Abstract
Background
To stop the spread of the new coronavirus disease in 2019 (COVID-19), many countries had completely locked down. This lockdown restricted the everyday life of the affected residents and changed their mobility pattern, but its effects on sleep pattern were largely unknown.
Methods
Here, utilizing one of the largest crowdsourced database (Sleep as Android), we analyzed the sleep pattern of 25 217 users with 1 352 513 sleep records between 1 January and 29 April 2020 in the US and 16 European countries (Germany, UK, Spain, France, Italy, The Netherlands, Belgium, Hungary, Denmark, Finland, Norway, Czech, Sweden, Austria, Poland and Switzerland) with more than 100 records in all days of 2020.
Results
During the COVID-19 pandemic, the sleeping pattern before and after the country-level lockdown largely differed. The subjects increased their sleep duration by an average of 11.3 to 18.6 min on weekday nights, except Denmark (4.9 min) and Finland (7.1 min). In addition, subjects form all 16 European countries delayed their sleep onset from 10.7 min (Sweden) to 29.6 min (Austria).
Conclusion
During the COVID-19 pandemic, residents in the US and 16 European countries delayed their bedtime and slept longer than usual.
Introduction
The outbreak of the new coronavirus disease in 2019 (COVID-19) is pandemic. Since its first recorded hospital admission on 16 December 2019,1 the number of cases was increased to 31 798 308 on 25 September 2020. Wuhan, the documented origin of the COVID-19 pandemic in China, was under lockdown and all public transport connecting Wuhan were suspended from 23 January 2020 for 79 days, which was the largest lockdown record in human history in terms of the number of people being quarantined (11 million).2 The success of the Wuhan lockdown in controlling the spread of COVID-19 led to similar quarantine policies in many regions experiencing rapid growth of the infection, including Lombardy, Italy on 21 February 20203 and Haro, Spain on 7 March 2020.4 The lockdown was soon extended to the entire country and many other countries in Europe. The situation in the country with the most confirmed cases, the USA, was similar. Most states were locked down except Arkansas, Iowa, Nebraska, North Dakota, and South Dakota.5
During the COVID-19 pandemic, regular sleep habits were being disrupted, as schools were shut down and some workers were required to work from home. We can expect that the pandemic has both positive and negative effects on sleep. Because of the lack of mandatory working time and the time saved from commuting, people may tend to oversleep. It was also possible that the changing mode of work introduced unexpected workload to some workers so that their working hours were lengthened. In addition, the anxiety about the pandemic and the depression caused by the isolation may reduce people’s sleep quality.6 Most importantly, the restrictive measures varied greatly across different regions and time, making the effect of lockdown unevenly distributed across populations. Several cross-sectional surveys examined the sleep pattern during the pandemic.7–12 Most of them were conducted in China and concluded that the COVID-19 outbreak had a negative impact on sleep quality, but they suffered from several major limitations. The most significant limitation was the cross-sectional nature of these surveys that does not allow comparison of sleep pattern before and after the pandemic.
Here, we utilized one of the largest crowdsourced databases of sleep records obtained from Sleep as Android app (methodological details of the app provided in the Methods section below) to acquire insights on how COVID-19 affect people’s sleep pattern. This app was launched in 2011 and the data collection is ongoing currently, thus the data allow us to examine the change in sleep pattern during the COVID-19 outbreak with reference to sleep records before the outbreak. We evaluated the impact of lockdown on the sleep pattern of Sleep as Android app users residing in the US and 16 European countries (Germany, UK, Spain, France, Italy, The Netherlands, Belgium, Hungary, Denmark, Finland, Norway, Czech, Sweden, Austria, Poland and Switzerland), and stratified the impact by age and gender.
Methods
Sleep as Android
The Sleep as Android smartphone application (https://sleep.urbandroid.org/) is developed for the Android operating system as a smart alarm clock that wakes the users according to their sleep cycles and can ensure the users have wakened up. Sleep onset time can be identified using two methods, namely subjective manual assignment and objective detection. Nearly all (99.6%) of the users selected the first method, where the sleep onset was defined as the moment when they pressed the ‘start sleep tracking’ button in the app. For the remaining 0.4% users, they used an automatic sleep tracking function that detects the sleep onset of the users via different sources, including external wearable wristbands, the built-in accelerometer in the smartphone, sleep sounds such as snores, and contactless ultrasonic tracking.13 The awake time was defined as the moment when they terminated the tracking manually, interacted with the phone, talked near the phone and detected by the app, or the light sensor of the phone showed >60 lux after the sunset time of the geographical location. It has accumulated more than 300 000 reviews in Google Play and is one of the most reviewed and highest rated apps for sleep analysis.14,15
Data retrieval
Only data from users who agreed to share their data were retrieved. Sleep as Android began to collect data in 2010, however, the sample size in 2010 was too small and we decided to analyze the sleep data from 1 January 2011. The end date was set on 29 April 2020. A total of 34 897 073 sleep records (hereby denoted as ns) from 143 733 users (hereby denoted as nu) were retrieved. Variables available in the dataset include the date of the sleep records, sleep duration, sleep onset time, self-rating of sleep quality (from 1 to 5 by 0.25 step) and time zone obtained from the smartphone’s system information. Age and sex were also collected but were available only for some sleep records.
Data processing
Outliers and impossible records of sleep duration were removed from the analysis. These included sleep duration of <3 h or >13 h and sleep onset time between 6:00 and 18:00. Furthermore, we treated all sleep records with sleep onset time between 0:00 and 6:00 as the sleep occurred at its previous day (e.g. sleep onset at 2 January 1:00 was treated as sleep occurred on 1 January). As records with sleep onset time between 6:00 and 18:00 may potentially indicate irregular sleep patterns, we compared the percentage of sleep records in 2020 with sleep onset fallen in this time interval before and during the lockdown and the results are shown in Supplementary table S1. Before lockdown, the percentages in the USA ranged from 3.1% to 6.8% and those in European countries ranged from 1.9% to 4.1%. These percentages reduced significantly during lockdown in most countries and regions, and the percentage point reduction ranged from 0.2% to 2.0%.
