = 287, 44.0% | 40.9% | 52.9% | 41.0% | 41.7% | 58.7% | 33.8% |
* P < 0.05; ** P < 0.001
Diagnostic tests
Participants were asked about COVID-19 testing issues in their geographic area. The most frequently reported problem was a delay in communicating the outcome of swab testing (n = 462, 40.8%). We found significant differences by region for all testing issues (see Figure 3).
Figure 3.
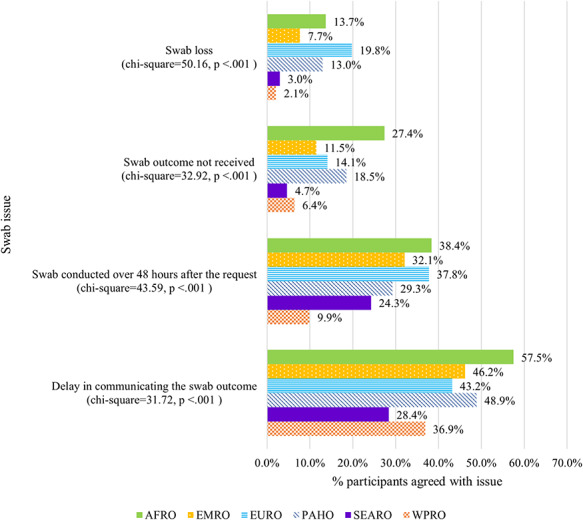
Reported issues with swab testing (n = 942).
Most participants reported that reverse transcription-polymerase chain reaction (RT-PCR) testing of swabs (oro-pharyngeal and/or naso-pharyngeal) (n = 642, 56.8%) was used for COVID-19 diagnosis and screening, rather than antibodies (Immunoglobulin M (IgM), Immunoglobulin G (IgG) blood). Most reported that screening of healthcare workers was a priority in their healthcare organization and associated geographical area (n = 476, 65.6%). However, this differed by region (χ2 (5, N = 626) = 31.72, P < 0.001) with only 55.4% of respondents from EURO reporting testing of health workers was a priority, compared with 82.3% from WPRO, 63.8% from AFRO, 70.7% from EMRO, 69.5% from PAHO and 76.9% from SEARO. Only 71 participants (6.3%) reported that no screening was being conducted in their healthcare organization.
PPE
At the time of survey response, the majority of participants indicated that in their local healthcare organization, healthcare workers were appropriately protected with masks, gowns and facial screens (n = 551, 82.2%). While most participants (n = 518, 74.3%) indicated that at least one healthcare worker at their organization had been infected with COVID-19, there were significant differences observed between regions, (χ2 (5, N = 591) = 116.14, P < 0.001; AFRO = 78.0%, EMRO = 71.2%, EURO = 91.3%, PAHO = 80.4%, SEARO = 46.0%, WPRO = 44.4%). Perceptions of appropriateness of PPE were significantly lower in AFRO, compared with other regions (Table 4). Further, just over half of participants (n = 405, 59.6%) reported that their friends and family had sufficient access to face masks as needed, with significant differences observed across regions, (χ2 (5, N = 582) = 47.72, P < 0.001; AFRO = 66.7%, EMRO = 64.7%, EURO = 46.5%, PAHO = 62.1%, SEARO = 84.9%, WPRO = 55.1%). Participants highlighted that this was more of an issue at the beginning of the outbreak: ‘Not sufficient access at the beginning’ (Italy); ‘There were some problems initially, but supplies are now adequate’ (Australia).
Table 4.
