Abstract
Objective
To evaluate the long-term functional outcome of interhospital transfer of patients with stroke with suspected large vessel occlusion (LVO) using Helicopter Emergency Medical Services (HEMS).
Methods
Records of consecutive patients evaluated through 2 telestroke networks and transferred to thrombectomy-capable stroke centers between March 2017 and March 2018 were reviewed. Inverse probability of treatment weighting (IPTW) using the propensity score was performed to address confounding factors. Multivariate logistic regression analysis with IPTW was used to determine whether HEMS were associated with good long-term functional outcome (modified Rankin scale score ≤ 2).
Results
A total of 199 patients were included; median age was 67 years (interquartile range [IQR] 55–79 years), 90 (45.2%) were female, 120 (60.3%) were white, and 100 (50.3%) were transferred by HEMS. No significant differences between the 2 groups were found in mean age, sex, race, IV tissue plasminogen activator (tPA) receipt, and thrombectomy receipt. The median baseline NIH Stroke Scale score was 14 (IQR 9–18) in the helicopter group vs 11 (IQR 6–18) for patients transferred by ground (p = 0.039). The median transportation time was 60 minutes (IQR 49–70 minutes) by HEMS and 84 minutes (IQR 25–102 minutes) by ground (p < 0.001). After weighting baseline characteristics, the use of HEMS was associated with higher odds of good long-term outcome (OR 4.738, 95% CI 2.15–10.444, p < 0.001) controlling for transportation time, door-in-door-out time, and thrombectomy and tPA receipt. The magnitude of the HEMS effect was larger in thrombectomy patients who had successful recanalization (OR 1.758, 95% CI 1.178–2.512, p = 0.027).
Conclusions
HEMS use was associated with better long-term functional outcome in patients with suspected LVO, independently of transportation time.
The expansion of telestroke networks has helped patients in rural community hospitals gain access to expert stroke management.1–3 However, interhospital transfer to a thrombectomy-capable stroke center (TSC) continues to play a crucial rule in the care process of stroke patients with suspected large vessel occlusion (LVO). One of the important decisions to be made by the telestroke consultant is whether to recommend air or ground transportation. Helicopter Emergency Medical Services (HEMS) are commonly used, given the shorter transportation times in different scenarios.4 However, HEMS are more expensive, and it is uncertain whether it results in better outcomes.5 Furthermore, HEMS have not been shown to result in a higher likelihood of receiving mechanical thrombectomy (MT),6 and the effect of the physical factors present in the helicopter on ischemia and reperfusion is uncertain.4 Therefore, we sought to examine the effect of mode of transportation and transportation time on the long-term functional outcomes across 2 large telestroke networks.
Methods
This was a retrospective cohort study using 2 telestroke networks of 2 TSCs located in the southeastern United States (the Medical University of South Carolina and the Medical College of Georgia at Augusta University). The clinical and operational outcomes of the spoke-and-hub telestroke networks of both centers were previously described.7–9 Both networks adopted clinical suspicion for acute LVO as the main criterion for transfer to the TSC with or without radiographic evidence of LVO. Patients with acute stroke with cortical signs on the neurologic examination during video telestroke consult within 24 hours of symptom onset and who do not have a contraindication for MT are transferred to the TSC hub for thrombectomy evaluation. Transportation can be done using HEMS or ground ambulance based on the assessment of the telestroke provider, and the spoke physician, and the availability of the transportation mode. On arrival to the TSC, patients undergo noncontrasted CT of the head in addition to CT angiography (CTA) of the head and neck and CT perfusion (if available). Patients with LVO on CTA who met either of the following criteria underwent MT:
Alberta Stroke Program Early CT (ASPECT) score ≥6.
≥50% mismatch between the area of relative decreased cerebral blood volume and area of relative decreased mean transit time or Tmax with a core volume <1/3–1/2 of the total occluded vessel territory on CT perfusion. CT perfusion criteria did not involve automated software to assess the perfusion mismatch, and it was used (when available) for patients with ASPECT score ≤5.