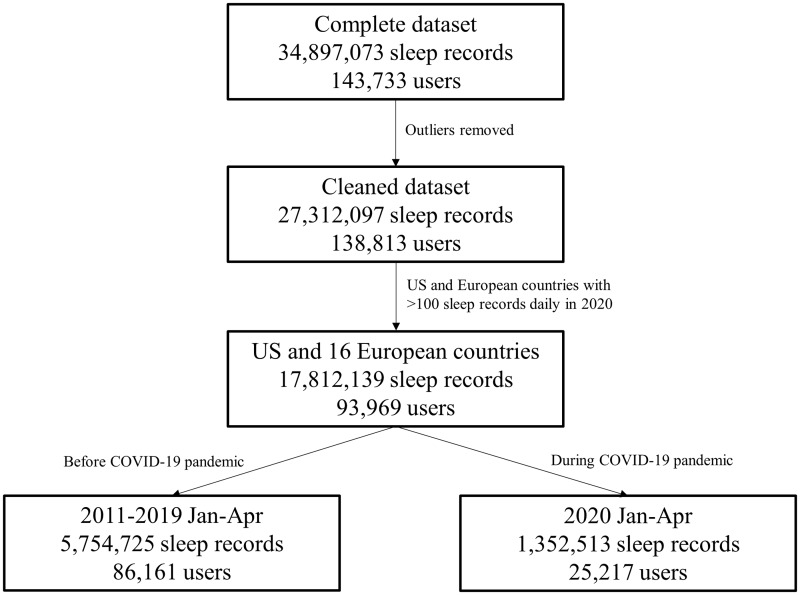
Our analysis of sleep records during the COVID-19 pandemic started on 1 January 2020. Sleep records from the USA were divided by time zones (America/Chicago [representing Central time zone], America/Denver [representing Mountain time zone], America/Los Angeles [representing Pacific time zone], America/New York [representing Eastern time zone] and others). Sleep records from European countries with more than 100 records in all days of 2020 (Germany, UK, Spain, France, Italy, The Netherlands, Belgium, Hungary, Denmark, Finland, Norway, Czech, Sweden, Austria, Poland and Switzerland) were included in the analysis. Time zones of Europe/Berlin and Europe/Busingen were classified as Germany and time zones of Europe/London, GB, and GB_Eire were classified as the UK. Similar to a previous report using data from Sleep as Android, the system time zone, instead of geographical coordinates, was used to classify the user location due to missing data.16 A total of 1 352 513 sleep records from 25 217 users from 1 January to 29 April 2020 were available for analysis. The flow chart describing the data selection process is shown in figure 1, and the sample size by country could be found in table 1.
Figure 1.
Flow of the data selection process
Table 1.
Descriptive statistics
| Country | Number of subjects nu (Jan–Apr, 2011–2019) | Number of sleep records ns (Jan–Apr, 2011–2019) | Number of subjects nu (Jan–Apr, 2020) | Number of subjects in nu Jan–Apr, 2020 who had data in Jan–Apr, 2011–2019 | Number of sleep records ns (Jan–Apr, 2020) | Age for sleep records in 2020 (years) a | ns (%) male for sleep records in 2020 a |
|---|---|---|---|---|---|---|---|
| USA | |||||||
| Chicago | 7893 | 545 322 | 2417 | 1482 (61.3%) | 131 158 | 40.11 (12.01) (ns = 41 498) | 34 910 (83.5%) |
| Denver | 2699 | 121 963 | 947 | 484 (51.1%) | 41 101 | 41.60 (14.62) (ns=14 008) | 11 510 (82.6%) |
| Los Angeles | 7234 | 474 932 | 2237 | 1338 (59.8%) | 119 009 | 38.22 (11.80) (ns=36 425) | 30 655 (83.5%) |
| New York | 12 802 | 837 360 | 4086 | 2479 (60.7%) | 222 419 | 39.21 (13.56) (ns=74 913) | 64 635 (85.3%) |
| Others | 3694 | 139 976 | 458 | 206 (45.0%) | 18 141 | 43.17 (12.74) (ns=5771) | 5108 (87.3%) |
| Germany | 9790 | 785 195 | 3251 | 2051 (63.1%) | 190 026 | 43.17 (12.74) (ns=5771) | 56 853 (91.0%) |
| UK | 7931 | 608 764 | 2422 | 1486 (61.4%) | 141 546 | 38.12 (12.50) (ns=61 888) | 39 975 (90.8%) |
| Spain | 2574 | 112 623 | 556 | 279 (50.2%) | 22 307 | 41.09 (10.92) (ns=8387) | 7688 (91.1%) |
| France | 4659 | 298 177 | 1313 | 744 (56.7%) | 65 140 | 36.86 (12.14) (ns=25 980) | 24 284 (92.9%) |
| Italy | 2984 | 147 910 | 758 | 400 (52.8%) | 33 830 | 37.67 (13.06) (ns=12 425) | 11 686 (94.7%) |
| The Netherlands | 5512 | 414 919 | 1437 | 922 (64.2%) | 86 726 | 38.02 (12.80) (ns=30 079) | 27 674 (91.2%) |
| Belgium | 2735 | 139 518 | 502 | 280 (55.8%) | 23 773 | 38.04 (12.64) (ns=8524) | 7825 (91.7%) |
| Hungary | 1366 | 101 815 | 378 | 224 (59.3%) | 21 887 | 38.13 (9.53) (ns=8078) | 7761 (96.1%) |
| Denmark | 963 | 67 114 | 279 | 155 (55.6%) | 14 575 | 40.43 (16.58) (ns=5098) | 4535 (91.6%) |
| Finland | 1406 | 126 127 | 433 | 280 (64.5%) | 26 303 | 39.05 (9.72) (ns=10 011) | 8005 (79.9%) |
| Norway | 1199 | 93 743 | 359 | 216 (60.2%) | 19 419 | 35.63 (10.46) (ns=6438) | 6430 (96.1%) |
| Czech | 2651 | 212 748 | 829 | 527 (63.6%) | 46 678 | 36.45 (11.29) (ns=16 709) | 16 323 (96.4%) |
| Sweden | 1896 | 148 737 | 593 | 393 (66.3%) | 34 639 | 39.03 (11.18) (ns=12 640) | 11 185 (87.7%) |
| Austria | 1880 | 78 799 | 569 | 281 (49.4%) | 19 044 | 36.86 (11.53) (ns=6680) | 5848 (87.4%) |
| Poland | 2729 | 189 905 | 912 | 531 (58.2%) | 50 033 | 34.27 (12.71) (ns=15 403) | 14 606 (95.3%) |
| Switzerland | 1564 | 109 078 | 481 | 280 (58.2%) | 24 759 | 37.28 (11.69) (ns=10 070) | 9719 (94.3%) |
| Total | 86 161 | 5 754 725 | 25 217 | 15 038 (59.6%) | 1 352 513 | 38.59 (12.63) (ns=455 195) | 407 215 (88.9%) |
Only for subjects who provided personal information.
