PREAMBLE
The American College of Cardiology (ACC) and the American Heart Association (AHA) performance measurement sets serve as vehicles to accelerate translation of scientific evidence into clinical practice. Measure sets developed by the ACC and AHA are intended to provide practitioners and institutions that deliver cardiovascular services with tools to measure the quality of care provided and identify opportunities for improvement.
Writing committees are instructed to consider the methodology of performance measure development1,2 and to ensure that the measures developed are aligned with ACC/AHA clinical guidelines. The writing committees also are charged with constructing measures that maximally capture important aspects of quality of care, including timeliness, safety, effectiveness, efficiency, equity, and patient-centeredness, while minimizing, when possible, the reporting burden imposed on hospitals, practices, and practitioners.
Potential challenges from measure implementation may lead to unintended consequences. The manner in which challenges are addressed is dependent on several factors, including the measure design, data collection method, performance attribution, baseline performance rates, reporting methods, and incentives linked to these reports.
The ACC/AHA Task Force on Performance Measures (Task Force) distinguishes quality measures from performance measures. Quality measures are those metrics that may be useful for local quality improvement but are not yet appropriate for public reporting or pay-for-performance programs (uses of performance measures). New measures are initially evaluated for potential inclusion as performance measures. In some cases, a measure is insufficiently supported by the guidelines. In other instances, when the guidelines support a measure, the writing committee may feel it is necessary to have the measure tested to identify the consequences of measure implementation. Quality measures may then be promoted to the status of performance measures as supporting evidence becomes available.
Gregg C. Fonarow, MD, FACC, FAHA Chair, ACC/AHA Task Force on Performance Measures
1. INTRODUCTION
In 2018, the Task Force convened the writing committee to begin the process of revising the existing performance measures set for hypertension that had been released in 2011.3 The writing committee also was charged with the task of developing new measures to evaluate the care of patients in accordance with the 2017 Hypertension Clinical Practice Guidelines.4
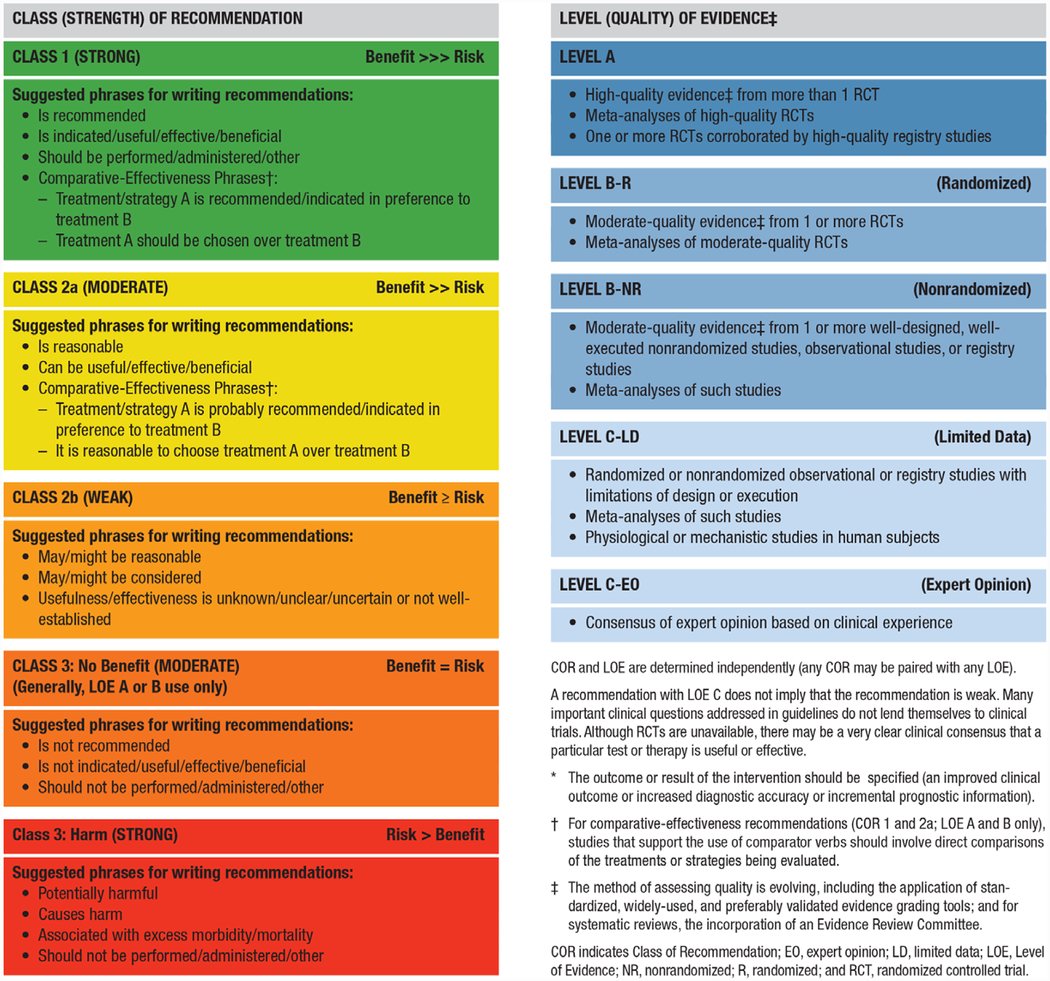
The writing committee developed a comprehensive measure set for the diagnosis and treatment of high blood pressure (HBP) that includes 22 new measures: 6 performance measures, 6 process quality measures, and 10 structural quality measures. In conceptualizing these measures, the writing committee paid very close attention to the current Class of Recommendation (COR) and Level of Evidence (LOE) guideline classification scheme used by ACC and AHA in all of its guidelines, as shown in Table 1.
Table 1.
Applying Class of Recommendation and Level of Evidence to Clinical Strategies, Interventions, Treatments, or Diagnostic Testing in Patient Care (Updated August 2015)*
|
Generally, performance measures are developed from Class 1 CORs and Level A and B LOEs (ie, strong recommendations based on the highest quality of evidence), but quality measures are generally based on lower ranges of CORs and LOEs. This distinction is important to remember throughout the present document, given that performance measures are most commonly designed to be considered for use in national quality payment and reporting programs by entities such as the Centers for Medicare & Medicaid Services (CMS) and the National Committee for Quality Assurance (NCQA), whereas quality measures are typically designed to support quality improvement initiatives and activities at the national or microsystem levels.
The effective implementation of this measure set by clinicians, care teams, and health systems will lead to significant improvements in effective detection and treatment of HBP for millions of people across the United States. Specifications for these new measures take into full account the revised classification taxonomy of HBP from the 2017 Hypertension Clinical Practice Guidelines,4 as noted in Table 2.
Table 2.
BP Classification (JNC 7 and the 2017 Hypertension Clinical Practice Guidelines)
| SBP (mmHg) | and/or | DBP (mmHg) | JNC 75 | 2017 GL4 |
|---|---|---|---|---|
| <120 | and | <80 | Normal BP | Normal BP |
| 120–129 | and | <80 | Prehypertension | Elevated BP |
| 130–139 | or | 80–89 | Prehypertension | Stage 1 hypertension |
| 140–159 | or | 90–99 | Stage 1 hypertension | Stage 2 hypertension |
| ≥160 | or | ≥100 | Stage 2 hypertension | Stage 2 hypertension |
BP should be based on an average of ≥2 careful readings on ≥2 occasions. Adults with SBP or DBP in 2 categories should be designated to the higher BP category.
BP indicates blood pressure; DBP, diastolic blood pressure; GL, guideline; JNC, Joint National Committee; and SBP, systolic blood pressure.
The writing committee felt that it was critically important to incorporate this revised classification into the construction of each of the new performance and quality measures presented in this document. The writing committee believed that the former HBP classification scheme previously published by the Joint National Committee5 was now out of date and needed replacement with that of the 2017 Hypertension Clinical Practice Guidelines,4 described in Table 2, to reduce confusion in the field. The current International Classification of Diseases, 10th edition, codes have not yet been modified to reflect the new classification from the 2017 Hypertension Clinical Practice Guidelines,4 which may create some initial challenges with implementation. The writing committee is sensitive to the fact that the current version (2019 at the time of this writing) of the performance measures for controlling HBP developed by the NCQA for the Healthcare Effectiveness Data and Information Set6 and currently in use in 2019 by CMS7 also does not incorporate the 2017 Hypertension Clinical Practice Guidelines classification scheme. It is well understood that these measures are already in widespread use, especially for quality-related payment programs promulgated by CMS, such as the Medicare Advantage “Stars” ratings, the Medicare Shared Savings Program, and the Physician Quality Payment Program, as well as many other programs promoted by commercial health insurers. In particular, the widespread use of the 2017 Hypertension Clinical Practice Guidelines4 classification scheme will also help to guide decision-making about when to prescribe antihypertensive medications in accordance with its current recommendations for the ACC/AHA stages of HBP (ie, stage 2, stage 1, and elevated blood pressure [BP]), as outlined in Table 3.
Table 3.
Guideline Recommendation for BP-Lowering Medications: ACC/AHA COR/LOE
| ASCVD Risk | Stage 2 High BP (≥140 mmHg) | Stage 1 High BP (139–130 mm Hg) | Elevated BP (129–120 mm Hg) |
|---|---|---|---|
| ASCVD Risk ≥10% | COR: 1, LOE: A | COR: 1, LOE: A | Not recommended |
| ASCVD Risk <10% | COR: 1, LOE: C-LD | Not recommended | Not recommended |
All require intensive lifestyle modification (COR: 1, LOE: A) (applies to the entire table).
For older adults (≥65 years of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit are reasonable for decisions about intensity of BP lowering and choice of antihypertensive drugs (COR: 2a, LOE: C-EO).
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; COR, Class of Recommendation; and LOE, Level of Evidence.
In the 2017 Hypertension Clinical Practice Guidelines,4 the authors emphasized the critical importance of measuring atherosclerotic cardiovascular disease (ASCVD) risk for all patients with HBP, regardless of stage. Therefore, it will be important for the end users of the new ACC/AHA performance measure set to incorporate this risk assessment process in order to achieve successful implementation as a key component of quality improvement for patients with HBP.
Because the current NCQA and CMS performance measures for controlling HBP assess only the population with ACC/AHA stage 2 HBP,6 the writing committee also felt that it was important to emphasize the 2017 Hypertension Clinical Practice Guidelines4 recommendations to lower BP below the 130/80-mm Hg threshold for both ACC/AHA stage 2 and stage 1 patients. In formulating these new performance measures, the writing committee was sensitive to the fact that there is currently not complete consensus among other guidelines from the American College of Physicians (ACP) and the American Academy of Family Physicians (AAFP)8 and also the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH).9 Nonetheless, despite this ongoing debate, the writing committee felt strongly that it is now time to move the US healthcare system ahead to reflect these differing points of view and expects that widespread use of this new measure set will help to achieve this goal.
In addition, the writing committee was concerned that NCQA and CMS would be less likely to consider testing and adopting performance measures with denominator specifications different from those of the “Controlling High Blood Pressure” measure currently in widespread use (and recently revised in 2019).10 Therefore, the writing committee chose to promote flexible denominator congruity and harmonization (as defined by the National Quality Forum [NQF]) with both NCQA and CMS measure specifications in the new ACC/AHA performance measure set to promote its initial widespread use by clinicians and entities who support the treatment recommendations for ACC/AHA stage 1 HBP as emphasized in the 2017 Hypertension Clinical Practice Guidelines.4 This new performance measure set also includes a new composite measure for control of HBP for both ACC/AHA stage 2 and ACC/AHA stage 1 to a systolic goal of <130 mm Hg. Furthermore, the new Process Quality Measures are intended for use in quality improvement initiatives that are designed to take into account management and control for all ACC/AHA stages of HBP without creating controversy or conflict with CMS, NCQA, NQF, and professional societies with differing recommendations and points of view about treatment of ACC/AHA stage 2 and stage 1 HBP. CMS recently determined that the evidence is sufficient to cover ambulatory BP monitoring for the diagnosis of hypertension in Medicare beneficiaries with suspected white coat or masked hypertension.11,12 Annals of Internal Medicine also published an “In the Clinic” section for screening, prevention, diagnosis, and treatment of hypertension, citing the 2017 Hypertension Clinical Practice Guidelines.13
The writing committee was also interested in translating some of the 2017 Hypertension Clinical Practice Guidelines recommendations for systematic strategies that support the consistent and accurate diagnosis and treatment of populations of patients with HBP.4 In its deliberations on this challenge, the writing committee felt that it would be cumbersome and challenging to collect data at the patient and individual clinician levels, thereby limiting the use and utility of measures specified at these levels. With these potential constraints in mind, the writing committee created 10 new structural quality measures designed to evaluate the capability and capacity of various levels of the US healthcare system to implement 2017 Hypertension Clinical Practice Guidelines recommended strategies, such as standardized BP measurement protocols, electronic health record surveillance, telehealth, team-based care, a single plan of care, and performance measurement.4 These new measures are intended for qualitative evaluation of process and infrastructure for these strategies at the care delivery unit (CDU) level (including solo/small physician offices, group practices, health systems, public health sites, accountable care organizations, and clinically integrated networks).
Summaries for these measures are displayed in Tables 4 and 5, which provide information on each measure. Tables 4 and 5 also list each of the new measures and which ACC/AHA classes of HBP are addressed for each. More detailed descriptive and technical specifications for each measure are listed in Appendix A, which provides additional details for each measure description, numerator, denominator (including denominator exclusions and exceptions), rationale for the measure, guideline recommendations that support the measure, measurement period, source of data, and attribution.
Table 4.
Summary of 2019 ACC/AHA Performance and Quality Measures for the Diagnosis and Management of HBP
| Measure No. | Measure Title/Description | ACC/AHA Stage 2 HBP | ACC/AHA Stage 1 HBP | ACC/AHA Elevated BP | COR/LOE |
|---|---|---|---|---|---|
| Performance Measures* | |||||
| PM-1a | ACC/AHA stage 2 HBP control SBP <140 mm Hg | + | - | - | COR: 1, LOE: A |
| PM-1b | ACC/AHA stage 2 HBP control SBP <130 mm Hg | + | - | - | COR: 1, LOE: A / COR: 2a, LOE: C-EO |
| PM-2 | ACC/AHA stage 1 HBP control SBP <130 mm Hg | - | + | - | COR: 1, LOE: A |
| PM-3 | ACC/AHA stage 2 and stage 1 HBP control SBP <130 mm Hg (composite measure combining PM-1b and PM-2) | + | + | - | COR: 1, LOE: A / COR: 2a, LOE: C-EO |
| PM-4 | Nonpharmacological interventions for ACC/AHA stage 2 HBP | + | - | - | COR: 1, LOE: A |
| PM-5 | Use of HBPM for management of ACC/AHA stage 2 HBP | + | - | - | COR: 1, LOE: A |
| Process Quality Measures* | |||||
| QM-1 | Nonpharmacological interventions for ACC/AHA stage elevated BP | - | - | + | COR: 1, LOE: A |
| QM-2 | Nonpharmacological interventions for ACC/AHA stage 1 HBP | - | + | - | COR: 1, LOE: A |
| QM-3 | Nonpharmacological interventions for all ACC/AHA stages of HBP (composite measure combining PM-4, QM-1, and QM-2) | + | + | + | COR: 1, LOE: A |
| QM-4 | Medication adherence to drug therapy for ACC/AHA stage 1 with ASCVD risk ≥10% or ACC/AHA stage 2 HBP | + | + | - | COR: 1, LOE: A |
| QM-5 | Use of HBPM for management of ACC/AHA stage 1 HBP | - | + | - | COR: 1, LOE: A |
| QM-6 | Use of HBPM for management of ACC/AHA stage 1 or ACC/AHA stage 2 (composite measure combining PM-5 and QM-5) | + | + | - | COR: 1, LOE: A |
Performance measures are used in national quality payment and reporting programs, whereas process quality measures support quality improvement initiatives and activities at the national or microsystem levels.
+Indicates the corresponding ACC/AHA stage for the measure.
-Indicates that the ACC/AHA stage does not correspond to the measure.
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; COR, Class of Recommendation; HBP, high blood pressure; HBPM, home blood pressure monitoring; LOE, Level of Evidence; PM, performance measure; QM, quality measure; and SBP, systolic blood pressure.
Table 5.
Summary of 2019 ACC/AHA Structural Measures for the Diagnosis and Management of HBP
| Measure No. | Measure Title/Description | ACC/AHA Stage 2 HBP | ACC/AHA Stage 1 HBP | ACC/AHA Elevated BP | COR/LOE |
|---|---|---|---|---|---|
| Diagnosis, Assessment, and Accurate Measurement | |||||
| SM-1 | Use of a standard protocol to consistently and correctly measure BP in the ambulatory setting | + | + | + | COR: 1, LOE: C-EO |
| SM-2 | Use of a standard process for assessing ASCVD risk (2019 Prevention Guideline14) | + | + | + | COR: 1, LOE: B-NR |
| SM-3 | Use of a standard process for properly screening all adults ≥18 years of age for HBP (USPSTF15) | + | + | + | Grade A (USPSTF) |
| SM-4 | Use of an EHR to accurately diagnose and assess HBP control | + | + | + | COR: 1, LOE: B-NR |
| Patient-Centered Approach for Controlling HBP | |||||
| SM-5 | Use of a standard process to engage patients in shared decision-making, tailored to their personal benefits, goals, and values for evidence-based interventions to improve control of HBP (2019 Prevention Guideline14) | + | + | + | COR: 1, LOE: B-R |
| SM-6 | Demonstration of infrastructure and personnel that assess and address social determinants of health of patients with HBP (2019 Prevention Guideline14) | + | + | + | COR: 1, LOE: B-NR |
| Implementation of a System of Care for Patients With HBP | |||||
| SM-7 | Use of team-based care to better manage HBP | + | + | + | COR: 1, LOE: A |
| SM-8 | Use of telehealth, m-health, e-health, and other digital technologies to better diagnose and manage HBP | + | + | + | COR: 2a, LOE: A / COR: 1, LOE: A |
| SM-9 | Use of a single, standardized plan of care for all patients with HBP | + | + | + | COR: 1, LOE: C-EO |
| Use of Performance Measures to Improve Care for HBP | |||||
| SM-10 | Use of performance and quality measures to improve quality of care for patients with HBP | + | + | - | COR: 2a, LOE: B-NR |
+Indicates the corresponding ACC/AHA stage for the measure.
-Indicates that the ACC/AHA stage does not correspond to the measure.
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; COR, Class of Recommendation; e-health, healthcare services provided electronically via the Internet; EHR, electronic health record; HBP, high blood pressure; LOE, Level of Evidence; m-health, practice of medicine and public health supported by mobile devices; SM, structural measure; and USPSTF, US Preventive Services Task Force.
1.1. Scope of the Problem
Failing to correctly diagnose and control HBP can put people at increased risk for cardiovascular disease, stroke, and renal failure. Recent analyses suggest that >100 million Americans currently have HBP, and the 2011–2014 US National Health and Nutrition Examination Survey estimated that 46% of US adults have HBP.16 An additional 12% of US adults have elevated BP and are at high risk of developing HBP. Among US adults taking antihypertensive medication, 53% have uncontrolled BP.16 Of US adults with hypertension, 20% were unaware they had the condition.17 In a large cohort study of US adults ≥45 years of age, the incidences of ASCVD and all-cause death were 20.5 and 29.6 per 1000 person-years, respectively, among participants with ACC/AHA stage 1 HBP who had been recommended to initiate antihypertensive medication, and 22.7 and 32.9 per 1000 person-years, respectively, among participants with ACC/AHA stage 2 HBP. Among participants taking antihypertensive medication with above-goal BP (ie, systolic BP ≥130 mm Hg or diastolic BP ≥80 mm Hg), the incidences of ASCVD and all-cause death were 33.6 and 42.5 events per 1000 person-years, respectively.18 In addition, individuals with HBP face on average nearly $2000 more in annual healthcare expenses than those without HBP.19
Two studies have projected large reductions in ASCVD and all-cause death among US adults through the achievement of the BP goals in the 2017 Hypertension Clinical Practice Guidelines.20,21 In 1 study, it was estimated that 3 million ASCVD events could be averted over the next 10 years through achievement and maintenance of the 2017 ACC/AHA BP goals (systolic/diastolic BP <130/80 mm Hg; <130 mm Hg for adults ≥65 years of age with low ASCVD risk), as compared with maintaining current BP and treatment and control levels.20 Overall, 33% of all ASCVD events prevented would be in those initiating antihypertensive treatment, and 67% would be in those intensifying current antihypertensive treatment.20
Despite the evidence-based recommendations for lower BP goals (<130/80 mm Hg) in the 2017 Hypertension Clinical Practice Guidelines,4 existing quality measures from the NCQA for controlling HBP (for hypertensive adults 18–59 years of age whose BP was <140/90 mm Hg)6 have not changed substantially over the past several years for various insured populations, including commercial, Medicaid, Medicare Fee for Service, and Medicare Advantage.10 Re-examining both the targets and processes of managing HBP are thus warranted to help support the use of the latest evidence in optimizing the quality of care and outcomes for patients with HBP.
