Abstract
Objective
Coronavirus disease 19 (COVID-19) caused by the highly pathogenic SARS-CoV-2, was first reported from Wuhan, China, in December 2019. The present study assessed possible associations between one-month mortality and demographic data, SpO2, underlying diseases and laboratory findings, in COVID-19 patients. Also, since recent studies on COVID-19, have focused on Neutrophil-to-lymphocyte ratio (NLR) as an independent risk factor of the in-hospital death and a significant prognostic biomarker of outcomes in critically ill patients, in this study, we assessed predictive potential of this factor in terms of one-month mortality.
Methods
Patients admitted to Imam Reza hospital, affiliated to Mashhad University of Medical Sciences, Mashhad, Iran, from March to June 2020, with positive RT-PCR results for SARS-CoV-2, were included in this study. Kaplan-Meier survival analysis and Cox proportional hazard model were used to respectively estimate one-month mortality since admission and determine factors associated with one-month mortality.
Results
In this retrospective cohort study, 219 patients were included (137 men and 82 women (mean age 58.2 ± 16 and 57 ± 17.3 years old, respectively)). Hypertension, ischemic heart disease and diabetes were respectively the most common comorbidities. Among these patients, 63 patients were admitted to the ICU and 31 deaths occurred during one-month follow-up. With respect to mean peripheral capillary oxygen saturation (SpO2), 142 patients had SpO2 ≤ 90%. Based on our analysis, older age and increased Neutrophil-to-lymphocyte ratio (NLR), and White blood cells (WBC) count were associated with increased risk of one-month mortality. Patients with SpO2 ≤ 90% had a 3.8-fold increase in risk of one-month death compared to those with SpO2 > 90%, although the difference did not reach a significant level.
Conclusion
Multivariate analysis introduced age, WBC count, and NLR as predictors of one-month mortality in COVID-19 patients.
Keywords: Coronavirus, COVID-19, Survival
1. Introduction
Severe Acute Respiratory Syndrome Coronavirus 2 (COVID-19) emerged in late December 2019 in Wuhan, China and The World Health Organization, on March 11, 2020, called the outbreak a pandemic [1]. COVID-19 is caused by novel SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) which is a β-coronavirus [2,3] and share similar symptoms such as cough, fever, dyspnea and breathing problems and in severe cases, pneumonia, severe acute respiratory syndrome (SARS), renal failure and death, with SARS-CoV infection [4]. COVID-19 patients may suffer from respiratory distress (as the most characteristic symptom) and spontaneous breathing becomes impossible for most of ICU-admitted patients. Besides, neurological sequelae such as headache, nausea and vomiting were reported [5]. Based on previous reports, 14% of patients showed serious COVID-19-associated pneumonia, one in 20 patients required intensive care [6] and in nearly 66% of severe and critically ill cases, death occurred [3,6,7].
High fatality rates in severely ill patients indicate that in spite of receiving intensive care, death occurs [3,6,7]; besides, fast spread of the disease raises concerns over the need for intensive care that may overwhelm health care system resources [8]. In order to make ideal treatment decisions, prognostic predictors of mortality in patients with COVID-19 should be identified to help in evaluation of the condition severity. Concerning the blood cells, lower WBC (white blood cells) and lymphocytes but higher neutrophil counts were found in COVID-19 patients, compared to the normal range [9,10]. With respect to biochemical indices, in comparison to non-ICU patients, it was found that higher levels of lactate dehydrogenase (LDH) were associated with increased rate of ICU admissions [11]. In case of SARS-infected patients, biochemical analyses showed higher levels of C-reactive protein (CRP), aminotransferase, LDH and creatine kinase [12]. Significantly increased levels of LDH were also shown in COVID-19 patients [13]. In term of patient's age, a report from China revealed a higher risk of severe COVID-19 outcomes and death in elderlies, especially subjects with serious underlying diseases, compared to younger individuals; based on this report, 81% of Chinese cases who had mild conditions and 80% of patients who died due to COVID-19, were > 60 years old [14]. Similarly, a preliminary report (based on data from February 12 to March 16, 2020) from the US showed a high mortality (10–27%) in patients aged ≥85 followed by individuals aged 65–84 years (3–11%) [1].