Statistical analysis
Three sleep parameters, namely sleep duration, sleep onset time and subjective sleep quality, were analyzed in the current study. We compared the deviation (with 95% confidence interval) from expected values of the three sleep parameters at each date from 1 January to 29 April 2020, which equaled the difference between actual and expected values. The expected value of these sleep parameters equaled their means in the same region at the same month and day (S/M/T/W/T/F/S) of the record,16,17 computed from 11 509 510 sleep records from 64 470 users from 1 January to 29 April of 2011–2019. The means and standard deviations of the sleep parameters from years 2011–2019 were similar, which justified the data pooling (Supplementary table S2). The sample size by country could be found in table 1. In addition, we compared the aforementioned three deviations of sleep parameters in 2020 before and after the date of the implementation of domestic lockdown at individual countries 18 using t-test. Sweden had only implemented partial lockdown from 14 March 2020 and this was used as her cutoff date. Similarly, we also compared these three deviations before and after the COVID-19 outbreak for each country using t-test, where the onset of the outbreak of a country was defined as the first day with at least 100 confirmed cases in that country.19 Additional subgroup analyses were performed to compare the sleep pattern by sex and age (nu=5519 [21.9%] users who provided their sex and date of birth, ns=117 230 [8.7%]). The age of the users was categorized as <25, 25–34, 35–44, 45–54 and 55–64. All data analysis was conducted using SPSS version 25.
Results
Supplementary figure S1 shows the sleep duration of subjects in the USA. For the five regions in the USA (Chicago, Denver, Los Angeles, New York and others), the actual and expected sleep duration was about 430 min at weekday and 460 min at weekend. Before 3 March, the actual and expected sleep duration coincided, and the sleep duration has positively deviated from the expected duration afterward. After the lockdown, the deviations of sleep duration on weekday nights and weekend nights ranged from 7.1 to 14.2 min and 6.6 to 11.1 min, respectively (table 2). Overall speaking, the expected weekday–weekend difference in sleep duration was reduced during the lockdown. The deviations in most of the nights after the lockdown were significant for subjects in Chicago, Denver, Los Angeles and New York. Supplementary figures S2 and S3 show the sleep duration of subjects in the 16 European countries. Similar to the sleep duration of subjects in the USA, the actual and expected sleep duration of the subjects in Europe had a very small difference (within 5–10 min) before the lockdown. After lockdown, the deviations of sleep duration on weekday nights ranged from 11.3 to 18.6 min, except Denmark (4.9 min) and Finland (7.1 min) (table 2). On weekend nights, the deviation between actual and expected sleep duration in 2020 was insignificantly different with the deviation in 2011–2019 for several European countries, including Spain (5.8 min), Denmark (−0.9 min), Finland (5.1 min), Norway (4.7 min), Czech (3.2 min), Sweden (7.3 min), Austria (2.0 min) and Switzerland (3.3 min). Note that subjects in France had a small deviation (2.3 min) but the comparison with the deviation in 2011–2019 was significant due to the large sample size. Supplementary figures S8 and S9 show the deviations of the actual sleep duration and their 95% confidence intervals for subjects in the 16 European countries. The deviations in most of the nights after the lockdown were significant except for subjects from Belgium, Denmark, Finland, Norway, Austria and Switzerland.
Table 2.