Participant perspectives: PPE and staffing during COVID-19 (n = 942)
| In the healthcare organization where I work… | % Participants responding yes to statement | Response by regions | |||||
|---|---|---|---|---|---|---|---|
| AFRO (n = 73) |
EMRO (n = 78) |
EURO (n = 389) |
PAHO (n = 92) |
SEARO (n = 169) |
WPRO (n = 141) |
||
| Clear guidelines have been given to healthcare professionals about how and when to wear protective equipment (i.e. masks, gowns, facial screens).** | n = 634, 89.4% | 82.0% | 91.2% | 84.3% | 93.1% | 98.1% | 96.6% |
| Health workers have been appropriately protected (e.g. masks, gowns, facial screens).** | n = 551, 82.2% | 68.1% | 88.9% | 74.9% | 83.9% | 95.2% | 91.7% |
| Self-isolation was mandatory for healthcare providers who had contacts, without PPE, with a COVID-19 case.** | n = 519, 81.6% | 87.2% | 96.2% | 70.5% | 75.5% | 94.7% | 95.0% |
| There is an emergency/pandemic plan.** | n = 510, 79.8% | 69.0% | 89.9% | 73.0% | 80.0% | 87.9% | 93.2% |
| There have been cases of healthcare personnel infected with SARS-CoV-2.** | n = 518, 74.3% | 78.0% | 71.2% | 91.3% | 80.4% | 46.0% | 44.4% |
| It was necessary to hire or acquire additional healthcare workers to deal with COVID-19.** | n = 422, 64.3% | 57.8% | 48.1% | 77.2% | 63.3% | 38.6% | 61.7% |
| Healthcare workers were provided with psychological support during the COVID-19 outbreak.** | n = 394, 62.3% | 44.4% | 50.0% | 60.0% | 65.3% | 73.9% | 81.5% |
| Recommendations to avoid burnout were given to healthcare staff.** | n = 354, 58.5% | 41.0% | 68.6% | 50.0% | 50.0% | 78.4% | 72.9% |
| The plan has been reviewed or updated in the last three years.** | n = 277, 54.9% | 47.5% | 53.1% | 39.7% | 54.8% | 77.3% | 73.4% |
| Health workers have not had any problems with the availability of PPE (e.g. masks, gowns, facial screens).** | n = 331, 49.7% | 29.4% | 59.2% | 41.7% | 47.4% | 76.0% | 50.0% |
| Healthcare workers have received training through simulation of an epidemic outbreak (in the last three years).** | n = 169, 28.9% | 41.9% | 41.7% | 11.6% | 27.0% | 63.7% | 20.3% |
** P < 0.001
Reaction time was an issue identified among participants. Specifically, when asked to evaluate the reaction time of their healthcare organizations to apply measures of infection prevention and control, a substantial proportion of participants rated their organization as slow or very slow (Figure 4), with significant differences between WHO regions (χ2 (10, N = 431) = 77.89, P < 0.001).
Figure 4.
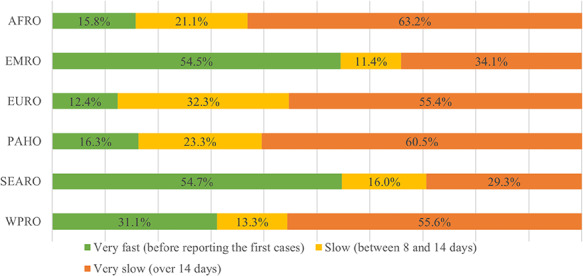
Perceptions of reaction time for infection prevention and control in healthcare organizations (n = 942).
Discussion
Statement of principal findings
Despite almost every country having some level of pandemic preparedness (e.g. a national plan; pre-existing public health capabilities), we found considerable variation reflected in the responses from participants about the way countries and regions dealt with preparedness and management at this stage in the pandemic. In general, respondents from SEARO, WPRO and EMRO were more positive in the reflection of their country’s management strategies of the pandemic compared with other regions.
Strengths and limitations
These study findings are limited to the perspectives and experiences of a selected group of domain experts and professionals. The survey did not investigate in detail healthcare workers’ experiences in aged care services and this would be of value in future surveys given the impact of COVID-19 on this vulnerable population. While this is an international study, we were unable to compare countries because of an over-representation of respondents from Italy, Australia and India, with a long tail of fewer responses from many other countries. Over-representation of countries may be a result of the survey distribution methods. Participants were email recipients of three organizations: one international society and two research groups in Italy and Australia. Another limitation of the study is that the sample size is not consistent across all analyses. This is due to missing responses (i.e. participants that did not answer every question), re-coding of data to only included responses of ‘Yes’ or ‘No’ for the chi-square analyses, and that some participants did not indicate where they work and were thus excluded from analyses comparing WHO regions.
Study findings are limited to the point in time and phase of the pandemic when data were collected (May to July 2020) and should be interpreted as a snapshot of a rapidly changing global pandemic. Further, as a result of the cross-sectional study design, it was not appropriate to statistically examine whether and how people and countries learnt from the experiences of others preceding them.
Interpretation within the context of the wider literature
While our survey results suggest that all regions have made progress in their preparedness and management of the COVID-19 outbreak, the response of some countries has clearly been more effective than others [16–18]. We found significant variation in the way different WHO regions managed the pandemic regarding infection control measures, health system organization, diagnostic testing, PPE and training and support for healthcare workers. It is well documented that there were early challenges facing all WHO member states ranging from short-term, resolvable problems [19] through to complete mishandling or misunderstanding of the consequences of the pandemic [11]. One example of progress is that while early on there were serious concerns reported about the availability of PPE [4, 19], we found that at the time of our survey, four in five frontline workers, professionals and healthcare managers reported that there was appropriate PPE in their healthcare organization. Further illustrating the positive reflections of international management of the COVID-19 outbreak, almost all respondents indicated that progressive care was implemented, hospital visits to patients were limited, and clear guidelines were given to healthcare professionals about the use of PPE.