We identified all consecutive patients who were seen through both telestroke networks from March 2017 through March 2018. Included patients received a telestroke consultation and were transferred to a TSC for MT candidacy evaluation. The following data were collected from the charts: age, race, sex, stroke severity on admission measured by the NIH stroke scale (NIHSS), receipt of IV tissue plasminogen activator (tPA) at spoke sites, door to needle time, transportation mode (air or ground), the distance between the spoke site and TSC, receipt of thrombectomy at TSCs, door to groin time, and modified treatment in cerebral infarction (mTICI) score. Successful recanalization was defined by achieving final mTICI ≥ 2b. The driving distance from the TSC was calculated using Google Maps (Google, CA) for ground ambulances. The straight line was also measured by Google Maps for HEMS. In addition, we collected last known normal (LKN) to spoke door time and door-in to door-out (DIDO) time at spoke sites in addition to the transportation time between spoke sites and TSCs. Outcome measures used were the 90-day modified Rankin scale (mRS) score and the length of hospitalization. Good long-term functional outcome was defined by functional independence (mRS score ≤2) at 90 days.
One of the important decisions to be made by the telestroke consultant is whether to recommend air or ground transportation.
Statistical analysis
Descriptive statistics were used to report patient demographic and clinical characteristics using median and interquartile range (IQR) for continuous variables and percentages for categorical variables. Characteristics of both groups (HEMS and ground transportation) were compared using the Wilcoxon rank-sum (Mann-Whitney) test and χ2 as appropriate. An alpha level of 0.05 was used as the level of statistical significance. We assessed the predictors of receiving MT at a TSC using multivariate logistic regression model controlling for age, sex, race, baseline NIHSS, tPA receipt, DIDO time, transportation time, and mode of transportation. We estimated a generalized linear regression model using gamma distribution and a logit link to predict the time of transportation as a function of air transportation controlling for transportation distance in miles.
To determine whether HEMS transportation was associated with good long-term functional outcome, logistic regression model was used controlling for transportation time, DIDO time, and thrombectomy and tPA receipt. Because the decision of choosing HEMS transportation or ground ambulance could be affected by some of the same factors that affect the outcome, the logistic regression model was derived with inverse probability of treatment weight (IPTW) using propensity scores. The propensity scores were calculated using a binary logistic regression model for transportation method adjusting for age, sex, race, LKN to spoke time, and baseline NIHSS. Covariates in the propensity score model that have a less than 0.20 standardized difference before and after weighting were considered well matched. The same logistic regression model (after excluding thrombectomy as a predictor) with IPTW using propensity score analysis was applied to thrombectomy patients who achieved successful recanalization in a separate analysis. Final models were tested for collinearity. The analysis was conducted using SPSS v25 (IBM Corporation, New York, NY).
Standard protocol approvals, registrations, and patient consents
This study is an observational minimal risk study, and no consent is required per the Medical University of South Carolina and Augusta University institutional policy. Our study was approved by the institutional review board in both institutions.
Data availability
Anonymized data not published within this article will be made available by request from any qualified investigator. Investigators interested in working with the data should contact the corresponding author.
Results
Included patients
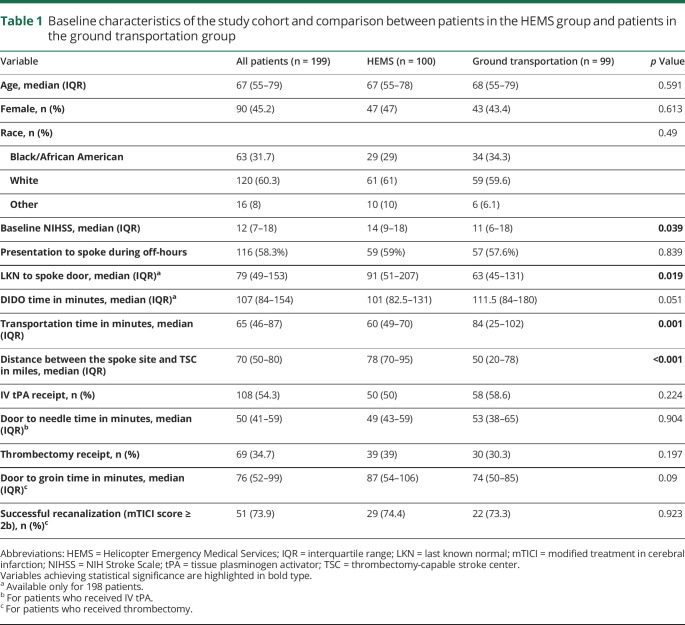
During the 1-year study period, a total of 210 consecutive patients met the study criteria. Eleven patients were excluded because of insufficient data in charts, resulting in a final sample of 199 patients. In the included patients, median age was 67 years (IQR 55–79 years), 90 (45.2%) patients were female, 120 (60.3%) patients were white, and 100 (50.3%) patients were transferred by HEMS. The median NIHSS score on presentation was 12 (IQR 7–18), and 108 (54.3%) patients received IV tPA at spoke sites before transfer. Sixty-nine (34.7%) patients received MT on arrival to the TSC. The most common reason for not undergoing MT was the absence of LVO in 76 (58.5%) patients, followed by low ASPECT or unfavorable perfusion profile in 42 (32.3%) on imaging studies on arrival to the TSC. In addition, 12 (9.2%) patients did not receive MT because of rapid improvement of symptoms on arrival to the TSC. The median DIDO time was 107 minutes (IQR 84–154 minutes). The median transportation time was 65 (IQR 46–87) minutes. The unadjusted patients' characteristics are summarized in table 1.