Deviation (standard deviation) between actual (Jan–Apr 2020) and expected (Jan–Apr, 2011–2019) sleep parameters before and after lockdown
| Country | Weekday |
Weekend |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before lockdown |
After lockdown |
Before lockdown |
After lockdown |
|||||||||
| Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | Sleep duration (min) | Sleep onset (min) | Sleep rating (1-5) | Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | |
| USA | ||||||||||||
| Chicago | 7.70 (90.19) | −4.05 (116.37) | 0.02 (1.07) | 14.21*** (90.13) | 7.76*** (124.32) | 0.003 (1.08) | 4.13 (101.68) | −8.22 (123.10) | 0.02 (1.07) | 10.23*** (102.16) | 2.50*** (132.00) | −0.01 (1.10) |
| Denver | 4.86 (89.60) | −13.26 (114.58) | 0.05 (1.07) | 14.13*** (89.91) | 0.67*** (122.56) | 0.06 (1.07) | 3.45 (99.53) | −12.58 (120.26) | 0.13 (1.07) | 10.90*** (99.17) | −2.39 (129.30) | 0.16 (1.10) |
| Los Angeles | 2.82 (91.02) | −5.54 (117.77) | 0.06 (1.04) | 7.62*** (91.23) | 11.46*** (126.71) | 0.06 (1.04) | 2.55 (101.10) | −10.86 (123.11) | 0.04 (1.02) | 10.91*** (97.28) | 3.47*** (129.33) | 0.03 (1.02) |
| New York | 7.83 (91.40) | −9.99 (117.07) | 0.06 (1.05) | 13.89*** (91.27) | 4.08*** (122.11) | 0.07 (1.03) | 4.73 (103.21) | −13.28 (122.29) | 0.06 (1.05) | 11.10*** (100.17) | −3.01*** (126.10) | 0.04 (1.05) |
| Others | −6.48 (96.33) | 0.07 (125.06) | 0.11 (1.14) | 7.10*** (95.48) | 24.18*** (125.42) | −0.0002 (1.12) | −3.23 (108.56) | −4.15 (129.25) | 0.17 (1.13) | 6.57** (105.12) | 11.89*** (132.01) | 0.07 (1.10) |
| Germany | 4.46 (86.02) | 0.94 (107.95) | 0.05 (1.04) | 13.89*** (85.45) | 19.37*** (115.66) | 0.08* (1.05) | 4.09 (98.31) | −4.80 (115.63) | 0.06 (1.04) | 6.79** (92.57) | 5.56*** (118.27) | 0.05 (1.04) |
| UK | 3.32 (84.82) | −1.67 (102.49) | 0.04 (1.04) | 11.99*** (86.09) | 15.26*** (110.43) | 0.06 (1.06) | 1.26 (96.11) | −4.48 (111.06) | 0.04 (1.05) | 4.91** (93.77) | 4.74*** (115.21) | 0.06 (1.04) |
| Spain | 2.92 (83.32) | −7.61 (93.23) | 0.11 (1.14) | 13.51*** (81.17) | 26.50*** (104.79) | 0.14 (1.19) | 7.18 (98.26) | −7.74 (102.80) | 0.03 (1.22) | 5.80 (89.06) | 20.66*** (108.69) | 0.20** (1.20) |
| France | 3.30 (86.40) | −0.89 (100.24) | 0.06 (1.10) | 18.34*** (85.16) | 28.96*** (109.58) | 0.12** (1.09) | −1.16 (96.32) | −4.79 (109.96) | 0.09 (1.09) | 2.32* (93.54) | 17.75*** (116.88) | 0.09 (1.10) |
| Italy | 6.32 (83.99) | −4.84 (96.40) | 0.05 (1.08) | 16.76*** (80.95) | 20.18*** (99.83) | −0.01* (1.06) | 2.77 (92.01) | −6.22 (102.30) | 0.05 (1.07) | 14.15*** (85.02) | 10.97*** (101.93) | 0.04 (1.06) |
| The Netherlands | 6.38 (83.43) | −5.67 (99.71) | 0.04 (1.06) | 13.14*** (80.77) | 11.40*** (101.08) | 0.07* (1.05) | 3.69 (93.74) | −4.55 (108.76) | 0.06 (1.05) | 9.17*** (87.49) | −0.13** (106.00) | 0.05 (1.04) |
| Belgium | 6.28 (81.60) | 3.34 (102.59) | 0.08 (1.03) | 13.03*** (78.88) | 20.21*** (108.03) | 0.04 (1.05) | −0.28 (92.10) | −5.78 (112.09) | 0.03 (1.03) | 6.93** (86.47) | 0.69 (107.67) | 0.08 (1.04) |
| Hungary | 7.98 (76.98) | −2.81 (96.99) | −0.12 (1.16) | 18.58*** (79.25) | 21.08*** (104.62) | −0.13 (1.19) | 6.32 (93.55) | −2.65 (109.85) | −0.12 (1.13) | 13.79** (83.80) | 17.32*** (112.11) | −0.10 (1.10) |
| Denmark | 2.46 (81.13) | −1.55 (97.58) | 0.08 (0.96) | 4.94 (78.52) | 17.10*** (105.70) | 0.03 (1.02) | 4.70 (91.62) | −13.05 (109.28) | 0.09 (0.95) | −0.94 (80.20) | −9.74 (111.46) | 0.06 (0.95) |
| Finland | 3.52 (87.17) | −7.07 (110.25) | −0.07 (0.98) | 7.12** (87.02) | 14.99*** (114.53) | −0.01* (1.03) | 1.87 (96.22) | −3.68 (118.08) | −0.03 (0.98) | 5.13 (88.82) | 5.98** (118.19) | −0.005 (1.01) |
| Norway | 7.36 (86.86) | −3.74 (105.46) | −0.03 (0.96) | 12.33** (85.43) | 14.90*** (110.34) | −0.10* (0.96) | 8.21 (97.24) | −3.13 (119.59) | −0.09 (0.96) | 4.74 (88.68) | 9.69** (121.10) | −0.14 (1.00) |
| Czech | 4.28 (86.22) | −3.54 (103.39) | 0.01 (1.06) | 16.78*** (85.16) | 19.30*** (110.62) | 0.07** (1.04) | 1.17 (97.21) | −5.50 (111.61) | 0.08 (1.04) | 3.21 (89.55) | 4.93*** (115.33) | 0.09 (1.03) |
| Sweden | 8.09 (85.13) | 1.27 (108.01) | −0.02 (1.07) | 13.38*** (82.36) | 10.66*** (110.04) | −0.0002 (1.03) | 6.61 (92.91) | −1.93 (111.20) | −0.04 (1.04) | 7.25 (88.74) | 1.29 (112.90) | −0.03 (1.03) |
| Austria | 2.77 (87.57) | 10.33 (104.22) | 0.13 (1.02) | 11.28*** (84.08) | 29.57*** (112.41) | 0.17 (1.04) | 1.91 (96.46) | 3.97 (113.85) | 0.12 (1.03) | 1.99 (91.83) | 22.98*** (116.72) | 0.23* (0.98) |
| Poland | 5.91 (86.22) | −0.56 (101.23) | 0.02 (1.08) | 17.95*** (85.73) | 20.00*** (104.79) | 0.07 (1.08) | 4.85 (99.81) | −4.81 (103.97) | 0.04 (1.06) | 11.21*** (93.33) | 10.52*** (103.88) | 0.09 (1.05) |
| Switzerland | 8.92 (81.74) | 9.71 (100.47) | −0.07 (1.12) | 12.42** (80.15) | 22.56*** (102.50) | −0.13* (1.13) | 1.86 (94.65) | −1.64 (110.41) | −0.06 (1.14) | 3.26 (91.11) | 4.29* (114.26) | −0.11 (1.14) |
*/**/*** comparison with sleep parameters before lockdown significant at 5%/1%/0.1% level.
