Abstract
To evaluate the change of cervical length and the best timing for pregnancy after cervical conization in patients with cervical intraepithelial neoplasia (CIN).
This was a retrospective study including patients under 40 years with fertility desire treated by cervical conization for CIN. To assess the cervical length, the patients were divided into 2 groups according to different surgery procedure: loop electrosurgical excision procedure (LEEP) and cold knife conisation (CKC). Patients with cervical length < 2.5 cm in CKC group were divided into 2 groups according to whether receiving cervical cerclage. Trans-vaginal ultrasound examination was used to measure cervical length by fixed professional sonographers.
In LEEP group, the cervical length preoperative was significantly longer than 3 months postoperatively (3.03 ± 0.45 cm vs 2.84 ± 0.44 cm, P = .000). In CKC group, the cervical length preoperative was significantly longer than 3 and 6 months postoperatively (2.90 ± 0.41 cm vs 2.43 ± 0.43 cm and 2.68 ± 0.41 cm, respectively, P = .000). Cervical length was significantly longer at 12 and 9 months after cerclage compared to that without cerclage. Eighteen patients got pregnant in LEEP group, among which one was pregnant at 5 months postoperatively and had premature delivery. There was 1 inevitable abortion and 1 preterm birth among 39 pregnant patients from CKC group.
Patients who have fertility desire with CIN were recommended for pregnancy at 6 and 9 months after LEEP and CKC, respectively. Cerclage effectively prolonged cervical length in patents with that less than 2.5 cm to prevent cervical incompetence.
Keywords: cervical cerclage, cervical conization, cervical intraepithelial neoplasia, cervical length
1. Introduction
Cervical intraepithelial neoplasia (CIN) is a premalignant lesion closely related to invasive cervical cancer. With the popularization of cervical cancer screening program, an increasing CIN was detected in women of childbearing age. The choice of treatment for CIN depends on histological grade and patient age. Cervical conization is the primary treatment for CIN, carcinoma in situ and microinvasive carcinoma in young patients with fertility desire, including loop electrosurgical excision procedure (LEEP) and cold knife conization (CKC).
Cervical incompetence induced by cervical conization is a main factor for premature delivery and abortion when used for cervical squamous intraepithelial lesions.[1,2] In a population-based cohort study including 15,108 patients treated with cervical conization (CKC, LEEP, and laser conization), 216,4006 patients never treated and 57,136 patients treated after delivery,[3] Albrechtsen S et al found that women who received cervical conization had a significantly higher rate of preterm delivery in subsequent pregnancies before 24 weeks’ gestation than those who underwent treatment after delivery or those who were never treated (1.5% vs 0.4%). The Norwegian study including 9554 women with singleton births showed that cervical conization was significantly associated with increased risks of spontaneous abortion (0.5% vs 0.2%; hazard ratio 2.5, 95% CI 1.7–3.7).[4] Several other studies investigating the association between depth of the excised cone and risk of preterm delivery showed that the depth more than 10 mm was an independent risk factor for preterm delivery and preterm premature rupture of membranes.[5,6] However, few studies have assessed cervical length and the best timing for pregnancy after cervical conization. The present study measured the cervical length in patients with CIN to explore the effect of cervical conization on cervical length.
2. Materials and methods
2.1. Study population
Patients treated in gynaecological department of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine between January 2015 and December 2016 were collected who received cervical biopsy and needed further cervical conization. Patients should meet the inclusion criteria: less than 40 years old; no history of CIN, cervical carcinoma or other tumors; without cervical incompetence or related surgery history; with fertility desire and not pregnant; histologically confirmed grade I-III CIN (including carcinoma in situ). The ethics committee of Sir Run Run Shaw Hospital reviewed and approved the study.
2.2. Procedures and outcome measures
Cervical conization included LEEP and CKC; the former was performed for cervical squamous atypical hyperplasia and grade I-II CIN and the latter was performed for grade III CIN. A non-absorbable suture was used in cerclage to sew cervix into about 0.5 to 1.0 cm up the bladder peritoneal reflection, just above the level of internal orifice of the uterus.
Trans-vaginal ultrasound examination was used to measure cervical length by fixed professional sonographers. All patients were checked preoperatively and at 2 months after surgery for cervical length. Patients were followed up at 3, 6, 9, 12 months postoperatively to make sure no lesions remained and to assess cervical length.