1.2. Disclosure of Relationships With Industry and Other Entities
The Task Force makes every effort to avoid actual, potential, or perceived conflicts of interest that could arise as a result of relationships with industry or other entities (RWI). Detailed information on the ACC/AHA policy on RWI can be found at http://www.acc.org/guidelines/about-guidelines-and-clinical-documents/relationships-with-industry-policy. All members of the writing committee, as well as those selected to serve as peer reviewers of this document, were required to disclose all current relationships and those existing within the 12 months before the initiation of this writing effort. ACC/AHA policy also requires that the writing committee chair and at least 50% of the writing committee have no relevant RWI.
Any writing committee member who develops new RWI during his or her tenure on the writing committee is required to notify staff in writing. These statements are reviewed periodically by the Task Force and by members of the writing committee. Author and peer reviewer RWI that are pertinent to the document are included in the appendixes: Appendix B for relevant writing committee RWI and Appendix C for comprehensive peer reviewer RWI. Additionally, to ensure complete transparency, the writing committee members’ comprehensive disclosure information, including RWI not relevant to the present document, is available online. Disclosure information for the Task Force is also available online at http://www.acc.org/guidelines/about-guidelines-and-clinical-documents/guidelines-and-documents-task-forces.
The work of the writing committee was supported exclusively by the ACC and the AHA without commercial support. Members of the writing committee volunteered their time for this effort. Meetings of the writing committee were confidential and attended only by writing committee members, staff from the ACC and AHA, and representatives of the American Medical Association (AMA) and Preventive Cardiovascular Nurses Association (PCNA), which served as collaborators on this project.
1.3. Abbreviations and Acronyms
| Abbreviation/Acronym | Meaning/Phrase |
|---|---|
| ASCVD | atherosclerotic cardiovascular disease |
| BP | blood pressure |
| CDU | care delivery unit |
| CMS | Centers for Medicare & Medicaid Services |
| COR | Class of Recommendation |
| HBP | high blood pressure |
| LOE | Level of Evidence |
| NCQA | National Committee for Quality Assurance |
| NQF | National Quality Forum |
2. METHODOLOGY
2.1. Literature Review
In developing the updated HBP measure set, the writing committee reviewed evidence-based guidelines and statements that would potentially impact the construction of the measures. The clinical practice guidelines and scientific statements that most directly contributed to the development of these measures are shown in Table 6.
Table 6.
Associated Clinical Practice Guidelines and Other Clinical Guidance Documents
| Clinical Practice Guidelines | |
|---|---|
| 1 | 2017 Hypertension Clinical Practice Guidelines4 |
| 2 | 2019 Cardiovascular Disease Prevention Guideline14 |
| 3 | 2017 USPSTF High Blood Pressure Guideline15 |
| Performance Measures and Scientific Statements | |
| 1 | 2011 Hypertension Performance Measures3 |
| 2 | NQF Measure 0018 Controlling High Blood Pressure (NCQA)22 |
| 3 | ACC/AHA Performance Measures Methodology1 |
ACC indicates American College of Cardiology; AHA, American Heart Association; NCQA, National Committee for Quality Assurance; NQF, National Quality Forum; and USPSTF, US Preventive Services Task Force.
2.2. Definition and Selection of Measures
In constructing the measure set, the writing committee recognized that other organizations (eg, CMS, NCQA) have developed or are continuing to develop HBP performance measures in response to the release of the 2017 Hypertension Clinical Practice Guidelines.4 Hence, the committee created performance measures for ACC/AHA stage 2 HBP that are aligned with these other groups, called harmonizing measures. In addition, the committee created enhancing measures that incorporate emerging evidence showing improved outcomes with more aggressive BP control (ie, for ACC/AHA stage 1 HBP). When defining harmonization, the writing committee followed the NQF Guidance for Measure Harmonization report, which states “measure harmonization should be considered when measures are intended to address either the same measure focus—the target process, condition, event, outcome (eg, numerator)—or the same target population (eg, denominator).”23 The enhancing performance and quality measures are intended to promote the widespread application in clinical practice of the current recommendations from the 2017 Hypertension Clinical Practice Guidelines4 to improve care and outcomes for all patients with HBP, including those with ACC/AHA stage 1 HBP and elevated BP. The writing committee acknowledges that adding new performance measures may not be initially feasible in the current regulatory environment, in which many healthcare entities already have a high burden to collect and report existing quality measures. Nonetheless, it is imperative that national quality improvement efforts urgently incorporate high-quality, evidence-based recommendations into practice, especially given the recent lack of significant progress in controlling HBP with national measures in current use by CMS, NCQA, state Medicaid agencies, NQF, and other entities (Figure 1).6
Figure 1. Performance of HEDIS Controlling HBP Measure 1999–2017 (percent of patients with hypertension treated in accordance with the HEDIS Controlling HBP Measure).
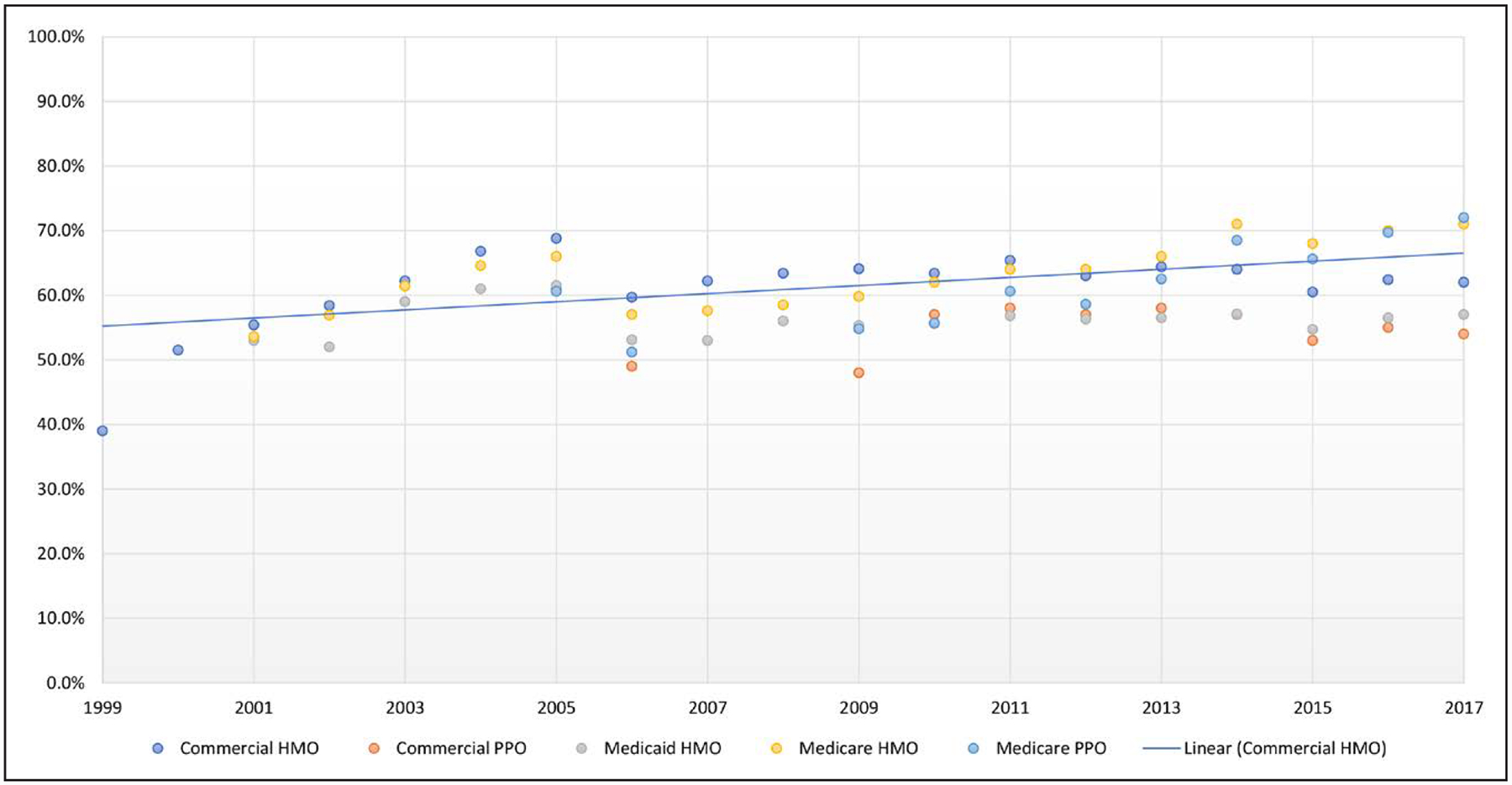
The HEDIS Hypertension Measure6 assesses adults 18–85 years of age who had a diagnosis of hypertension and whose blood pressure was adequately controlled according to the following criteria: 1) Adults 18–59 years of age whose blood pressure was <140/90 mm Hg. 2) Adults 60–85 years of age, with a diagnosis of diabetes mellitus, whose blood pressure was <140/90 mm Hg. 3) Adults 60–85 years of age, without a diagnosis of diabetes mellitus, whose blood pressure was <150/90 mm Hg (likely to be lowered in 2018 to <140/90 mm Hg). Data in graph from National Committee for Quality Assurance (NCQA).6 HBP indicates high blood pressure; HEDIS, Healthcare Effectiveness Data and Information Set; HMO, health maintenance organization; and PPO, preferred provider organization.
The writing committee reviewed clinical practice guidelines and other clinical guidance documents recently published by other entities, in addition to ACC/AHA documents. The writing committee also examined available information on gaps in care to address which new measures might be appropriate as performance measures or quality measures for this measure set update, based on the attributes for performance measures outlined in Table 7.
Table 7.
ACC/AHA Task Force on Performance Measures: Attributes for Performance Measures24
| 1. Evidence Based | |
| High-impact area that is useful in improving patient outcomes |
|
| 2. Measure Selection | |
| Measure definition | a. The patient group to whom the measure applies (denominator) and the patient group for whom conformance is achieved (numerator) are clearly defined and clinically meaningful. |
| Measure exceptions and exclusions | b. Exceptions and exclusions are supported by evidence. |
| Reliability | c. The measure is reproducible across organizations and delivery settings. |
| Face validity | d. The measure appears to assess what it is intended to. |
| Content validity | e. The measure captures most meaningful aspects of care. |
| Construct validity | f. The measure correlates well with other measures of the same aspect of care. |
| 3. Measure Feasibility | |
| Reasonable effort and cost | a. The data required for the measure can be obtained with reasonable effort and cost. |
| Reasonable time period | b. The data required for the measure can be obtained within the period allowed for data collection. |
| 4. Accountability | |
| Actionable | a. Those held accountable can affect the care process or outcome. |
| Unintended consequences avoided | b. The likelihood of negative unintended consequences with the measure is low. |
Reproduced with permission from Thomas et al.25 Copyright © 2018, American Heart Association, Inc., and American College of Cardiology Foundation. ACC indicates American College of Cardiology; and AHA, American Heart Association.
3. AHA/ACC HBP MEASURE SET PERFORMANCE MEASURES
3.1. Discussion of Changes to 2011 Hypertension Measure Set
After reviewing the existing guidelines and the 2011 hypertension measure set,3 the writing committee discussed which measures required revision to reflect updated science related to HBP and identified which guideline recommendations could serve as the basis for new performance or quality measures. The writing committee also reviewed existing publicly available measure sets.
These subsections serve as a synopsis of the revisions that were made to previous measures and a description of why the new measures were created for both the inpatient and outpatient settings.
3.1.1. Retired Measures
The writing committee decided to retire the BP Control Measure because it was not concordant with the 2017 Hypertension Clinical Practice Guidelines.4
3.1.2. New Measures
On the basis of the 2017 Hypertension Clinical Practice Guidelines4 and the 2019 Prevention Guideline,14 the writing committee created a comprehensive list of measures intended to be used to improve important gaps in the quality of care for patients with HBP.4,14 This set includes 22 new measures: 6 performance measures, 6 process quality measures, and 10 structural quality measures. Table 8 includes a list of the measures with information on the attribution and a brief rationale. Performance measures are typically outcome measures that target meaningful gaps in the quality of care, are based on Class 1 clinical practice guideline recommendations, and are appropriately designed for use in accountability in programs that rely on public reporting and pay-for-value initiatives promoted by organizations such as CMS, commercial payers, the NCQA, and the NQF. The writing committee believes that it is important to confirm its full support of the performance measure for BP control in current widespread use by CMS and NCQA for HBP (ie, the proportion of stage 2 patients with HBP with control below the Joint National Committee5 traditional target of 140/90 mm Hg). In addition, the writing committee unanimously feels it important to include new harmonizing measures for stage 1 HBP and a composite measure (ie, for ACC/AHA stage 2 and ACC/AHA stage 1 combined) that emphasize the importance of controlling HBP below the new ACC/AHA target of 130/80 mm Hg, as recommended by the 2017 Hypertension Clinical Practice Guidelines.4 Because of the importance of the promotion of intensive nonpharmacological “healthy lifestyle” modifications and home BP monitoring for patients with stage 2 HBP (as emphasized in the 2017 Hypertension Clinical Practice Guidelines,4 new performance measures to assess quality of care in this regard have been included. These new performance measures are also intended to harmonize with the performance measure for stage 2 HBP currently in use by CMS and NCQA.
Table 8.
New Performance, Quality, and Structural Measures for the Diagnosis and Management of HBP in the Outpatient Care Setting*
| Measure No. | Measure Title | Attribution | Rationale for Creating New Measure |
|---|---|---|---|
| PM-1a | ACC/AHA stage 2 HBP control SBP <140 mm Hg (harmonizing measure) | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) | Harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use. |
| PM-1b | ACC/AHA stage 2 HBP control SBP <130 mm Hg (enhancing measure) | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) | Harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use and adds lower target for further risk reduction. |
| PM-2 | ACC/AHA stage 1 HBP control SBP <130 mm Hg (harmonizing measure) | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) | Harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use. Adds emphasis on including the ACC/AHA stage 1 HBP population. |
| PM-3 | ACC/AHA stage 2 and stage 1 HBP control SBP <130 mm Hg (composite measure combining PM-1b and PM-2) | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) | Harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use. Adds emphasis on including the ACC/AHA stage 1 HBP population and combines both ACC/AHA stage 2 and stage 1 HBP populations. |
| PM-4 | Nonpharmacological interventions for ACC/AHA stage 2 HBP | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system | Harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use. Adds new emphasis on high-quality evidence and strong recommendation for promoting lifestyle modification, as recommended in the 2017 Hypertension Clinical Practice Guidelines for this population as an important strategy for controlling HBP. |
| PM-5 | Use of HBPM for management of ACC/AHA stage 2 HBP | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) | Harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use. Adds new emphasis on correct measurement of BP by individuals at home or elsewhere outside the clinic setting, as recommended in the 2017 Hypertension Clinical Practice Guidelines for this population as an important strategy for evaluating control of HBP. |
| QM-1 | Nonpharmacological interventions for ACC/AHA stage elevated BP | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system | Adds new emphasis on high-quality evidence and strong recommendation for promoting lifestyle modification, as recommended in the 2017 Hypertension Clinical Practice Guidelines for ACC/AHA elevated BP population as an important strategy for controlling HBP. |
| QM-2 | Nonpharmacological interventions for ACC/AHA stage 1 HBP | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system | Adds new emphasis high-quality evidence and strong recommendation for promoting lifestyle modification, as recommended in the 2017 Hypertension Clinical Practice Guidelines for ACC/AHA stage 1 population as an important strategy for controlling HBP. |
| QM-3 | Nonpharmacological interventions for all ACC/AHA stages of HBP (composite measure combining PM-4, QM-1, and QM-2) | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system | Adds new emphasis on high-quality evidence and strong recommendation for promoting lifestyle modification, as recommended in the 2017 Hypertension Clinical Practice Guidelines for all 3 ACC/AHA stages of HBP population as an important strategy for controlling HBP. Composite measure permits assessment of effectiveness for all stages combined. |
| QM-4 | Medication adherence to drug therapy for ACC/AHA stage 1 with ASCVD risk ≥10% or ACC/AHA stage 2 HBP | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system | Adds new emphasis on high-quality evidence and strong recommendation for assessing and promoting medication adherence, as recommended in the 2017 Hypertension Clinical Practice Guidelines for the combined ACC/AHA stage 1 with ASCVD risk ≥10% and ACC/AHA stage 2 HBP population as an important strategy for controlling HBP. |
| QM-5 | Use of HBPM for management of ACC/AHA stage 1 HBP | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system | Harmonizes with new performance measure PM-5 for ACC/AHA stage 2 HBP. Adds new emphasis on correct measurement of BP by individuals at home or elsewhere outside the clinic setting, as recommended in the 2017 Hypertension Clinical Practice Guidelines for this population as an important strategy for evaluating control of ACC/AHA stage 1 HBP and ASCVD risk ≥10%. |
| QM-6 | Use of HBPM for management of ACC/AHA stage 1 or ACC/AHA stage 2 (composite measure combining PM-5 and QM-5) | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) | Harmonizes with new measures PM-5 and QM-5 and adds new emphasis on correct measurement of BP by individuals at home or elsewhere outside the clinic setting, as recommended in the 2017 Hypertension Clinical Practice Guidelines for this population as an important strategy for evaluating control of ACC/AHA stage 2 and stage 1 HBP and ASCVD risk ≥10%. Composite measure permits assessment of effectiveness for these 2 stages combined. |
| SM-1 | Use of a standard protocol to consistently and correctly measure BP in the ambulatory setting | CDU† | Accurate measurement and recording of BP are essential to categorize level of BP, ascertain BP-related CVD risk, and guide management of high BP Office BP measurement is often unstandardized, despite the well-known consequences of inaccurate measurement. Errors are common and can result in a misleading estimation of an individual’s true level of BP if staff are not trained and a protocol is not followed. |
| SM-2 | Use of a standard process for assessing ASCVD risk | CDU† | To facilitate decisions about preventive interventions, it is recommended to screen for traditional ASCVD risk factors and apply the race- and sex-specific PCE (ASCVD Risk Estimator) to estimate 10-year ASCVD risk for asymptomatic adults 40–79 years of age. |
| SM-3 | Use of a standard process for properly screening all adults ≥18 y of age for HBP | CDU† | The evidence on the benefits of screening for HBP is well established. In 2007, the USPSTF reaffirmed its 2003 recommendation to screen for HBP in adults ≥18 y of age. |
| SM-4 | Use of an EHR to accurately diagnose and assess HBP control | CDU† | A growing number of health systems are developing or using registries and EHRs that permit large-scale queries to support population health management strategies to identify undiagnosed or undertreated HBP. |
| SM-5 | Use of a standard process to engage patients in shared decision-making, tailored to their personal benefits, goals, and values for evidence-based interventions to improve control of HBP | CDU† | Decisions about primary prevention should be collaborative decisions made between a clinician and a patient. |
| SM-6 | Demonstration of infrastructure and personnel that assess and address social determinants of health of patients with HBP | CDU† | It is important to tailor advice to an individual’s socioeconomic and educational status, as well as cultural, work, and home environments. |
| SM-7 | Use of team-based care to better manage HBP | CDU† | RCTs and meta-analyses of RCTs of team-based HBP care involving nurse or pharmacist intervention demonstrated reductions in SBP and DBP and/or greater achievement of BP goals when compared with usual care. |
| SM-8 | Use of telehealth, m-health, e-health, and other digital technologies to better diagnose and manage HBP | CDU† | Meta-analyses of RCTs of different telehealth interventions have demonstrated greater SBP and DBP reductions and a larger proportion of patients achieving BP control than those achieved with usual care without telehealth. |
| SM-9 | Use of a single, standardized plan of care for all patients with HBP | CDU† | Studies demonstrate that implementation of a plan of care for HBP can lead to sustained reduction of BP and attainment of BP targets over several years. |
| SM-10 | Use of performance and quality measures to improve quality of care for patients with HBP | CDU† | A large observational study showed that a systematic approach to HBP control, including the use of performance measures, was associated with significant improvement in HBP control compared with historical control groups. |
Including office, clinic, home, or ambulatory.
Including, but not limited to, solo/small physician offices, group practices, ambulatory care centers, health systems, public health sites, accountable care organizations, and clinically integrated networks that diagnose and treat patients with HBP.
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CDU, care delivery unit; CVD, cardiovascular disease; DBP, diastolic blood pressure; e-health, healthcare services provided electronically via the Internet; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; m-health, practice of medicine and public health supported by mobile devices; PCE, pooled cohort equations; PM, performance measure; QM, quality measure; RCT, randomized controlled trial; SBP, systolic blood pressure; SM, structural measure; and USPSTF, US Preventive Services Task Force.
Quality measures, on the other hand, are intended to be deployed in collaborative quality improvement initiatives (such as those promoted by the ACC and AHA) that do not require the degrees of technical rigor required for performance measures. The writing committee decided to include 6 new process quality measures based on Class 1 recommendations from the 2017 Hypertension Clinical Practice Guidelines4 recommendations that address important gaps in care for patients with HBP. If additional evidence evolves that demonstrates significant impact on the quality of care and meets NQF requirements for reliability, feasibility, usability, validity, and acceptable burden of data collection for these measures, then they may be considered as potential future performance measures by the writing committee and other entities, such as CMS, NCQA, state Medicaid agencies, and NQF.
