Abstract
Introduction
The primary purpose of this work is to study coronavirus disease 2019 (COVID-19) in China and to identify the prognostic characteristics of patients with the highest death risk.
Material and methods
The statistical methods used to derive the results of this work are the chi-square test and one-way analysis of variance (ANOVA) to examine the characteristics of COVID-19 associated deaths. A multiple logistic regression analysis was used with the odds ratio (OR) to find statistically significant prognostic factors with the highest death risk for this type of disease.
Results
According to multiple logistic regression analyses, males (OR = 1.68; 95% CI: 1.48–1.91) who are over 50 years old (OR = 7.2; 95% CI: 1.01–51.6) from Hubei (OR = 7.73; 95% CI: 5.71–10.47) have the highest risk of death from this type of disease. Moreover, individuals who are retirees (OR = 2.83; 95% CI: 2.47–3.25) and had a Wuhan-related exposure (OR = 2.17; 95% CI: 1.68–2.79) have two times higher risk of death from COVID-19, while the risk is thirteen times higher with the comorbid condition “cardiovascular disease” (OR = 13.6; 95% CI: 10.3–17.9).
Conclusions
The results of this study describe for the first time the importance of cardiovascular disease as a primary prognostic risk factor for death from coronavirus disease 2019.
Keywords: prognostic factors, cardiovascular disease, COVID-19
Introduction
Coronavirus disease in 2019 (COVID-19) is a new virus belonging to the family of coronaviruses (CoV), which are single-stranded RNA viruses that infect not only humans but also animals [1]. Most of the initial outbreaks of COVID-19 are epidemiologically associated with exposure to Wuhan’s Huanan seafood market, which is why the original transmission mechanism was considered animal-to-human [2, 3]. It is assessed that 2% of the population are healthy carriers of a coronavirus and that these viruses are responsible for about 5–10% of the infections of the human respiratory system [4]. The number of patients is increasing rapidly, with confirmed cases reaching 84 385 and 4 643 deaths in China alone by April 2020 [5]. Symptoms that patients are faced with are fever, dry cough, and breathing difficulty [6]. Gastrointestinal symptoms and asymptomatic infections have also been reported [7–9]. In genetic terms, the new 2019-nCoV has 89% nucleotide identity with bat SARS-like-CoVZXC21 and 82% with that of human SARS-CoV, so it has been called SARS-CoV-2 [10]. Five days is the mean incubation period [11]. Drugs such as baricitinib, used in the treatment of rheumatoid arthritis, remdesivir, used to treat Ebola, and chloroquine, used to treat malaria, have the potential of blocking viral infection [12–14]. Age and underlying diseases have been reported as major risk factors for COVID-19. More specifically, patients over 60 years of age are at higher risk than children, who may have mild symptoms or even asymptomatic infection [11], while patients with comorbidities are more likely to develop respiratory failure [15].
This work studies COVID-19 in China during the period of December 2019 to February 2020 to identify the characteristics of patients with the highest death risk.
Material and methods
The data used in this work come from the World Health Organization dataset [16] and Chinese Center for Disease Control and Prevention [17] and cover the period of December 2019 to February 2020. The target population of the analysis is the 44 672 confirmed cases of patients with COVID-19 in China. The statistical methods used in this work are the χ2 test for categorical variables and one-way analysis of variance (ANOVA) for continuous variables to examine the statistical significance of the characteristics of COVID-19 associated deaths such as age, gender, province, occupation, Wuhan-related exposure, and comorbid condition. A multiple logistic regression analysis was used to assess the prognostic characteristics of patients with the highest risk of death from COVID-19. In particular, a cross-sectional study was performed, where the patients were divided into two groups: the case group and the control group. The control group comprised all patients who were infected with COVID-19 and survived. In contrast, the case group comprised all patients with the same characteristics as the control group who died from this disease. The data were weighted before being analyzed.
Statistical analysis
Predictors were represented using the OR and 95% confidence intervals and p < 0.05 was considered as statistically significant. The study was carried out using the IBM SPSS 25 software package for Windows.