2.3. Statistical analysis
Measurement data was in accordance with normal distribution by using Kolmogorov–Smirnov test and presented as mean ± standard deviation. The Student t-test was used to compare continuous data. Count data was analyzed with χ2 test and present as absolute value or proportions. P value < .05 was regarded as significant. All statistical analyses were carried out in SPSS statistical software (version 20.0 for Windows, SPSS, Inc.).
3. Results
A total of 190 patients were included in this retrospective study, including 95 patients with grade I-II CIN and 95 patients with grade III CIN. Average age was 30.34 ± 2.73 and 30.17 ± 4.35, respectively.
3.1. Pre- and postoperative evaluation of cervical length in LEEP group
In LEEP group, the length of cervix at 3 months after surgery was significantly shorter than pre-operation (P = .000). Also, a statistic difference was seen in cervical length at 6 months and 3 months postoperatively (2.97 ± 0.51 and 2.84 ± 0.44, P = .000). Comparison of cervical length between pre-operation and 6 or 9 months post-operation demonstrated no significant difference, neither did 9 and 6 months post-operation (Table 1).
Table 1.
Comparison of the length of cervix after coning with loop electrosurgical excision procedure (N = 95).
| Cervical length ( ± s, cm) | T | P | |
| Preoperative | 3.03 ± 0.45 | ||
| Three mo after surgery | 2.84 ± 0.44 | 7.629 | .000∗ |
| Preoperative | 3.03 ± 0.45 | ||
| Six mo after surgery | 2.97 ± 0.51 | 1.970 | .052 |
| Preoperative | 3.03 ± 0.45 | ||
| Nine mo after surgery | 3.01 ± 0.41 | 1.461 | .147 |
| Three mo after surgery | 2.84 ± 0.44 | ||
| Six mo after surgery | 2.97 ± 0.51 | –3.979 | .000∗ |
| Six mo after surgery | 2.97 ± 0.51 | ||
| Nine mo after surgery | 3.01 ± 0.41 | –1.255 | .213 |
LEEP = loop electrosurgical excision procedure.
P < .05.
3.2. Pre- and postoperative evaluation of cervical length in CKC group
Analysis of 95 patients in CKC groups showed that cervical length preoperative was 2.90 ± 0.41 cm, which was significantly longer than that at 3 and 6 months after surgery (P = .000). The comparison of cervical length between 6 and 3 months as well as 9 and 6 months showed significant difference (P = .000). Cervical length at 12 and 15 months post-CKC were also measured, but other comparisons demonstrated no significant difference (P > .05) (Table 2).
Table 2.
Comparison of the length of cervix after coning with cold knife (N = 95).
| Cervical length ( ± s, cm) | T | P | |
| Preoperative | 2.90 ± 0.41 | ||
| Three mo after surgery | 2.43 ± 0.43 | 17.633 | .000∗ |
| Preoperative | 2.90 ± 0.41 | ||
| Six mo after surgery | 2.68 ± 0.41 | 9.893 | .000∗ |
| Preoperative | 2.90 ± 0.41 | ||
| Nine mo after surgery | 2.90 ± 0.39 | –0.094 | .925 |
| Preoperative | 2.90 ± 0.41 | ||
| Twelve mo after surgery | 2.90 ± 0.39 | –0.286 | .776 |
| Preoperative | 2.90 ± 0.41 | ||
| Fifteen mo after surgery | 2.90 ± 0.64 | 0.373 | .710 |
| Three mo after surgery | 2.43 ± 0.43 | ||
| Six mo after surgery | 2.68 ± 0.41 | –15.904 | .000∗ |
| Six mo after surgery | 2.68 ± 0.41 | ||
| Nine mo after surgery | 2.90 ± 0.39 | –14.276 | .000∗ |
| Nine mo after surgery | 2.90 ± 0.39 | ||
| Twelve mo after surgery | 2.90 ± 0.39 | –1.626 | .107 |
| Twelve mo after surgery | 2.90 ± 0.39 | ||
| Fifteen mo after surgery | 2.90 ± 0.64 | 0.577 | .566 |
P < .05.
3.3. Comparison of the cervical length between cerclage and no cerclage group (cervical length < 2.5 cm)
In CKC group, 19 patients had their cervical length less than 2.5 cm. They were assessed to investigate the effect of cerclage on cervical length in patients who were willing to get pregnancy in 2 years. In this subgroup, cervical length was significantly longer at 12 and 9 months postoperatively compared to that without cerclage (Table 3).