Given the extensive emphasis on developing more effective systems of care for patients with HBP, the writing committee also feels it is important to present a new concept of structural measures, which are designed to improve these systems. This category of quality measure is intended to evaluate care at the aggregate care delivery unit (CDU) level, as opposed to the performance and quality measures, which are designed to summarize the evaluation of care of prespecified populations with HBP at the individual, group clinician, or health plan levels. A CDU represents the organizational structure of the clinicians who are delivering care to these patients. This measurement includes a hierarchical scale of the health delivery infrastructure for optimal management of patients with HBP that is available to organizations such as a small medical practice, a multispecialty clinic, a community-based health center (eg, a Federally Qualified Health Center), a hospital-owned ambulatory care site, or even a large, geographically dispersed health system (eg, the US Department of Veterans Affairs).
The writing committee developed this new category of 10 structural measures in hopes that they could be implemented within a CDU at any level of the health system to assess strengths and weaknesses of available infrastructure designed to improve accurate diagnosis and management of patients with HBP, again in accordance with relevant recommendations from the 2017 Hypertension Clinical Practice Guidelines.4 The writing committee emphasizes that expecting the structural measures to be interpreted as rigid requirements for CDUs would not permit the high level of flexibility these diverse entities need to use these measures for their own self-assessment and collaborative quality improvement implementation initiatives. Hence, these new measures are currently not designed or intended to be used for accountability “standards” but rather to be used as a roadmap for solo/small physician offices, group practices, health systems, public health sites, accountable care organizations, and clinically integrated networks, etc., in their collective journeys to establish better and more standardized guideline-based systems of care for the many millions of patients with HBP across the United States.
More detailed information on the specifications for these new performance, quality, and structural measures for care of patients with HBP is presented in Appendix A.
4. AREAS FOR FURTHER RESEARCH
Several additional areas of research will potentially have an impact on HBP performance and quality measures:
Further research is needed on devices for measuring BP for diagnosis and control, including continuous measurements from digital devices and entering BP measurements into electronic health records.
Further research is needed on improving the accuracy of office BP measurements, including appropriate technique, number of measurements, and training of healthcare providers in measuring BP to help standardize care and improve utilization of performance measures.
Technology for measurement of BP continues to evolve. Several ambulatory BP monitoring and home BP monitoring devices, including cuffless devices that incorporate optical BP monitoring algorithms, are available, although out-of-office BP measurements using validated upper-arm devices with appropriately sized cuffs are recommended to confirm the diagnosis of HBP and for titration of BP-lowering medications. Additional data on accuracy, reproducibility, costs, and device comparisons are needed.
The field would benefit from further research on how improvement in HBP measurement, such as the use of home BP monitoring and use of a standard protocol to measure BP accurately, as incorporated into guideline-based clinical interventions (eg, AHA and AMA Target: BP), translates into improvement in BP care.26
Field testing is needed to determine the utilization of new process and structural quality measures for the future development of new performance measures. This is especially true for lifestyle modifications, shared decision making, and implementation of a standardized protocol to consistently and correctly measure BP.
Efforts to standardize BP data entry into electronic health records are needed to improve diagnosis and management of HBP. These include entering multiple readings and averages of readings, with electronic health record systems having the ability to perform the averaging function automatically for multiple BP readings within a visit and across ≥2 visits. Future HBP patient registries should include a broader range of races/ethnicities and incorporate data on other socioeconomic determinants of health, as well as patient engagement and activation, to better understand the impact of these variables on medication adherence and BP control.
Continued research to examine temporal trends and disparities (with respect to sex, race/ethnicity, and socioeconomic status) in the achievement of performance and quality measures is critical for future revisions of these measure sets. Before adoption of behavioral and motivational strategies as new performance measures, prospective studies evaluating their efficacy in achieving a healthy lifestyle and a standardized process for patient-centered shared decision making for BP control are needed.
Utilization of new performance measures in public accountability and payment programs is needed. The impact of inclusion of HBP performance measures in pay-for-performance strategies on HBP diagnosis, management, and outcomes should be prospectively evaluated. The impact of compliance with some or all performance measures on hospital quality of care and short- and long-term clinical outcomes should be assessed.
The HBP performance measures may further evolve on the basis of additional evidence, along with future focused updates and revisions to the 2017 Hypertension Clinical Practice Guidelines.
Supplementary Material
Acknowledgments
ACC/AHA TASK FORCE MEMBERS
Gregg C. Fonarow, MD, FACC, FAHA, Chair*; Biykem Bozkurt, MD, PhD, FACC*; Sandeep Das, MD, MPH*; Michael E. Hall, MD, MS, FAHA, FACC*; Hani Jneid, MD, FACC, FAHA*; Corrine Y. Jurgens, PhD, RN, ANP-BC, FAHA*†; Patricia Keegan, DNP, APRN, NP-C‡; Rohan Khera, MD*†; Leo Lopez, MD, FACC‡; Jeffrey W. Olin, DO, FACC, FAHA*; Manesh Patel, MD, FACC*; Faisal Rahman, BM BCh‡; Matthew Roe, MD, FACC‡; Alex Sandhu, MD, MS‡; Randal J. Thomas, MD, MS, FACC, FAHA‡; Muthiah Vaduganathan, MD, MPH†‡; Paul D. Varosy, MD, FACC†‡; Siqin Ye, MD, MS‡; Boback Ziaeian, MD, PhD, FACC‡
*American Heart Association Representative.
† Former Task Force member; current member during the writing effort.
‡American College of Cardiology Representative.
STAFF
American College of Cardiology
Richard J. Kovacs, MD, FACC, President
Timothy W. Attebery, MBA, FACHE, Chief Executive Officer
William J. Oetgen, MD, MBA, FACC, FACP, Executive Vice
President, Science, Education, Quality, and Publishing
Lara Slattery, Team Lead/Division Vice President, Clinical Registry and Accreditation
Esteban Perla, MPH, Team Lead, Quality Measurement
Amelia Scholtz, PhD, Publications Manager, Science, Education, Quality, and Publishing
American College of Cardiology/American Heart Association
Abdul R. Abdullah, MD, Director, Guideline Science and Methodology
Rebecca L. Diekemper, MPH, Guideline Advisor, Performance Measures
American Heart Association
Ivor J. Benjamin, MD, FAHA, President
Nancy Brown, Chief Executive Officer
Mariell Jessup, MD, FAHA, Chief Science and Medical Officer
Rose Marie Robertson, MD, FAHA, Deputy Chief Science and Medical Officer
Gayle R. Whitman, PhD, RN, FAHA, FAAN, Senior Vice President, Office of Science Operations
Radhika Rajgopal Singh, PhD, Director, Science and Medicine, Office of Science Operations
Anne Leonard, MPH, RN, FAHA, Senior Science and Medicine Advisor, Office of Science Operations
Melanie Shahriary, RN, BSN, Senior Manager, Performance Metrics, Quality and Health IT
Jody Hundley, Production and Operations Manager, Scientific Publications, Office of Science Operations
Appendix A. HBP Measure Set
Performance Measures for HBP
Short Title: PM-1a: ACC/AHA Stage 2 HBP Control SBP <140 mm Hg (Harmonizing Measure)
PM-1a: Percentage of Patients 18 to 85 years of Age Who Had a Diagnosis of ACC/AHA Stage 2 HBP and Whose SBP Was <140 mm Hg During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 2 HBP with SBP <140 mm Hg (harmonizes with current performance measure “Controlling High Blood Pressure” in widespread use) | |
| Numerator | Patients with SBP <140 mm Hg |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 2 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | Documentation of a medical reason (eg, treatment intolerance, significant risk of treatment intolerance, especially for frail patients ≥65 y of age) Documentation of a patient reason (eg, economic/access issues) |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of BP in patients with hypertension can help prevent cardiovascular events, including MI, stroke, and the development of HF, and reduce the risk of death from these complications. This performance measure harmonizes with NCQA HEDIS 2019, ICSI, VHA, NQF Measure 0018, Medicaid, Medicare Physician QPP (formerly PQRS), MSSP, Million Hearts, physician feedback/QRUR, physician VBM, QHP, QRS commonly used in payment programs, public reporting, quality improvement (internal to the specific organization), and regulatory and accreditation programs. National average rates of performance have been consistently <70% for several years for HEDIS. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. BP should be categorized as normal, elevated, or stage 1 or 2 hypertension to prevent and treat high BP.27–46 (Class 1, Level of Evidence: B-NR) | |
| 2. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
| 3. For adults with confirmed hypertension and known CVD or 10-y ASCVD event risk of 10% or higher, a BP target of less than 130/80 mm Hg is recommended.46,51–54 (Class 1, Level of Evidence: SBP: B-RSR, DBP: C-EO) | |
| 4. For older adults (≥65 y of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit are reasonable for decisions regarding intensity of BP lowering and choice of antihypertensive drugs. (Class 2a, Level of Evidence: C-EO) | |
| 5. Use of the EHR and patient registries is beneficial for identification of patients with undiagnosed or undertreated hypertension.55–57 (Class 1, Level of Evidence: B-NR) | |
| 6. Treatment of hypertension with a SBP treatment goal of less than 130 mm Hg is recommended for noninstitutionalized ambulatory community-dwelling adults (≥65 y of age) with an average SBP of 130 mm Hg or higher.58 (Class 1, Level of Evidence: A) | |
| 7. Adults with stage 2 hypertension should be evaluated by or referred to a primary care provider within 1 month of the initial diagnosis, have a combination of nonpharmacological and antihypertensive drug therapy (with 2 agents of different classes) initiated, and have a repeat BP evaluation in 1 month.59,60 (Class 1, Level of Evidence: B-R) | |
| 8. In adults with an untreated SBP greater than 130 mm Hg but less than 160 mm Hg or DBP greater than 80 mm Hg but less than 100 mm Hg, it is reasonable to screen for the presence of white coat hypertension by using either daytime ABPM or HBPM before diagnosis of hypertension.61–68 (Class 2a, Level of Evidence: B-NR) | |
Resources: 1) Qualified Electronic Health Record,69 2) PCPI National Quality Registry Network (NQRN).70 3) American College of Cardiology Foundation (ACCF) American Heart Association (AHA) Physician Consortium for Performance Improvement (PCPI) Hypertension Performance Measurement Set. 4) NQF Measure 0018 Controlling High Blood Pressure (NCQA).22
Additional note: 2017 Hypertension Clinical Practice Guidelines relies on average BP readings. NCQA HEDIS relies on most recent BP reading: The member is numerator compliant if the BP is <140/90 mm Hg. The member is not compliant if the BP is ≥140/90 mm Hg, if there is no BP reading during the measurement year, or if the reading is incomplete (eg, the systolic or diastolic level is missing). If there are multiple BPs on the same date of service, use the lowest systolic and diastolic BP on that date as the representative BP.
ABPM indicates ambulatory blood pressure monitoring; ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CVD, cardiovascular disease; DBP, diastolic blood pressure; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; HEDIS, Healthcare Effectiveness Data and Information Set; HF, heart failure; ICSI, Institute for Clinical Systems Improvement; MI, myocardial infarction; MSSP, Medicare Shared Savings Program; NCQA, National Committee for Quality Assurance; NQF, National Quality Forum; PCPI, Physician Consortium for Performance Improvement; QCDR, Qualified Clinical Data Registry; QHP, Qualified Health Plan; QPP, Quality Payment Program; QRS, Quality Rating System; QRUR, Quality and Resource Use Reports; SBP, systolic blood pressure; VBM, Value-Based Payment Modifier; and VHA, Veterans Health Administration.
Short Title: PM-1b: ACC/AHA Stage 2 HBP Control SBP <130 mm Hg (Enhancing Measure)
PM-1b: Percentage of Patients 18 to 85 Years of Age Who Had a Diagnosis of ACC/AHA Stage 2 HBP and Whose SBP Was <130 mm Hg During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 2 HBP with SBP <130 mm Hg (harmonizes with current performance measure “Controlling High Blood Pressure” in widespread use) | |
| Numerator | Patients with SBP <130 mm Hg |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 2 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | Documentation of a medical reason (eg, treatment intolerance, significant risk of treatment intolerance, especially for frail patients ≥65 y of age) Documentation of a patient reason (eg, economic/access issues) |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of BP in patients with hypertension can help prevent cardiovascular events, including MI, stroke, and the development of HF, and reduce the risk of death from these complications. This performance measure enhances NCQA HEDIS 2019, ICSI, VHA, NQF Measure 0018, Medicaid, Medicare Physician QPP (formerly PQRS), MSSP, Million Hearts, physician feedback/QRUR, physician VBM, QHP, QRS commonly used in payment programs, public reporting, quality improvement (internal to the specific organization), and regulatory and accreditation programs. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. BP should be categorized as normal, elevated, or stage 1 or 2 hypertension to prevent and treat high BP.27–46 (Class 1, Level of Evidence: B-NR) | |
| 2. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
| 3. For adults with confirmed hypertension and known CVD or 10-year ASCVD event risk of 10% or higher, a BP target of less than 130/80 mm Hg is recommended.46,51–54 (Class 1, Level of Evidence: SBP: B-RSR, DBP: C-EO) | |
| 4. For older adults (≥65 y of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit are reasonable for decisions regarding intensity of BP lowering and choice of antihypertensive drugs. (Class 2a, Level of Evidence: C-EO) | |
| 5. Use of the EHR and patient registries is beneficial for identification of patients with undiagnosed or undertreated hypertension.55–57 (Class 1, Level of Evidence: B-NR) | |
| 6. Treatment of hypertension with a SBP treatment goal of less than 130 mm Hg is recommended for noninstitutionalized ambulatory community-dwelling adults (≥65 y of age) with an average SBP of 130 mm Hg or higher.58 (Class 1, Level of Evidence: A) | |
| 7. Adults with stage 2 hypertension should be evaluated by or referred to a primary care provider within 1 month of the initial diagnosis, have a combination of nonpharmacological and antihypertensive drug therapy (with 2 agents of different classes) initiated, and have a repeat BP evaluation in 1 month.59,60 (Class 1, Level of Evidence: B-R) | |
| 8. In adults with an untreated SBP greater than 130 mm Hg but less than 160 mm Hg or DBP greater than 80 mm Hg but less than 100 mm Hg, it is reasonable to screen for the presence of white coat hypertension by using either daytime ABPM or HBPM before diagnosis of hypertension.61–68 (Class 2a, Level of Evidence: B-NR) | |
Resources: 1) Qualified Electronic Health Record.69 2) PCPI National Quality Registry Network (NQRN).70 3) American College of Cardiology Foundation (ACCF) American Heart Association (AHA) Physician Consortium for Performance Improvement (PCPI) Hypertension Performance Measurement Set. 4) NQF Measure 0018 Controlling High Blood Pressure (NCQA).22
Additional note: 2017 Hypertension Clinical Practice Guidelines relies on average BP readings. NCQA HEDIS relies on most recent BP reading: The member is numerator compliant if the BP is <140/90 mm Hg. The member is not compliant if the BP is ≥140/90 mm Hg, if there is no BP reading during the measurement year, or if the reading is incomplete (eg, the systolic or diastolic level is missing). If there are multiple BPs on the same date of service, use the lowest systolic and diastolic BP on that date as the representative BP.
ABPM indicates ambulatory blood pressure monitoring; ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CVD, cardiovascular disease; DBP, diastolic blood pressure; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; HEDIS, Healthcare Effectiveness Data and Information Set; HF, heart failure; ICSI, Institute for Clinical Systems Improvement; MI, myocardial infarction; MSSP, Medicare Shared Savings Program; NCQA, National Committee for Quality Assurance; NMA, National Medical Association; NQF, National Quality Forum; PCPI, Physician Consortium for Performance Improvement; QCDR, Qualified Clinical Data Registry; QHP, Qualified Health Plan; QPP, Quality Payment Program; QRS, Quality Rating System; QRUR, Quality and Resource Use Reports; SBP, systolic blood pressure; VBM, Value-Based Payment Modifier; and VHA, Veterans Health Administration.
Short Title: PM-2: ACC/AHA Stage 1 HBP Control SBP <130 mm Hg (Harmonizing Measure)
PM-2: Percentage of Patients 18 to 85 Years of Age Who Had a Diagnosis of ACC/AHA Stage 1 HBP and Whose SBP Was <130 mm Hg During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 1 HBP with SBP <130 mm Hg (harmonizes with current performance measure “Controlling High Blood Pressure” for ACC/AHA stage 2 HBP currently in widespread use) | |
| Numerator | Patients with SBP <130 mm Hg |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 1 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | Documentation of a medical reason (eg, treatment intolerance, significant risk of treatment intolerance, especially for frail patients ≥65 y of age) Documentation of a patient reason (eg, economic/access issues) |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of BP in patients with hypertension can help prevent cardiovascular events, including MI, stroke, and the development of HF, and reduce the risk of death from these complications. This performance measure harmonizes and supplements the existing measure for stage 2 with NCQA HEDIS 2019 (currently in draft form for public comment), ICSI, VHA, NQF Measure 0018, Medicaid, Medicare Physician QPP (formerly PQRS), MSSP, Million Hearts, physician feedback/QRUR, physician VBM, QHP, QRS commonly used in payment programs, public reporting, quality improvement (internal to the specific organization), and regulatory and accreditation programs. There is currently no HEDIS or other standardized measurement of a national average rate of performance for stage 1 HBP | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. BP should be categorized as normal, elevated, or stage 1 or 2 hypertension to prevent and treat high BP.27–46 (Class 1, Level of Evidence: B-NR) | |
| 2. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
| 3. For adults with confirmed hypertension and known CVD or 10-year ASCVD event risk of 10% or higher, a BP target of less than 130/80 mm Hg is recommended.46,51–54 (Class 1, Level of Evidence: SBP: B-RSR, DBP: C-EO) | |
| 4. For older adults (≥65 y of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit are reasonable for decisions regarding intensity of BP lowering and choice of antihypertensive drugs. (Class 2a, Level of Evidence: C-EO) | |
| 5. Use of the EHR and patient registries is beneficial for identification of patients with undiagnosed or undertreated hypertension.55–57 (Class 1, Level of Evidence: B-NR) | |
| 6. Treatment of hypertension with a SBP treatment goal of less than 130 mm Hg is recommended for noninstitutionalized ambulatory community-dwelling adults (≥65 y of age) with an average SBP of 130 mm Hg or higher.58 (Class 1, Level of Evidence: A) | |
| 7. Adults with stage 2 hypertension should be evaluated by or referred to a primary care provider within 1 month of the initial diagnosis, have a combination of nonpharmacological and antihypertensive drug therapy (with 2 agents of different classes) initiated, and have a repeat BP evaluation in 1 month.59,60 (Class 1, Level of Evidence: B-R) | |
| 8. In adults with an untreated SBP greater than 130 mm Hg but less than 160 mm Hg or DBP greater than 80 mm Hg but less than 100 mm Hg, it is reasonable to screen for the presence of white coat hypertension by using either daytime ABPM or HBPM before diagnosis of hypertension.61–68 (Class 2a, Level of Evidence: B-NR) | |
Resources: 1) Qualified Electronic Health Record.69 2) PCPI National Quality Registry Network (NQRN).70 3) American College of Cardiology Foundation (ACCF) American Heart Association (AHA) Physician Consortium for Performance Improvement (PCPI) Hypertension Performance Measurement Set. 4) NQF Measure 0018 Controlling High Blood Pressure (NCQA).22
Additional note: 2017 Hypertension Clinical Practice Guidelines relies on average BP readings. NCQA HEDIS relies on most recent BP reading: The member is numerator compliant if the BP is <140/90 mm Hg. The member is not compliant if the BP is ≥140/90 mm Hg, if there is no BP reading during the measurement year, or if the reading is incomplete (eg, the systolic or diastolic level is missing). If there are multiple BPs on the same date of service, use the lowest systolic and diastolic BP on that date as the representative BP.
ABPM indicates ambulatory blood pressure monitoring; ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CVD, cardiovascular disease; DBP, diastolic blood pressure; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; HEDIS, Healthcare Effectiveness Data and Information Set; HF, heart failure; ICSI, Institute for Clinical Systems Improvement; MI, myocardial infarction; MSSP, Medicare Shared Savings Program; NCQA, National Committee for Quality Assurance; NQF, National Quality Forum; PCPI, Physician Consortium for Performance Improvement; QCDR, Qualified Clinical Data Registry; QHP, Qualified Health Plan; QPP, Quality Payment Program; QRS, Quality Rating System; QRUR, Quality and Resource Use Reports; SBP, systolic blood pressure; VBM, Value-Based Payment Modifier; and VHA, Veterans Health Administration.