Health systems have clearly learnt from the international experience of facing a pandemic which has left no one unaffected [1, 13]. The results suggest that leadership from WHO, with support from other peak bodies such as the Organization for Economic Co-operation and Development (OECD). and the ISQua, alongside much international discussion, exchange and scholarly and media attention, may have been helpful in gaining greater consistency in responses across regions.
Implications for policy, practice and research
Notwithstanding some positive reflections, the study identifies prominent issues that have implications for policy, practice and research. First, approximately one-third of respondents reported that healthcare workers did not receive recommendations to avoid burnout, despite overburdened healthcare workers being a key challenge throughout this pandemic [4, 14, 20]. Second, less than one-third of respondents indicated that healthcare workers received simulation training of an epidemic outbreak, and while most respondents had an active pandemic plan in their healthcare organization prior to the outbreak, almost half indicated that the plan had not been updated in the last 3 years. This highlights the importance of anticipating risk rather than reactive responses to global outbreaks [21]. We need well-documented infection control plans, rehearsed and prepared for application to any pandemic, with suitable levels of flexibility. Indeed, guidelines have already begun to emerge, which can help in the development of such plans (e.g. the role of human factors and ergonomics to inform pandemic response and preparedness [22, 23]).
Box 1. Recommendations to prepare for future waves and pandemics
Have revised, flexible pandemic response plans in place
Pick a task force that is familiar with having worked together
Streamline guidelines by which to manage the pandemic
Look after healthcare workers’ mental and physical well-being
Have regular pandemic simulations
Use human factors to design guidelines for pandemic response
Learn from the success of the first wave to spread good practice
Conclusion
No one should underestimate how far countries and regions have come in tackling the COVID-19 pandemic. Yet equally, no one should be under any misapprehensions that this is a wicked disease, which will continue to challenge our health systems. In this paper, we report a variation in initial pandemic responses across WHO regions, although there is room for improvement as some measures known to support mitigation, for example, effective swab testing and social control measures, are yet to be implemented widely.
Acknowledgements
We gratefully acknowledge the contributions of Gianni Biancofiore, Elisa Rom-ano, Maria Pia Ruggeri, Giulio Toccafondi and Giorgio Tulli for their input into the development of the survey. We also gratefully acknowledge Kelly Ngu-yen, Jackie Mullins and Kate Gibbons for administrative and logistical support.
Appendix 1. Participants per state (N = 1131)
| Frequency | Valid Per cent | |
|---|---|---|
| Afghanistan | 2 | 0.2 |
| Algeria | 2 | 0.2 |
| Antigua and Barbuda | 1 | 0.1 |
| Argentina | 5 | 0.5 |
| Australia | 90 | 9.6 |
| Austria | 2 | 0.2 |
| Bahrain | 1 | 0.1 |
| Bangladesh | 1 | 0.1 |
| Belgium | 8 | 0.8 |
| Bosnia and Herzegovina | 2 | 0.2 |
| Botswana | 1 | 0.1 |
| Brazil | 20 | 2.1 |
| Bulgaria | 1 | 0.1 |
| Burundi | 2 | 0.2 |
| Cambodia | 3 | 0.3 |
| Canada | 14 | 1.5 |
| Chile | 2 | 0.2 |
| China | 3 | 0.3 |
| Colombia | 6 | 0.6 |
| Cyprus | 1 | 0.1 |
| Denmark | 5 | 0.5 |
| Ecuador | 3 | 0.3 |
| Egypt | 5 | 0.5 |
| Estonia | 1 | 0.1 |
| Ethiopia | 7 | 0.7 |