Table 3.
Comparison the length of cervix after cerclage with no cerclage.
| Cervical cerclage | N | Cervical length ( ± s, cm) | T | P | |
| Preoperative | cerclage | 10 | 2.33 ± 0.25 | ||
| No cerclage | 9 | 2.35 ± 0.17 | –0.264 | .795 | |
| Three mo after surgery | cerclage | 10 | 2.11 ± 0.28 | ||
| No cerclage | 9 | 1.87 ± 0.29 | 1.783 | .092 | |
| Six mo after surgery | cerclage | 10 | 2.36 ± 0.24 | ||
| No cerclage | 9 | 2.13 ± 0.26 | 2.009 | .061 | |
| Nine mo after surgery | cerclage | 10 | 2.61 ± 0.28 | ||
| No cerclage | 9 | 2.28 ± 0.25 | 2.678 | .016∗ | |
| Twelve mo after surgery | cerclage | 10 | 2.61 ± 0.28 | ||
| No cerclage | 9 | 2.32 ± 0.21 | 2.531 | .022∗ | |
| Fifteen mo after surgery | cerclage | 10 | 2.46 ± 0.88 | ||
| No cerclage | 9 | 2.38 ± 0.15 | 0.214 | .834 |
P < .05.
3.4. Pregnancy outcomes
In LEEP group, 18 patients got pregnant, among which one was pregnant at 5 months postoperatively and had premature delivery (at 30 weeks of gestation), one was in the second trimester and the rest had full-term pregnancy. In CKC group, 39 patients got pregnant, among which 10 patients received cerclage, 35 patients had full-term pregnancy, 1 suffered premature rupture of membrane (at 36 weeks of gestation), 2 were in the second trimester and 1 was in test tube programme (Table 4).
Table 4.
Pregnancy outcome after loop electrosurgical excision procedure and cold knife conization.
| Pregnancy outcomes | LEEP | CKC |
| Inevitable abortion | 0 | 1 |
| In pregnancy | 1 | 2 |
| Premature delivery | 1 | 1 |
| Full-term pregnancy | 16 | 35 |
LEEP = loop electrosurgical excision procedure, CKC = cold knife conization.
4. Discussion and conclusions
There is an increasing number of young CIN patients with fertility desire. American Society for Colposcopy and Cervical Pathology recommended cervical conization as the primary therapeutic strategy for grade II-III CIN. Cervical tissue loss after cervical conization could result in cervical incompetence, a primary reason for habitual abortion in the second trimester of pregnancy. Few studies have reported the change of cervical length after conization. It was reported that cervical canal could return to normal length at 6 months postoperatively.[7,8] Therefore, regeneration of cervical tissue occurred generally at 3 to 12 months after conization.
Previous studies have indicated that the shortened cervix at 3 months after LEEP or CKC would elongate with the wound healing. A retrospective study conducted by Dannie J[9] and his colleagues showed that cervix would recover at 3 months after LEEP and stop shortening. The results in Konno R’ study[10] revealed that immediate pregnancy after LEEP increased the risk of premature delivery and pregnancy was recommended at 3 to 6 months postoperatively. In the present study, cervical length shortened remarkably at 3 months after LEEP (P < .05). However, it returned to normal length at 6 months and had no difference with 9 months which indicated that cervix would stop growing at 6 months postoperatively. Therefore, it was suggested that cervix was during regeneration period at 3 to 6 months after LEEP, and 6 months postoperative was suitable for pregnancy in case of complications. In CKC group, because of the wider excision range, our results showed no difference was seen in cervical length between pre-operation and 9 months after surgery. No significant increase was found in cervix between the periods of 9 to 15 months postoperatively. Therefore, it took 9 months for cervix to recover completely, which was a recommended timing for pregnancy.
Cervical cerclage is the primary treatment for cervical incompetence. Prophylactic cerclage was used to prevent cervical incompetence caused by CKC.[11] In the present study, CKC increased the risk of postoperative cervical incompetence in patients with cervical length less than 2.5 cm. Therefore, a preoperative communication was necessary and CKC plus prophylactic cerclage was performed based on the patient's wishes. Interestingly, cervical length in cerclage group (10 cases) was longer in patients without cerclage (9 cases) after 1-and-a-half-year follow-up (P < .05). A non-absorbable suture was used in cerclage which could constantly stimulate tissue proliferative response, resulting in fibrous tissue proliferation and cervical fibrosis. It accelerated cervical growth in favor of cervical function recovery.