Short Title: PM-3: ACC/AHA Stage 2 and Stage 1 HBP Control SBP <130 mm Hg (Composite Measure Combining PM-1b and PM-2)
PM-3: Percentage of Patients 18 to 85 years of Age Who Had a Diagnosis of Either ACC/AHA Stage 2 or Stage 1 HBP and Whose SBP Was <130 mm Hg During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 2 or stage 1 HBP with SBP <130 mm Hg (enhances current performance measure “Controlling High Blood Pressure” in widespread use based on current ACC/AHA guidelines by including patients with ACC/AHA stage 1 HBP) | |
| Numerator | Patients with SBP <130 mm Hg |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 2 or stage 1 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | Documentation of a medical reason (eg, treatment intolerance, significant risk of treatment intolerance, especially for frail patients ≥65 y of age) Documentation of a patient reason (eg, economic/access issues) |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of BP in patients with hypertension can help prevent cardiovascular events, including MI, stroke, and the development of HF, and reduce the risk of death from these complications. This performance measure harmonizes and supplements the existing measure for stage 2 with NCQA HEDIS 2019 (currently in draft form for public comment), ICSI, VHA, NQF Measure 0018, Medicaid, Medicare Physician QPP (formerly PQRS), MSSP, Million Hearts, physician feedback/QRUR, physician VBM, QHP, QRS commonly used in payment programs, public reporting, quality improvement (internal to the specific organization), and regulatory and accreditation programs. There is currently no HEDIS or other standardized composite measurement of a national average rate of performance for stage 2 and stage 1 HBP combined. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. BP should be categorized as normal, elevated, or stage 1 or 2 hypertension to prevent and treat high BP.27–46 (Class 1, Level of Evidence: B-NR) | |
| 2. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
| 3. For adults with confirmed hypertension and known CVD or 10-y ASCVD event risk of 10% or higher, a BP target of less than 130/80 mm Hg is recommended.46,51–54 (Class 1, Level of Evidence: SBP: B-RSR, DBP: C-EO) | |
| 4. For older adults (≥65 y of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit are reasonable for decisions regarding intensity of BP lowering and choice of antihypertensive drugs. (Class 2a, Level of Evidence: C-EO) | |
| 5. Use of the EHR and patient registries is beneficial for identification of patients with undiagnosed or undertreated hypertension.55–57 (Class 1, Level of Evidence: B-NR) | |
| 6. Treatment of hypertension with a SBP treatment goal of less than 130 mm Hg is recommended for noninstitutionalized ambulatory community-dwelling adults (≥65 y of age) with an average SBP of 130 mm Hg or higher.58 (Class 1, Level of Evidence: A) | |
| 7. Adults with stage 2 hypertension should be evaluated by or referred to a primary care provider within 1 month of the initial diagnosis, have a combination of nonpharmacological and antihypertensive drug therapy (with 2 agents of different classes) initiated, and have a repeat BP evaluation in 1 month.59,60 (Class 1, Level of Evidence: B-R) | |
| 8. In adults with an untreated SBP greater than 130 mm Hg but less than 160 mm Hg or DBP greater than 80 mm Hg but less than 100 mm Hg, it is reasonable to screen for the presence of white coat hypertension by using either daytime ABPM or HBPM before diagnosis of hypertension.61–68 (Class 2a, Level of Evidence: B-NR) | |
Resources: 1) Qualified Electronic Health Record.69 2) PCPI National Quality Registry Network (NQRN).70 3) American College of Cardiology Foundation (ACCF) American Heart Association (AHA) Physician Consortium for Performance Improvement (PCPI) Hypertension Performance Measurement Set. 4) NQF Measure 0018 Controlling High Blood Pressure (NCQA).22
Additional note: 2017 Hypertension Clinical Practice Guidelines relies on average BP readings. NCQA HEDIS relies on most recent BP reading: The member is numerator compliant if the BP is <140/90 mm Hg. The member is not compliant if the BP is ≥140/90 mm Hg, if there is no BP reading during the measurement year, or if the reading is incomplete (eg, the systolic or diastolic level is missing). If there are multiple BPs on the same date of service, use the lowest systolic and diastolic BP on that date as the representative BP.
ABPM indicates ambulatory blood pressure monitoring; ACC, American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CVD, cardiovascular disease; DBP, diastolic blood pressure; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; HEDIS, Healthcare Effectiveness Data and Information Set; HF, heart failure; ICSI, Institute for Clinical Systems Improvement; MI, myocardial infarction; MSSP, Medicare Shared Savings Program; NCQA, National Committee for Quality Assurance; NQF, National Quality Forum; PCPI, Physician Consortium for Performance Improvement; QCDR, Qualified Clinical Data Registry; QHP, Qualified Health Plan; QPP, Quality Payment Program; QRS, Quality Rating System; QRUR, Quality and Resource Use Reports; SBP, systolic blood pressure; VBM, Value-Based Payment Modifier; and VHA, Veterans Health Administration.
Short Title: PM-4: Nonpharmacological Interventions for ACC/AHA Stage 2 HBP
PM-4: Percentage of Adults 18 to 85 Years of Age Who Had a Diagnosis of ACC/AHA Stage 2 HBP Who Have Documentation of a Discussion of Intensive Lifestyle Modification With Their Healthcare Providers During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 2 HBP who have a documented discussion of intensive lifestyle modification in ≥1 visits during the measurement year | |
| Numerator | Patients who have a documented discussion of intensive lifestyle modification at least once in the performance year and in accordance with ACC/AHA guidelines on nonpharmacological therapy |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 2 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | BP readings taken during an inpatient stay |
| Denominator Exceptions | None |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Nonpharmacological therapy in combination with drug therapy is an integral part of management of ACC/AHA stage 2 hypertension. Prompt and frequent discussion of lifestyle modification among patients with ACC/AHA stage 2 hypertension is important because of the elevated risk of ASCVD events. Dietary modification is a fundamental approach to the prevention and management of hypertension and complements pharmacological management of hypertension. The DASH diet, which is high in fruits, vegetables, potassium, calcium, magnesium, and fiber and low in saturated and total fat, has been demonstrated to be effective in lowering BP. Among those diagnosed with hypertension, the DASH diet produces, on average, overall reductions in SBP and DBP and is particularly effective among black patients.71 Conversely, among blacks, a US Southern-style diet characterized by high intake of fried foods, organ meats, processed meats, added fats, high-fat dairy foods, sugar-sweetened beverages, and bread contributes to the disproportionate burden of hypertension.72 The Mediterranean,73,74 low-carbohydrate,75 high-protein,76 and vegetarian dietary patterns77 have been demonstrated to lower BP. There is a strong and dose-dependent association between excessive alcohol consumption (>3 standard drinks per day) and BP. | |
| There is strong evidence that adequate physical activity lowers BP. The average reductions in SBP with aerobic exercise are approximately 2–4 mm Hg and 5–8 mm Hg in adult patients who are normotensive and hypertensive, respectively. In patients with elevated BP, weight loss has been demonstrated to lower BP, with a dose-response relationship of about 1 mm Hg per kilogram of weight loss. Among patients who do not achieve weight-loss goals, pharmacological therapy or surgical procedures may be considered, with careful consideration of complications. SDM78,79 between the provider and patient should be considered in selecting specific lifestyle interventions, with consideration of the patient’s individual values, preferences, socioeconomic status, associated conditions, and comorbidities to enhance adherence to lifestyle modification. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, that facilitates achieving a desirable weight is recommended for adults with elevated BP or hypertension.80–82 (Class 1, Level of Evidence: A) | |
| 2. Sodium reduction is recommended for adults with elevated BP or hypertension.83–87 (Class 1, Level of Evidence: A) | |
| 3. Potassium supplementation, preferably in dietary modification, is recommended for adults with elevated BP or hypertension, unless contraindicated by the presence of CKD or use of drugs that reduce potassium excretion.88–92 (Class 1, Level of Evidence: A) | |
| 4. Adult men and women with elevated BP or hypertension who currently consume alcohol should be advised to drink no more than 2 and 1 standard drinks* per day, respectively.93–98 (Class 1, Level of Evidence: A) | |
| 5. Increased physical activity with a structured exercise program is recommended for adults with elevated BP or hypertension.87,99–105 (Class 1, Level of Evidence: | |
| 6. Weight loss is recommended to reduce BP in adults with elevated BP or hypertension who are overweight or obese.99,100,106,107 (Class 1, Level of Evidence: A) | |
| 7. Effective behavioral and motivational strategies to achieve a healthy lifestyle (ie, tobacco cessation, weight loss, moderation in alcohol intake, increased physical activity, reduced sodium intake, and consumption of a healthy diet) are recommended for adults with hypertension.108,109 (Class 1, Level of Evidence: C-EO) | |
In the United States, 1 “standard” drink contains roughly 14 g of pure alcohol, which is typically found in 12 oz of regular beer (usually about 5% alcohol), 5 oz of wine (usually about 12% alcohol), and 1.5 oz of distilled spirits (usually about 40% alcohol).
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CKD, chronic kidney disease; DASH, Dietary Approaches to Stop Hypertension; DBP, diastolic blood pressure; HBP, high blood pressure; QCDR, Qualified Clinical Data Registry; SBP, systolic blood pressure; and SDM, shared decision making.
Short Title: PM-5: Use of HBPM for Management of ACC/AHA Stage 2 HBP
PM-5: Use of HBPM for Management of ACC/AHA Stage 2 HBP
| Measure Description: Percentage of patients who had a diagnosis of ACC/AHA stage 2 HBP for whom HBPM is recommended and HBPM data are documented in the patient record | |
| Numerator | Documentation of home BP readings in the medical record |
| Denominator | All patients 18–85 y of age who had a diagnosis of ACC/AHA stage 2 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | Documentation of a patient reason (eg, economic issues, refusal, cognitive deficits) |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| HBPM or self-monitoring of BP refers to the regular measurement of BP by an individual at home or elsewhere outside the clinic setting. Home-based measurement has been found to be a better predictor of cardiovascular risk than clinic-based measurement. Evidence also suggests that home-based BP measurement in combination interventions with telemedicine with nurse- or pharmacist-led care may be effective for improving hypertension management. | |
| Procedures for Use of HBPM4 | |
| Patient training should occur under medical supervision, including: | |
| • Information about hypertension | |
| • Selection of equipment | |
| • Acknowledgment that individual BP readings may vary substantially | |
| • Interpretation of results | |
| Devices: | |
| • Verify use of automated validated devices. Use of auscultatory devices (mercury, aneroid, or other) is not generally useful for HBPM because patients rarely master the technique required for measurement of BP with auscultatory devices. | |
| • Monitors with provision for storage of readings in memory are preferred. | |
| • Verify use of appropriate cuff size to fit the arm. | |
| • Verify that left/right inter-arm differences are insignificant. If differences are significant, instruct patient to measure BPs in the arm with higher readings. | |
| Instructions on HBPM procedures: | |
| • Remain still: | |
| - Avoid smoking, caffeinated beverages, or exercise within 30 min before BP measurements. | |
| - Ensure ≥5 min of quiet rest before BP measurements. | |
| • Sit correctly: | |
| - Sit with back straight and supported (on a straight-backed dining chair, for example, rather than a sofa). | |
| - Sit with feet flat on the floor and legs uncrossed. | |
| - Keep arm supported on a flat surface (such as a table), with the upper arm at heart level. | |
| • Bottom of the cuff should be placed directly above the antecubital fossa (bend of the elbow). | |
| • Take multiple readings: | |
| - Take at least 2 readings 1 min apart in morning before taking medications and in evening before supper. Optimally, measure and record BP daily. Ideally, obtain weekly BP readings beginning 2 wk after a change in the treatment regimen and during the week before a clinic visit. | |
| • Record all readings accurately: | |
| - Monitors with built-in memory should be brought to all clinic appointments. | |
| - BP should be based on an average of readings on ≥2 occasions for clinical decision making. | |
| Clinical Recommendation | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; BP, blood pressure; HBP, high blood pressure; HBPM, home blood pressure monitoring; and QCDR, Qualified Clinical Data Registry.
Process Quality Measures
Short Title: QM-1: Nonpharmacological Interventions for ACC/AHA Stage Elevated BP
QM-1: Percentage of Adults 18 to 85 Years of Age Who Had a Diagnosis of ACC/AHA Stage Elevated BP Who Have a Documented Discussion of Intensive Lifestyle Modification in ≥1 Visits During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage elevated BP who have a documented discussion of intensive lifestyle modification in ≥1 visits during the measurement year | |
| Numerator | Patients who have a documented discussion of intensive lifestyle modification at least once in the performance year and in accordance with ACC/AHA guidelines on nonpharmacological therapy |
| Denominator | All patients 18–85 y of age who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | Pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | None |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of elevated BP requires intensive lifestyle modification. In those diagnosed with elevated BP, nonpharmacological therapy is useful in preventing ACC/AHA stage 1 or 2 hypertension. Dietary modification is a fundamental approach to the prevention and management of elevated BP and complements pharmacological management of hypertension. The DASH diet, which is high in fruits, vegetables, potassium, calcium, magnesium, and fiber and low in saturated and total fat, has been demonstrated to be effective in lowering BP Among those diagnosed with hypertension, the DASH diet produces, on average, overall reductions in SBP and is particularly effective among black patients.71 Conversely, among blacks, a US Southern-style diet characterized by high intake of fried foods, organ meats, processed meats, added fats, high-fat dairy foods, sugar-sweetened beverages, and bread contributes to the disproportionate burden of hypertension.72 The Mediterranean,73,74 low-carbohydrate,75 high-protein,76 and vegetarian dietary patterns77 have been demonstrated to lower BP. There is a strong and dose-dependent association between excessive alcohol consumption (>3 standard drinks per day) and BP. | |
| There is strong evidence that adequate physical activity lowers BP. The average reductions in SBP with aerobic exercise are approximately 2–4 mm Hg and 5–8 mm Hg in adult patients who are normotensive and hypertensive, respectively. In patients with ACC/AHA elevated BP, weight loss has been demonstrated to lower BP, with a dose-response relationship of about 1 mm Hg per kilogram of weight loss. Among patients who do not achieve weight-loss goals, pharmacological therapy or surgical procedures may be considered, with careful consideration of complications. SDM78,79 between the provider and patient should be considered in selecting specific lifestyle interventions, with consideration of the patient’s individual values, preferences, socioeconomic status, associated conditions, and comorbidities to enhance adherence to lifestyle modification. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, that facilitates achieving a desirable weight is recommended for adults with elevated BP or hypertension.80–82 (Class 1, Level of Evidence: A) | |
| 2. Sodium reduction is recommended for adults with elevated BP or hypertension.83–87 (Class 1, Level of Evidence: A) | |
| 3. Potassium supplementation, preferably in dietary modification, is recommended for adults with elevated BP or hypertension, unless contraindicated by the presence of CKD or use of drugs that reduce potassium excretion.88–92 (Class 1, Level of Evidence: A) | |
| 4. Adult men and women with elevated BP or hypertension who currently consume alcohol should be advised to drink no more than 2 and 1 standard drinks* per day, respectively.93–98 (Class 1, Level of Evidence: A) | |
| 5. Increased physical activity with a structured exercise program is recommended for adults with elevated BP or hypertension.87,99–105 (Class 1, Level of Evidence: A) | |
| 6. Weight loss is recommended to reduce BP in adults with elevated BP or hypertension who are overweight or obese.99,100,106,107 (Class 1, Level of Evidence: A) | |
| 7. Effective behavioral and motivational strategies to achieve a healthy lifestyle (ie, tobacco cessation, weight loss, moderation in alcohol intake, increased physical activity, reduced sodium intake, and consumption of a healthy diet) are recommended for adults with hypertension.108,109 (Class 1, Level of Evidence: C-EO) | |
| 8. Adults with an elevated BP or stage 1 hypertension who have an estimated 10-y ASCVD risk less than 10% should be managed with nonpharmacological therapy and have a repeat BP evaluation within 3 to 6 months.59,60 (Class 1, Level of Evidence: B-R) | |
In the United States, 1 “standard” drink contains roughly 14 g of pure alcohol, which is typically found in 12 oz of regular beer (usually about 5% alcohol), 5 oz of wine (usually about 12% alcohol), and 1.5 oz of distilled spirits (usually about 40% alcohol).
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CKD, chronic kidney disease; DASH, Dietary Approaches to Stop Hypertension; HBP, high blood pressure; QCDR, Qualified Clinical Data Registry; SBP, systolic blood pressure; and SDM, shared decision making.
Short Title: QM-2: Nonpharmacological Interventions for ACC/AHA Stage 1 HBP
QM-2: Percentage of Adults 18 to 85 Years of Age Who Had a Diagnosis of ACC/AHA Stage 1 HBP Who Have a Documented Discussion of Intensive Lifestyle Modification in ≥1 Visits During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 1 HBP who have a documented discussion of intensive lifestyle modification in ≥1 visits during the measurement year | |
| Numerator | Patients who have a documented discussion of intensive lifestyle modification at least once in the performance year and in accordance with ACC/AHA guidelines on nonpharmacological therapy |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 1 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | Pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | None |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of ACC/AHA stage 1 hypertension requires intensive lifestyle modification. Among patients with ACC/AHA stage 1 hypertension with ASCVD risk ≥10%, nonpharmacological therapy should be used in addition to pharmacological therapy as first-line therapy. Lifestyle modification is also a fundamental approach to prevention and management of ACC/AHA stage 1 BP and complements pharmacological management of hypertension. The DASH diet, which is high in fruits, vegetables, potassium, calcium, magnesium, and fiber and low in saturated and total fat, has been demonstrated to be effective in lowering BP. Among those diagnosed with hypertension, the DASH diet produces, on average, overall reductions in SBP and is particularly effective among black patients.71 Conversely, among blacks, a US Southern-style diet characterized by high intake of fried foods, organ meats, processed meats, added fats, high-fat dairy foods, sugar-sweetened beverages, and bread contributes to the disproportionate burden of hypertension.72 The Mediterranean,73,74 low-carbohydrate,75 high-protein,76 and vegetarian dietary patterns77 have been demonstrated to lower BP. There is a strong and dose-dependent association between excessive alcohol consumption (>3 standard drinks per day) and BP. | |
| There is strong evidence that adequate physical activity lowers BP. The average reductions in SBP with aerobic exercise are approximately 2–4 mm Hg and 5–8 mm Hg in adult patients who are normotensive and hypertensive, respectively. In patients with elevated BP, weight loss has been demonstrated to lower BP, with a dose-response relationship of about 1 mm Hg per kilogram of weight loss. Among patients who do not achieve weight-loss goals, pharmacological therapy or surgical procedures may be considered, with careful consideration of complications. SDM78,79 between the provider and patient should be considered in selecting specific lifestyle interventions, with consideration of the patient’s individual values, preferences, socioeconomic status, associated conditions, and comorbidities to enhance adherence to lifestyle modification. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, that facilitates achieving a desirable weight is recommended for adults with elevated BP or hypertension.80–82 (Class 1, Level of Evidence: A) | |
| 2. Sodium reduction is recommended for adults with elevated BP or hypertension.83–87 (Class 1, Level of Evidence: A) | |
| 3. Potassium supplementation, preferably in dietary modification, is recommended for adults with elevated BP or hypertension, unless contraindicated by the presence of CKD or use of drugs that reduce potassium excretion.88–92 (Class 1, Level of Evidence: A) | |
| 4. Adult men and women with elevated BP or hypertension who currently consume alcohol should be advised to drink no more than 2 and 1 standard drinks* per day, respectively.93–98 (Class 1, Level of Evidence: A) | |
| 5. Increased physical activity with a structured exercise program is recommended for adults with elevated BP or hypertension.87,99–105 (Class 1, Level of Evidence: A) | |
| 6. Weight loss is recommended to reduce BP in adults with elevated BP or hypertension who are overweight or obese.99,100,106,107 (Class 1, Level of Evidence: A) | |
| 7. Effective behavioral and motivational strategies to achieve a healthy lifestyle (ie, tobacco cessation, weight loss, moderation in alcohol intake, increased physical activity, reduced sodium intake, and consumption of a healthy diet) are recommended for adults with hypertension.108,109 (Class 1, Level of Evidence: C-EO) | |
| 8. Adults with an elevated BP or stage 1 hypertension who have an estimated 10-y ASCVD risk less than 10% should be managed with nonpharmacological therapy and have a repeat BP evaluation within 3 to 6 months.59,60 (Class 1, Level of Evidence: B-R) | |
| 9. Adults with stage 1 hypertension who have an estimated 10-y ASCVD risk of 10% or higher should be managed initially with a combination of nonpharmacological and antihypertensive drug therapy and have a repeat BP evaluation in 1 month.59,60 (Class 1, Level of Evidence: B-R) | |
In the United States, 1 “standard” drink contains roughly 14 g of pure alcohol, which is typically found in 12 oz of regular beer (usually about 5% alcohol), 5 oz of wine (usually about 12% alcohol), and 1.5 oz of distilled spirits (usually about 40% alcohol).
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CKD, chronic kidney disease; DASH, Dietary Approaches to Stop Hypertension; HBP, high blood pressure; QCDR, Qualified Clinical Data Registry; SBP, systolic blood pressure; and SDM, shared decision making.