Table 1.
Baseline characteristics of the study cohort and comparison between patients in the HEMS group and patients in the ground transportation group
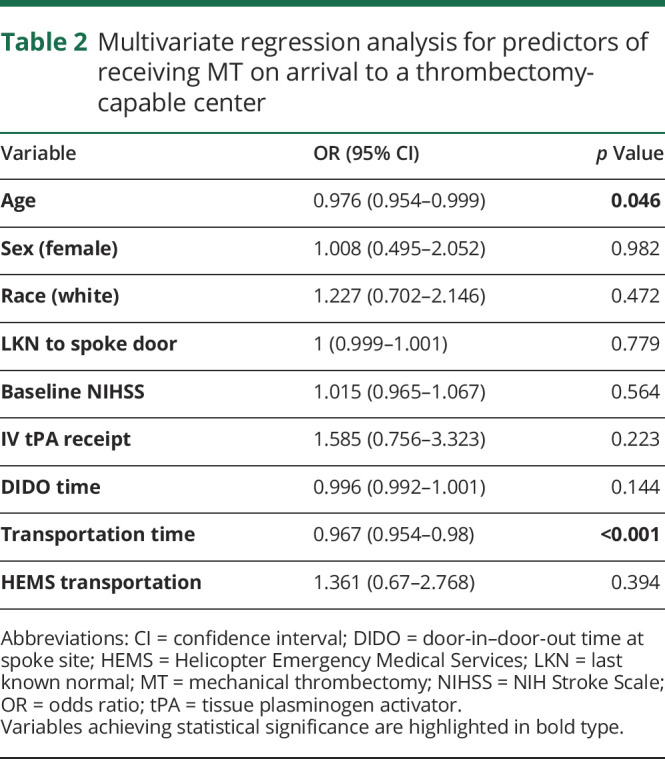
The median transportation time was 50 minutes (IQR 15–64 minutes) for patients who underwent MT and 72 minutes (IQR 54–96 minutes) for patients who did not receive MT (p < 0.001). Using logistic regression analysis, transportation time was an independent predictor for receiving MT (OR 0.967, 95% CI 0.954–0.98, p < 0.001). Although HEMS resulted in shorter transportation times, this mode of transportation did not independently predict MT receipt (p = 0.394), as shown in table 2.
Table 2.
Multivariate regression analysis for predictors of receiving MT on arrival to a thrombectomy-capable center
HEMS vs ground ambulances
No significant difference was found in mean age, sex, race, IV alteplase receipt, and thrombectomy receipt between both groups (table 1). None of the transported patients had direct complication related to the transportation. The median baseline NIHSS score was 14 (IQR 9–18) in the helicopter group vs 11 (IQR 6–18) for patients transferred by ground (p = 0.039). The median transportation time when helicopter transportation was used was 60 minutes (IQR 49–70 minutes) and 84 minutes (IQR 25–102 minutes) when ground transportation was used (p = 0.001). The median distance to the TSC was greater for patients transported by HEMS than by ground, 78 vs 50 miles, respectively (p < 0.001). Controlling for distance traveled, the transportation time is predicted to be 38.4 minutes (95% CI 15.7–61.2) shorter for patients who were transferred by HEMS (p = 0.001).