Bearing in mind the fact that critical care resources are restricted, it is of crucial importance to recognize trustworthy predictors for survival in COVID-19 patients. In this study, we assessed associations between one-month mortality and clinical/demographic/biochemical data, to identify potentially reliable prognostic indicators for the disease, in COVID-19 patients admitted to Imam Reza hospital, Mashhad, Iran, during a 3-month (March to June 2020) period. Particularly, since recent studies on COVID-19, have focused on Neutrophil-to-lymphocyte ratio (NLR) as an independent risk factor of the in-hospital death [15] and a significant prognostic biomarker of outcomes in critically ill patients [16], in this study, we investigated predictive potential of this factor in terms of one-month mortality.
2. Methods
The present retrospective cohort was approved by Ethics committee of Mashhad University of Medical Sciences (approval No. IR.MUMS.REC.1399.202). Data collection was performed based on retrospective medical chart reviews method [17]. Some strategies suggested by Gilbert et al. (1996), were used to achieve a “well-conducted” chart reviews. In this study, 219 individuals (of both sexes) diagnosed with COVID-19 (based on a polymerase chain reaction (PCR) positive test), referring to Imam Reza hospital, affiliated to Mashhad University of Medical Sciences, Mashhad, Iran, from March to June 2020, were included in this study, based on the inclusion criteria.
The inclusion criteria were as follows: (1) being a PCR-confirmed COVID-19 case and (2) being admitted to hospital due to COVID-19. A trained researcher who was blind to the study hypothesis, extracted patients' information from the hospital information system (HIS) and completed a checklist for each patient. A second researcher monitored all completed checklists and excluded missing data.
Demographic data (age and sex), medical history (e.g. diabetes mellitus, asthma, chronic obstructive disease (COPD), hypertension, ischemic heart disease (IHD) and cancer), and at-admission data in terms of body temperature, heart rate, respiratory rate, systolic blood pressure (SBP), diastolic blood pressure (DBP) and peripheral venous blood oxygen saturation value (SpO2), were recorded using the checklist. Also, assess one-month mortality among these patients was assessed with follow-up by phone call. Since the oxygen saturation level is regarded as one of the factors associated with in-hospital mortality in patients with COVID-19, we divided the patients in two groups based on at-admission peripheral venous blood oxygen saturation value (SpO2) namely, SpO2 ≤ 90 and SpO2 > 90 and analyzed the data.
NLR was reported as a prognostic marker in COVID-19 patients by previous reports [18,19]; one of these studies indicated that an NLR cut-off value higher than 3.3 is independently associated with more severe COVID-19 compared with those with NLR < 3.3 [19]. Thus, in the present study, COVID-19 patients were also categorized into two groups based on at-admission NLR (≥3.3 or < 3.3).
2.1. Statistical analysis
Continuous data are reported as median and interquartile range (IQR), and categorical data are expressed as frequency and percentage. Man-Whitney and Chi square tests were done to respectively compare continuous and categorical data between the two groups (patients with SpO2 values >90% vs those with SpO2 values ≤90% at admission). Kaplan-Meier survival analysis was used to estimate one-month mortality of study patients since admission based on SpO2 (>90% or ≤ 90%) and NLR (≥3.3 or < 3.3). Univariate and multivariable Cox proportional hazards models were used. Associations are expressed as hazard ratios (HRs) and 95% CIs. Statistical analysis was performed using SPSS software, version 16 and a 2-sided P < 0.05 was considered significant.
3. Results
Among 219 patients included in the present retrospective cohort study, 137 (62.6%) were men (mean age 58.2 ± 16 years old) and 82 (37.4%) were women (mean age 57 ± 17.3 years old). Overall, 63 (28.8%) patients were admitted to the ICU. Among patients, 83 (38%) had diabetes mellitus, 46 (21%) had IHD, 42 (19.2%) had hyperlipidemia, 85 (38.8%) had hypertension, 9 (4.1%) had asthma, and 15 (6.8%) had COPD as a comorbid disease. Moreover, 23(10.5%) were smoker and 13 (5.9%) were addicted to opium.