Results
As shown in Table I, there is a statistically significant difference in the number of age-related deaths from COVID-19, predominantly in the age group of 70–79 (30.5%), while the most common gender is male (63.8%). Most patients who died from COVID-19 were retirees (46.1%) from Hubei (95.7%). However, most of them did not have a comorbid condition (31.9%). In addition, most patients who died from COVID-19 had a Wuhan-related exposure (92.8%). Finally, the period with the most deaths from COVID-19 in China was January 21–31, 2020 (48.3%).
Table I.
Characteristics of patients who died from COVID-19: China 2020 (χ2 and one-way analysis of variance (ANOVA) test)
| Paramter | Deaths | Percentages | P-value |
|---|---|---|---|
| Gender: | < 0.05 | ||
| Male | 653 | 63.8 | |
| Female | 370 | 36.2 | |
| Age: | < 0.05 | ||
| ≥ 80 | 208 | 20.3 | |
| 70–79 | 312 | 30.5 | |
| 60–69 | 309 | 30.2 | |
| 50–59 | 130 | 12.7 | |
| 40–49 | 38 | 3.7 | |
| 30–39 | 18 | 1.8 | |
| 20–29 | 7 | 0.7 | |
| 10–19 | 1 | 0.1 | |
| Occupation: | < 0.05 | ||
| Service industry | 23 | 2.2 | |
| Farmer/laborer | 139 | 13.6 | |
| Health worker | 5 | 0.5 | |
| Retiree | 472 | 46.1 | |
| Other/none | 384 | 37.5 | |
| Province: | < 0.05 | ||
| Hubei | 979 | 95.7 | |
| Other | 44 | 4.3 | |
| Wuhan-related exposure: | < 0.05 | ||
| Yes | 853 | 92.8 | |
| No | 66 | 7.2 | |
| Comorbid condition: | < 0.05 | ||
| Hypertension | 161 | 1.2 | |
| Diabetes | 80 | 6.3 | |
| Cardiovascular disease | 92 | 15.9 | |
| Chronic respiratory disease | 32 | 18.3 | |
| Cancer (any) | 6 | 26.4 | |
| None | 133 | 31.9 | |
| Period (by date of onset): | < 0.05 | ||
| Before Dec 31, 2019 | 15 | 1.5 | |
| Jan 1–10, 2020 | 102 | 10 | |
| Jan 11–20, 2020 | 310 | 30.3 | |
| Jan 21–31, 2020 | 494 | 48.3 | |
| After Feb 1, 2020 | 102 | 10 | |
Table II shows the multiple logistic regression analysis and odds ratios to find the prognostic characteristics of individuals with the highest risk of death from COVID-19. As shown in Table II, all prognostic factors are statistically significant (p < 0.05). According to multiple logistic regression, the risk of death from COVID-19 is significantly higher in men (OR = 1.68; 95% CI: 1.48–1.91), from Hubei (OR = 7.73; 95% CI: 5.71–10.47), in the age group of 50 and over. The age group of 50-59 has seven times higher risk than younger ages (OR = 7.2; 95% CI: 1.01–51.6) and the risk is significantly higher as age increases. Finally, those who are retirees (OR = 2.83; 95% CI: 2.47–3.25) and had a Wuhan-related exposure (OR = 2.17; 95% CI: 1.68–2.79) have two times higher risk of death from COVID-19, while the risk is thirteen times higher with the comorbid condition “cardiovascular disease” (OR = 13.6; 95% CI: 10.3–17.9).
Table II.