Short Title: QM-3: Nonpharmacological Interventions for All ACC/AHA Stages of HBP (Composite Measure Combining PM-4, QM-1, and QM-2)
QM-3: Percentage of Adults 18 to 85 Years of Age Who Had a Diagnosis of Any ACC/AHA Stage of HBP (Elevated BP, Stage 1 HBP, or Stage 2 HBP) Who Have a Documented Discussion of Intensive Lifestyle Modification in ≥1 Visits During the Measurement Year
| Measure Description: Percentage of patients with any ACC/AHA stage of HBP (elevated BP, stage 1 HBP, or stage 2 HBP) who have a documented discussion of intensive lifestyle modification in ≥1 visits during the measurement year | |
| Numerator | Patients who have a documented discussion of intensive lifestyle modification at least once in the performance year and in accordance with ACC/AHA guidelines on nonpharmacological therapy |
| Denominator | All patients 18–85 y of age with any ACC/AHA stage of HBP (elevated BP, stage 1 HBP, or stage 2 HBP) who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | BP readings taken during an inpatient stay |
| Denominator Exceptions | None |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Effective management of HBP requires intensive lifestyle modification. Dietary modification is a fundamental approach to prevention and management of elevated BP and complements pharmacological management of hypertension. The DASH diet, which is high in fruits, vegetables, potassium, calcium, magnesium, and fiber and low in saturated and total fat, has been demonstrated to be effective in lowering BP. Among those diagnosed with hypertension, the DASH diet produces, on average, overall reductions in SBP and is particularly effective among black patients.71 Conversely, among blacks, a US Southern- style diet characterized by high intake of fried foods, organ meats, processed meats, added fats, high-fat dairy foods, sugar-sweetened beverages, and bread contributes to the disproportionate burden of hypertension.72 The Mediterranean,73,74 low-carbohydrate,75 high-protein,76 and vegetarian dietary patterns77 have been demonstrated to lower BP. There is a strong and dose-dependent association between excessive alcohol consumption (>3 standard drinks per day) and BP. | |
| There is strong evidence that adequate physical activity lowers BP. The average reductions in SBP with aerobic exercise are approximately 2–4 mm Hg and 5–8 mm Hg in adult patients who are normotensive and hypertensive, respectively. In patients with elevated BP, weight loss has been demonstrated to lower BP, with a dose-response relationship of about 1 mm Hg per kilogram of weight loss. Among patients who do not achieve weight-loss goals, pharmacological therapy or surgical procedures may be considered, with careful consideration of complications. SDM78,79 between the provider and patient should be considered in selecting specific lifestyle interventions, with consideration of the patient’s individual values, preferences, socioeconomic status, associated conditions, and comorbidities to enhance adherence to lifestyle modification. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. A heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, that facilitates achieving a desirable weight is recommended for adults with elevated BP or hypertension.80–82 (Class 1, Level of Evidence: A) | |
| 2. Sodium reduction is recommended for adults with elevated BP or hypertension.83–87 (Class 1, Level of Evidence: A) | |
| 3. Potassium supplementation, preferably in dietary modification, is recommended for adults with elevated BP or hypertension, unless contraindicated by the presence of CKD or use of drugs that reduce potassium excretion.88–92 (Class 1, Level of Evidence: A) | |
| 4. Adult men and women with elevated BP or hypertension who currently consume alcohol should be advised to drink no more than 2 and 1 standard drinks* per day, respectively.93–98 (Class 1, Level of Evidence: A) | |
| 5. Increased physical activity with a structured exercise program is recommended for adults with elevated BP or hypertension.87,99–105 (Class 1, Level of Evidence: A) | |
| 6. Weight loss is recommended to reduce BP in adults with elevated BP or hypertension who are overweight or obese.99,100,106,107 (Class 1, Level of Evidence: A) | |
| 7. Effective behavioral and motivational strategies to achieve a healthy lifestyle (ie, tobacco cessation, weight loss, moderation in alcohol intake, increased physical activity, reduced sodium intake, and consumption of a healthy diet) are recommended for adults with hypertension.108,109 (Class 1, Level of Evidence: C-EO) | |
| 8. Adults with an elevated BP or stage 1 hypertension who have an estimated 10-y ASCVD risk less than 10% should be managed with nonpharmacological therapy and have a repeat BP evaluation within 3 to 6 months.59,60 (Class 1, Level of Evidence: B-R) | |
| 9. Adults with stage 1 hypertension who have an estimated 10-y ASCVD risk of 10% or higher should be managed initially with a combination of nonpharmacological and antihypertensive drug therapy and have a repeat BP evaluation in 1 month.59,60 (Class 1, Level of Evidence: B-R) | |
In the United States, 1 “standard” drink contains roughly 14 g of pure alcohol, which is typically found in 12 oz of regular beer (usually about 5% alcohol), 5 oz of wine (usually about 12% alcohol), and 1.5 oz of distilled spirits (usually about 40% alcohol).
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CKD, chronic kidney disease; DASH, Dietary Approaches to Stop Hypertension; HBP, high blood pressure; QCDR, Qualified Clinical Data Registry; SBP, systolic blood pressure; and SDM, shared decision making.
Short Title: QM-4: Medication Adherence to Drug Therapy for ACC/AHA Stage 1 With ASCVD Risk ≥10% or ACC/AHA Stage 2 HBP
QM-4: Percentage of Adults 18 to 85 Years of Age Who Had a Diagnosis of ACC/AHA Stage 1 HBP With ASCVD Risk ≥10% or ACC/AHA Stage 2 HBP With ≥1 Prescriptions for BP Medication Who Had ≥80% Adherence to BP Medication(s) During the Measurement Year
| Measure Description: Percentage of patients with ACC/AHA stage 1 HBP and ASCVD risk ≥10% or ACC/AHA stage 2 HBP who had ≥80% adherence to prescribed BP medication(s) during the measurement year | |
| Numerator | Patients with ≥1 prescriptions for BP medication(s) who met the PDC threshold of ≥80% during the measurement year |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 1 HBP and ASCVD risk ≥10% or ACC/AHA stage 2 HBP who had at least 1 outpatient encounter with a diagnosis of HBP and had ≥1 or more prescriptions for BP medications during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay, patients solely on nonpharmacological therapy |
| Denominator Exceptions | Documentation of a medical reason (eg, treatment intolerance, significant risk of treatment intolerance, especially for frail patients ≥65 y of age) Documentation of a patient reason (eg, economic/access issues) |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Medicaid claims data, commercial claims data, Medicare claims data, Tricare claims data |
| Attribution | Physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| Adherence to drug therapy lowers BP and reduces the risk of cardiovascular events and death.110–112 As many as 50% to 80% of patients prescribed antihypertensive medications demonstrate suboptimal adherence.113 Adherence to drug therapy is influenced by several interrelated factors, including large pill burden, complex drug regimen, cost of medications, side effects of multidrug antihypertensive regimens, poor patient-provider relationship, and clinical inertia.114 | |
| No single strategy has been found to be more effective than others in improving adherence, but rather, a combination of patient-level, provider-level, and system-level strategies is likely to be the most effective. Medication adherence is highest with once-daily dosing and declines within increasing dosing frequency.115,116 Medication adherence tools, such as the Hill-Bone Compliance to HBP Therapy Scale,117 may be used to identify barriers to medication adherence, in combination with other more objective methods, such as pill counts and data on medication refills. PDC is one of the most popular methods to calculate medication adherence and is endorsed and validated by the PQA as a high-quality measure of medication adherence.118,119* | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. In adults with hypertension, dosing of antihypertensive medication once daily rather than multiple times daily is beneficial to improve adherence.115,116,120 (Class 1, Level of Evidence: B-R) | |
| 2. Adults initiating a new or adjusted drug regimen for hypertension should have a follow-up evaluation of adherence and response to treatment at monthly intervals until control is achieved.59,60,121 (Class 1, Level of Evidence: B-R) | |
| 3. Use of BP-lowering medications is recommended for secondary prevention of recurrent CVD events in patients with clinical CVD and an average SBP of 130 mm Hg or higher or an average DBP of 80 mm Hg or higher, and for primary prevention in adults with an estimated 10-y atherosclerotic cardiovascular disease (ASCVD) risk of 10% or higher and an average SBP 130 mm Hg or higher or an average DBP 80 mm Hg or higher.29,37,42,43,46,122–125 (Class 1, Level of Evidence: SBP: A, DBP: C-EO) | |
| 4. Use of BP-lowering medication is recommended for primary prevention of CVD in adults with no history of CVD and with an estimated 10-y ASCVD risk <10% and an SBP of 140 mm Hg or higher or a DBP of 90 mm Hg or higher.39,125–128 (Class 1, Level of Evidence: C-LD) | |
| 5. Initiation of antihypertensive drug therapy with 2 first-line agents of different classes, either as separate agents or in a fixed-dose combination, is recommended in adults with stage 2 hypertension and an average BP more than 20/10 mm Hg above their BP target. (Class 1, Level of Evidence: C-EO) | |
| 6. Use of combination pills rather than free individual components can be useful to improve adherence to antihypertensive therapy.129–132 (Class 2a, Level of Evidence: B-NR) | |
| 7. Initiation of antihypertensive drug therapy with a single antihypertensive drug is reasonable in adults with stage 1 hypertension and BP goal <130/80 mm Hg with dosage titration and sequential addition of other agents to achieve the BP target. (Class 2a, Level of Evidence: C-EO) | |
We encourage stratification by clinically relevant subsets, such as stage 1 with ASCVD risk ≥10, or stage 2, for quality improvement efforts.
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CVD, cardiovascular disease; DBP, diastolic blood pressure; HBP, high blood pressure; PDC, proportion of days covered; PQA, Pharmacy Quality Alliance; and SBP, systolic blood pressure.
Short Title: QM-5: Use of HBPM for Management of ACC/AHA Stage 1 HBP
QM-5: Use of HBPM for Management of ACC/AHA Stage 1 HBP
| Measure Description: Percentage of patients 18–85 y of age who had a diagnosis of ACC/AHA stage 1 HBP for whom HBPM is recommended and HBPM data are documented in the patient record | |
| Numerator | Documentation of home BP readings in the medical record |
| Denominator | All patients 18–85 y of age with ACC/AHA stage 1 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | None |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| HBPM or self-monitoring of BP refers to the regular measurement of BP by an individual at home or elsewhere outside the clinic setting. Home-based measurement has been found to be a better predictor of cardiovascular risk than clinic-based measurement. Evidence also suggests that home-based BP measurement in combination interventions with telemedicine with nurse- or pharmacist-led care may be effective for improving hypertension management. | |
| Recommended procedures for the collection of HBPM data are as follows4: | |
| Patient training should occur under medical supervision, including: | |
| • Information about hypertension | |
| • Selection of equipment | |
| • Acknowledgment that individual BP readings may vary substantially | |
| • Interpretation of results | |
| Devices: | |
| • Verify use of automated validated devices. Use of auscultatory devices (mercury, aneroid, or other) is not generally useful for HBPM because patients rarely master the technique required for measurement of BP with auscultatory devices. | |
| • Monitors with provision for storage of readings in memory are preferred. | |
| • Verify use of appropriate cuff size to fit the arm. | |
| • Verify that left/right inter-arm differences are insignificant. If differences are significant, instruct patient to measure BPs in the arm with higher readings. | |
| Instructions on HBPM procedures: | |
| • Remain still: | |
| - Avoid smoking, caffeinated beverages, or exercise within 30 min before BP measurements. | |
| - Ensure ≥5 min of quiet rest before BP measurements. | |
| • Sit correctly: | |
| - Sit with back straight and supported (on a straight-backed dining chair, for example, rather than a sofa). | |
| - Sit with feet flat on the floor and legs uncrossed. | |
| - Keep arm supported on a flat surface (such as a table), with the upper arm at heart level. | |
| • Bottom of the cuff should be placed directly above the antecubital fossa (bend of the elbow). | |
| • Take multiple readings: | |
| - Take at least 2 readings 1 min apart in morning before taking medications and in evening before supper. Optimally, measure and record BP daily. Ideally, obtain weekly BP readings beginning 2 wk after a change in the treatment regimen and during the week before a clinic visit. | |
| • Record all readings accurately: | |
| - Monitors with built-in memory should be brought to all clinic appointments. | |
| - BP should be based on an average of readings on ≥2 occasions for clinical decision making. | |
| Clinical Recommendation | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; BP, blood pressure; HBP, high blood pressure; HBPM, home blood pressure monitoring; and QCDR, Qualified Clinical Data Registry.
Short Title: QM-6: Use of HBPM for Management of ACC/AHA Stage 1 or ACC/AHA Stage 2 (Composite Measure Combining PM-5 and QM-5)
QM-6: Use of HBPM for Management of ACC/AHA Stage 1 HBP or ACC/AHA Stage 2 HBP (Composite Measure Combining PM-5 and Process QM-5)
| Measure Description: Percentage of patients 18–85 y of age who had a diagnosis of either ACC/AHA stage 1 HBP or ACC/AHA stage 2 HBP for whom HBPM is recommended and HBPM data are documented in the patient record | |
| Numerator | Documentation of home BP readings in the medical record |
| Denominator | All patients 18–85 y of age who had a diagnosis of either ACC/AHA stage 1 HBP or ACC/AHA stage 2 HBP who had at least 1 outpatient encounter with a diagnosis of HBP during the first 6 mo of the measurement year or any time before the measurement period |
| Denominator Exclusions | End-stage renal disease, kidney transplantation, pregnancy, BP readings taken during an inpatient stay |
| Denominator Exceptions | None |
| Measurement Period | 12 mo/measurement year |
| Sources of Data | Paper medical record/prospective data collection flow sheet, Qualified Electronic Health Record, QCDR, electronic administrative data (claims), expanded (multiple source) administrative data, electronically or telephonically transmitted BP readings |
| Attribution | Healthcare provider (healthcare provider, physician group practice, accountable care organization, clinically integrated network, health plan, integrated delivery system) |
| Care Setting | Outpatient (office, clinic, home, or ambulatory) |
| Rationale | |
| HBPM or self-monitoring of BP refers to the regular measurement of BP by an individual at home or elsewhere outside the clinic setting. Home-based measurement has been found to be a better predictor of cardiovascular risk than clinic-based measurement. Evidence also suggests that home-based BP measurement in combination interventions with telemedicine with nurse- or pharmacist-led care may be effective for improving hypertension management. | |
| Recommended procedures for the collection of HBPM data are as follows4: | |
| Patient training should occur under medical supervision, including: | |
| • Information about hypertension | |
| • Selection of equipment | |
| • Acknowledgment that individual BP readings may vary substantially | |
| • Interpretation of results | |
| Devices: | |
| • Verify use of automated validated devices. Use of auscultatory devices (mercury, aneroid, or other) is not generally useful for HBPM because patients rarely master the technique required for measurement of BP with auscultatory devices. | |
| • Monitors with provision for storage of readings in memory are preferred. | |
| • Verify use of appropriate cuff size to fit the arm. | |
| • Verify that left/right inter-arm differences are insignificant. If differences are significant, instruct patient to measure BPs in the arm with higher readings. | |
| Instructions on HBPM procedures: | |
| • Remain still: | |
| - Avoid smoking, caffeinated beverages, or exercise within 30 min before BP measurements. | |
| - Ensure ≥5 min of quiet rest before BP measurements. | |
| • Sit correctly: | |
| - Sit with back straight and supported (on a straight-backed dining chair, for example, rather than a sofa). | |
| - Sit with feet flat on the floor and legs uncrossed. | |
| - Keep arm supported on a flat surface (such as a table), with the upper arm at heart level. | |
| • Bottom of the cuff should be placed directly above the antecubital fossa (bend of the elbow). | |
| • Take multiple readings: | |
| - Take at least 2 readings 1 min apart in morning before taking medications and in evening before supper. Optimally, measure and record BP daily. Ideally, obtain weekly BP readings beginning 2 wk after a change in the treatment regimen and during the week before a clinic visit. | |
| • Record all readings accurately: | |
| - Monitors with built-in memory should be brought to all clinic appointments. | |
| - BP should be based on an average of readings on ≥2 occasions for clinical decision making. | |
| Clinical Recommendation | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| 1. Out-of-office BP measurements are recommended to confirm the diagnosis of hypertension and for titration of BP-lowering medication, in conjunction with telehealth counseling or clinical interventions.47–50 (Class 1, Level of Evidence: ASR) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; BP, blood pressure; HBP, high blood pressure; HBPM, home blood pressure monitoring; and QCDR, Qualified Clinical Data Registry.
Structural Qualipty Measures
The Structural Quality Measure domain should be considered to be at the CDU level (can be a physician group practice, accountable care organization, clinically integrated network, health plan, or integrated delivery system), as opposed to the specific patient or physician/clinician level. The goal will be to guide and motivate CDUs to implement and evaluate these specific guideline recommendations to improve the various and necessary evidence-based components of a guideline-driven system of care and accompanying infrastructure needed for effective identification and management of patients with HBP.
Diagnosis, Assessment, and Accurate Measurement
SM-1: Use of a Standard Protocol to Consistently and Correctly Measure BP in the Ambulatory Setting
| Measure Components | The CDU uses a standard process/protocol for properly measuring BP consistently and correctly, including: |
| • Adoption and implementation of a protocol for accurate measurement and documentation of BP. | |
| • Availability of staff who are trained in measurement and documentation of BP. | |
| • Documentation of staff assessment of correct BP measurement skill. | |
| Elements | Protocol includes preassessment tools, checklists, and metrics to assess gaps in care. |
| Certification of staff in correct BP measurement skills. | |
| Recommended Protocol | 2017 Hypertension Clinical Practice Guidelines.4 |
| Blood Pressure Assessment in Adults in Clinical Practice and Clinic-Based Research.133 | |
| Documentation | Documenting the implementing protocols may impose additional burdens on HCOs. Potential options to consider: |
| • Attestation, self-reported information | |
| • External auditor/rater | |
| • Competency testing | |
| Rationale | |
| Accurate measurement and recording of BP are essential to categorize level of BP, ascertain BP-related ASCVD risk, and guide management of high BP. Office BP measurement is often unstandardized, despite the well-known consequences of inaccurate measurement. Errors are common and can result in a misleading estimation of an individual’s true level of BP if staff are not trained and a protocol is not followed. The use of automated office BP measurements should be considered as part of the protocol for accurate measurement.134 | |
| Checklist for Accurate Measurement of BP135,136 | |
| Key Steps for Proper BP Measurements | |
| Specific Instructions: | |
| Step 1: Properly prepare the patient | |
| 1. Have the patient relax, sitting in a chair (feet on floor, back supported) for >5 min. | |
| 2. The patient should avoid caffeine, exercise, and smoking for at least 30 min before measurement. | |
| 3. Ensure patient has emptied his/her bladder. | |
| 4. Neither the patient nor the observer should talk during the rest period or during the measurement. | |
| 5. Remove all clothing covering the location of cuff placement. | |
| 6. Measurements made while the patient is sitting or lying on an examining table do not fulfill these criteria. | |
| Step 2: Use proper technique for BP measurements | |
| 1. Use a BP measurement device that has been validated, and ensure that the device is calibrated periodically. | |
| 2. Support the patient’s arm (eg, resting on a desk). | |
| 3. Position the middle of the cuff on the patient’s upper arm at the level of the right atrium (the midpoint of the sternum). | |
| 4. Use the correct cuff size, such that the bladder encircles 80% of the arm, and note if a larger- or smaller-than-normal cuff size is used. | |
| 5. Either the stethoscope diaphragm or bell may be used for auscultatory readings.137,138 | |
| Step 3: Take the proper measurements needed for diagnosis and treatment of elevated BP/hypertension | |
| 1. At the first visit, record BP in both arms. Use the arm that gives the higher reading for subsequent readings. | |
| 2. Separate repeated measurements by 1–2 min. | |
| 3. For auscultatory determinations, use a palpated estimate of radial pulse obliteration pressure to estimate SBP. Inflate the cuff 20–30 mm Hg above this level for an auscultatory determination of the BP level. | |
| 4. For auscultatory readings, deflate the cuff pressure 2 mm Hg per second, and listen for Korotkoff sounds. | |
| Step 4: Properly document accurate BP readings | |
| 1. Record SBP and DBP. If using the auscultatory technique, record SBP and DBP as onset of the first Korotkoff sound and disappearance of all Korotkoff sounds, respectively, using the nearest even number. | |
| 2. Note the time of most recent BP medication taken before measurements. | |
| Step 5: Average the readings | |
| 1. Use an average of ≥2 readings obtained on ≥2 occasions to estimate the individual’s level of BP | |
| Step 6: Provide BP readings to patient | |
| 1. Provide patients the SBP/DBP readings both verbally and in writing. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| Recommendation for Accurate Measurement of BP in the Office (Guideline Section 4) | |
| 1. For diagnosis and management of high BP, proper methods are recommended for accurate measurement and documentation of BP. (Class 1, Level of Evidence: C-EO) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CDU, care delivery unit; DBP, diastolic blood pressure; HCO, home care organization; QCDR, Qualified Clinical Data Registry; and SBP, systolic blood pressure.
