ABSTRACT
We investigated a multi-family cluster of 22 cases in Jixi, where pre-symptomatic and asymptomatic transmission resulted in at least 41% of household infections of SARS-CoV-2. Our study illustrates the challenge of controlling COVID-19 due to the presence of asymptomatic and pre-symptomatic transmission even when extensive testing and contact tracing are conducted.
KEYWORDS: Asymptomatic transmission, pre-symptomatic transmission, COVID-19, cluster, household close contact, contact tracing
Introduction
A sizeable proportion of COVID-19 cases are asymptomatic, though estimates vary greatly [1–4]. Estimated shorter serial interval of COVID-19 in comparison to its incubation period promotes pre-symptomatic spread of COVID-19 [5,6]. Modelling studies have suggested asymptomatic carriers of SARS-CoV-2 are major contributors in the propagation of COVID-19 [7]. Given the high risk of infection among household close contacts [8], asymptomatic transmission may complicate the control of household transmission. However, case reports showing asymptomatic transmission driving the spread of COVID-19 among household close contacts are still limited. Here we report a multi-family cluster of 22 cases in Jixi, a northern city of China, where pre-symptomatic and asymptomatic cases were key components of the transmission chains.
Materials and methods
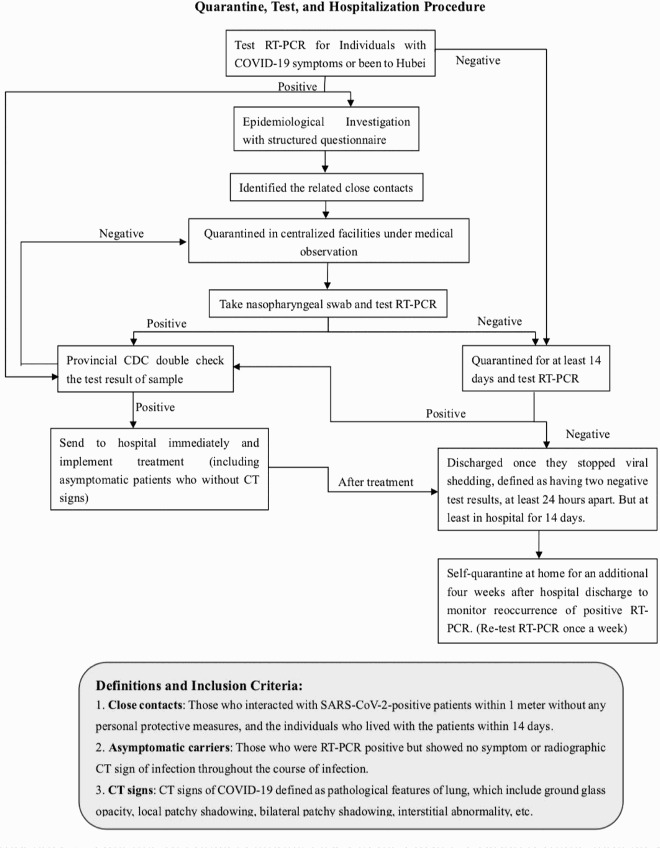
The investigators interviewed patients with positive RT-PCR using a structured questionnaire and collected their demographic information, travelling history, and date of symptom onset within 14 days before confirmation. Questions on travel history to Wuhan city or Hubei province, contacts with febrile individuals, and visits to seafood markets were meant to capture other potential source of infection. Close contacts were individuals who lived with a PCR-confirmed case or interacted with a case within 1 meter from the case without any personal protections. All close contacts were quarantined in centralized facilities and were tested by RT-PCR. Positive cases with and without symptoms were immediately sent to hospitals for treatment after results were verified by provincial CDC. We defined those who were RT-PCR positive but showed no symptom or radiographic CT sign of infection throughout the course of infection as asymptomatic carriers. CT signs of SARS-CoV-2 infection included ground glass opacity, local patchy shadowing, bilateral patchy shadowing, and interstitial abnormality. All RT-PCR positive patients were isolated in the hospital for at least 14 days and were discharged once they stopped viral shedding. Those with negative results continued to be quarantined and were released once they had two negative test results, at least 24 hours apart (Appendix 1).