COVID-19 patients: China 2020. Statistically significant predictors of death from COVID-19 using multivariate logistic regression
| Parameter | Confirmed cases | Dead | Alive | Odds ratio (95% CI) | P-value |
|---|---|---|---|---|---|
| Gender: | < 0.05 | ||||
| Male | 22981 | 653 | 22.328 | 1.68 (1.48–1.91) | |
| Female | 21691 | 370 | 21.321 | 1.00 | |
| Age: | < 0.05 | ||||
| ≥ 80 | 1408 | 208 | 1.200 | 94.9 (13.2–679.2) | |
| 70–79 | 3918 | 312 | 3.606 | 47.4 (6.6–338.3) | |
| 60–69 | 8583 | 309 | 8.274 | 20.4 (2.8–146.0) | |
| 50–59 | 10008 | 130 | 9.878 | 7.2 (1.01–51.6) | |
| 40–49 | 8571 | 38 | 8.533 | 2.4 (0.3–17.8) | |
| 30–39 | 7600 | 18 | 7.582 | 1.3 (0.1–9.7) | |
| 20–29 | 3619 | 7 | 3.612 | 1.0 (0.1–8.6) | |
| 10–19 | 549 | 1 | 548 | 1.00 | |
| Occupation: | < 0.05 | ||||
| Service industry | 3449 | 23 | 3.426 | 0.35 (0.23–0.53) | |
| Farmer/laborer | 9811 | 139 | 9.672 | 0.75 (0.61–0.91) | |
| Health worker | 1.716 | 5 | 1.711 | 0.15 (0.06–0.37) | |
| Retiree | 9.193 | 472 | 8.721 | 2.83 (2.47–3.25) | |
| Other/none | 20503 | 384 | 20.119 | 1.00 | |
| Province: | < 0.05 | ||||
| Hubei | 33367 | 979 | 32.388 | 7.73 (5.71–10.47) | |
| Other | 11305 | 44 | 11.261 | 1.00 | |
| Wuhan-related exposure: | < 0.05 | ||||
| Yes | 31974 | 853 | 31.121 | 2.17 (1.68–2.79) | |
| No | 5.295 | 66 | 5.229 | 1.00 | |
| Comorbid condition: | < 0.05 | ||||
| Hypertension | 2683 | 161 | 2.522 | 7.3 (5.8–9.3) | |
| Diabetes | 1102 | 80 | 1.022 | 9.0 (6.8–12.0) | |
| Cardiovascular disease | 873 | 92 | 781 | 13.6 (10.3–17.9) | |
| Chronic respiratory disease | 511 | 32 | 479 | 7.7 (5.2–11.5) | |
| Cancer (any) | 107 | 6 | 101 | 6.8 (2.9–15.9) | |
| None | 15.536 | 133 | 15.403 | 1.00 | |
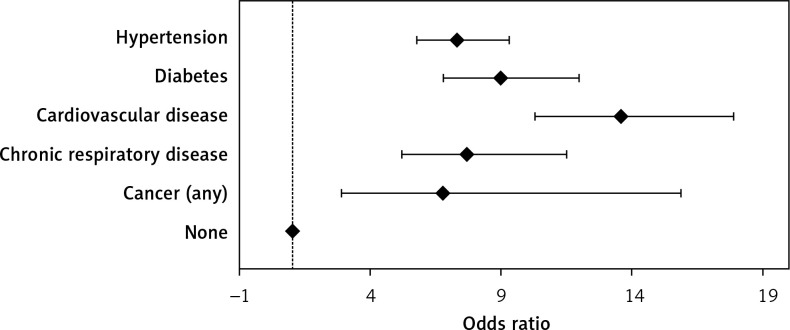
Figure 1 shows the underlying diseases with the odds ratios for the risk of death from COVID-19 in China. As can be seen, cardiovascular disease ranks first, followed by diabetes, chronic respiratory disease, hypertension, and cancer.
Figure 1.
Underlying diseases with the odds ratios for death risk from COVID-19 in China during the period 2012–2018
Discussion
Greater focus should be given to the prognostic factors that had the highest odds ratio. It is noted that the characteristic of patients with the highest risk of death from COVID-19 is age and more specifically, it was found that the age group of 50–59 has seven times higher risk than younger ages, while the risk is significantly higher as age increases. Moreover, comorbid conditions play a crucial role in this type of disease. Individuals with cardiovascular disease have a thirteen-fold increased death risk compared to those without underlying diseases. Finally, the death risk is nine times higher with the comorbid condition diabetes and eight times higher with chronic respiratory disease, while the risk is seven times higher for those who have hypertension and cancer.