SM-2: Use of a Standard Process for Assessing ASCVD Risk
| Measure Components | The CDU uses a standard process/protocol for properly measuring/assessing ASCVD risk, including: |
| 1. Measurement of ASCVD Risk | |
| a. Use of ACC/AHA Risk Estimator139,140 is recommended. Others may be used as alternatives when evaluated in the population seen clinically. | |
| b. Healthcare providers identify the health provider responsible for insuring competency and implementation of risk assessment in practice. | |
| 2. Incorporation Into Record | |
| a. Baseline risk should be part of patient demographics and included in each note when BP is 130–139/80–89 mm Hg, with indication of how it is used in defining treatment strategy. | |
| b. EMR for systems (eg, Epic, Cerner) should be requested to automatically place cardiovascular risk assessment in the patient record as part of vital signs. | |
| 3. Confirmation of Patient-Clinician Discussion | |
| a. The risk assessment used in the patient-clinician discussion should be entered 1) directly by EHR (eg, Epic, Cerner) or 2) by physician or other healthcare provider as part of documentation of the discussion. | |
| b. Patients should be knowledgeable about their results and, if interested, may be instructed on how to use the mobile ASCVD risk assessment app.139,140 | |
| Rationale | |
| Assessment of cardiovascular risk is the fundamental first step toward developing effective evidence-based therapy for treatment strategies for and shared decision discussions with patients. This includes using this assessment to correctly classify a patient’s current stage of HBP in accordance with recommendations from the 2017 Hypertension Clinical Practice Guidelines.4 In general, the ACC/AHA race- and sex-specific PCE (ASCVD Risk Estimator139,140) should be used for screening and management of hypertension. The 10-y risk is used for patients without ASCVD who have stage 1 hypertension (130/80–139/89 mm Hg) to determine those who should be treated with medical therapy (10-y risk >10%) and those who should who should be managed with nonpharmacological therapy (10-y risk <10%). Patients should know their current cardiovascular risk and how it relates to decisions about their therapy. | |
| Observational studies have demonstrated that ASCVD risk factors frequently occur in combination, with ≥3 risk factors present in 17% of patients.141 A meta-analysis from 18 cohort studies involving 257 384 patients identified a lifetime risk of ASCVD death, nonfatal MI, and fatal or nonfatal stroke that was substantially higher in adults with ≥2 ASCVD risk factors than in those with only 1 risk factor.141,142 | |
| To facilitate decisions about preventive interventions, it is recommended to screen for traditional ASCVD risk factors and apply the race- and sex-specific PCE (ASCVD Risk Estimator139,140) to estimate 10-y ASCVD risk for asymptomatic adults 40–75 y of age.59,139,140 For management of blood cholesterol, adults should be categorized as having low (<5%), borderline (5% to <7.5%), intermediate (≥7.5% to <20%), or high (≥20%) 10-y risk.143 The PCEs are best validated among non-Hispanic whites and non-Hispanic blacks living in the United States.19,144–147 In other racial/ethnic groups148,149 or in some non-US populations,148–151 the PCE may over- or under-estimate risk. Therefore, clinicians may consider use of another risk prediction tool, as an alternative to the PCE, if validated in a population with similar characteristics to the evaluated patient. Examples include the general Framingham ASCVD risk score,152 Reynolds risk scores,153,154 SCORE,155 and QRISK/JBS3156 tools. Other professional societies have incorporated some of these alternative validated risk scores into their lipid management guidelines or have considered different risk thresholds for preventive interventions.155–160 Although slight differences exist across organizational guidelines, they are all very similar in their overarching goal of matching the intensity of preventive therapies to absolute (generally 10-y) risk of the patient.155–160 | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| Recommendation for Screening and Management of CVD Risk (Guideline Section 2.4) | |
| 1. Screening for and management of other modifiable CVD risk factors are recommended in adults with hypertension.141,142 (Class 1, Level of Evidence: B-NR) | |
| 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease14 | |
| Recommendation for ASCVD Risk Assessment (Section 2.2, 2019 Prevention Guideline) | |
| 1. For adults 40 to 75 y of age, clinicians should routinely assess traditional cardiovascular risk factors and calculate 10-y risk of ASCVD by using the pooled cohort equations (PCE).139,140,146 (Class 1, Level of Evidence: B-NR) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CDU, care delivery unit; CVD, cardiovascular disease; DBP, diastolic blood pressure; EHR, electronic health record; HBP, high blood pressure; MI, myocardial infarction; PCE, pooled cohort equations; QCDR, Qualified Clinical Data Registry; and SBP, systolic blood pressure.
SM-3: Use of a Standard Process for Properly Screening All Adults ≥18 Years of Age for HBP (USPSTF)
| Measure Components | The CDU uses a standard process/protocol for properly screening all adults ≥18 years of age for HBP (based on an average of ≥2 BP measurements), including: |
| 1. Adults ages 18–39 y with office-measured SBP/DBP <120/80 mm Hg who do not have other hypertension risk factors can space out screenings to every 3–5 y (USPSTF).15 | |
| 2. Annual BP screening should be done for adults at increased risk for hypertension, defined as those ≥40 y of age and those <40 y of age who are overweight or obese or black, regardless of age. | |
| 3. For adults, the finding of an office BP consistent with hypertension and with SBP/DBP <160/100 mm Hg at an initial visit should be confirmed at a follow-up visit within 1 month, based on an average of ≥2 BP measurements at each visit. | |
| 4. 2017 Hypertension Clinical Practice Guidelines Recommendation4: In adults with an untreated SBP >130 mm Hg but <160 mm Hg or DBP >80 mm Hg but <100 mm Hg, it is reasonable to screen for the presence of white-coat hypertension by using either daytime ABPM or HBPM before diagnosis of hypertension.61–68 (Class 2a, Level of Evidence: B-NR) | |
| 5. 2017 Hypertension Clinical Practice Guidelines Recommendation4: In adults with untreated office BPs that are consistently between 120 mm Hg and 129 mm Hg for SBP or between 75 mm Hg and 79 mm Hg for DBP, screening for masked hypertension with HBPM (or ABPM) is reasonable.61,62,65,67,161 (Class 2a, Level of Evidence: B-NR) | |
| Rationale | |
| The evidence for the benefits of screening for HBP is well established. In 2007, the USPSTF reaffirmed its 2003 recommendation to screen for hypertension in adults ≥18 y of age (Grade A recommendation). Previous evidence reviews commissioned by the USPSTF found good-quality evidence that screening for hypertension has few major harms and provides substantial benefits.162,163 However, these reviews did not address the diagnostic accuracy of different BP measurement protocols or identify a reference standard for measurement confirmation. For the present recommendation, the USPSTF examined the diagnostic accuracy of office BP measurement, ABPM, and HBPM. The USPSTF also assessed the accuracy of these BP measurements and methods in confirming the diagnosis of hypertension. In addition, it reviewed data on optimal screening intervals for diagnosing hypertension in adults. | |
| The USPSTF found good evidence that screening for and treatment of HBP has few major harms. The USPSTF concluded with high certainty that the net benefit of screening for HBP in adults is substantial.15 No clinical trials randomly assigned patients to different rescreening intervals and evaluated clinical outcomes. Many observational studies have followed patients over time to determine how many develop hypertension at intervals of 1 to 5 y.15,164 | |
| Clinical Recommendations | |
| USPSTF Final Recommendation Statement on HBP in Adults15 | |
| 1. The USPSTF recommends screening for HBP in adults aged 18 y or older. The USPSTF recommends obtaining measurements outside of the clinical setting for diagnostic confirmation before starting treatment.164 (USPSTF, Grade A) | |
ABPM indicates ambulatory blood pressure monitoring; BP, blood pressure; CDU, care delivery unit; DBP, diastolic blood pressure; HBP, high blood pressure; HBPM, home blood pressure monitoring; SBP, systolic blood pressure; and USPSTF, US Preventive Services Task Force.
SM-4: Use of an EHR to Accurately Diagnose and Assess HBP Control
| Measure Components | The CDU uses an EHR system to obtain data that permit assessment of accurate diagnosis and assessment of HBP control and documentation of ASCVD risk, including: |
| The EHR/registry vendor shoul d be able to export SDP and DBP measurements associated with ambulatory clinic visits, including the date of service. | |
| The CDU should consider a standardized field in which the clinician can document the BP used in decision making and the date of service. | |
| The CDU should consider a standardized field to record home BP determinations and ASCVD risk assessment. | |
| The EHR/registry vendors should consider creating structured data elements using established, standardized nomenclature. | |
| Rationale | |
| A growing number of health systems are developing or using registries and EHRs that permit large-scale queries to support population health management strategies to identify undiagnosed or undertreated hypertension. Such innovations are implemented as ongoing quality improvement initiatives in clinical practice. To reduce undiagnosed hypertension and improve hypertension management, a multipronged approach may include 1) application of hypertension screening algorithms to EHR databases to identify at-risk patients, 2) contacting at-risk patients to schedule BP measurements, 3) monthly written feedback to clinicians about at-risk patients who have yet to complete a BP measurement, and 4) electronic prompts for BP measurements whenever at-risk patients visit the clinic.55,57 | |
| Since passage of the Hitech Act, the use of EHRs and registries in clinical practice has become nearly ubiquitous. The purpose of this SM is to provide guidance to the CDU to aid in the identification of patients with elevated BP or stage 1 or stage 2 HBP through the EHR and/or registry. | |
| Previous studies have demonstrated that many patients with elevated BP or stage 1 or stage 2 HBP are undiagnosed with conventional administrative data sets (ICD-10). Use of free-text data searches or structured data searches can facilitate the identification of appropriate patients. In particular, we recommend the use of NQF’s denominator exceptions for medical, patient, and system exceptions to improve the accuracy of the data. | |
| The evaluation of structured data will greatly facilitate the accuracy of this hypertension performance measure. The intention of this measure is to promote the accurate collection and analysis of BP and demographics through the EHR by using standards-based tools. Currently, most EHRs and registries do not have a specific mapping of sufficient elements to allow the accurate recording and attribution of BPs. | |
| The intention of this SM is to provide guidance to EHR and registry vendors to support fluid data flow between the EHR and the registry, using existing established structured data elements. | |
| Potential additional benefits and characteristics of using properly configured EHRs and registries include: | |
| 1. CDS-based algorithms that support evidence-based guideline recommendations for accurate measurement, risk assessment, diagnosis, classification, and appropriate treatment for patients with or at risk of HBP | |
| 2. Properly vetted reminders and alerts for both clinicians and patients to ensure follow-up appointments, patient engagement, and adherence to GDMT. | |
| 3. Compliance with current national interoperability standards to facilitate exchange of information, including the timely transmission of digital data from BP measurement and monitoring devices. | |
| 4. Easy extraction of data needed for advanced analytic approaches to accurate classification and treatment of populations with or at risk of HBP. | |
| 5. Accurate and automated extraction of necessary data elements for construction, benchmarking, auditing, and feedback to providers and external reporting (eg, to CMS, NCQA, commercial payers, quality improvement initiatives, and professional society accrediting bodies) of standardized performance and quality measures. | |
| 6. Facilitation of internal and external quality improvement initiatives, such as Target: BP (AHA and AMA) and The Million Hearts campaign (HHS, CDC). | |
| 7. Documentation of nonclinical data, such as social determinants of health, health literacy, and shared decision making. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| Recommendations for EHR and Patient Registries (Guideline Section 12.3) | |
| 1. Use of the EHR and patient registries is beneficial for identification of patients with undiagnosed or undertreated hypertension.55–57 (Class 1, Level of Evidence: B-NR) | |
| 2. Use of the EHR and patient registries is beneficial for guiding quality improvement efforts designed to improve hypertension control.55–57 (Class 1, Level of Evidence: B-NR) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CDC, Centers for Disease Control and Prevention; CDS, clinical decision support; CDU, care delivery unit; EHR, electronic health record; GDMT, guideline-directed medical therapy/treatment; HBP, high blood pressure; HHS, Health and Human Services; ICD-10, International Classification of Diseases, 10th edition; NCQA, National Committee for Quality Assurance; PCE, pooled cohort equations; and SM, structural measure.
A Patient-Centered Approach for Controlling HBP
SM-5: Use of a Standard Process to Engage Patients in Shared Decision-Making, Tailored to Their Personal Benefits, Goals, and Values for Evidence-Based Interventions to Improve Control of HBP
| Measure Components | The CDU uses a standard process/protocol for implementing SDM in clinical settings for patients with HBP, including: |
| One of the following: | |
| • Structured decision aids | |
| - A formal SDM tool is available, with evidence that it is being routinely used in clinical encounters. | |
| ■ The choice of a decision aid should be informed by a formal quality assessment, as recommended by IPDAS.165 The tool should be published, free of bias, and ideally endorsed by professional organizations. | |
| - A process exists whereby patients with hypertension are identified and exposed to the SDM tool. | |
| ■ A formal SDM encounter occurs between the patient and provider using an evidence-based decision tool before initiation or adjustment of GDMT. | |
| • Communication skills training for providers | |
| - A program exists to provide skills in SDM to practitioners, with periodic assessments of providers’ skills. | |
| • Built-in triggers in EHRs to remind clinicians to provide a decision aid to patients with hypertension. | |
| - The use of an SDM tool is documented within the EHR. | |
| - A process exists for identifying patients with hypertension who have not participated in SDM so that such a process can be offered. | |
| Rationale | |
| Decisions about primary prevention should be collaborative between a clinician and a patient. SDM occurs when practitioners engage patients in discussions about personalized ASCVD risk estimates and their implications on the perceived benefits of preventive strategies, including lifestyle habits, goals, and medical therapies. Collaborative decisions are more likely to address potential barriers to treatment options.166–169 | |
| SDM is defined as “an approach where clinician and patients share the best available evidence when faced with the task of making decisions, and where patients are supported to consider options, to achieve informed preferences.”79,170 It draws on the principles of patient-centered care to increase patient commitment to treatment plans, including long-term adherence to drug therapy and lifestyle modification.168,171,172 | |
| Adherence to GDMT of hypertension can be enhanced by SDM between clinicians and patients. Patients should be engaged in the selection of antihypertensive drug therapy and lifestyle modification strategies, with consideration of individual values, preferences, and associated conditions and comorbidities (2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease14). | |
| Measuring SDM in clinical settings | |
| One of the following, supplemented with a process for systematic analysis and feedback to practitioners: | |
| • Patient-reported measures of SDM | |
| - The 3-item CollaboRATE Scale173 | |
| - The 9-item Shared Decision-Making Questionnaire (SDM-Q-9 Patient Version)174 | |
| - The 4-item SURE Scale175 | |
| • Provider-reported measures of SDM | |
| - The 9-item Shared Decision-Making Questionnaire (SDM-Q-Doc)176 | |
| Clinical Recommendations | |
| 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease14 | |
| Recommendations for Shared Decision Making (Section 2.1, 2019 Prevention Guideline) | |
| 1. Shared decision making should guide discussions regarding the best strategies to reduce ASCVD risk.166–169 (Class 1, Level of Evidence: B-R) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CDU, care delivery unit; EHR, electronic health record; GDMT, guideline-directed medical therapy/treatment; HBP, high blood pressure; IPDAS, International Patient Decision Aid Standards; and SDM, shared decision making.
SM-6: Demonstration of Infrastructure and Personnel That Assess and Address Social Determinants of Health of Patients With HBP
| Measure Components | The CDU uses a standard process/protocol for addressing SDoH in clinical settings for patients with HBP, including: |
| • Utilization of a standardized tool, such as the Accountable Health Communities Screening Tool,177 to screen health-related social needs in clinical settings. | |
| • Integration of social and behavioral domains (Table A) into EHRs to monitor efforts to address SDoH. | |
| • Documentation of patient assessments of SDoH and referrals to social services in medical records. | |
| • Integration of clinical staff members (eg, social workers, case managers, registered dietitians) to link patients with appropriate community resources. | |
| • Training of volunteers within the CDU to access a database of resources to address SDoH and provide follow-up until a resolution of unmet social needs is achieved. | |
| • Identification of community health workers to conduct home social assessments to connect socially deprived patients with community resources. | |
| • Creation of partnerships with community organizations that provide healthy food and assist with enrollment in federal nutrition assistance programs. | |
| • Creation of partnerships with pharmacies to provide access to home delivery options for obtaining medication to manage HBP | |
| Rationale | |
| Socioeconomic inequalities are strong determinants of ASCVD risk internationally.178,179 Therefore, it is important to tailor advice to a patient’s socioeconomic and educational status, as well as cultural, work, and home environments.180 The CMS has developed a tool to assess 5 domains of non-health-related measures that impact health outcomes: housing instability, food insecurity, transportation difficulties, utility assistance needs, and interpersonal safety.177 ASCVD prevention could benefit from such screening. ASCVD risk begins early in life, with heightened susceptibility tied to low socioeconomic status.181 Examples of upstream SDoH that affect adherence and ASCVD health outcomes include comorbid mental illness, low health literacy, exposure to adversity (eg, home/community violence, trauma exposures, safety concerns), financial strain, inadequate housing conditions, food insecurity (eg, access to affordable and nutritious food), and inadequate social support.182 Systems of care should evaluate SDoH that affect care delivery for the primary prevention of ASCVD (eg, transportation barriers, the availability of health services). | |
| Important considerations related to socioeconomic disadvantage are not captured by existing ASCVD risk equations.183 Addressing unmet social needs improves management of BP and lipids,184 highlighting the importance of dietary counseling and encouraging physical activity.185 More time may be required to address ASCVD prevention when working with adults of low health literacy or disadvantaged educational backgrounds. Differential cardiovascular outcomes persist by important sociodemographic characteristics, including but not limited to age, gender, and race/ethnicity.186–189 Failure to address the impact of SDoH impedes efficacy of proven prevention recommendations. Standardized use of EHRs that include social and behavioral domains could improve care for patients with HBP. Table A outlines social and behavioral domains that may be integrated into EHRs to address SDoH.190 | |
| Clinical Recommendations | |
| 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease14 | |
| Recommendations for Addressing Social Determinants of Health (SDoH) (Section 2.1, 2019 Prevention Guideline) | |
| 1. Social determinants of health should inform optimal implementation of treatment recommendations for the prevention of ASCVD.178–181,185,189,191 (Class 1, Level of Evidence: B-NR) | |
Table A.
Core Domain and Measures
| Domain | Measure |
|---|---|
| Social | |
| Race/ethnicity | US Census (2 questions) |
| Education | Educational attainment (2 questions) |
| Financial resource strain | Overall financial resource strain (1 question) |
| Stress | Stress symptoms192 (1 question) |
| Depression | PHQ-2 (2 questions) |
| Social connections and social isolation | NHANES III (4 questions) |
| Exposure to violence: intimate partner violence | HARK (4 questions) |
| Neighborhood and community compositional characteristics | Residential address Census tract-median income |
| Behavioral | |
| Physical activity | Exercise Vital Sign (2 questions) |
| Tobacco use and exposure | NHIS (2 questions) |
| Alcohol use | AUDIT-C (3 questions) |
ACC indicates American College of Cardiology; AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; CDU, care delivery unit; EHR, electronic health record; HBP, high blood pressure; and SDoH, social determinants of health.
Republished with permission of the Institute of Medicine, from “Capturing social and behavioral domains and measures in electronic health records: phase 2.” Washington, DC: The National Academies Press, 2014; permission conveyed through Copyright Clearance Center, Inc.190
AUDIT-C indicates Alcohol Use Disorders Identification Test-C; HARK, Humiliation, Afraid, Rape, Kick; NHANES III, National Health and Nutrition Examination Survey III; NHIS, National Health Interview Survey; and PHQ-2, Patient Health Qu estionnaire-2.