The adverse pregnancy outcomes post-conization were associated with internal orifice damage, cervix stenosis, and destroyed cervical gland that secreted mucus. A study has reported that gestational age at birth presented a linear inverse correlation with depth not volume or transverse diameter of excised specimen. The rate of preterm delivery and abortion in the second trimester of pregnancy was significantly higher in patients with deeper excision specimen.[12] Some studies thought that cervical conization increased 4 to 7-fold the risk of preterm delivery, abortion and premature rupture of membranes.[13,14] The disagreement might be caused by different sample sizes, depth and diameter of the cone and gestation time. In the present study, 18 patients got pregnant in LEEP group, among which one was pregnant at 5 months postoperatively and had premature delivery (at 30 weeks of gestation), and the rest had full-term pregnancy. In CKC group, all 39 patients got pregnant 1 year after surgery, among which one suffered inevitable abortion due to chromosome abnormality.
Currently, the efficiency of cervical cerclage post-conization remained controversial. Shin MY et al[15] analyzed the data from 19 patients (12 with cerclage and 7 without cerclage) with cervical length less than 2.5 cm. The results showed the pregnancy outcomes and fetal conditions between 2 groups presented no significant difference. Althuisius et al[16] randomized patients with cervical length of < 25 mm into 2 groups: therapeutic cerclage (cerclage group) and bed rest alone (bed rest group). No spontaneous preterm delivery was found in 19 patients in cerclage group, yet the rate of preterm delivery before 34 weeks of gestation was up to 44% in bed rest group (P = .02). It was reported that cerclage could reduce preterm delivery by 30% and reduce morbidity and mortality of perinatal infant by 36% in patients with cervical length < 25 mm.[17] A study of Kindinger including 725 patients at 3 London university Hospitals over a 10-year period (2004–2014) has shown that cerclage could significantly reduce preterm delivery rate in patients with shortened cervix post-conization.[18] CKC is a risk factor for cervical incompetence in pregnancy. It was wide accepted that cerclage should be performed in patients with short cervix measured preoperatively. In the present study, 10 patients with cervical length < 2.5 cm received cerclage, among which 5 had full-term pregnancy, 1 suffered premature rupture of membrane (at 36 weeks of gestation) and 2 were in the second trimester of pregnancy. Patients without cerclage have not been willing to get pregnancy until now. It was suggested that the contradiction between the 2 points was caused by the fact that we chose the position above isthmus of uterus for cerclage (Fig. 1) instead of the level of internal orifice of the uterus, which maintained a uniform pressure in uterine cavity during pregnancy in case of cervical expansion (Fig. 2). One-stage operation of cervical conization plus cerclage was technically easier with less pain and injury. If cerclage was performed after conization, surgery would become more difficult due to shortened cervix or postoperative adhesions even a laparoscopic cervical cerclage was necessary. This would increase surgery cost and injury. A limitation for 1-stage operation was a secondary surgery to take out cerclage stiches if postoperative pathology showed positive lesion margin or lesion was adjacent to margin. Therefore, in our study cerclage was selected according to patients’ fertility desire. The results lacked verification from randomized controlled trial and needed more cases for further study.
Figure 1.