Supplementary figure S4 shows the sleep onset time of subjects in the USA. Note that the sleep onset time has not been adjusted for daylight saving time which began on 8 March due to the overlap with the lockdown which began on 3 March. The sleep onset time was at 00:00 on weekdays and 00:30–01:00 on weekends. In Chicago, Los Angeles and other time zones, there were no deviations with the expected sleep onset immediately after the lockdown, and the deviations began in early April which was caused by the change of expected sleep onset time. In Denver and New York time zones, the actual sleep onset time was about 20–30 min earlier than the expected sleep onset, and such a deviation only lasted for 2–3 weeks. Table 2 shows that the deviation of sleep onset time varied among subjects in different US time zones on weekday nights (from 0.7 min to 24.2 min), but the deviation on weekend nights was consistent (within 3.5 min for Chicago, Denver, Los Angeles and New York time zones). Supplementary figure S10 shows the deviations of the actual sleep onset and their 95% confidence intervals for subjects in the USA. For Chicago, Los Angeles and New York time zones, the deviation was significantly smaller than zero from lockdown to early April and was significantly larger than zero from early April. Supplementary figures S5 and S6 show the sleep onset time of subjects in the 16 European countries. Again, the sleep onset time has not been adjusted for daylight saving time which began on 29 March due to the overlap with the lockdown which began on 9–21 March. Subjects from most European countries (except The Netherlands, Belgium, Finland and Norway) began to delay their sleep onset time 1–2 weeks before the lockdown. The deviations of sleep onset on weekday nights after lockdown were significantly differed with the deviation before lockdown for all 16 European countries, ranged from 10.7 min (Sweden) to 29.6 min (Austria) (table 2). On the other hand, the delay on weekend nights was within 6 min in some countries (Germany, UK, The Netherlands, Belgium, Denmark, Finland, Czech, Sweden and Switzerland), but in some other countries, the delay was larger than 20 min (Spain and Austria). Supplementary figures S8 and S9 show the deviations of the actual sleep onset and their 95% confidence intervals for subjects in the 16 European countries. After lockdown, the deviations for all countries were mostly positive except on 29–31 March which were negative.
Supplementary figures S13–S18 shows the sleep rating (a rating from 1 to 5) and the deviation to the expected sleep rating of all subjects. No special pattern was found. Deviations in all regions after lockdown were less than 0.2 except the weekend sleep rating of subjects in Spain.
Table 3 shows the deviations of sleep parameters before and after COVID-19 outbreak, and the deviation patterns were very similar to the comparison before and after lockdown. Supplementary table S3 shows the results of the subgroup analysis. At weekdays, females had a significantly larger increase in sleep duration during the lockdown in the USA (except Los Angeles), Germany, UK, Italy, Belgium, Hungary, Denmark, Finland, Czech, Sweden and Austria, while in the remaining countries females and males had similar sleep duration. Females had a larger delay in sleep onset during the lockdown in the USA (New York and others), Spain, Denmark, Sweden, Austria and Switzerland, and less delay in the USA (Chicago), Germany, UK, The Netherlands, Belgium and Hungary. In most countries, females and males had similar deviations in sleep ratings, and significant differences were found in the USA (New York and others), UK, Belgium, Czech, Austria and Switzerland. Across age groups, significant differences in sleep duration and sleep onset were found in all countries except Hungary (sleep duration). In general, younger users had larger deviations in sleep duration and sleep onset. Trends for weekends were similar to that for weekdays.
Table 3.
Deviation (standard deviation) between actual (Jan–Apr 2020) and expected (Jan–Apr, 2011–2019) sleep parameters before and after COVID-19 outbreak (defined as the first day with >100 confirmed cases in a country)
| Country | Weekday |
Weekend |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before outbreak |
After outbreak |
Before outbreak |
After outbreak |
|||||||||
| Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | Sleep duration (min) | Sleep onset (min) | Sleep rating (1–5) | |