This study’s importance lies in the emergence of cardiovascular disease as a primary risk factor for death from COVID-19. The underlying mechanism in which COVID-19 is associated with cardiovascular disease is uncertain. Prior studies have reported that SARS-CoV-2 infects host cells through angiotensin-converting enzyme 2 (ACE2) to cause COVID-19, and also causes damage to the myocardium [18, 19]. The current uncertainty about the exact mechanisms by which COVID-19 causes severe clinical complications, and possibly death, makes it difficult for physicians to administer optimal therapeutic regimens [20–22].
There are two major limitations in this study that could be addressed in future research. First, the study focused on data from only one country, compared to the major geographic area this pandemic affected. Second, the duration of the study of this new virus is very short, which is a barrier in drawing safe conclusions.
In conclusion, this paper highlights the statistically significant characteristics of COVID-19-associated deaths in China. Moreover, the results of this study describe for the first time the importance of cardiovascular disease as a primary prognostic risk factor for death from coronavirus disease 2019.
Conflic of interest
The author declares no conflict of interest.
References
- 1.Velavan TP, Meyer CG. The Covid-19 epidemic. Tropical Med Int Health. 2020;25:278–80. doi: 10.1111/tmi.13383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tan W, Zhao X, Ma X, et al. Notes from the field: a novel coronavirus genome identified in a cluster of pneumonia cases – Wuhan, China 2019–2020. China CDC Weekly. 2020;2:61–2. [PMC free article] [PubMed] [Google Scholar]
- 3.Na Z, Ding Z, Wen W, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–605. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen Y, Liu Q, Guo D. Emerging coronaviruses: genome structure, replication, and pathogenesis. J Med Virol. 2020;92:418–23. doi: 10.1002/jmv.25681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Coronavirus disease (COVID-19) outbreak. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed Mar 13, 2020)
- 6.Na Z, Ding Z, Wen W, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–605. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395:514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. medRxiv. 2020 2020.02.06.20020974. [Google Scholar]
- 9.Rothe C, Schunk M, Sothmann P, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382:970–1. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chan JF, Kok KH, Zhu Z, et al. Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9:221–36. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richardson P, Griffin I, Tucker C, et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395:e30–1. doi: 10.1016/S0140-6736(20)30304-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Holshue ML, DeBolt C, Lindquist S, et al. Novel coronavirus in the United States. N Engl J Med. 2020;382:929–36. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang M, Cao R, Zhang L, et al. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–71. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO Coronavirus disease (COVID-19) situation reports. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed Mar 13, 2020)
- 17.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) – China, 2020. China CDC Weekly. 2020;2:113–22. [PMC free article] [PubMed] [Google Scholar]
- 18.Turner AJ, Hiscox JA, Hooper NM. ACE2: from vasopeptidase to SARS virus receptor. Trends Pharmacol Sci. 2004;25:291–4. doi: 10.1016/j.tips.2004.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zheng Y, Ma Y, Zhang J, et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–60. doi: 10.1038/s41569-020-0360-5. published online March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katsiki N, Banach M, Mikhailidis DP. Lipid-lowering therapy and renin-angiotensin-aldosterone system inhibitors in the era of the COVID-19 pandemic. Arch Med Sci. 2020;16:485–9. doi: 10.5114/aoms.2020.94503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iaccarino G, Borghi C, Cicero AFG, et al. Renin-angiotensin system inhibition in cardiovascular patients at the time of COVID19: much ado for nothing? A statement of activity from the directors of the board and the scientific directors of the Italian Society of Hypertension. High Blood Press Cardiovasc Prev. 2020;27:105–8. doi: 10.1007/s40292-020-00380-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Azeez SA, Ghalib Alhashim Z, Al Otaibi W, et al. State-of-the-art tools to identify druggable protein ligand of SARS-CoV-2. Arch Med Sci. 2020;16:497–507. doi: 10.5114/aoms.2020.94046. [DOI] [PMC free article] [PubMed] [Google Scholar]