| France | 2 | 0.2 |
| Gambia | 1 | 0.1 |
| Germany | 6 | 0.6 |
| Ghana | 4 | 0.4 |
| Greece | 1 | 0.1 |
| Hong Kong (S.A.R.) | 9 | 1.0 |
| India | 54 | 5.7 |
| Indonesia | 11 | 1.2 |
| Iran, Islamic Republic of Iran | 5 | 0.5 |
| Ireland | 29 | 3.1 |
| Israel | 2 | 0.2 |
| Italy | 257 | 27.3 |
| Japan | 6 | 0.6 |
| Jordan | 10 | 1.1 |
| Kenya | 1 | 0.1 |
| Kuwait | 2 | 0.2 |
| Latvia | 1 | 0.1 |
| Lebanon | 1 | 0.1 |
| Liberia | 1 | 0.1 |
| Malawi | 1 | 0.1 |
| Malaysia | 17 | 1.8 |
| Malta | 1 | 0.1 |
| Mexico | 5 | 0.5 |
| Morocco | 1 | 0.1 |
| Mozambique | 1 | 0.1 |
| Myanmar | 1 | 0.1 |
| Namibia | 3 | 0.3 |
| Nepal | 3 | 0.3 |
| Netherlands | 10 | 1.1 |
| New Zealand | 18 | 1.9 |
| Nigeria | 26 | 2.8 |
| Norway | 5 | 0.5 |
| Oman | 1 | 0.1 |
| Pakistan | 6 | 0.6 |
| Peru | 3 | 0.3 |
| Philippines | 3 | 0.3 |
| Poland | 2 | 0.2 |
| Portugal | 2 | 0.2 |
| Qatar | 4 | 0.4 |
| Republic of Korea | 7 | 0.7 |
| Romania | 2 | 0.2 |
| Russian Federation | 3 | 0.3 |
| Rwanda | 2 | 0.2 |
| Saint Kitts and Nevis | 1 | 0.1 |
| São Tomé and Príncipe | 1 | 0.1 |
| Saudi Arabia | 15 | 1.6 |
| Sierra Leone | 1 | 0.1 |
| Singapore | 4 | 0.4 |
| Slovenia | 1 | 0.1 |
| Somalia | 1 | 0.1 |
| South Africa | 16 | 1.7 |
| South Korea | 17 | 1.8 |
| Spain | 5 | 0.5 |
| Sri Lanka | 2 | 0.2 |
| Sudan | 1 | 0.1 |
| Sweden | 5 | 0.5 |
| Switzerland | 4 | 0.4 |
| Taiwan | 38 | 4.0 |
| Thailand | 2 | 0.2 |
| Tonga | 2 | 0.2 |
| Trinidad and Tobago | 3 | 0.3 |
| Tunisia | 32 | 3.4 |
| Turkey | 5 | 0.5 |
| Uganda | 2 | 0.2 |
| Ukraine | 1 | 0.1 |
| United Arab Emirates | 5 | 0.5 |
| UK and Northern Ireland | 28 | 3.0 |
| United Republic of Tanzania | 1 | 0.1 |
| USA | 28 | 3.0 |
| Uruguay | 1 | 0.1 |
| Vietnam | 1 | 0.1 |
| Yemen | 1 | 0.1 |
| No state selected | 189 | 16.7 |
Contributor Information
Riccardo Tartaglia, Italian Network for Safety in Health Care, Florence, Via de Renai, 23, 50125, Italy.
Micaela La Regina, Italian Network for Safety in Health Care, Florence, Via de Renai, 23, 50125, Italy.
Michela Tanzini, Italian Network for Safety in Health Care, Florence, Via de Renai, 23, 50125, Italy.
Chiara Pomare, Centre for Healthcare Resilience and Implementation Science, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia.
Rachel Urwin, Centre for Health Systems and Safety Research, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia.
Louise A Ellis, Centre for Healthcare Resilience and Implementation Science, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia; NHMRC Partnership Centre in Health System Sustainability, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia.
Vittorio Fineschi, University La Sapienza, Rome, Piazzale Aldo Moro, 5, 00185 Roma RM, Italy.
Francesco Venneri, Centre Gestione Rischio Clinico, Via Pietro Dazzi, 1, 50141 Firenze FI, Italy.
Chiara Seghieri, Sant’Anna Pisa School of Advanced Studies, Piazza Martiri della Libertá, 33, 56127 Pisa PI, Italy.
Peter Lachman, International Society for Quality in Health Care, Huguenot House, 4th Floor, 35-38 St Stephen’s Green, Dublin D02 NY63, Ireland.
Johanna Westbrook, Centre for Health Systems and Safety Research, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia.
Jeffrey Braithwaite, Centre for Healthcare Resilience and Implementation Science, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia; NHMRC Partnership Centre in Health System Sustainability, Australian Institute of Health Innovation, Macquarie University, Level 6, 75 Talavera Road, NSW, Sydney 2109, Australia; International Society for Quality in Health Care, Huguenot House, 4th Floor, 35-38 St Stephen’s Green, Dublin D02 NY63, Ireland.