Implementation of a System of Care for Patients With HBP
SM-7: Use of Team-Based Care to Better Manage HBP
| Measure Components | The CDU relies on various available components of team-based care in clinical settings for patients with HBP, which may include: |
| • Pharmacists | |
| • RNs/APRNs | |
| • Physician assistants | |
| • Medical assistants | |
| • Community health workers | |
| • Integrated care managers | |
| • Social workers | |
| • Behavioral interventionists | |
| • Trainees | |
| • Algorithms to support clinicians | |
| • EHR support (BP recording, actionable prompts for clinicians, population health management) | |
| • Remote HBPM (EHR integration) | |
| • Monitoring performance metrics | |
| • Population health management | |
| • Telephone-based follow-up | |
| • Regular team meetings (best practice updates, workflow evaluation) | |
| • Assigned roles and responsibilities (patient and clinicians, clarity about team member roles) | |
| • *Optional: SM-4: EHR to diagnose and assess, SM-8: use of telehealth, SM-10: performance measurement | |
| Goals of team-based care: | |
| • Improve clinical workflow | |
| • Patient education | |
| • Closer follow-up of BP after initiation | |
| • Medication titration | |
| • Laboratory follow-up | |
| • Improved adherence | |
| • Lower clinician burn-out193 | |
| Checklist | |
| Goal: To optimize outpatient hypertension management (to be specifically stated as team’s purpose/responsibility). | |
| Team Members: | |
| • Lead clinician (at least 1): APRN or physician | |
| • Clinical support (at least 1): pharmacist, nurse, physician assistant, medical assistant, community health worker, care manager, or EHR support modules specific to hypertension | |
| • Administrative support (at least 1): scheduler, receptionist | |
| • Expert referral (onsite or external): designated referral system for refractory patients: cardiologist, nephrologist, endocrinologist | |
| Team meetings: regular meetings on at least a quarterly basis to evaluate delivery of care for patients with hypertension. | |
| Performance monitoring: Use of PM 1–5 and QM 1–6 for feedback on performance and quality of care. | |
| Program elements (at least 2): | |
| 1. Patient educational materials or sessions on hypertension. | |
| 2. Availability of BP-specific follow-up in 1 mo (telephone based, with HBPM, telehealth, or clinical support or clinician follow-up). | |
| 3. Ability of patients to contact team-based care team in a timely fashion about hypertension concerns (telephone, secure EHR messaging, email, urgent appointments). | |
| 4. Algorithm for medication titration led by clinical support team member and lead clinician supervision. | |
| 5. Timely follow-up and monitoring of laboratory results, with titration of relevant drug classes. | |
| 6. Monitoring adherence by using pharmacy fill data. | |
| 7. Provider-specific performance reports with hypertension metrics. | |
| Rationale | |
| RCTs and meta-analyses of RCTs of team-based hypertension care involving nurse or pharmacist intervention demonstrated reductions in SBP and DBP and/or greater achievement of BP goals when compared with usual care.194–197 | |
| Similarly, systematic reviews of team-based care for patients with primary hypertension, including a review of studies that included community health workers, showed reductions in SBP and DBP and improvements in BP control, appointment keeping, and hypertension medication adherence as compared with usual care.198,199 | |
| Team-based care can be defined by numerous structures that are functional and improve care in various settings and patient populations. Inherently, they try to provide a division of labor and improved workflows so that the delivery of quality care is maximized/optimized. Disease-management-specific programs and protocols help identify areas to improve workflow and patient-centered care. | |
| AHRQ summary statement of team-based care: “the primary goal of medical teamwork is to optimize the timely and effective use of information, skills, and resources by teams of health care professionals for the purpose of enhancing the quality and safety of patient care.”200 | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| Recommendation for Structured, Team-Based Care Interventions for Hypertension Control (Guideline Sections 8.3.2 and 12.2) | |
| 1. A team-based care approach is recommended for adults with hypertension.194–197,199,201,202 (Class 1, Level of Evidence: A) | |
| 2. For older adults (≥65 y of age) with hypertension and a high burden of comorbidity and limited life expectancy, clinical judgment, patient preference, and a team-based approach to assess risk/benefit are reasonable for decisions regarding intensity of BP lowering and choice of antihypertensive drugs. (Class 2a, Level of Evidence: C-EO) | |
| 3. Follow-up and monitoring after initiation of drug therapy for hypertension control should include systematic strategies to help improve BP, including use of HBPM, team-based care, and telehealth strategies.47,203–207 (Class 1, Level of Evidence: A) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; AHRQ, Agency for Healthcare Research and Quality; APRN, advanced practice registered nurse; BP, blood pressure; CDU, care delivery unit; DBP, diastolic blood pressure; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; NAM, National Academy of Medicine; PM, performance measure; QM, quality measure; RCTs, randomized controlled trials; RN, registered nurse; SM, structural measure; and SBP, systolic blood pressure.
SM-8: Use of Telehealth, m-Health, e-Health, and Other Digital Technologies to Better Diagnose and Manage HBP
| Measure Components | The CDU uses various available components of telehealth, m-health, e-health, and other digital technologies proven by high-quality evidence to better diagnose and manage HBP in clinical settings for patients with HBP, which may include: |
| • Deployment of ≥1 telehealth, m-health, or e-health strategies (eg, Table B) | |
| • For patients engaged in self-monitoring, a platform is required to communicate home BP measurements to the healthcare provider team. This may require several methods including: | |
| - Telephonic communication of BP readings | |
| - Written communication of BP readings | |
| - Direct integration and delivery of BP readings via the EHR | |
| • Designating ≥1 individuals to implement changes in nonpharmacological or pharmacological treatment based on self-monitoring or behavioral/coaching strategies. This may include development of algorithms and involve several members of the care team, including but not limited to: | |
| - Medical practice coordinators | |
| - Pharmacists | |
| - Physician assistants | |
| - Nurse practitioners | |
| - Nutritionists | |
| - Nurses | |
| - Physicians | |
| • Developing a framework to iteratively and routinely assess ongoing efficacy of different telehealth strategies for the CDU | |
| • Maintaining flexibility to modify strategies as new telehealth technologies emerge (eg, novel BP measurement devices, data integration software) | |
| Rationale | |
| Meta-analyses of RCTs of different telehealth interventions have demonstrated greater SBP and DBP reductions208–210 and a larger proportion of patients achieving BP control210 than those achieved with usual care without telehealth. The effect of various telehealth interventions on BP lowering was significantly greater than that of BP self-monitoring without transmission of BP data, which suggests a possible added value of the teletransmission approach.209,211 Although m-health interventions in general showed promise in reducing SBP in patients with hypertension, results were inconsistent.212 It is unclear which combination of telehealth intervention features is most effective, and telehealth has not been demonstrated to be effective as a standalone strategy for improving hypertension control. | |
| Telehealth, m-health, and e-health technologies refer to means of transmission with wired or wireless devices to communicate with a healthcare provider.212 E- health, or digital health, is the use of emerging communication and information technologies to improve health and health care. M-health, a subsegment of e- health, is the use of mobile computing and communication technologies (eg, mobile phones, wearable sensors) for health services and information.212 Table B provides a list of examples of telehealth strategies and telehealth technologies. Importantly, these strategies include interventions beyond reminders for nonpharmacological or pharmacological intervention and increased awareness of BP measurement. They include active self-titration of medication and in-person coaching or e-coaching. M-health technologies are becoming more prevalent, and their use will continue to grow, consistent with recommendations from the Institute of Medicine.213 As new technologies emerge, including new devices for self-monitoring, it is unlikely that clinical trials will be repeated using each new technology. However, if self-monitoring is used, it is important to ensure that the BP measurement device used has been validated with an internationally accepted protocol and the results have been published in a peer-reviewed journal.214 Telehealth strategies that compare different frequencies of HBPM or ABPM have not been rigorously tested. | |
| Systems-level support, such as use of EHR (see SM-4), clinical decision support (ie, treatment algorithms), technology-based remote monitoring (see Table B), self-management support tools, and monitoring of performance, are likely to augment and intensify team-based care efforts to reduce HBP (see SM-7). | |
| Select telehealth strategies incorporate self-monitoring of BP Among individuals with hypertension, self-monitoring of BP, without other interventions, has shown limited evidence for treatment-related BP reduction and achievement of BP control.50,211,215 However, with the increased recognition of inconsistencies between office and out-of-office BPs and closer correlation of out-of-office BPs versus office BPs with cardiovascular outcomes,216 and with greater reductions in BP being recommended for hypertension control, increased attention is being paid to out-of-office BP readings. Thus, telehealth, m-health, and e-health strategies will likely increasingly incorporate self-monitoring, as well. | |
| As outlined in Table B, there are a wide variety of m-health, e-health, and telehealth strategies that may or may not be available to a specific CDU and therefore to the individual provider/patient. Because development of new mobile technologies is ongoing, we also wished to provide flexibility for each CDU to choose among these and any future strategies that are developed. | |
| Although ABPM is generally accepted as the best out-of-office measurement method, HBPM is often a more practical approach in clinical practice. Recommended procedures for the collection of HBPM data are provided in Table C. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| Recommendation for Telehealth Interventions to Improve Hypertension Control (Guideline Sections 8.3.2 and 12.3) | |
| 1. Telehealth strategies can be useful adjuncts to interventions shown to reduce BP for adults with hypertension.208–212 (Class 2a, Level of Evidence: A) | |
| 2. Follow-up and monitoring after initiation of drug therapy for hypertension control should include systematic strategies to help improve BP, including use of HBPM, team-based care, and telehealth strategies.47,203–207 (Class 1, Level of Evidence: A) | |
Table B.
Examples of Telehealth Strategies and Technologies to Promote Effective Hypertension Management
| Telehealth strategies |
| • Automated BP data capture and transmission of the patient’s self-measured BP |
| • Self-management support, including education, reminders, and feedback that is automated or delivered by a healthcare professional |
| • Medication titration and follow-up monitoring protocols/algorithm |
| • Prescription refill reminders |
| • Medication adherence assessments |
| • Self-monitoring of lifestyle behaviors |
| • Integration of behavior change techniques, including in-person counseling or e-counseling |
| • Case/care/population health management |
| Commonly used telehealth technologies |
| • Wired “landline” telephone |
| • Wireless smartphone applications |
| • Website accessed via computers and handheld devices |
| • Text messaging |
| • Email messaging |
| • Social networking and social media websites/applications |
| • Wireless BP measurement devices |
| • Electronic pill dispensers/counters |
ABPM indicates ambulatory blood pressure monitoring; ACC, American College of Cardiology; AHA, American Heart Association; BP, blood pressure; CDU, care delivery unit; DBP, diastolic blood pressure; e-health, healthcare services provided electronically via the Internet; EHR, electronic health record; HBP, high blood pressure; HBPM, home blood pressure monitoring; m-health, practice of medicine and public health supported by mobile devices; RCTs, randomized controlled trials; SM, structural measure; and SBP, systolic blood pressure.
Reproduced with permission from Whelton et al.4 Copyright © 2018, American Heart Association, Inc., and American College of Cardiology Foundation.
BP indicates blood pressure.
Table C:
Procedures for Use of HBPM
| Patient training should occur under medical supervision, including: |
| • Information about hypertension |
| • Selection of equipment |
| • Acknowledgment that individual BP readings may vary substantially |
| • Interpretation of results |
| Devices: |
| • Verify use of automated validated devices. Use of auscultatory devices (mercury, aneroid, or other) is not generally useful for HBPM because patients rarely master the technique required for measurement of BP with auscultatory devices. |
| • Monitors with provision for storage of readings in memory are preferred. |
| • Verify use of appropriate cuff size to fit the arm. |
| • Verify that left/right inter-arm differences are insignificant. If differences are significant, instruct patient to measure BPs in the arm with higher readings. |
| Instructions on HBPM procedures: |
| • Remain still: |
| • Avoid smoking, caffeinated beverages, or exercise within 30 min before BP measurements. |
| • Ensure ≥5 min of quiet rest before BP measurements. |
| • Sit correctly: |
| - Sit with back straight and supported (on a straight-backed dining chair, for example, rather than a sofa). |
| - Sit with feet flat on the floor and legs uncrossed. |
| - Keep arm supported on a flat surface (such as a table), with the upper arm at heart level. |
| - Bottom of the cuff should be placed directly above the antecubital fossa (bend of the elbow). |
| • Take multiple readings: |
| - Take at least 2 readings 1 min apart in morning before taking medications and in evening before supper. Optimally, measure and record BP daily. Ideally, obtain weekly BP readings beginning 2 wk after a change in the treatment regimen and during the week before a clinic visit. |
| • Record all readings accurately: |
| - Monitors with built-in memory should be brought to all clinic appointments. |
| - BP should be based on an average of readings on ≥2 occasions for clinical decision making. |
| The information above may be reinforced with the following: AHA webpage “Monitoring Your Pressure at Home”217 and AHA video “At home blood pressure monitoring”218 |
Reproduced with permission from Whelton et al.4 Copyright © 2018, American Heart Association, Inc., and American College of Cardiology Foundation.
BP indicates blood pressure; and HBPM, home blood pressure monitoring.
SM-9: Use of a Single, Standardized Plan of Care for All Patients With HBP
| Measure Components | The CDU has developed and implemented a single, standardized plan of care for HBP that addresses health behaviors, comorbid conditions, follow-up, and treatment goals through shared decision making, in accordance with Table D. |
| Rationale | |
| A specific plan of care for hypertension is essential and should reflect understanding of the modifiable and nonmodifiable determinants of health behaviors, including the social determinants of risk and outcomes. A clinician’s sequential flow chart for management of hypertension is presented (Table D). The determinants will vary among demographic subgroups. | |
| Studies demonstrate that implementation of a plan of care for hypertension can lead to sustained reduction of BP and attainment of BP targets over several years.219–224 Meta-analysis of RCTs shows reductions in BP of patients with hypertension and achievement of BP goals at 6 months and 1 year when compared with usual care.4 (See Table D.) | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| The Plan of Care for Hypertension (Guideline Section 13) | |
| 1. Every adult with hypertension should have a clear, detailed, and current evidence-based plan of care that ensures the achievement of treatment and self-management goals, encourages effective management of comorbid conditions, prompts timely follow-up with the healthcare team, and adheres to CVD GDMT. (Class 1, Level of Evidence: C-EO) | |
Table D.
Clinician’s Steps for the Management of Hypertension
| Clinician’s Sequential Flowchart for the Management of Hypertension |
| Measure office BP accurately |
| Detect white-coat hypertension or masked hypertension by using ABPM and HBPM |
| Evaluate for secondary hypertension |
| Identify target-organ damage |
| Introduce lifestyle interventions |
| Identify and discuss treatment goals |
| Use ASCVD risk estimation to guide BP threshold for pharmacological therapy |
| Align treatment options with comorbidities |
| Account for age, race, ethnicity, sex, and special circumstances in antihypertensive treatment |
| Initiate antihypertensive pharmacological therapy |
| Insure appropriate follow-up |
| Use team-based care |
| Connect patient to clinician via telehealth |
| Detect and reverse nonadherence |
| Use health information technology for remote monitoring and self-monitoring of BP |
ACC indicates American College of Cardiology; AHA, American Heart Association; BP, blood pressure; CDU, care delivery unit; CVD, cardiovascular disease; GDMT, guideline-directed medical therapy/treatment; HBP, high blood pressure; and RCTs, randomized controlled trials.
Reproduced with permission from Whelton et al.4 Copyright © 2018, American Heart Association, Inc., and American College of Cardiology Foundation.
ABPM indicates ambulatory blood pressure monitoring; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; and HBPM, home blood pressure monitoring.
Use of Performance Measures to Improve Care for HBP
SM-10: Use of Performance and Quality Measures to Improve Quality of Care for Patients With HBP
| Measure Components | The CDU uses performance and quality measures for evaluation and improvement in clinical settings for the diagnosis and management of patients with HBP, which include: |
| • Performance measures that are developed according to established ACC/AHA standards. | |
| • Performance measures that identify key structural components, care processes, and/or outcomes that are highly correlatec with important, high-priority patient care goals. | |
| • Methods to accurately and feasibly collect data in order to assess performance measures. | |
| • Process to identify appropriate patient groups, healthcare providers, and/or observation periods to be included in the measurement process. | |
| • Process to include outcomes of performance measurement in quality improvement strategies. | |
| Rationale | |
| Performance measures are systematic and standardized methods that are aimed at identifying and improving suboptimal medical care and patient outcomes Performance measures represent one of several potential strategies that can be used, together or alone, to help reduce gaps in the quality of health care. Effective performance measures are those that are associated with meaningful, desirable patient outcomes and include broad sampling from appropriate and related medical domains.2 Performance measure design should follow established standards, as outlined by national organizations,2 and have precise, validated components that are feasible, actionable, and meaningful. Performance measures usually reflect clinical practice guidelines of the highest levels of recommendation and evidence. Given that the identification, treatment, and control of HBP are suboptimal,3,225,226 use of effective performance measures ca help improve these gaps in care, as has been shown in 1 observational study from Kaiser Permanente of Northern California.56 No RCTs of HBP performance measures have been published.4 | |
| Implementation of Performance Measures | |
| 1. Identify performances measures for hypertension that: | |
| a. Meet established ACC/AHA standards. | |
| b. Include key components that influence the impact and sustainability of hypertension detection, treatment, and control for the target population (medical care, cost of care, patient-reported factors). | |
| c. Help address the most pressing gaps in hypertension-related care for the healthcare provider, practice, or system. | |
| 2. Coordinate the most feasible and meaningful collection of performance measures data with available data sources (eg, electronic health records, national data registries, administrative databases). | |
| Uses of Performance Measures | |
| 1. To assess performance of the healthcare provider, practice, or system, identifying and characterizing gaps in quality of hypertension care (based on comparison to a national “benchmark” standard or based on comparison to previous performance by the same healthcare provider, practice, or system). | |
| 2. To be used to design and implement quality improvement plans to help address gaps in quality of hypertension care identified by performance measures. | |
| 3. To report the use and outcomes of performance measurement as part of healthcare quality payment programs that are used by organizations to determine reimbursement to healthcare providers, practices, and systems on the basis of achievement and reporting of various performance metrics. | |
| Clinical Recommendations | |
| 2017 Hypertension Clinical Practice Guidelines4 | |
| Recommendation for Performance Measures (Guideline Section 12.4.1) | |
| 1. Use of performance measures in combination with other quality improvement strategies at patient-, provider-, and system-based levels is reasonable to facilitate optimal hypertension control.56,227,228 (Class 2a, Level of Evidence: B-NR) | |
ACC indicates American College of Cardiology; AHA, American Heart Association; CDU, care delivery unit; HBP, high blood pressure; and RCT, randomized controlled trial.
Appendix B. Author Listing of Relationships With Industry and Other Entities (Relevant)—2019 AHA/ACC Clinical Performance and Quality Measures for Adults With High Blood Pressure
| Committee Member | Employment | Consultant | Speakers Bureau | Ownership/Partnership/Principal | Personal Research | Institutional, Organizational, or Other Financial Benefit | Expert Witness |
|---|---|---|---|---|---|---|---|
| Donald E. Casey Jr, Chair | Thomas Jefferson College of Population Health—Adjunct Faculty; Rush Medical College—Faculty; University of Minnesota, Institute of Health Informatics—Affiliate Faculty; President, American College of Medical Quality; IPO 4 Health—Principal and Founder | None | None | None | None | None | None |
| Randal J. Thomas, Vice Chair | Mayo Clinic—Medical Director, Cardiac Rehabilitation Program | None | None | None | None | None | None |
| Vivek Bhalla | Stanford University Medical Center—Assistant Professor of Medicine, Nephrology; Stanford Hypertension Center—Director |
|
None | None | None |
|
None |
| Yvonne Commodore-Mensah | Johns Hopkins School of Nursing—Assistant Professor | None | None | None | None | None | None |
| Paul A. Heidenreich | Stanford VA Palo Alto Health Care System—Professor of Medicine | None | None | None | None | None | None |
| Dhaval Kolte | Massachusetts General Hospital and Harvard Medical School—International Cardiology Fellow | None | None | None | None | None | None |
| Paul Muntner | University of Alabama at Birmingham—Professor, Department of Epidemiology | None | None | None | None | None | None |
| Sidney C. Smith Jr | University of North Carolina at Chapel Hill—Professor of Medicine; Division of Cardiology, Department of Medicine | None | None | None | None | None | None |
| John A. Spertus | Washington University School of Medicine in St. Louis—Adjunct Professor of Medicine, Cardiovascular Division; Saint Luke’s Mid America Heart Institute—Director, Health Outcomes Research; University of Missouri-Kansas City—Professor, Daniel J. Lauer Missouri Endowed Chair in Metabolism and Vascular Disease Research | None | None | None |
|
None | |
| John R. Windle | University of Nebraska College of Medicine—Professor, Internal Medicine, Division of Cardiovascular Medicine | None | None | None | None | None | None |
| Gregory D. Wozniak | American Medical Association—Director, Outcomes Analytics; Northwestern University, Feinberg School of Medicine—Adjunct Assistant Professor | None | None | None | None | None | None |
| Boback Ziaeian | UCLA David Geffen School of Medicine—Assistant Professor; US Department of Veterans Affairs—Assistant Professor | None | None | None | None | None | None |
This table represents the relationships of committee members with industry and other entities that were determined to be relevant to this document. These relationships were reviewed and updated in conjunction with all meetings and/or conference calls of the writing committee during the document development process. The table does not necessarily reflect relationships with industry at the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$5 000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person’s gross income for the previous year. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted.
According to the ACC/AHA, a person has a relevant relationship IF: a) the relationship or interest relates to the same or similar subject matter, intellectual property or asset, topic, or issue addressed in the document; or b) the company/entity (with whom the relationship exists) makes a drug, drug class, or device addressed in the document or makes a competing drug or device addressed in the document; or c) the person or a member of the person’s household, has a reasonable potential for financial, professional or other personal gain or loss as a result of the issues/content addressed in the document.
Significant relationship.
No financial benefit.
ACC indicates American College of Cardiology; AHA, American Heart Association; UCLA, University of California, Los Angeles; and VA, Veterans Affairs.