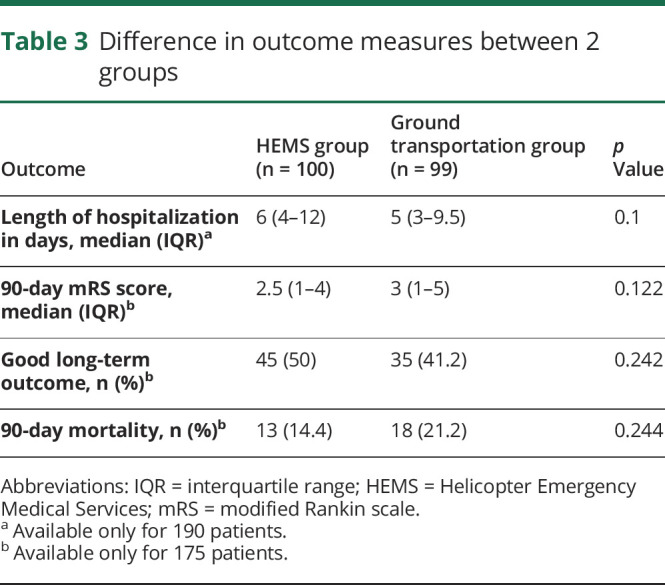
Patients who were transferred by HEMS had a median length of hospitalization of 6 days (IQR 4–12 days) compared with 5 days (IQR 3–9.5 days) for patients in the ground transportation group (p = 0.1). On univariate analysis, there was no association between good long-term functional outcome or 90-day mortality and the mode of transportation (90-day mRS score ≤2: 50% in the HEMS group and 41.2% in the ground transportation group, p = 0.242; 90-day mortality: 14.4% in the HEMS group and 21.2% in the ground transportation group, p = 0.244) (table 3).
Table 3.
Difference in outcome measures between 2 groups
On multivariate analysis using logistic regression model with IPTW and propensity score, HEMS was associated with better long-term outcome (OR 4.738, 95% CI 2.15–10.444, p < 0.001) (table 4). Additional independent predictors of good long-term outcome included tPA receipt (OR 2.57, 95% CI 1.491–4.612, p = 0.018), and transportation time (OR 0.986, 95% CI 0.978–0.995, p = 0.002).
Table 4.
Logistic regression analysis for good functional outcome at 90-day (mRS ≤ 2) using the inverse probability of treatment weights
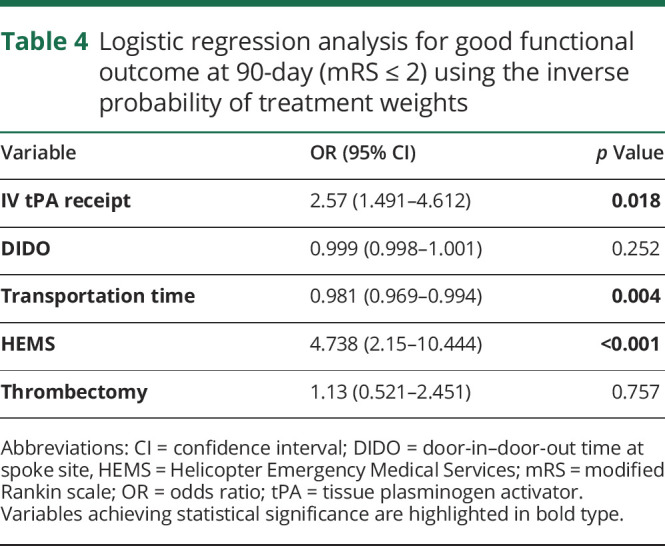
On sensitivity analysis for successful recanalization in thrombectomy patients, HEMS continued to be a strong predictor of good outcome independent of transportation time, DIDO time, and tPA receipt (OR 1.758, 95% CI 1.178–2.512, p = 0.027).
Discussion
In this dual-center study, we found that telestroke patients with a suspected LVO who were transferred to a TSC using HEMS had better long-term functional outcome than patients who were transferred by a ground ambulance after adjusting for confounders, including the transport time or the use of tPA. As expected, we found that HEMS is faster than ground ambulances, which accords with previous studies that reported shorter transportation times using a helicopter.5,10 Still, the observed benefit of HEMS could not be explained only by a shorter transportation time, especially in MT patients who had successful recanalization. We found no differences in the baseline characteristics or in the use of IV tPA or MT between both modes of transportation, which leaves only 2 potential explanations for the benefit of HEMS: differences in the quality of ancillary care during transportation, an intrinsic beneficial effect of the flight itself, or both.
