The ongoing COVID-19 pandemic is a global crisis of unprecedented scale in modern times. As we approach the second half of 2020, the SARS-CoV-2 virus has already infected over 4.5 million worldwide with more than 300,000 deaths.1 The collective focus on combating this pathogen has led to an exponential increase in knowledge on COVID-19. Nonetheless, effective antiviral therapy and a vaccine remain elusive. What is established and repeatedly emphasised include the importance of hand hygiene and physical distancing measures to minimise disease transmission.
The overarching need to reduce disease transmission has had an enormous impact on sports and exercise. From an individual perspective, geographical restrictions on outdoor exercise and the need to stay home have led to reduced physical activity and increased sedentary behaviour. Within the sporting community, all forms of organised sport have been either cancelled or postponed. These range from mass participation events such as marathon races, to financially lucrative football leagues, and even the pinnacle of sporting excellence, the Summer Olympic Games. As the pandemic runs its course, uncertainties persist regarding exercise safety, resumption of sporting activity and how to manage infected athletes.
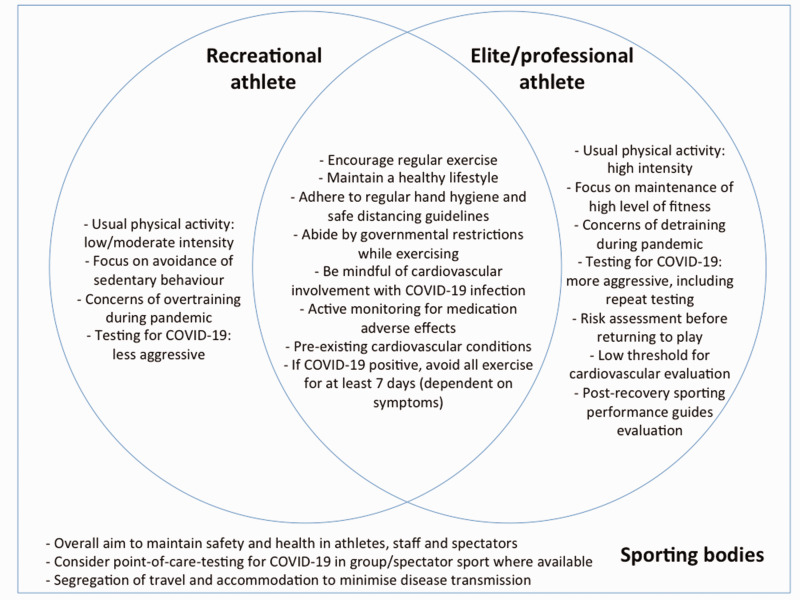
In this issue of the European Journal of Preventive Cardiology, Bhatia and colleagues2 utilise a ‘question and answer’ format to: (a) highlight the impact of COVID-19 on the heart, (b) stress the importance of regular physical activity and (c) provide guidance outlining the management of athletes and competitive sport during and beyond this pandemic (Figure 1).
Figure 1.
Considerations for sport and exercise amidst the COVID-19 pandemic.
While primarily a respiratory illness, COVID-19 may manifest multiple cardiovascular sequelae as highlighted by the authors in part one of the document. These sequelae range from troponin elevation to myocarditis, coagulopathy and cardiogenic shock.3 In addition, off-label medication use may predispose to malignant arrhythmias. The authors also raise the possibility of adverse outcomes in those with underlying channelopathies such as long QT syndrome. These are pertinent considerations for those caring for athletes with COVID-19.
Emerging data suggests cardiovascular involvement during acute COVID-19 infection is not unusual, with myocardial injury – defined as cardiac troponin (cTn) level above the 99th percentile of the upper reference limit – present in more than 15% of hospitalised patients with COVID-19.4 Independent predictors of myocardial injury include advanced age, presence of comorbidities and elevated inflammatory markers. The degree of cTn elevation appears to predict in-hospital mortality, reinforcing the importance of this biomarker in risk stratification.4
In part two of the article, the authors reiterate the importance of personal hygiene, social distancing and maintaining a healthy lifestyle to reduce the risk of COVID-19 infection. Physical activity is encouraged – while adhering to pandemic restrictions – due to its irrefutable physical and mental benefits. Nonetheless, caution is advised for those planning prolonged endurance activity such as marathon running, in order to avoid the risks of overtraining. These include a theoretical reduction in immunity following high intensity activity by untrained individuals.