Compared to patients with SpO2 > 90%, those with SpO2 ≤ 90% were older and hypertension was more common in these patients (Table 1 ). There were no significant differences in sex or different comorbidities between the two groups. Respiratory rate was higher in patients with SpO2 ≤ 90% compared to patients with SpO2 > 90% (Table 1). The two groups did not differ significantly with respect to other vital signs at admission. Neutrophil counts were higher in patients with SpO2 ≤ 90% (Table 1), while lymphocyte counts did not vary significantly between the groups. Neutrophil-to-lymphocyte ratio (NLR) was greater in patients with SpO2 ≤ 90%. In patients with SpO2 ≤ 90%, compared to those with SpO2 > 90%, hospital stay (number of days) was longer and ICU admission rate was higher (Table 1).
Table 1.
Demographic data, comorbidities, physical examinations results, blood cells counts and hospital stay data of patients with COVID-19 associated pneumonia, grouped in two groups based on oxygen saturation levels at admission
| SpO2 ≤ 90% (N = 142) |
SpO2 > 90% (N = 77) |
P value | |
|---|---|---|---|
| |||
| Age (years old) | 62 (53–75) | 48 (37–60) | <0.001 |
| Male | 86 (60.6) | 51 (66.2) | 0.4 |
| |||
| Hypertension | 65 (45.8) | 20 (26) | 0.004 |
| Ischemic heart disease | 35 (24.6) | 11 (14.3) | 0.07 |
| Diabetes mellitus | 55 (38.7) | 28 (36.4) | 0.7 |
| Hyperlipidemia | 27 (19) | 15 (19.5) | 0.9 |
| Asthma | 6 (4.2) | 3 (3.9) | 0.9 |
| COPD | 12 (8.5) | 3 (3.9) | 0.2 |
| Smoker | 15 (10.6) | 8 (10.4) | 0.9 |
| Addiction | 8 (6.3) | 3 (4.1) | 0.7 |
| |||
| Temperature | 37.3 (37–38) | 37.4 (37–38) | 0.7 |
| Heart rate | 95 (84–110) | 96 (86–107) | 0.8 |
| Respiratory rate | 25 (22−30) | 21 (18–27) | <0.001 |
| Systolic blood pressure | 133 (120–149) | 130 (120–149) | 0.4 |
| Diastolic blood pressure | 80 (75–90) | 80 (75–87) | 0.6 |
| |||
| WBC count | 7.4 (5.7–10.8) | 6.4 (4.3–9) | 0.02 |
| Neutrophil count | 5.7 (4.15–9.5) | 4.8(3.09–6.8) | 0.007 |
| Lymphocyte count | 1.03 (0.78–1.3) | 1.1 (0.76–1.6) | 0.3 |
| NLR | 5 (3.7–8.5) | 4.1 (2.6–6.7) | 0.008 |
| |||
| Hospital stay (days) | 9 (5.5–14) | 7 (5–11) | 0.01 |
| ICU admission | 55 (39) | 8 (10.4) | <0.001 |
| ICU stay (days) | 6 (4–10) | 4 (3−10) | 0.6 |
COPD: Chronic obstructive pulmonary disease; ICU: Intensive care unit; WBC: White blood cells; NLR: Neutrophil-to-lymphocyte ratio; SpO2: Peripheral venous blood oxygen saturation value.
Values are reported as median (IQR) or number (%).
Of 31 (14.2%) individuals who died during one-month follow-up (admission time was considered day 1), 2 (2.6%) individuals had SpO2 values >90%, and 29 (20.4%) had SpO2 values ≤90% (p < 0.001, Fig. 1 ). In addition, our results showed that out of 31 individuals who died, 26 (15.8%) had NLR values ≥3.3, and 4 (7.7%) had NLR <3.3 (p = 0.16, Fig. 2 ); for one of the patients who died, NLR data were not recorded.
Fig. 1.