Funding
The work was supported by the organizations involved. J.B. and J.W. report holding research grants from the National Health and Medical Research Council (APP9100002, APP1134459 and APP1135048) and the Medical Research Future Fund (APP1178554).
Conflict of Interest
The authors declare that they have no competing interests.
Ethics
Ethical approval was granted by the Macquarie University Human Research Ethics Committee (no: 52020669415528).
Contributorship
RT, ML, MT, PL, JW and JB conceptualized the project. RT, MR, MT, CP, RU, LAE, VF, FV, CS, PL, JH and JB contributed to the design of the survey. CP, JB, JW, RU and LAE drafted the manuscript. CP analysed the data with the support of CS and LE All authors contributed to the final version of the manuscript.
Data availability
The data are available from the corresponding author upon reasonable request.
References
- 1. World Health Organization WHO coronavirus disease (COVID-19) dashboard. Geneva: WHO, 2020. https://covid19.who.int/ (6 October, date last accessed).
- 2. World Health Organization Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19). Geneva: WHO, 2020. https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-report.pdf (31 August, date last accessed). [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mario T. No more normal. Lancet 2020;396:71. [Google Scholar]
- 5. Brindle ME, Gawande A. Managing COVID-19 in surgical systems. Ann Surg 2020;272:pe1-e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Phua J, Weng L, Ling L et al. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med 2020;8:506–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pan A, Liu L, Wang C et al. Association of public health interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA 2020;323:1915–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Remuzzi A, Remuzzi G. COVID-19 and Italy: what next? Lancet 2020;395:1225–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Alderwick H, Dunn P, Dixon J. England’s health policy response to COVID-19. BMJ 2020;369:m1937. [DOI] [PubMed] [Google Scholar]
- 10. Fisher D, Teo YY, Nabarro D. Assessing national performance in response to COVID-19 [Epub ahead of print]. Lancet 2020;doi: 10.1016/S0140-6736(20)31601-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Habib H. Has Sweden’s controversial COVID-19 strategy been successful? BMJ 2020;369:m2376. [DOI] [PubMed] [Google Scholar]
- 12. Haffajee RL, Mello MM. Thinking globally, acting locally—the US response to COVID-19. N Engl J Med 2020;382:e75. [DOI] [PubMed] [Google Scholar]
- 13. World Health Organization 2019 novel coronavirus (2019-nCoV): strategic preparedness and response plan. Geneva: WHO, 2020. https://www.who.int/docs/default-source/coronaviruse/srp-04022020.pdf?ua=1 (31 August, date last accessed). [Google Scholar]
- 14. DeForest A. The new stability. [published online ahead of print]. N Engl J Med 2020;doi: 10.1056/NEJMp2016293 [DOI] [Google Scholar]
- 15. Rutter H, Horton R, Marteau TM. The Lancet–Chatham House Commission on improving population health post COVID-19. Lancet 2020;396:152–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Boccia S, Ricciardi W, Ioannidis JP. What other countries can learn from Italy during the COVID-19 pandemic. JAMA Intern Med 2020;180:927–28. [DOI] [PubMed] [Google Scholar]
- 17. Loder E. Getting it right in the pandemic. BMJ 2020;370:m2637. [Google Scholar]
- 18. Braithwaite J, Tran Y, Ellis L et al. The 40 health systems, COVID-19 (40HS, C-19) study. Int J Qual Health Care 2020;doi: 10.1093/intqhc/mzaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tabah A, Ramanan M, Laupland KB et al. Personal protective equipment and intensive care unit healthcare worker safety in the COVID-19 era (PPE-SAFE): an international survey. J Crit Care 2020;59:70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wu AW, Buckle P, Haut ER et al. Supporting the emotional well-being of health care workers during the COVID-19 pandemic. J Patient Saf Risk Manag 2020;25:93–96. [Google Scholar]
- 21. Hollnagel E. RAG – the resilience analysis grid Hollnagel E, Pariès J, Woods JJ, Wreathall J eds.. Resilience Engineering in Practice: A Guidebook. Farnham, UK: Ashgate, 2011, 275–96. [Google Scholar]
- 22. Gurses AP, Tschudy MM, McGrath-Morrow S et al. Overcoming COVID-19: what can human factors and ergonomics offer?. J Patient Saf Risk Manag 2020;25:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Staines A, Amalberti R, Berwick DM et al. COVID-19: patient safety and quality improvement skills to deploy during the surge. Int J Qual Health Care 2020;doi: 10.1093/intqhc/mzaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data are available from the corresponding author upon reasonable request.