Ancillary care is an important factor that is known to influence stroke outcomes.11,12 The ancillary care in HEMS is presumably better than in ground ambulances given the difference of expertise between the 2 modes of transportation. HEMS are typically staffed by a small cadre of highly trained paramedics and nurses with critical care expertise.13–15 This is especially important for patients with LVO who require strict blood pressure management. In contrast, ground ambulances are usually staffed with emergency medical technicians who usually have lesser level of expertise and training.16–18 This is particularly crucial in rural areas where the ground ambulances are often staffed by volunteer firefighters.18
Another intriguing possibility is the potential beneficial effect of HEMS on maintaining the collateral flow and “freezing the penumbra.” Given that the effect of HEMS in our study was related to the transportation mode itself independent of time of transportation and receiving MT, we speculate that the complex physiologic environment in HEMS may play a role in augmenting the collateral flow before MT which may, theoretically, result in better outcomes following the procedure.19 In addition, low-frequency (50 Hz) vibrations during HEMS20,21 might have thrombolytic properties that enhance the efficacy of IV tPA, facilitating reperfusion.22
Shorter transportation time was associated with higher odds of receiving MT likely because expedited transport results in higher likelihood of penumbra sustenance.
In our study, we found that shorter transportation time was associated with higher odds of receiving MT likely because expedited transport results in higher likelihood of penumbra sustenance. These findings are consistent with a previous study, which reported that the odds of receiving intra-arterial therapy decrease by 2.5% for each minute of delay during transfer.23 Another study by Regenhardt et al.6 found that the probability of receiving MT decreases by 1% for each additional minute of transfer after 60 minutes. However, the authors were unable to find an association between the transportation time and the 90-day mRS score, likely because the 90-day mRS score was available only for patients who received MT in their study.6
Safety of air transportation in acute stroke setting has been assessed before, especially for patients who received IV tPA before transfer. In a study that included 122 patients who were transferred following IV tPA administration, there was no difference in the rate of complication by 6 hours, death at 24 hours, intracerebral hemorrhage, length of hospitalization, and 30-day mortality between patients who were transferred by air compared with patients who were transferred by ground.10 However, this study was conducted in a general population of patients with stroke before MT became an established therapy. Also, ground transportation was uniformly provided by the Mayo ground ambulance system, which might have a higher standard than the emergency ground services available in other rural areas.
The optimal protocol to screen patients with stroke symptoms at telestroke spokes to be transferred to a TSC has not been established yet. On the one hand, doing CTA before transfer can ensure that only patients with LVO are transferred for thrombectomy evaluation. On the other hand, doing CTA for all patients before transfer may delay transfers by as much as 93 minutes.8 Most of the patients included in this study did not have CTA performed before transfer, and as a result, a high percentage (65.3%) of the patients who were transferred to a TSC in our study did not receive thrombectomy on arrival.
Our study has a few limitations. First, although the telestroke logs at the included centers are prospectively maintained, the study parameters were reviewed retrospectively. Second, the mode of transportation (HEMS or ground) was determined by multiple factors including the telestroke consultant assessment, the treating spoke physician assessment, weather conditions, and other operational aeronautical factors, which may introduce different confounding factors one of which is the possibility that patients with fewer comorbidities being transferred using HEMS. Finally, the results of the study may not be generalizable to other telestroke networks. However, our study has a few important strengths including the dual-center design, the control for distance for time analysis, and the use of IPTW to address potential selection bias.
This study reports a positive independent association between HEMS use and functional outcomes of patients with acute stroke using the data from 2 large spoke-and-hub telestroke networks. These findings need to be corroborated and further investigated to isolate potential beneficial variables that could be used in the care of patients with stroke in the future.
Appendix. Authors

Study funding
No targeted funding reported.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
TAKE-HOME POINTS
→ Interhospital transfer plays an important role in the care of patients with acute stroke with LVO.
→ Helicopter transportation was associated with shorter transportation time.
→ Patients who were transferred by a helicopter were more likely to have good long-term functional outcome after controlling for transportation time.