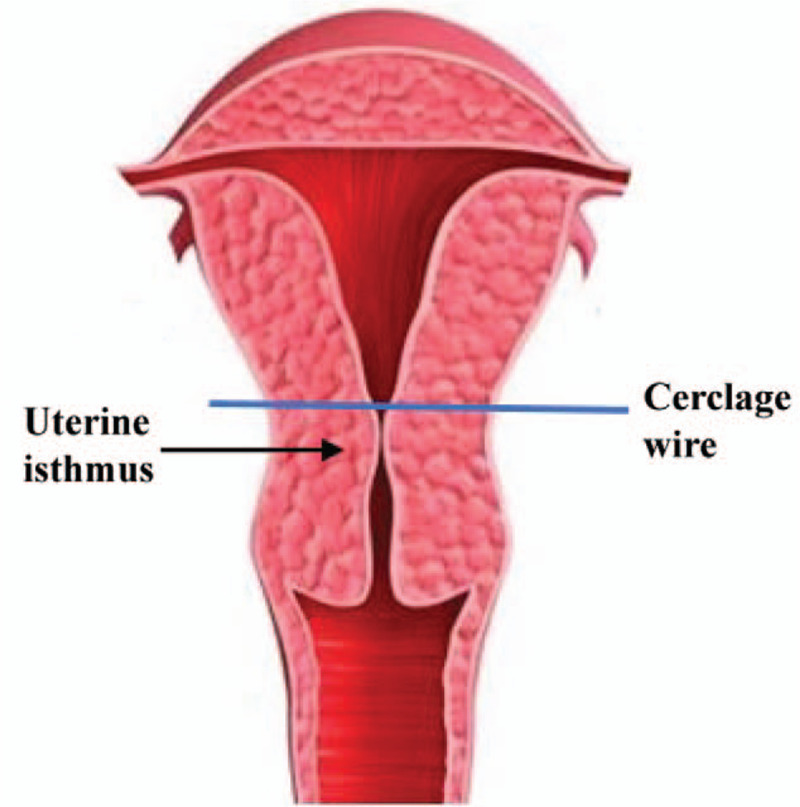
Cerclage position.
Figure 2.
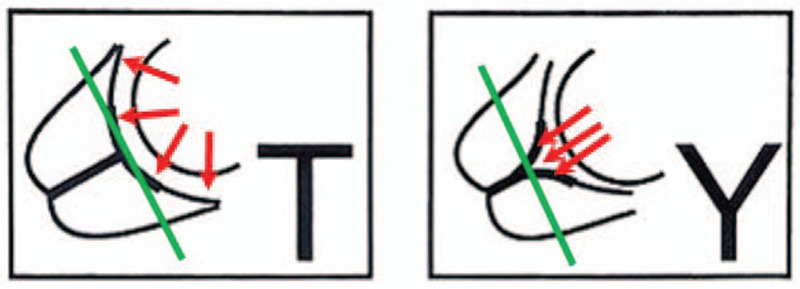
Cerclage position and pressure in the uterine cavity during pregnancy. The shape of cervical internal orifice was T-shaped and Y-shaped, respectively.
In conclusion, the depth and range of excised specimen might affect pregnancy outcome post-conization. A deeper and wider wound postoperative took longer for cervix to heal. Therefore, the range of conization depended on several factors including times of conization, degree of the lesion and fertility desire. According to our research result, 6 months was recommended for pregnancy after LEEP, while 9 months recommended after CKC. Prophylactic cerclage was considered for patents with cervical length less than 2.5 cm to stimulate cervical growth. Cervical length and uterine contraction supervision should be enhanced during pregnancy. It was suggested that experienced surgeons took the operation on patients with fertility desire to prevent not only the residual lesions but also the excessive resection particularly deeper excised specimen and subsequent cervical incompetence.
Author contributions
Conceptualization: Xiao Zhang, Jianhua Yang.
Data curation: Jinfei Tong, Xudong Ma, Hailan Yu.
Investigation: Jinfei Tong, Xiaojing Guan.
Methodology: Jianqiong Li.
Project administration: Xiao Zhang.
Supervision: Jianhua Yang.
Visualization: Xiao Zhang.
Writing – original draft: Xiao Zhang.
Writing – review & editing: Jinfei Tong, Jianhua Yang.
Footnotes
Abbreviations: CIN = cervical intraepithelial neoplasia, CKC = cold knife conization, LEEP = loop electrosurgical excision procedure.
How to cite this article: Zhang X, Tong J, Ma X, Yu H, Guan X, Li J, Yang J. Evaluation of cervical length and optimal timing for pregnancy after cervical conization in patients with cervical intraepithelial neoplasia: a retrospective study. Medicine. 2020;99:49(e23411).
This study was supported by a grant from the Zhejiang Medical and Health Science and Technology Project (No. 2017186075).