This is a crucial opportunity to underscore not only the vital importance of regular exercise, but also the staggering consequences of inactivity. The global prevalence of physical inactivity exceeds 30%, with its deleterious effects on physical and mental health causing over three million deaths annually even prior to COVID-19.5 Amidst the current pandemic, the closure of communal sporting facilities such as swimming pools and gymnasiums has severely depleted options for exercise, leading to a surge in sedentary behaviour. Instead of merely encouraging exercise, individuals should be exhorted to avoid inactivity whenever possible.
In the final section, the authors elaborate on the impact of COVID-19 on elite athletes. Testing of athletes for COVID-19 is deemed appropriate in those with symptoms or confirmed exposure to disease, with resource availability guiding decisions on universal testing. Repeat testing in athletes with persistent symptoms is also recommended, given the possibility of false negative results.
It is sensible to retest symptomatic athletes with negative tests. With many countries ramping up COVID-19 testing, the number of false negative tests will correspondingly increase. Even when the diagnostic sensitivity of a test kit approaches 99%, universal testing in a population of one million reveals at least 10,000 individuals incorrectly identified as disease-free, substantially jeopardising public health and safety.
The authors then provide recommendations on physical training after an acute infection. Athletes with positive tests are recommended to refrain from exercise for at least 7 days. Following resolution of symptoms for 7 days, progressive return to training over an additional 7 days is advised. Measurement of cTn in athletes with cardiovascular symptoms is suggested to evaluate for possible myocardial injury and myocarditis. Should myocarditis be confirmed following diagnostic evaluation, existing guidelines can be used to guide management.
Before COVID-19, even after outbreaks of Severe Acute Respiratory Syndrome (SARS) in 2002, H1N1 influenza in 2009 and Middle Eastern Respiratory Syndrome in 2012, athletes with respiratory tract infections could resume low intensity training after being symptom-free for 2–3 days.6 In comparison, the proposed durations of rest and subsequent resumption of training after COVID-19 infection are substantially longer than before. This is consistent with reported estimates of 2 weeks from disease onset to medical recovery.1 Given the predilection for cardiovascular involvement in COVID-19, utilisation of cTn is prudent to facilitate early detection and treatment of potential adverse cardiac conditions.
In preparation for the eventual resumption of competitive sport, the authors propose a framework for evaluating athletes for return to play. Athletes are categorised into three tiers of risk based on: 1) duration of illness >7 days, 2) persistent cardiac or incapacitating symptoms, 3) any hospitalisation with COVID-19, and 4) inability to perform at pre-illness levels after appropriate retraining. Asymptomatic athletes with no abnormal clinical signs are considered lowest risk and return to play is allowed without additional testing. Conversely, athletes fulfilling any of points 2 to 4 above are regarded as highest risk and require full cardiovascular evaluation comprising electrocardiogram (ECG), echocardiogram, cTn and cardiac magnetic resonance imaging with or without additional stress testing and ambulatory ECG monitoring. Athletes with prolonged illness beyond 7 days or symptoms suggestive of myocarditis are screened with ECG and echocardiogram, followed by maximal exercise stress testing.