| USA | ||||||||||||
| Chicago | 7.60 (90.03) | −2.24 (116.59) | 0.02 (1.08) | 14.98*** (90.35) | 5.96*** (124.91) | 0.003 (1.08) | 3.67 (101.92) | −6.15 (123.12) | 0.02 (1.07) | 12.00*** (101.74) | 0.61*** (133.52) | −0.01 (1.09) |
| Denver | 4.94 (89.72) | −11.14 (115.01) | 0.05 (1.07) | 15.02*** (89.68) | −1.71*** (122.98) | 0.06 (1.07) | 2.77 (99.62) | −10.27 (120.48) | 0.13 (1.07) | 13.72*** (98.70) | −5.23* (130.75) | 0.18 (1.11) |
| Los Angeles | 2.73 (90.95) | −3.39 (118.10) | 0.06 (1.04) | 8.20*** (91.35) | 9.56*** (127.34) | 0.06 (1.03) | 2.27 (101.26) | −8.25 (123.59) | 0.03 (1.02) | 12.77*** (96.21) | 1.15*** (129.80) | 0.04 (1.02) |
| New York | 7.74 (91.31) | −7.98 (117.19) | 0.06 (1.05) | 14.61*** (91.36) | 2.14*** (122.65) | 0.07 (1.03) | 4.13 (103.13) | −10.72 (122.35) | 0.05 (1.05) | 13.20*** (99.68) | −5.90*** (126.85) | 0.05 (1.05) |
| Others | −6.62 (96.55) | 2.34 (125.42) | 0.12 (1.15) | 8.11*** (95.10) | 23.44*** (125.33) | −0.01*** (1.11) | −3.34 (108.64) | −1.99 (129.96) | 0.17 (1.14) | 7.81** (104.56) | 11.28*** (131.71) | 0.06 (1.09) |
| Germany | 4.48 (86.32) | −2.70 (108.02) | 0.05 (1.04) | 11.58*** (85.22) | 17.27*** (113.64) | 0.08** (1.05) | 3.15 (98.43) | −5.66 (115.83) | 0.05 (1.04) | 7.34*** (93.95) | 3.95*** (117.30) | 0.06 (1.03) |
| UK | 3.29 (84.83) | −2.83 (102.35) | 0.04 (1.04) | 10.55*** (85.89) | 14.83*** (109.21) | 0.05 (1.06) | 0.93 (96.47) | −5.30 (111.03) | 0.04 (1.05) | 4.69*** (93.60) | 4.13*** (114.23) | 0.07 (1.05) |
| Spain | 2.31 (83.80) | −9.54 (92.93) | 0.09 (1.14) | 12.21*** (80.82) | 22.28*** (102.87) | 0.15 (1.19) | 6.54 (98.83) | −9.61 (102.64) | 0.02 (1.22) | 7.15 (90.20) | 17.31*** (107.60) | 0.19** (1.21) |
| France | 3.54 (86.65) | −2.98 (100.15) | 0.06 (1.10) | 14.61*** (85.30) | 25.90*** (107.59) | 0.10* (1.09) | −1.39 (96.57) | −6.28 (110.12) | 0.08 (1.09) | 1.95* (93.72) | 15.31*** (115.16) | 0.10 (1.09) |
| Italy | 8.27 (83.42) | 0.27 (96.90) | 0.04 (1.08) | 16.58*** (81.43) | 18.01*** (102.62) | 0.02 (1.07) | 5.10 (91.02) | −2.43 (102.18) | 0.05 (1.06) | 12.74** (84.92) | 7.95*** (103.18) | 0.05 (1.04) |
| The Netherlands | 6.47 (83.43) | −5.94 (99.62) | 0.04 (1.06) | 12.75*** (80.89) | 11.36*** (101.15) | 0.07* (1.06) | 3.69 (93.74) | −4.55 (108.77) | 0.06 (1.05) | 9.17*** (87.49) | −0.13** (106.00) | 0.05 (1.04) |
| Belgium | 5.13 (82.34) | −0.44 (100.89) | 0.07 (1.03) | 13.15*** (78.04) | 22.53*** (108.66) | 0.06 (1.06) | −0.84 (93.35) | −8.10 (111.56) | 0.01 (1.03) | 5.88** (85.43) | 3.57*** (109.87) | 0.10* (1.03) |
| Hungary | 9.82 (77.87) | −0.89 (97.97) | −0.12 (1.16) | 13.93** (77.85) | 14.00*** (102.81) | −0.11 (1.18) | 7.63 (93.69) | −2.67 (111.63) | −0.14 (1.13) | 10.71 (84.69) | 15.44*** (108.84) | −0.06 (1.12) |
| Denmark | 2.53 (81.11) | −3.95 (96.98) | 0.08 (0.96) | 4.51 (78.90) | 19.02*** (105.07) | 0.03 (1.01) | 5.05 (91.83) | −13.88 (108.79) | 0.09 (0.96) | −0.70 (81.55) | −8.86 (111.88) | 0.09 (0.94) |
| Finland | 3.86 (86.96) | −5.10 (110.38) | −0.07 (0.99) | 6.95* (87.58) | 14.23*** (115.60) | −0.003* (1.03) | 2.86 (95.66) | −3.45 (117.49) | −0.03 (0.99) | 3.07 (88.93) | 7.43** (119.81) | −0.001 (0.99) |
| Norway | 7.17 (87.01) | −4.83 (105.37) | −0.03 (0.97) | 12.05** (85.33) | 14.57*** (109.72) | −0.09* (0.95) | 6.95 (97.38) | −3.60 (120.58) | −0.10 (0.96) | 7.40 (89.85) | 8.50** (119.22) | −0.12 (0.99) |
| Czech | 5.17 (86.40) | −1.95 (103.84) | 0.01 (1.06) | 16.43*** (84.69) | 18.77*** (111.11) | 0.06* (1.01) | 1.17 (97.21) | −5.50 (111.61) | 0.08 (1.04) | 3.21 (89.55) | 4.93*** (115.33) | 0.09 (1.04) |
| Sweden | 8.16 (85.28) | 0.97 (108.19) | −0.03 (1.07) | 12.90*** (82.29) | 10.60*** (109.57) | 0.001 (1.03) | 6.86 (92.79) | −2.51 (110.88) | −0.03 (1.05) | 6.78 (89.29) | 2.03 (113.27) | −0.04 (1.03) |
| Austria | 2.64 (87.54) | 9.29 (103.98) | 0.13 (1.02) | 11.01*** (84.38) | 30.53*** (112.10) | 0.17 (1.07) | 1.36 (96.83) | 3.73 (113.86) | 0.11 (1.03) | 3.09 (91.41) | 21.98*** (116.51) | 0.23* (0.97) |
| Poland | 7.15 (86.32) | 0.96 (101.46) | 0.03 (1.08) | 17.03*** (85.63) | 20.07*** (105.07) | 0.06 (1.09) | 5.34 (99.67) | −4.44 (103.84) | 0.04 (1.06) | 10.71** (93.10) | 11.10*** (104.16) | 0.09 (1.04) |
| Switzerland | 9.29 (81.88) | 8.31 (100.73) | −0.07 (1.12) | 11.31 (80.21) | 22.70*** (101.64) | −0.13 (1.13) | 1.17 (95.01) | −2.55 (111.00) | −0.08 (1.14) | 3.96 (91.30) | 4.37* (112.61) | −0.08 (1.15) |
*/**/***Comparison with sleep parameters before lockdown significant at 5%/1%/0.1% level.