This study was approved by the Institutional Review Board of Sir Run Run Shaw Hospital, Zhejiang University School of Medicine (9 May 2019, file record 20190509-01).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- [1].Hagen B, Skjeldestad FE. The outcome of pregnancy after CO2 laser conisation of the cervix. Br J Obstet Gynaecol 1993;100:717–20. [DOI] [PubMed] [Google Scholar]
- [2].Buller RE, Jones HW. Pregnancy following cervical conization. Am J Obstet Gynecol 1982;142:506–12. [DOI] [PubMed] [Google Scholar]
- [3].Albrechtsen S, Rasmussen S, Thoresen S, et al. Pregnancy outcome in women before and after cervical conisation: population based cohort study. Br Med J 2008;337:a1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bjorge T, Skare GB, Bjorge L, et al. Adverse pregnancy outcomes after treatment for cervical intraepithelial neoplasia. Obstet Gynecol 2016;128:1265–73. [DOI] [PubMed] [Google Scholar]
- [5].Kyrgiou M, Koliopoulos G, Martin-Hirsch P, et al. Obstetric outcomes after conservative treatment for intraepithelial or early invasive cervical lesions: systematic review and meta-analysis. Lancet 2006;367:489–98. [DOI] [PubMed] [Google Scholar]
- [6].Noehr B, Jensen A, Frederiksen K, et al. Loop electrosurgical excision of the cervix and subsequent risk for spontaneous preterm delivery: a population-based study of singleton deliveries during a 9-year period. Am J Obstet Gynecol 2009;201:33.e1–6. [DOI] [PubMed] [Google Scholar]
- [7].Bhatla N, Puri K, Joseph E, et al. Association of chlamydia trachomatis infection with human papillomavirus (HPV) & cervical intraepithelial neoplasia - a pilot study. Indian J Med Res 2013;137:533–9. [PMC free article] [PubMed] [Google Scholar]
- [8].Al-Halal H, Kezouh A, Abenhaim HA. Incidence and obstetrical outcomes of cervical intraepithelial neoplasia and cervical cancer in pregnancy: a population-based study on 8.8 million births. Arch Gynecol Obstet 2013;287:245–50. [DOI] [PubMed] [Google Scholar]
- [9].Gentry DJ, Baggish MS, Brady K, et al. The effects of loop excision of the transformation zone on cervical length: implications for pregnancy. Am J Obstet Gynecol 2000;182:516–20. [DOI] [PubMed] [Google Scholar]
- [10]. Konno R. Sitteokitai sikyukeigan sinryo handobook (Handbook for the management of cervical cancer). Tokyo, Japan 2012. [Google Scholar]
- [11].Namouz S, Porat S, Okun N, et al. Emergency cerclage: literature review. Obstet Gynecol Surv 2013;68:379–88. [DOI] [PubMed] [Google Scholar]
- [12].Liverani CA, Di Giuseppe J, Clemente N, et al. Length but not transverse diameter of the excision specimen for high-grade cervical intraepithelial neoplasia (CIN 2-3) is a predictor of pregnancy outcome. Eur J Cancer Prev 2016;25:416–22. [DOI] [PubMed] [Google Scholar]
- [13].Ortoft G, Henriksen T, Hansen E, et al. After conisation of the cervix, the perinatal mortality as a result of preterm delivery increases in subsequent pregnancy. Br J Obstet Gynaecol 2010;117:258–67. [DOI] [PubMed] [Google Scholar]
- [14].van de Vijver A, Poppe W, Verguts J, et al. Pregnancy outcome after cervical conisation: a retrospective cohort study in the Leuven university hospital. Br J Obstet Gynaecol 2010;117:268–73. [DOI] [PubMed] [Google Scholar]
- [15].Shin M-Y, Seo E-S, Choi S-J, et al. The role of prophylactic cerclage in preventing preterm delivery after electrosurgical conization. J Gynecol Oncol 2010;21:230–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Althuisius SM, Dekker GA, Hummel P, et al. Final results of the cervical incompetence prevention randomized cerclage trial (CIPRACT): therapeutic cerclage with bed rest versus bed rest alone. Am J Obstet Gynecol 2001;185:1106–12. [DOI] [PubMed] [Google Scholar]
- [17].Berghella V, Rafael TJ, Szychowski JM, et al. Cerclage for short cervix on ultrasonography in women with singleton gestations and previous preterm birth a meta-analysis. Obstet Gynecol 2011;117:663–71. [DOI] [PubMed] [Google Scholar]
- [18].Kindinger LM, Kyrgiou M, MacIntyre DA, et al. Preterm birth prevention post-conization: a model of cervical length screening with targeted cerclage. Plos One 2016;11:e0163793. [DOI] [PMC free article] [PubMed] [Google Scholar]


