An entity related to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection associated with a multisystem inflammatory state in children (MIS-C) and acute heart failure has been described.1 Early treatment of MIS-C has mimicked that of Kawasaki disease with the use of intravenous immunoglobulin (IVIG) and other anti-inflammatory agents.1–3 This strategy seems to be effective because the outcomes are usually favorable with a very limited number of fatalities.1,3 Yet, there is no consensus or evidence for the optimal treatment strategy in MIS-C, and the effect of treatment strategies on the recovery of cardiac function has not been yet described.
We report the evolution of cardiac function in children admitted at our institution for MIS-C, defined by persistent fever (>38.5 °C) for >3 days, multiorgan involvement, evidence for coagulopathy (D-dimers>1000 ng/mL), inflammation (C-reactive protein>80 mg/L), and positive antibody assays for SARS-CoV-2 infection. Three clinical criteria among the following had to be observed to define multiorgan involvement in this series: cervical lymphadenopathy, bulbar conjunctivitis, skin rash, erythema of oral and pharyngeal mucosa, gastrointestinal symptoms, asthenia, respiratory signs, heart failure, or cardiogenic shock.
Median age was 8.6 years (interquartile range [IQR], 6.7–11.2). The median delay between symptom onset and hospital admission was 4 days and was stable over the study period. All patients had positive assays for SARS-CoV-2 antibodies. Echocardiographic monitoring was regularly performed from admission to discharge. Eighteen patients admitted before May 1, 2020, received IVIG (2g/kg once) as first-line treatment, and the 22 patients admitted after this date received a combination of IVIG and intravenous methylprednisolone (0.8 mg·kg–1·d–1 for 5 days). These 2 populations had similar clinical, cardiac, and biological characteristics at baseline. The study was approved by the local ethics committee that waived the need for parental informed consent (authorization number: MR004: 2020–0505172058).
The cumulative incidence to recovery defined as left ventricle ejection fraction [LVEF] >55% for systolic function and isovolumic relaxation time (IVRT) >90 ms for diastolic function was calculated using the Kaplan-Meier approach (IBM SPSS version 23 statistical software).
At the time of admission, LVEF was <55% in 77.5% of patients with a median LVEF of 48% (IQR, 39–54), whereas median left ventricle end-diastolic dimension z score was normal (0.8 [IQR, 0.06–1.7]). Cardiac index was normal in most patients with a high proportion having low systolic blood pressure and tachycardia. Left ventricular diastolic dysfunction assessed by shortening of IVRT was observed in all patients during the first week after admission (median, 60 ms [IQR, 48–70]).
Median time to recovery of LVEF (>55%) was 4 days (IQR, 2–6), and median time to recovery of IVRT (>90 ms) was 7 days (IQR, 4–17). The main finding was the reduction of time to recovery of LVEF and IVRT, and pediatric intensive care unit stay in the group receiving a combination of IVIG and steroids in comparison with the group receiving only IVIG, respectively, 2.9 versus 5.4 days, 6.4 versus 20.6 days, and 3.4 versus 5.3 days (P<0.05) (Figure). Left main coronary artery zscore was 0 (IQR, –0.7 to 0.6) at baseline and –0.5 (IQR, –1.3 to 0) at discharge without significant differences between the groups.
Figure.
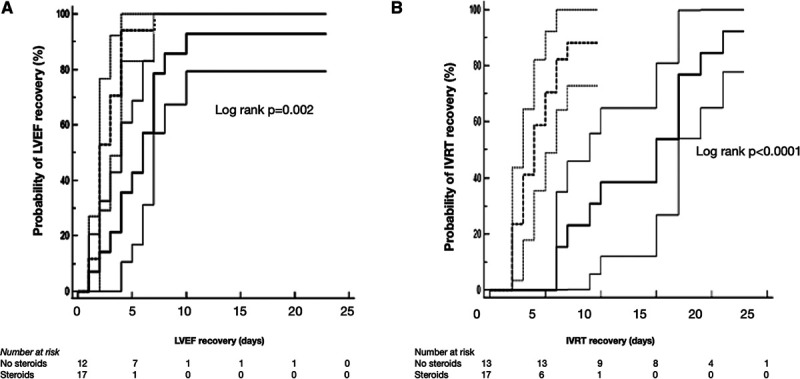
Kaplan-Meier recovery curves, along with the 95% confidence interval for patients who received intravenous immunoglobulin and steroid treatment (dashed line) versus those who were treated with intravenous immunoglobulin only (full line). A, LVEF recovery. (Only 29 of 40 patients who had LVEF<55% at admission were included in this analysis.) B, IVRT recovery. (IVRT was measured at admission in 30 of 40 patients who all had sequential evaluations.) IVRT indicates isovolumic relaxation time; and LVEF, left ventricular ejection fraction.