Discussion
Using crowdsourced smartphone-measured sleep data (Sleep as Android) of more than 10 million records, this study examined the sleep pattern in the USA and 16 European countries during the COVID-19 outbreak. To summarize, the results showed that the sleep pattern changed immediately after the law of quarantine and suspension. The subjects increased their sleep duration by an average of 11.3–18.6 min on weekday nights, except Denmark (4.9 min) and Finland (7.1 min). In addition, subjects form all 16 European countries delayed their sleep onset from 10.7 min (Sweden) to 29.6 min (Austria). The magnitude of the change in sleep duration and sleep onset was similar to those found among subjects in China before and after the Wuhan lockdown on 23 January20 and data from Finnish from another smartphone app, Polar Research Center.21
At the time of complete lockdown, all employees were required to work from home except those who have to work at their offices, such as healthcare professionals or police. This mode of work might be the main driver of this change of sleep pattern as those under quarantine were not required to work at scheduled hours, and such a change in work mode increased the proportion of healthy sleep duration (7–9 h per day22,23) from 50.1% to 52.3% in our data. This change was a short-term one and we can expect that such a change might improve the mood and mental health conditions of the users.6 Longitudinal objective data suggested that residents under lockdown would reduce their physical activity level,24,25 and this reduction was likely to affect sleep quality substantially. However, our results showed that subjective sleep quality was unchanged during the lockdown, which implied that the protective factors (in particular working from home) had a similar effect on sleep quality on the risk factors. Many countries had announced their plan to ease the lockdown from early May,26 therefore this special sleep pattern found during the lockdown will be back to usual very soon, even when the COVID-19 pandemic is still ongoing. Whether this short period (about 2 months) of change will have any long-term impact on future sleep pattern and mental health should be investigated.
The advantages of using crowdsourced data lie on the large sample size and participants from all regions around the world, and the research participation burden in such kind of research is minimal. Also, with a large number of sleep records from 2011 to 2019, we were able to estimate the expected, normal sleep pattern, thus determining the change in sleep pattern during the COVID-19 outbreak. This kind of longitudinal observation is almost impossible using traditional prospective design as the sleep pattern before and during the outbreak need to be both measured.27
A major limitation of our study was on the unknown measurement error of the Sleep as Android app. The first source of measurement error was the measurement on sleep onset time, where the delay between the time of pressing the ‘start sleep tracking’ button and the exact sleep onset was not measurable. The second source of measurement error was the calibration algorithm of subjective sleep onset and awake detections. The sensitivity of such detections varied across smartphone devices and environmental factors,27 and it is almost impossible to be adjusted for in this large-scale study. A comparison study between the Sleep as Android app and polysomnography/actigraphy could quantify the measurement error of the Sleep as Android app, but no similar studies were conducted to our knowledge. Another major limitation was the composition of our sample. More than half of the sleep records missed the data in age and sex, therefore the representativeness of our sample in terms of age–sex distribution could not be evaluated. A previous study found that males and females were equally likely to use smartphone app to monitor sleep,28 therefore it was likely that we have a balanced gender in our dataset. The reason for the large male proportion in our sample might be because fewer female participants were willing to reveal their personal information due to their sensitivity to internet privacy.29 Although not assessable, we can expect that the users of the Sleep as Android app would be younger and wealthier than non-users.30 It was also likely that the users were more interested in monitoring their sleep so that their sleeping pattern might be different from that of the non-users. Here, we used a binary indicator to classify the lockdown status of a country, which simplified the actual situation that different levels of lockdown measures were implemented within different regions of a country, and the level varied by time. This approach simplified the spatial–temporal details of lockdown measures, however, our data lack the information to perform such an analysis. Furthermore, the app did not provide any flexibility to add information specific questions and some important variables were unable to collect, for example, whether the users or those having close contact with them had been diagnosed for COVID-19. Concerning the impact of a disease outbreak on sleep pattern and other mental health problems, healthcare workers, patients and the general population are expected to behave differently,31–35 but we were unable to identify the occupation of the users. Finally, although the physical activity level of the users can be measured by smartphone, Sleep as Android app did not measure the physical activity level outside the sleep tracking period, hence the association between physical activity and sleep pattern could not be examined. There may exist other smartphone apps that collect both types of data and examination of these data would be valuable.
Several studies showed that the general public and healthcare workers suffered from various psychological impacts including depression, anxiety and insomnia during the COVID-19 outbreak.7,10,35 The results of this study add new knowledge on top of this existing study that the general public in the USA and Europe also experienced a change in sleep pattern. It is well-known that lack of sleep causes mental health problems,23 and lockdown and suspension were causing an increase in sleep duration and mental health problems concurrently. It is worth investigating the role of such an increase in sleep duration as a protective effect on people's mental health.
Large-scale studies revealed that sleep pattern would be affected by national events. A previous study using the same source of data (Sleep as Android) as the current study found that the sleep duration was reduced at the immediate night after national events such as Brexit poll and US presidential election.16 Subjects had reduced sleep duration because they might have spent some of the sleep time on other activities, for example, social media and news. Similarly, information on COVID-19 is also spreading as fast as the virus itself, with an estimated basic reproduction number (R0) of 3.4 on YouTube and 4.6 on Twitter.36 It is believed that such a spread of news will lead to fear 37 so that people might have reduced their sleep duration, however, our results do not support this postulation, as shown by the fact that the subjective sleep ratings remained constant throughout the period of COVID-19 outbreak.
Conclusion/Policy recommendations
Due to the expected sleep problems caused by the lockdown, the European Academy for Cognitive‐Behavioral Treatment of Insomnia had published several recommendations to prevent possible sleep problems.38 They have noted several sleep parameters that are likely to be affected during the COVID-19 pandemic, including sleep disruption, insomnia and parent–child co-sleeping. These variables were not collected by Sleep as Android, and further research examining the change of these sleeping parameters, especially with objective data and longitudinal design, is warranted.
Supplementary Material
Acknowledgements
The authors would like to thank Jiri Ritcher (Urbandroid Team) for processing the study data.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
No funding was received for this study.
Conflicts of interest: None declared.