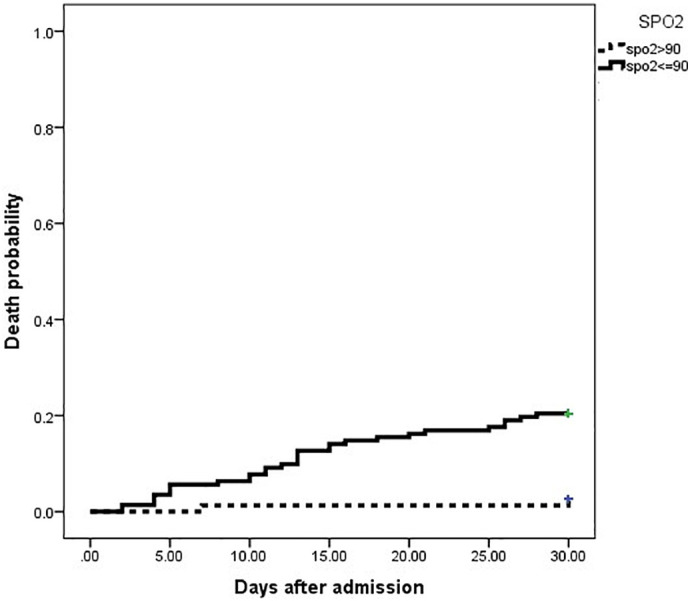
Kaplan-Meier curves for one-month mortality in 219 COVID-19 patients grouped into two groups based on SpO2 (>90% or ≤ 90%) at admission.
SpO2: Peripheral venous blood oxygen saturation value.
Fig. 2.
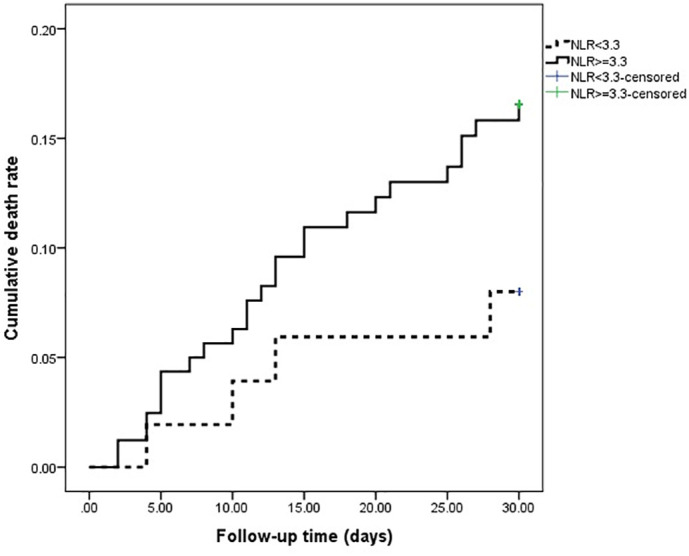
Kaplan-Meier curve for one-month mortality in 219 COVID-19 patients grouped into two groups based on at-admission NLR (≥3.3 or < 3.3).
NLR: Neutrophil-to-lymphocyte ratio.
Univariate Cox regression analysis revealed that older age, SpO2 ≤ 90%, IHD, respiratory rate, WBC, neutrophil and lymphocyte count, and NLR were associated with increased risk of one-month mortality in our patients (Table 2 ).
Table 2.
Factors associated with in-hospital mortality in patients with COVID-19 associated pneumonia
| Factors |
Hazard ratio (95%CI) |
P value |
|---|---|---|
| Univariate analysis | ||
| Age (years) | 1.05 (1.02–1.07) | <0.001 |
| Male | 1.31 (0.61–2.8) | 0.4 |
| SpO2 ≤ 90% | 8.66 (2.06–36.3) | 0.003 |
| Hypertension | 1.32 (0.65–2.70) | 0.4 |
| Diabetes mellitus | 0.9 (0.4–1.8) | 0.7 |
| Smoker | 1.26 (0.44–3.6) | 0.6 |
| Ischemic heart disease | 3.02 (1.47–6.16) | 0.002 |
| Respiratory rate | 1.09 (1.04–1.14) | <0.001 |
| WBC count | 1.08 (1.03–1.10) | <0.001 |
| NLR | 1.05 (1.02–1.07) | <0.001 |
| Multivariate analysis (Backward method) | ||
| Ischemic heart disease | 1.98 (0.94–4.17) | 0.07 |
| Respiratory rate | 1.05 (0.99–1.11) | 0.06 |
| SpO2 ≤ 90% | 3.82 (0.86–16.90) | 0.07 |
| WBC count | 1.05 (1.01–1.08) | 0.006 |
| NLR | 1.03 (1.003–1.07) | 0.03 |
| Age | 1.03 (1.004–1.05) | 0.02 |
WBC: White blood cells; NLR: Neutrophil-to-Lymphocyte Ratio; SpO2: Peripheral venous blood oxygen saturation value.