Results
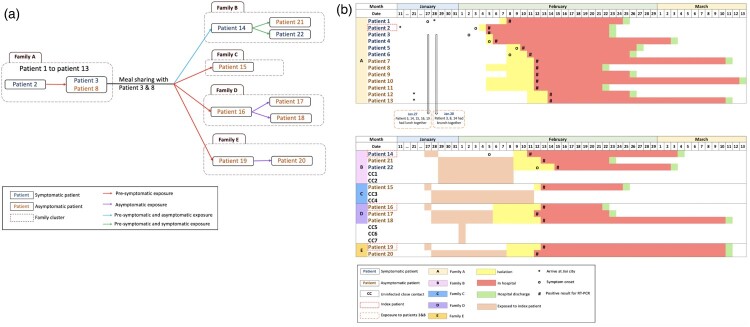
On February 5 2020, the Jixi City Centre for Disease Control (Jixi CDC) in Heilongjiang province was notified of the first two cases (patient 2 and patient 3) diagnosed with COVID-19 in Jixi by a local hospital. After detailed epidemiological investigations of 93 close contacts, Jixi CDC identified a large cluster of 22 COVID-19 confirmed cases from 5 families, including 8 symptomatic and 14 asymptomatic cases. The outbreak first started and propagated in family A over a series of family gatherings and subsequently spread to four other families through pre-symptomatic or asymptomatic transmission (Figure 1(A)).
Figure 1.
Transmission chain of 22 COVID-19 cases associated with a multi-family cluster. (A) Family structure and transmission chains linking all 22 infected patients in the cluster. (B) Duration of exposure to index case, dates of symptom onset, duration of isolation, hospitalization for all close contacts of patients 14, 15, 16, and 19 outside of family A. Exposure history in family A were not presented because of heavily overlapping contact history between cases.
Family A
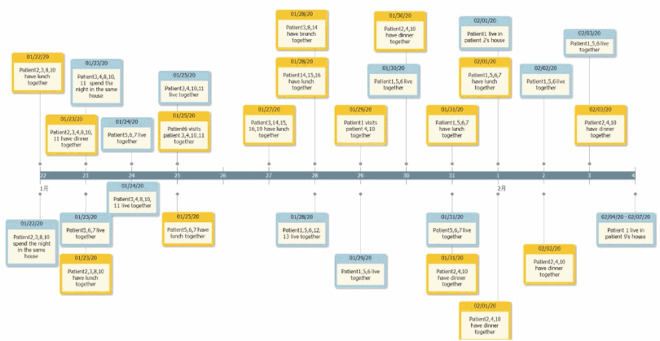
Between January 22 and February 4, the 14-day period before case 2 was confirmed, Jixi CDC identified 25 people who participated in family A’s 30 gatherings (Appendix 1), and 13 of them (52%) were infected. Of the 13 infected family members, six were symptomatic (patients 1–6) and seven were asymptomatic (patients 7–13). However, the heavily overlapping contact history made it impossible to tease apart distinct transmission chains within family A (Appendix 2). Nevertheless, Jixi CDC considered patient 2 the most probable index case of the cluster after analysing possible transmission chains that resulted in the infection of the four index cases outside of family A. On January 27 and 28, the four index cases outside of family A shared meals with patients 3 and 8 from family A. Since patients 3 and 8 were their only possible source of infection, and patients 3 and 8 did not interact with any other cases with a travel history in family A before January 27 except for patient 2 (Figure 1), patient 2 was considered the most probable index case of the cluster.
The four index patients in families B to E were most likely infected either by a pre-symptomatic case (patient 3) about five days before patient 3’s symptom onset or by an asymptomatic carrier (patient 8). Except for patient 15 who did not infect her close contacts, the other three cases subsequently infected five of their household close contacts. Out of the nine patients who were infected outside of family A, seven were asymptomatic (Figure 1(B)).
Family B
Patient 14 (50, female), the index case in family B, subsequently exposed four household members for 11 days after sharing meals with patients 3 and 8 on January 27 and 28. She felt eye discomfort on February 5 and was isolated four days after. Two of her household close contacts (patient 21 and 22) were tested positive, of whom patient 21 was asymptomatic and patient 22 had symptom onset on February 12, seven days after the index case (patient 14)’s symptom onset date. Patient 14 experienced viral shedding for at least 23 days.
Family D
Patient 16 (52, male), the index case in family D, infected his wife (patient 18) and daughter (patient 17) who all lived together between January 28 and February 5. They did not interact with any other known patients diagnosed with COVID-19. All three of them were asymptomatic. The other three contacts who were only exposed to the index case for an hour were not infected.