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Reuters. Wuhan lockdown ‘unprecedented’, shows commitment to contain virus: WHO representative in China. 2020. Available at: https://www.reuters.com/article/us-china-health-who/wuhan-lockdown-unprecedented-shows-commitment-to-contain-virus-who-representative-in-china-idUSKBN1ZM1G9 (26 March 2020, date last accessed).
- 3. Paul A. What towns in Italy are on lockdown because of coronavirus? 2020. Available at: https://metro.co.uk/2020/02/25/towns-italy-lockdown-coronavirus-12298246/ (14 May 2020, date last accessed).
- 4. Jones S. Spanish town faces police lockdown to contain coronavirus. 2020. Available at: https://www.theguardian.com/world/2020/mar/07/spanish-town-faces-police-lockdown-to-contain-coronavirus (14 May 2020, date last accessed).
- 5. Secon H, Woodward A. A map of the US cities and states under lockdown—and those that are reopening. 2020. Available at: https://www.businessinsider.com/us-map-stay-at-home-orders-lockdowns-2020-3 (14 May 2020, date last accessed).
- 6. National Sleep Foundation. Sleep Guidelines During the COVID-19 Pandemic. 2020. Available at: https://www.sleepfoundation.org/sleep-guidelines-covid-19-isolation [14 May 2020, date last accessed).
- 7. Xiao H, Zhang Y, Kong D, et al. The effects of social support on sleep quality of medical staff treating patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit 2020;26:e923549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 epidemic in China: a web-based cross-sectional survey. Psychiatr Res 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time, and digital media use during COVID-19 lockdown in Italy. J Sleep Res 2020;29:e13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatr Res 2020;289:113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020;88:901–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Xue Z, Lin L, Zhang S, et al. Sleep problems and medical isolation during the SARS-CoV-2 outbreak. Sleep Med 2020;70:112–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chaudhry BM. Sleeping with an Android. Mhealth 2017;3:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Choi YK, Demiris G, Lin SY, et al. Smartphone applications to support sleep self-management: review and evaluation. J Clin Sleep Med 2018;14:1783–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ong AA, Gillespie MB. Overview of smartphone applications for sleep analysis. World J Otorhinolaryngol Head Neck Surg 2016;2:45–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Anýž J, Bakštein E, Dudysová D, et al. No wink of sleep: population sleep characteristics in response to the brexit poll and the 2016 U.S. presidential election. Soc Sci Med 2019;222:112–21. [DOI] [PubMed] [Google Scholar]
- 17. Walch OJ, Cochran A, Forger DB. A global quantification of “normal” sleep schedules using smartphone data. Sci Adv 2016;2:e1501705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Porcher S. A novel dataset of governments’ responses to COVID-19 all around the world. 2020. halshs-02865150. [DOI] [PMC free article] [PubMed]
- 19. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis 2020;20:533–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lee PH, Marek J, Nálevka P. Crowdsourced smartphone data reveal altered sleep/wake pattern in quarantined Chinese during the COVID-19 outbreak. Chronobiol Int 2020;37:1181–90. [DOI] [PubMed] [Google Scholar]
- 21. Polar Research Center. Exercise and sleep habits in Finland during COVID-19 epidemic. 2020. Available at: https://www.polar.com/en/science/news/exercise-and-sleep-habits-in-finland-during-COVID-19-epidemic (8 September 2020, date last accessed].
- 22. Sun X, Zheng B, Lv J, et al. Sleep behavior and depression: findings from the China Kadoorie Biobank of 0.5 million Chinese adults. J Affect Dis 2018;229:120–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wang S, Li B, Wu Y, et al. Relationship of sleep duration with sociodemographic characteristics, lifestyle, mental health, and chronic diseases in a large Chinese adult population. J Clin Sleep Med 2017;13:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Di Sebastiano KM, Chulak-Bozzer T, Vanderloo LM, Faulkner G. Don’t walk so close to me: physical distancing and adult physical activity in Canada. Front Psychol 2020;11:1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. He M, Xian Y, Lv X, et al. Changes in body weight, physical activity, and lifestyle during the semi-lockdown period after the outbreak of COVID-19 in China: an online survey. Disaster Med Public Health Prep 2020. doi:10.1017/dmp.2020.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. VOA News. Italy, US Ease Coronavirus Lockdowns. 2020. Available at: https://www.voanews.com/covid-19-pandemic/italy-us-ease-coronavirus-lockdowns (15 May 2020, date last accessed).
- 27. Robbins R, Affouf M, Seixas A, et al. Four-year trends in sleep duration and quality: a longitudinal study using data from a commercially available sleep tracker. J Med Internet Res 2020;22:e14735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Escoffery C. Gender similarities and differences for e-health behaviors among U.S. adults. Telemed J E Health 2018;24:335–43. [DOI] [PubMed] [Google Scholar]
- 29. Hoy MG, Milne G. Gender differences in privacy-related measures for young adult Facebook users. J Interact Advert 2010;10:28–45. [Google Scholar]
- 30. Krebs P, Duncan DT. Health app use among US mobile phone owners: a national survey. JMIR mHealth uHealth 2015;3:e101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bai YM, Lin CC, Lin CY, et al. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv 2004;55:1055–7. [DOI] [PubMed] [Google Scholar]
- 32. Chua SE, Cheung V, McAlonan GM, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry 2004;49:385–90. [DOI] [PubMed] [Google Scholar]
- 33. Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Phil Trans R Soc Lond B 2004;359:1117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry 2007;52:241–7. [DOI] [PubMed] [Google Scholar]
- 35. Wang C, Pan R, Wang X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cinelli M, Quattrociocchi W, Galeazzi A, et al. The COVID-19 social media infodemic. Sci Rep 2020;10:16598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Chiolero A. Covid-19: a digital epidemic. BMJ 2020;368:m764. [DOI] [PubMed] [Google Scholar]
- 38. Altena E, Baglioni C, Espie C, et al. Dealing with sleep problems during home confinement due to the COVID‐19 outbreak: practical recommendations from a task force of the European CBT‐I Academy. J Sleep Res 2020;29:e13052. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.