Among factors included in the multivariate Cox regression model, patients with SpO2 values ≤90%, had a 3.8-fold increased risk of one-month death compared to those with SpO2 > 90%; however, this difference did not reach a significant level. Also, we found that patients with older age and those with higher WBC count or NLR had a higher risk of one-month mortality, after adjusting for sex, IHD, respiratory rate, and SpO2 levels.
4. Discussion
Previously published reports indicated associations between age, sex, comorbidities, and inflammatory biomarkers and mortality in COVID-19 patients [6,8,20]. In this context, independent death-associated value of dyspnea and hypoxemia (SpO2 ≤ 90% in spite of oxygen supplementation) was reported [8]. Though COVID-19 affects both healthy and non-healthy subjects, a report from China showed that 50% of hospital-admitted COVID-19 patients in Huabei province, had comorbidities; this rate increased to almost 66% among ICU-admitted ones or those who did not survive. Importantly, the highest mortality was found in patients with cardiovascular conditions, especially hypertension. Other comorbidities such as diabetes, lung diseases, and obesity, were shown to be associated with poor outcomes [21,22]. Moreover, another report on 5700 COVID-19 hospitalized cases from New York City Area, showed that hypertension was the most frequent comorbidity followed by obesity and diabetes [23]. Also, in 72,314 COVID-19 patients reported by the Chinese center of the disease control, mean death rate increased from 2.3 to 5 and 7.3%, respectively in patients with cardiovascular and diabetic conditions [6,8]. Consistently, in our study, the most common comorbidity was hypertension followed by diabetes and IHD. Also, we found that IHD was associated with an increased risk of one-month mortality among the patients. Despite considerable evidence about worse outcomes in COVID-19 patients with cardiovascular diseases, it is not fully understood whether there exists a casual relation or just an association between such comorbidities and COVID-19 prognosis [24]. An explanation to relate hypertension and COVID-19 is that the immune system is deregulated by hypertension and COVID-19 and when the blood pressure is not appropriately controlled, this dysregulation is exacerbated [25,26]. Thus, blood pressure control in such patients seems to be of crucial importance.
The components of the immune system are the organs, after the lungs, that are most frequently affected by COVID-19. Splenic atrophy and marked decrement of lymphocytes and neutrophils counts along with necrosis and hemorrhage, were indicated in these patients. Also, lymph nodes become depleted from lymphocytes and CD4+ and CD8+ cells counts reduce [25].
Neutrophils are of crucial importance in the innate immune responses while lymphocytes have an important role in inflammatory responses. Thus, an increased NLR reflects an imbalance of the inflammatory response and it could be considered a probable indicator of disease severity in infectious illnesses, such as sepsis and bacteremia [27]. In a meta-analysis of 15 studies, higher neutrophils numbers and NLR but a lower lymphocyte count were observed in severe cases of COVID-19 compared to non-severe cases [28]. The credibility of NLR in diagnosis/prognosis of viral diseases was shown; for instance, NLR was reported to be a more sensitive indicator in influenza patients compared to neutrophil or lymphocyte counts alone [29]. Another study also introduced NLR as an independent predictor of clinical outcomes in COVID-19 patients [19]. Similarly, significantly augmented NLR was found in severe cases of COVID-19 [30]. In line with augmenting clinical evidence on predictive and prognostic potential of NLR [16,31,32], in the present study, higher NLR was associated with increased risk of one-month mortality.