Acute left ventricular systolic and diastolic dysfunction are prominent findings in MIS-C. All recent reports show that B-type natriuretic peptide or N-terminal pro B-type natriuretic peptide levels are very high, whereas troponin elevation is usually mild to moderate.1,3 Together with the rapid recovery of cardiac function, these findings are in favor of myocardial stunning rather than myocarditis in MIS-C. A recent cardiac magnetic resonance study in patients with MIS-C reported evidence of myocardial edema with no late gadolinium enhancement that would be suggestive of necrosis.4
Patients with MIS-C appear to be responsive to IVIG.1,3 Still, there is no direct evidence that IVIG improves outcomes in MIS-C2 or that an adjunct of other anti-inflammatory agents is effective. To resolve the severe inflammatory state associated with MIS-C, some children have been successfully treated with steroids, anakinra, an interleukin-1 receptor antagonist, or with infliximab.1,3 During the second period of our series, we added steroids to target systemic inflammation and reduce cytokine storm. Recent data suggest some benefit of corticosteroid therapy in the treatment of inflammatory lung complications of coronavirus disease 2019 (COVID-19), and corticosteroids could play a similar role in other later inflammatory complications of SARS-CoV-2 infection such as MIS-C.5
The major limitation of our study is the absence of randomization, but it was not possible to set up this type of trial in the context of a severe emerging syndrome. Increasing awareness on MIS-C and more standardized management could have influenced outcomes, but the day of admission and cardiac parameters were similar in the 2 study groups.
This observational study suggests that adding corticosteroids to immunoglobulins is associated with a shorter time to recovery of cardiac function in patients with MIS-C. Further evaluation in randomized controlled trials is needed to confirm these findings and to define the optimal treatment strategy in MIS-C.
Disclosures
None.
Footnotes
Drs Houyel and Bonnet are co–senior authors.
Data are available on request.
Contributor Information
Zahra Belhadjer, Email: zahra.belhadjer@aphp.fr.
Johanne Auriau, Email: johanne.auriau@aphp.fr.
Mathilde Méot, Email: mathilde.meot2@aphp.fr.
Mehdi Oualha, Email: mehdi.oualha@aphp.fr.
Sylvain Renolleau, Email: sylvain.renolleau@nck.aphp.fr.
Lucile Houyel, Email: lucile.houyel@aphp.fr.
References
- 1.Belhadjer Z, Méot M, Bajolle F, Khraiche D, Legendre A, Abakka S, Auriau J, Grimaud M, Oualha M, Beghetti M, et al. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation. 2020;142:429–436. doi: 10.1161/CIRCULATIONAHA.120.048360 [DOI] [PubMed] [Google Scholar]
- 2.McCrindle BW, Rowley AH, Newburger JW, Burns JC, Bolger AF, Gewitz M, Baker AL, Jackson MA, Takahashi M, Shah PB, et al. ; American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; and Council on Epidemiology and Prevention. Diagnosis, treatment, and long-term management of Kawasaki disease: a scientific statement for health professionals from the American Heart Association [published correction appears in Circulation. 2019;140:e181–e184]. Circulation. 2017;135:e927–e999 [DOI] [PubMed] [Google Scholar]
- 3.Whittaker E, Bamford A, Kenny J, Kaforou M, Jones CE, Shah P, Ramnarayan P, Fraisse A, Miller O, Davies P, et al. ; PIMS-TS Study Group and EUCLIDS and PERFORM Consortia. Clinical characteristics of 58 children with a pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2. JAMA. 2020;324:259–269. doi: 10.1001/jama.2020.10369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blondiaux E, Parisot P, Redheuil A, Tzaroukian L, Levy Y, Sileo C, Schnuriger A, Lorrot M, Guedj R, Ducou le Pointe H. Cardiac MRI of children with multisystem inflammatory syndrome (MIS-C) associated with COVID-19: case series. Radiology. 2020202288 doi: 10.1148/radiol.2020202288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.RECOVERY Collaborative Group. Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, et al. ; RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19–preliminary report [published online July 17, 2020]. N Engl J Med. doi: 10.1056/NEJMoa2021436 [Google Scholar]