To date, other return to play algorithms have been published.7,8 Common to all approaches – including Bhatia and colleagues’ – is the use of symptoms and COVID-19 hospitalisation to risk stratify athletes and guide further evaluation. Unique to the authors’ strategy is the incorporation of symptom duration and sporting performance as part of risk assessment, showing cognisance of possible long-term adverse outcomes in athletes after COVID-19 infection. Given the relatively high prevalence of cardiovascular involvement in those with COVID-19, subclinical myocardial dysfunction may account for reduced exercise capacity in those who have recovered from COVID-19 but are unable to return to their previous level of fitness despite retraining. Exercise capacity in SARS survivors was markedly reduced at 1 year compared with population norms.9 As COVID-19 and SARS are both coronavirus infections, a comparable pattern in COVID-19 patients may be anticipated. Apart from disease-specific consequences, healthcare providers should also actively monitor athletes receiving pharmacotherapy due to potential medication-related adverse effects.10 Examples include: direct myocardial toxicity with hydroxychloroquine and increased risk of bleeding from anticoagulation therapy, especially in athletes from contact sports.
Several considerations for planning future sporting events are put forth by the authors. Many of these require close cooperation with governmental organisations – for instance, screening of staff and spectators for COVID-19, and segregation of travel and accommodation. The UK government has recently released guidance documents for the phased return to sport and recreation, which elaborates on these aspects in greater detail.11
While the sporting community prepares for a gradual return to normalcy, expert guidance provides much-needed reassurance and direction for all involved in recreational and competitive sport.12 As knowledge on COVID-19 continues to evolve, collaboration between international sporting bodies will be vital to facilitate global consensus on best practices and recommendations for sports and exercise.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. World Health Organization. Coronavirus disease (COVID-19) pandemic, https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (2020, accessed 17 May 2020).
- 2.Bhatia RT, Marwaha S, Malhotra A, et al. Exercise in the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) era: A Question and Answer session with the experts Endorsed by the section of Sports Cardiology & Exercise of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol 2020. 27: 1242–1251. [DOI] [PMC free article] [PubMed]
- 3. Guzik TJ, Mohiddin SA, Dimarco A, et al. COVID-19 and the cardiovascular system: Implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. Epub ahead of print 30 April 2020. DOI: 10.1093/cvr/cvaa106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. Epub ahead of print 11 May 2020. DOI: 10.1093/eurheartj/ehaa408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. Physical inactivity: A global public health problem, https://www.who.int/dietphysicalactivity/factsheet_inactivity/en/ (2020, accessed 13 May 2020).
- 6. Scharhag J, Meyer T Return to play after acute infectious disease in football players. J Sports Sci 2014; 32: 1237–1242. [DOI] [PubMed] [Google Scholar]
- 7. Phelan D, Kim JH, Chung EH A game plan for the resumption of sport and exercise after coronavirus disease 2019 (COVID-19) Infection. JAMA Cardiol. Epub ahead of print 13 May 2020. DOI: 10.1001/jamacardio.2020.2136 [DOI] [PubMed]
- 8. Baggish AL, Drezner JA, Kim JH, et al. The resurgence of sport in the wake of COVID-19: Cardiac considerations in competitive athletes, https://blogs.bmj.com/bjsm/2020/04/24/the-resurgence-of-sport-in-the-wake-of-covid-19-cardiac-considerations-in-competitive-athletes/ (2020, accessed 14 May 2020). [DOI] [PMC free article] [PubMed]
- 9. Hui DS, Wong KT, Ko FW, et al. The 1-year impact of severe acute respiratory syndrome on pulmonary function, exercise capacity, and quality of life in a cohort of survivors. Chest 2005; 128: 2247–2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Naksuk N, Lazar S, Peeraphatdit TB Cardiac safety of off-label COVID-19 drug therapy: A review and proposed monitoring protocol. Eur Heart J Acute Cardiovasc Care 2020; 9: 215–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gov.UK Department for Digital, Culture, Media & Sport. Coronavirus (COVID-19): Guidance on the phased return of sport and recreation, https://www.gov.uk/government/publications/coronavirus-covid-19-guidance-on-phased-return-of-sport-and-recreation (2020, accessed 15 May 2020).
- 12. Niebauer J, Börjesson M, Carre F, et al. Brief recommendations for participation in competitive sports of athletes with arterial hypertension: Summary of a Position Statement from the Sports Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol 2019; 26: 1549–1555. [DOI] [PubMed] [Google Scholar]