It has been generally shown that subjects of older ages are grouped as “most vulnerable” towards COVID-19 mortality (mortality rate ~ 15%) [6,33,34]. Moreover, a previous report introduced higher age as a predictor of poor prognosis in COVID-19 patients [19]; consistently, another study showed poorer clinical outcomes and higher severity in COVID-19 patients aged ≥60 years old compared to those below 60 [29]. Similarly, we found that elevated age was associated with an increased risk of one-month mortality.
5. Conclusion
In our study population, lymphocytes count in the peripheral blood was non-significantly lower in patients admitted with SpO2 ≤ 90% compared to those with SpO2 > 90%. Nevertheless, statistical analysis showed a significantly higher neutrophil count in patients with SpO2 ≤ 90% compared to the other group; beside, neutrophil count was found to be associated with an increased risk of one-month mortality.
Overall, the findings of the present study, in line with reports from different countries, confirmed that IHD, age, neutrophil count and NLR can be considered predictors of survival in COVID-19 patients.
Author contribution statement
E.V.M. conceived, designed the experiments and collected the data; A. T., M. F., P. L., B. R. K., and A. K. collected data and interpreted the data; N. M., V. G., and R. R. analyzed, discussed and interpreted the data. R. R. and N. M. composed the first draft of the manuscript. All authors approved the final version of the manuscript for submission.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgments
Authors express their appreciation for financial and moral support provided by the Vice Chancellor for Research, Mashhad University of Medical Sciences (project No. 990211).
References
- 1.COVID C, Team R Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb. Mortal. Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coen M., Allali G., Adler D., Serratrice J. Hypoxemia in COVID-19; Comment on: “The neuroinvasive potential of SARS - CoV2 may play a role in the respiratory failure of COVID-19 patients”. J. Med. Virol. 2020;92:1705–1706. doi: 10.1002/jmv.26020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arentz M., Yim E., Klaff L., Lokhandwala S., Riedo F.X., Chong M. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020;323:1612–1614. doi: 10.1001/jama.2020.4326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abedi F., Rezaee R., Karimi G. Plausibility of therapeutic effects of Rho kinase inhibitors against severe acute respiratory syndrome coronavirus 2 (COVID-19) Pharmacol. Res. 2020;156:104808. doi: 10.1016/j.phrs.2020.104808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Y.C., Bai W.Z., Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J. Med. Virol. 2020;92:552–555. doi: 10.1002/jmv.25728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu C., Chen X., Cai Y., Zhou X., Xu S., Huang H. China; JAMA: 2020. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang X., Yu Y., Xu J., Shu H., Liu H., Wu Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie J., Covassin N., Fan Z., Singh P., Gao W., Li G. Elsevier; Mayo Clinic Proceedings: 2020. Association between hypoxemia and mortality in patients with COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qu R., Ling Y., YhZ Zhang, Ly Wei, Chen X., Li X.M. Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J. Med. Virol. 2020;92:1533–1541. doi: 10.1002/jmv.25767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mardani R., Vasmehjani A.A., Zali F., Gholami A., Nasab S.D.M., Kaghazian H. Laboratory parameters in detection of COVID-19 patients with positive RT-PCR; a diagnostic accuracy study. Arch Acad Emerg Med. 2020;8(1) [PMC free article] [PubMed] [Google Scholar]
- 11.Fan B.E., Chong V.C.L., Chan S.S.W., Lim G.H., Lim K.G.E., Tan G.B. Hematologic parameters in patients with COVID-19 infection. Am. J. Hematol. 2020 doi: 10.1002/ajh.25774. In press. [DOI] [PubMed] [Google Scholar]