References
- 1.Asaithambi G, Castle AL, Sperl MA, et al. The door to needle time metric can be achieved via telestroke. Neurohospitalist 2017;7:188–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Kasab S, Harvey JB, Debenham E, Jones DJ, Turner N, Holmstedt CA. Door to needle time over Telestroke-a comprehensive stroke center experience. Telemed J E Health 2018;24:111–115. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen-Huynh MN, Klingman JG, Avins AL, et al. Novel telestroke Program improves thrombolysis for acute stroke across 21 hospitals of an integrated healthcare system. Stroke 2018;49:133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leira EC, Stilley JD, Schnell T, Audebert HJ, Adams HP. Helicopter transportation in the era of thrombectomy: the next frontier for acute stroke treatment and research. Eur Stroke J 2016;1:171–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reiner-Deitemyer V, Teuschl Y, Matz K, et al. Helicopter transport of stroke patients and its influence on thrombolysis rates: data from the Austrian Stroke Unit Registry. Stroke 2011;42:1295–1300. [DOI] [PubMed] [Google Scholar]
- 6.Regenhardt RW, Mecca AP, Flavin SA, et al. Delays in the air or ground transfer of patients for endovascular thrombectomy. Stroke 2018;49:1419–1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kulcsar M, Gilchrist S, George MG. Improving stroke outcomes in rural areas through telestroke programs: an examination of barriers, facilitators, and state policies. Telemed J E Health 2014;20:3–10. [DOI] [PubMed] [Google Scholar]
- 8.Al Kasab S, Almallouhi E, Harvey J, et al. Door in door out and transportation times in 2 telestroke networks. Neurol Clin Pract 2019;9:41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Almallouhi E, Holmstedt CA, Harvey J, et al. Long-term functional outcome of telestroke patients treated under drip-and-stay paradigm compared with patients treated in a comprehensive stroke center: a single center experience. Telemed J E Health 2019;25:724–729. [DOI] [PubMed] [Google Scholar]
- 10.Olson Michael D, Rabinstein Alejandro A. Does helicopter emergency medical service transfer offer benefit to patients with stroke? Stroke 2012;43:878–880. [DOI] [PubMed] [Google Scholar]
- 11.How do stroke units improve patient outcomes? A collaborative systematic review of the randomized trials. Stroke Unit Trialists Collaboration. Stroke 1997;28:2139–2144. [DOI] [PubMed] [Google Scholar]
- 12.Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev 2013;11:CD000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leira Enrique C, Lamb Diane L, Nugent Andrew S, et al. Feasibility of acute clinical trials during aerial interhospital transfer. Stroke 2006;37:2504–2507. [DOI] [PubMed] [Google Scholar]
- 14.Leira EC, Hess DC, Torner JC, Adams HP Jr. Rural-urban differences in acute stroke management practices: a modifiable disparity. Arch Neurol 2008;65:887–891. [DOI] [PubMed] [Google Scholar]
- 15.Willis S, Dalrymple R. Fundamentals of Paramedic Practice: A Systems Approach. Chichester; Malden: John Wiley & Sons Inc; 2015. [Google Scholar]
- 16.What's the difference between an EMT and a paramedic? [online]. Available at: cpc.mednet.ucla.edu/node/27. Accessed November 4, 2018.
- 17.Paramedics in the United States [online]. Available at: en.wikipedia.org/w/index.php?title=Paramedics_in_the_United_States&oldid=864518729. Accessed November 4, 2018. 18:46 UTC.
- 18.Emergency medical technician [online]. Available at: en.wikipedia.org/w/index.php?title=Emergency_medical_technician&oldid=863066895. Accessed November 4, 2018 18:38 UTC.
- 19.Grissom T. Critical-care air transport: patient flight physiology and organizational considerations. In: Hurd W, Jernigan J, editors. Aeromedical Evacuation. New York: Springer; 2003:111–135. [Google Scholar]
- 20.De Oliveira CG, Nadal J. Transmissibility of helicopter vibration in the spines of pilots in flight. Aviation Space Environ Med 2005;76:576–580. [PubMed] [Google Scholar]
- 21.Carchietti E, Cecchi A, Valent F, Rammer R. Flight vibrations and bleeding in helicoptered patients with pelvic fracture. Air Medical J 2013;32:80–83. [DOI] [PubMed] [Google Scholar]
- 22.Andrew Hoffman HG. Externally applied vibration at 50hz facilitates dissolution of blood clots in-vitro. Am J Biomed Sci 2012;4:274–284. [Google Scholar]
- 23.Prabhakaran S, Ward E, John S, et al. Transfer delay is a major factor limiting the use of intra-arterial treatment in acute ischemic stroke. Stroke 2011;42:1626–1630. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data not published within this article will be made available by request from any qualified investigator. Investigators interested in working with the data should contact the corresponding author.