Family E
Patient 19 (50, female), the index case in family E, infected her husband (patient 20). The couple shared meals and lived together for 11 days from January 28 to February 7. They were both asymptomatic and had viral shedding for at least a month.
Discussion
In summary, this investigation identified a large cluster of 22 confirmed COVID-19 cases from 5 families, among whom 14 (64%) were asymptomatic. These asymptomatic cases in our study represent 61% (14 of 23) of asymptomatic patients in Jixi. Pre-symptomatic or asymptomatic transmission was responsible for at least 41% of infections whose transmission chains can be identified (9/22) (Figure 1(A)). Duration of viral shedding, defined as time of first positive RT-PCR test to hospital discharge after consecutively tested negative by RT–PCR twice, ranged from 9 days to 29 days, with a median of 17.5 days (range 15–26) for all symptomatic cases and 12.5 days (range 9–29) for asymptomatic cases.
This cluster investigation has at least two limitations. First, due to the lack of serological testing and the complexity of this cluster, it is impossible to capture precise transmission chains and rule out the possibility that cases were infected from other unknown sources. Second, there was evidence that multiple introductions of imported cases could have caused infections among members in family A (patient 1 and possibly patients 12 and 13).
This multi-family cluster presented additional evidence that asymptomatic and pre-asymptomatic cases can play a key role in silent household transmission of COVID-19. Extensively testing and isolating close contacts of confirmed cases reduced onward transmission. Early diagnosis and treatment may have also reduced duration of viral shedding [9]. Our investigation that was conducted outside of COVID-19 epicentres provided a snapshot of the possible scale of undetected asymptomatic transmission in epicentres of COVID-19 pandemic. Our results highlighted the important role of asymptomatic and pre-symptomatic cases in estimating the burden of COVID-19 pandemic. Extensive laboratory testing among close contacts can identify cases at early phase of infection and prevent onward transmission, and it is key to an effective COVID-19 surveillance programme.
Supplementary Material
Acknowledgements
We thank the investigators of the Jixi CDC who collected these important epidemiological investigation reports. We thank all patients, close contacts, and their families involved in the study, as well as the cooperative front-line medical staff and public health workers.
Appendices.
Appendix 1. The quarantine, test and hospitalization procedures, and the related definitions.
Appendix 2. Timeline of contacts among cases in the cluster. Coloured frame indicates types of contact, orange for meal sharing and blue for living in the same household.
Funding Statement
This work was supported by Emergency Program for COVID-19 Prevention and Control of Guangdong Province: [Grant Number 2020KZDZX1226]; Emergency Response Program of Peng Cheng Laboratory: [Grant Number PCLERP001].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Bai Y, Yao L, Wei T, et al. . Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 Feb 21; 323(14):1406–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heneghan C, Brassey J, Jefferson T. COVID-19: What proportion are asymptomatic? [Online]. CEBM,The Centre for Evidence-Based Medicine. Available: https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/.
- 3.Mizumoto K, Kagaya K, Zarebski A, et al. . Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 2020;25(10):2000180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nishiura H, Kobayashi T, Miyama T, et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). medRxiv. 2020 Jan 1. Available from: 10.1101/2020.02.03.20020248. [DOI] [PMC free article] [PubMed]
- 5.Tindale L, Coombe M, Stockdale JE, et al. Transmission interval estimates suggest pre-symptomatic spread of COVID-19. MedRxiv. 2020 Jan 1. Available from: 10.1101/2020.03.03.20029983. [DOI]
- 6.He X, Lau EH, Wu P, et al. Temporal dynamics in viral shedding. and transmissibility of COVID-19. Nature medicine. 2020 Apr 15:1-4. [DOI] [PubMed]
- 7.Li R, Pei S, Chen B, et al. . Substantial undocumented infection. facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020 May 1;368(6490):489–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bi Q, Wu Y, Mei S, et al. . Epidemiology and transmission of. COVID-19 in Shenzhen China: Analysis of 391.cases and 1,286 of their close contacts. Lancet Infect Dis. 2020 Aug;20(8):911–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hung I, Lung K, Tso E, et al. . Triple combination of interferon beta-1b, lopinavir–ritonavir, and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. The Lancet. 2020 May 30–Jun 5;395(10238):1695–1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.