- 12.Wang J.-T., Sheng W.-H., Fang C.-T., Chen Y.-C., Wang J.-L., Yu C.-J. Clinical manifestations, laboratory findings, and treatment outcomes of SARS patients. Emerg. Infect. Dis. 2004;10(5):818. doi: 10.3201/eid1005.030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in ChinaZhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Liu Y., Du X., Chen J., Jin Y., Peng L., Wang H.H. Neutrophil-to-lymphocyte ratio as an independent risk factor for mortality in hospitalized patients with COVID-19. J. Inf. Secur. 2020;81:e6–e12. doi: 10.1016/j.jinf.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan X., Li F., Wang X., Yan J., Zhu F., Tang S. Neutrophil to lymphocyte ratio as prognostic and predictive factor in patients with coronavirus disease 2019: A retrospective cross-sectional study. J. Med. Virol. 2020;92:2573–2581. doi: 10.1002/jmv.26061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gilbert E.H., Lowenstein S.R., Koziol-McLain J., Barta D.C., Steiner J. Chart reviews in emergency medicine research: where are the methods? Ann. Emerg. Med. 1996;27(3):305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 18.Pimentel G.D., Vega M.C.D., Laviano A. High neutrophil to lymphocyte ratio as a prognostic marker in COVID-19 patients. Clin Nutr ESPEN. 2020;40:101–102. doi: 10.1016/j.clnesp.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang A.-P., Liu J., Tao W., Li H.M. The diagnostic and predictive role of NLR, d-NLR and PLR in COVID-19 patients. Int. Immunopharmacol. 2020;106504 doi: 10.1016/j.intimp.2020.106504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Novel C.P.E.R.E. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [PubMed] [Google Scholar]
- 22.Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Biondi-Zoccai G. Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. J. Am. Coll. Cardiol. 2020;75(18):2352–2371. doi: 10.1016/j.jacc.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cheng P., Zhu H., Witteles R.M., Wu J.C., Quertermous T., Wu S.M. Cardiovascular risks in patients with COVID-19: potential mechanisms and areas of uncertainty. Curr. Cardiol. Rep. 2020;22(5) doi: 10.1007/s11886-020-01293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guzik T.J., Mohiddin S.A., Dimarco A., Patel V., Savvatis K., Marelli-Berg F.M. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc. Res. 2020;116:1666–1687. doi: 10.1093/cvr/cvaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loperena R., Van Beusecum J.P., Itani H.A., Engel N., Laroumanie F., Xiao L. Hypertension and increased endothelial mechanical stretch promote monocyte differentiation and activation: roles of STAT3, interleukin 6 and hydrogen peroxide. Cardiovasc. Res. 2018;114(11):1547–1563. doi: 10.1093/cvr/cvy112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Song H., Kim H.J., Park K.N., Kim S.H., Oh S.H., Youn C.S. Neutrophil to lymphocyte ratio is associated with in-hospital mortality in older adults admitted to the emergency department. Am. J. Emerg. Med. 2020 doi: 10.1016/j.ajem.2020.01.044. In press. [DOI] [PubMed] [Google Scholar]
- 28.Zeng F., Li L., Zeng J., Deng Y., Huang H., Chen B. Can we predict the severity of COVID-19 with a routine blood test? Pol Arch Intern Med. 2020;130:400–405. doi: 10.20452/pamw.15331. [DOI] [PubMed] [Google Scholar]
- 29.Ding X., Yu Y., Lu B., Huo J., Chen M., Kang Y. Dynamic profile and clinical implications of hematological parameters in hospitalized patients with coronavirus disease 2019. Clin. Chem. Lab. Med. 2020;1 doi: 10.1515/cclm-2020-0411. ahead-of-print. [DOI] [PubMed] [Google Scholar]
- 30.Lagunas-Rangel F.A. Neutrophil-to-lymphocyte ratio and lymphocyte-to-C-reactive protein ratio in patients with severe coronavirus disease 2019 (COVID-19): a meta-analysis. J. Med. Virol. 2020;92:1733–1734. doi: 10.1002/jmv.25819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan. China JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y. Dysregulation of immune response in patients with COVID-19 in Wuhan, China. Clin. Infect. Dis. 2020;71:762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morley J.E., Vellas B. COVID-19 and older adult. J. Nutr. Health Aging. 2020;24(4):364–365. doi: 10.1007/s12603-020-1349-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chhetri J.K., Chan P., Arai H., Park S.C., Sriyani Gunaratne P., Setiati S. Prevention of COVID-19 in older adults: a brief guidance from the International Association for Gerontology and Geriatrics (IAGG) Asia/Oceania region. J. Nutr. Health Aging. 2020:1–2. doi: 10.1007/s12603-020-1359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]