Appendix C. Reviewer Listing of Relationships With Industry and Other Entities (Comprehensive)—2019 AHA/ACC Clinical Performance and Quality Measures for Adults With High Blood Pressure
| Reviewer | Representation | Employment | Consultant | Speakers Bureau | Ownership/Partnership/Principal | Personal Research | Institutional, Organizational, or Other Financial Benefit | Expert Witness | Salary |
|---|---|---|---|---|---|---|---|---|---|
| Biykem Bozkurt | Official TFPM Lead; TFDS Content Reviewer | Baylor College of Medicine—Mary and Gordon Cain Chair Professor of Medicine and Director, Winters Center for Heart Failure Research; Michael E. DeBakey VA Medical Center, Cardiology—Chief, Cardiology Section |
|
None | None |
|
|
None | None |
| Nicole L. Lohr | Official ACC | Medical College of Wisconsin—Assistant Professor | None | None | None | None |
|
None | None |
| Andrea L. Price | Official ACC | Indiana University Health—Director, Quality Databases | None | None | None | None |
|
None | None |
| Brent Egan | Official AHA | Medical University of South Carolina, Charleston (MUSC)—Professor of Medicine and Pharmacology |
|
|
None | None |
|
None | None |
| John M. Flack | Official AHA | Southern Illinois University School of Medicine, Internal Medicine—Professor, Chair, and Chief of Hypertension Specialty Services | None | None | None |
|
None | None | |
| Sandra J. Taler | Official AHA | Mayo Clinic—Professor of Medicine | None | None | None | None | None | None | None |
| Michael Rakotz | Official AMA | American Medical Association—Vice President, Health Outcomes | None | None | None | None |
|
None | None |
| Cheryl Dennison-Himmelfarb | Official PCNA | Johns Hopkins School of Nursing—Associate Dean for Research, Sarah E. Allison Endowed Professor, and Deputy Director, Institute for Clinical Translational Research | None | None | None |
|
None |
|
|
| Nathalie De Michelis | Content ACC | University of California, Irvine—Cardiovascular Program Manager | None | None | None | None | None | None | None |
| Eugene Yang | Content ACC | University of Washington School of Medicine—Medical Director and Clinical Associate Professor of Medicine, Division of Cardiology, Carl and Renee Behnke Endowed Professorship for Asian Health | None | None | None |
|
|
None | |
| Marjorie L. King | Content ACC/AHA | Helen Hayes Hospital—Chief Medical Officer, Internal Medicine (Cardiology) and Director, Cardiopulmonary, Rehabilitation |
|
None | None | None | None | None | None |
| Raj Padwal | Content AMA | University of Alberta—Professor of Medicine and Director, Hypertension Dyslipidemia Clinic | None | None |
|
None | None | None | None |
| Nancy Houston-Miller | Content PCNA | The Lifecare Company—Associate Director |
|
None | None | None | None | None | None |
This table represents all relationships of reviewers with industry and other entities that were reported at the time of peer review, including those not deemed to be relevant to this document, at the time this document was under review. The table does not necessarily reflect relationships with industry at the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$5 000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person’s gross income for the previous year. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted. Names are listed in alphabetical order within each category of review. Please refer to http://www.acc.org/guidelines/about-guidelines-and-clinical-documents/relationships-with-industry-policy for definitions of disclosure categories or additional information about the ACC/AHA Disclosure Policy for Writing Committees.
Significant relationship.
No financial benefit.
This disclosure was entered under the Clinical Trial Enroller category in the ACC’s disclosure system. To appear in this category, the reviewer acknowledges that there is no direct or institutional relationship with the trial sponsor as defined in the ACCF or ACC/AHA Disclosure Policy for Writing Committees.
ACC indicates American College of Cardiology; AHA, American Heart Association; AMA, American Medical Association; DSMB, Data Safety and Monitoring Board; HBP, high blood pressure; NIH, National Institutes of Health; PCNA, Preventive Cardiovascular Nurses Association; TFDS, Task Force for Data Standards; and TFPM, Task Force on Performance Measures.
Footnotes
This Physician Performance Measurement Set (PPMS) and related data specifications were developed by the Physician Consortium for Performance Improvement (the Consortium), including the American College of Cardiology (ACC), the American Heart Association (AHA), and the American Medical Association (AMA), to facilitate quality-improvement activities by physicians. The performance measures contained in this PPMS are not clinical guidelines, do not establish a standard of medical care, and have not been tested for all potential applications. Although copyrighted, they can be reproduced and distributed, without modification, for noncommercial purposes for example, use by health care providers in connection with their practices. Commercial use is defined as the sale, license, or distribution of the performance measures for commercial gain, or incorporation of the performance measures into a product or service that is sold, licensed, or distributed for commercial gain. Commercial uses of the PPMS require a license agreement between the user and the AMA (on behalf of the Consortium) or the ACC or the AHA. Neither the AMA, ACC, AHA, the Consortium, nor its members shall be responsible for any use of this PPMS.
The measures and specifications are provided “as is” without warranty of any kind.
Limited proprietary coding is contained in the measure specifications for convenience. Users of the proprietary code sets should obtain all necessary licenses from the owners of the code sets. The AMA, the ACC, the AHA, the National Committee for Quality Assurance (NCQA), and the Physician Consortium for Performance Improvement (PCPI) and its members disclaim all liability for use or accuracy of any Current Procedural Terminology (CPT) or other coding contained in the specifications.
CPT contained in the measures specifications is copyright 2004–2012 American Medical Association. LOINC copyright 2004–2012 Regenstrief Institute, Inc. This material contains SNOMED CLINICAL TERMS (SNOMED CT) copyright 2004–2012 International Health Terminology Standards Development Organization. All rights reserved.
This document underwent a 14-day peer review between March 18, 2019, and April 1, 2019, and a 30-day public comment period between March 18, 2019, and April 16, 2019.
The American Heart Association and the American College of Cardiology make every effort to avoid any actual or potential conflicts of interest that may arise as a result of an outside relationship or a personal, professional, or business interest of a member of the writing panel. Specifically, all members of the writing group are required to complete and submit a Disclosure Questionnaire showing all such relationships that might be perceived as real or potential conflicts of interest.
This document was approved by the American College of Cardiology Clinical Policy Approval Committee and the American Heart Association Science Advisory and Coordinating Committee in June 2019; by the American Heart Association Executive Committee on August 9, 2019; and by the American Medical Association and the Preventive Cardiovascular Nurses Association on July 25, 2019.
Supplemental materials are available with this article at https://www.ahajournals.org/doi/suppl/10.1161/HCQ.0000000000000057.
Copies: This document is available on the websites of the American College of Cardiology (www.acc.org) and the American Heart Association (professional.heart.org). A copy of the document is also available at https://professional.heart.org/statements by selecting the “Guidelines & Statements” button. To purchase additional reprints, call 843-216-2533 or kelle.ramsay@wolterskluwer.com.
Developed in Collaboration With the American Medical Association and the Preventive Cardiovascular Nurses Association
Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, American Association of Clinical Endocrinologists, American Nurses Association, American Society for Preventive Cardiology, American Society of Health-System Pharmacists, and Association of Black Cardiologists
ACC/AHA Task Force Members, see page 13
Contributor Information
Donald E. Casey, Jr, Thomas Jefferson College of Population Health—Adjunct Faculty; Rush Medical College—Faculty; University of Minnesota, Institute of Health Informatics—Affiliate Faculty; President, American College of Medical Quality; IPO 4 Health—Principal and Founder.
Randal J. Thomas, Mayo Clinic—Medical Director, Cardiac Rehabilitation Program.
Vivek Bhalla, Stanford University Medical Center—Assistant Professor of Medicine, Nephrology; Stanford Hypertension Center—Director.
Yvonne Commodore-Mensah, Johns Hopkins School of Nursing—Assistant Professor.
Paul A. Heidenreich, Stanford VA Palo Alto Health Care System—Professor of Medicine.
Dhaval Kolte, Massachusetts General Hospital and Harvard Medical School—International Cardiology Fellow.
Paul Muntner, University of Alabama at Birmingham—Professor, Department of Epidemiology.
Sidney C. Smith, Jr, University of North Carolina at Chapel Hill—Professor of Medicine; Division of Cardiology, Department of Medicine.
John A. Spertus, Washington University School of Medicine in St. Louis—Adjunct Professor of Medicine, Cardiovascular Division; Saint Luke’s Mid America Heart Institute—Director, Health Outcomes Research; University of Missouri-Kansas City—Professor, Daniel J. Lauer Missouri Endowed Chair in Metabolism and Vascular Disease Research.
John R. Windle, University of Nebraska College of Medicine—Professor, Internal Medicine, Division of Cardiovascular Medicine.
Gregory D. Wozniak, American Medical Association—Director, Outcomes Analytics; Northwestern University, Feinberg School of Medicine—Adjunct Assistant Professor.
Boback Ziaeian, UCLA David Geffen School of Medicine—Assistant Professor; US Department of Veterans Affairs—Assistant Professor.
REFERENCES
- 1.Spertus JA, Eagle KA, Krumholz HM, et al. American College of Cardiology and American Heart Association methodology for the selection and creation of performance measures for quantifying the quality of cardiovascular care. Circulation. 2005;111:1703–12. [DOI] [PubMed] [Google Scholar]
- 2.Spertus JA, Bonow RO, Chan P, et al. ACCF/AHA new insights into the methodology of performance measurement: a report of the American College of Cardiology Foundation/American Heart Association Task Force on performance measures. Circulation. 2010;122:2091–106. [DOI] [PubMed] [Google Scholar]
- 3.Drozda J, Messer JV, Spertus J, et al. ACCF/AHA/AMA-PCPI 2011 performance measures for adults with coronary artery disease and hypertension: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures and the American Medical Association-Physician Consortium for Performance Improvement. Circulation. 2011;124:248–70. [DOI] [PubMed] [Google Scholar]
- 4.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13–115. [DOI] [PubMed] [Google Scholar]
- 5.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–52. [DOI] [PubMed] [Google Scholar]
- 6.National Committee for Quality Assurance (NCQA). Controlling high blood pressure (CPB). Available at: https://www.ncqa.org/hedis/measures/controlling-high-blood-pressure/. Accessed July 15, 2019.
- 7.Centers for Medicare & Medicaid Services. HTN-2 (NQF 0018): controlling high blood pressure. Available at: https://qpp.cms.gov/docs/QPP_quality_measure_specifications/Web-Interface-Measures/2019_Measure_HTN2_CMSWebInterface.pdf. Accessed July 15, 2019.
- 8.Crawford C AAFP decides to not endorse AHA/ACC hypertension guideline. Available at: https://www.aafp.org/news/health-of-the-public/20171212notendorseaha-accgdlne.html. Accessed July 15, 2019.
- 9.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018;36:1953–2041. [DOI] [PubMed] [Google Scholar]
- 10.National Committee for Quality Assurance. NCQA updates quality measures for HEDIS® 2019. Available at: https://www.ncqa.org/news/ncqa-updates-quality-measures-for-hedis-2019/. Accessed July 15, 2019.
- 11.Centers for Medicare & Medicaid Services. CMS expands coverage of ambulatory blood pressure monitoring (ABPM). Available at: https://www.cms.gov/newsroom/press-releases/cms-expands-coverage-ambulatory-blood-pressure-monitoring-abpm. Accessed July 22, 2019.
- 12.Centers for Medicare & Medicaid Services. Decision memo for ambulatory blood pressure monitoring (ABPM) (CAG-00067R2). Available at: https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=294. Accessed July 22, 2019.
- 13.Byrd JB, Brook RD. Hypertension. Ann Intern Med. 2019;170:ITC65–80. [DOI] [PubMed] [Google Scholar]
- 14.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–e646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.US Preventive Services Task Force. Final recommendation statement: high blood pressure in adults: screening. Available at: https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/high-blood-pressure-in-adults-screening. Accessed July 15, 2019.
- 16.Muntner P, Carey RM, Gidding S, et al. Potential US population impact of the 2017 ACC/AHA high blood pressure guideline. Circulation. 2018;137:109–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959–68. [DOI] [PubMed] [Google Scholar]
- 18.Colantonio LD, Booth JN, Bress AP, et al. 2017 ACC/AHA blood pressure treatment guideline recommendations and cardiovascular risk. J Am Coll Cardiol. 2018;72:1187–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kirkland EB, Heincelman M, Bishu KG, et al. Trends in healthcare expenditures among US adults with hypertension: national estimates, 2003–2014. J Am Heart Assoc. 2018;7:e008731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bress AP, Colantonio LD, Cooper RS, et al. Potential cardiovascular disease events prevented with adoption of the 2017 American College of Cardiology/American Heart Association blood pressure guideline. Circulation. 2019;139:24–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bundy JD, Mills KT, Chen J, et al. Estimating the association of the 2017 and 2014 hypertension guidelines with cardiovascular events and deaths in US adults: an analysis of national data. JAMA Cardiol. 2018;3:572–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Quality Forum. Controlling high blood pressure: NQF measure 0018. Available at: http://www.qualityforum.org/QPS/MeasureDetails.aspx?standardID=1236&print=0&entityTypeID=1. Accessed July 15, 2019.
- 23.National Quality Forum. Guidance for measure harmonization. Available at: https://www.qualityforum.org/Publications/2011/05/Guidance_for_Measure_Harmonization.aspx. Accessed July 15, 2019.
- 24.Normand SL, McNeil BJ, Peterson LE, et al. Eliciting expert opinion using the Delphi technique: identifying performance indicators for cardiovascular disease. Int J Qual Health Care. 1998;10:247–60. [DOI] [PubMed] [Google Scholar]
- 25.Thomas RJ, Balady G, Banka G, et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes. 2018;11:e000037. [DOI] [PubMed] [Google Scholar]
- 26.Egan BM, Sutherland SE, Rakotz M, et al. Improving hypertension control in primary care with the Measure Accurately, Act Rapidly, and Partner With Patients protocol. Hypertension. 2018;72:1320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4:393–404. [DOI] [PubMed] [Google Scholar]
- 28.Dahlöf B, Devereux RB, Kjeldsen SE, et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet. 2002;359:995–1003. [DOI] [PubMed] [Google Scholar]
- 29.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- 30.Guo X, Zhang X, Guo L, et al. Association between pre-hypertension and cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Curr Hypertens Rep. 2013;15:703–16. [DOI] [PubMed] [Google Scholar]
- 31.Guo X, Zhang X, Zheng L, et al. Prehypertension is not associated with all-cause mortality: a systematic review and meta-analysis of prospective studies. PLoS ONE. 2013;8:e61796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huang Y, Cai X, Li Y, et al. Prehypertension and the risk of stroke: a meta-analysis. Neurology. 2014;82:1153–61. [DOI] [PubMed] [Google Scholar]
- 33.Huang Y, Cai X, Liu C, et al. Prehypertension and the risk of coronary heart disease in Asian and Western populations: a meta-analysis. J Am Heart Assoc. 2015;4:e001519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang Y, Cai X, Zhang J, et al. Prehypertension and incidence of ESRD: a systematic review and meta-analysis. Am J Kidney Dis. 2014;63:76–83. [DOI] [PubMed] [Google Scholar]
- 35.Huang Y, Su L, Cai X, et al. Association of all-cause and cardiovascular mortality with prehypertension: a meta-analysis. Am Heart J. 2014;167:160–168.e1. [DOI] [PubMed] [Google Scholar]
- 36.Huang Y, Wang S, Cai X, et al. Prehypertension and incidence of cardiovascular disease: a meta-analysis. BMC Med. 2013;11:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ. 2009;338:b1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee M, Saver JL, Chang B, et al. Presence of baseline prehypertension and risk of incident stroke: a meta-analysis. Neurology. 2011;77:1330–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13. [DOI] [PubMed] [Google Scholar]
- 40.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet. 2014;383:1899–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shen L, Ma H, Xiang M-X, et al. Meta-analysis of cohort studies of baseline prehypertension and risk of coronary heart disease. Am J Cardiol. 2013;112:266–71. [DOI] [PubMed] [Google Scholar]
- 42.Sundström J, Arima H, Jackson R, et al. Effects of blood pressure reduction in mild hypertension: a systematic review and meta-analysis. Ann Intern Med. 2015;162:184–91. [DOI] [PubMed] [Google Scholar]
- 43.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 2. Effects at different baseline and achieved blood pressure levels–overview and meta-analyses of randomized trials. J Hypertens. 2014;32:2296–304. [DOI] [PubMed] [Google Scholar]
- 44.Wald DS, Law M, Morris JK, et al. Combination therapy versus mono-therapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009;122:290–300. [DOI] [PubMed] [Google Scholar]
- 45.Wang S, Wu H, Zhang Q, et al. Impact of baseline prehypertension on cardiovascular events and all-cause mortality in the general population: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168:4857–60. [DOI] [PubMed] [Google Scholar]
- 46.Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387:435–43. [DOI] [PubMed] [Google Scholar]
- 47.Margolis KL, Asche SE, Bergdall AR, et al. Effect of home blood pressure telemonitoring and pharmacist management on blood pressure control: a cluster randomized clinical trial. JAMA. 2013;310:46–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McManus RJ, Mant J, Haque MS, et al. Effect of self-monitoring and medication self-titration on systolic blood pressure in hypertensive patients at high risk of cardiovascular disease: the TASMIN-SR randomized clinical trial. JAMA. 2014;312:799–808. [DOI] [PubMed] [Google Scholar]
- 49.Siu AL, on behalf of the U.S. Preventive Services Task Force. Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–86. [DOI] [PubMed] [Google Scholar]
- 50.Uhlig K, Balk EM, Patel K, et al. Self-Measured Blood Pressure Monitoring: Comparative Effectiveness. Prepared by the Tufts Evidence-based Practice Center under Contract No. HHSA 290-2007-10055-I AHRQ Publication No. 12-EHC002-EF Rockville, MD: Agency for Healthcare Research and Quality (US); 2012. [PubMed] [Google Scholar]
- 51.Bangalore S, Toklu B, Gianos E, et al. Optimal systolic blood pressure target after SPRINT: insights from a network meta-analysis of randomized trials. Am J Med. 2017;130:707–719.e8. [DOI] [PubMed] [Google Scholar]
- 52.Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol. 2017;2:775–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thomopoulos C, Parati G, Zanchetti A. Effects of blood pressure lowering on outcome incidence in hypertension: 7. Effects of more vs. less intensive blood pressure lowering and different achieved blood pressure levels - updated overview and meta-analyses of randomized trials. J Hypertens. 2016;34:613–22. [DOI] [PubMed] [Google Scholar]
- 54.Verdecchia P, Angeli F, Gentile G, et al. More versus less intensive blood pressure-lowering strategy: cumulative evidence and trial sequential analysis. Hypertension. 2016;68:642–53. [DOI] [PubMed] [Google Scholar]
- 55.Borden WB, Maddox TM, Tang F, et al. Impact of the 2014 expert panel recommendations for management of high blood pressure on contemporary cardiovascular practice: insights from the NCDR PINNACLE registry. J Am Coll Cardiol. 2014;64:2196–203. [DOI] [PubMed] [Google Scholar]
- 56.Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rakotz MK, Ewigman BG, Sarav M, et al. A technology-based quality innovation to identify undiagnosed hypertension among active primary care patients. Ann Fam Med. 2014;12:352–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Williamson JD, Supiano MA, Applegate WB, et al. Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥75 years: a randomized clinical trial. JAMA. 2016;315:2673–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ambrosius WT, Sink KM, Foy CG, et al. The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Trials. 2014;11:532–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cushman WC, Grimm RH, Cutler JA, et al. Rationale and design for the blood pressure intervention of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. Am J Cardiol. 2007;99:44i–55i. [DOI] [PubMed] [Google Scholar]
- 61.Asayama K, Thijs L, Li Y, et al. Setting thresholds to varying blood pressure monitoring intervals differentially affects risk estimates associated with white-coat and masked hypertension in the population. Hypertension. 2014;64:935–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25:2193–8. [DOI] [PubMed] [Google Scholar]
- 63.Mancia G, Bombelli M, Brambilla G, et al. Long-term prognostic value of white coat hypertension: an insight from diagnostic use of both ambulatory and home blood pressure measurements. Hypertension. 2013;62:168–74. [DOI] [PubMed] [Google Scholar]
- 64.National Clinical Guideline Centre (UK). Hypertension in adults: diagnosis and management. NICE Clinical Guidelines, No. 127 London, UK: Royal College of Physicians (UK); 2011. Available at: https://www.nice.org.uk/guidance/cg127. Accessed July 15, 2019. [Google Scholar]
- 65.Ohkubo T, Kikuya M, Metoki H, et al. Prognosis of “masked” hypertension and “white-coat” hypertension detected by 24-h ambulatory blood pressure monitoring 10-year follow-up from the Ohasama study. J Am Coll Cardiol. 2005;46:508–15. [DOI] [PubMed] [Google Scholar]
- 66.Pickering TG, James GD, Boddie C, et al. How common is white coat hypertension? JAMA. 1988;259:225–8. [PubMed] [Google Scholar]
- 67.Pierdomenico SD, Cuccurullo F. Prognostic value of white-coat and masked hypertension diagnosed by ambulatory monitoring in initially untreated subjects: an updated meta analysis. Am J Hypertens. 2011;24: 52–8. [DOI] [PubMed] [Google Scholar]
- 68.Piper MA, Evans CV, Burda BU, et al. Diagnostic and predictive accuracy of blood pressure screening methods with consideration of rescreening intervals: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2015;162:192–204. [DOI] [PubMed] [Google Scholar]
- 69.Qualified Electronic Health Record Law and Legal Definition. Available at: https://definitions.uslegal.com/q/qualified-electronic-health-record/. Accessed July 15, 2019.
- 70.NQRN. PCPI’s Registry Community. Available at: https://www.thepcpi.org/page/NQRNresources. Accessed July 15, 2019.
- 71.Svetkey LP, Simons-Morton D, Vollmer WM, et al. Effects of dietary patterns on blood pressure: subgroup analysis of the Dietary Approaches to Stop Hypertension (DASH) randomized clinical trial. Arch Intern Med. 1999;159:285–93. [DOI] [PubMed] [Google Scholar]
- 72.Howard G, Cushman M, Moy CS, et al. Association of clinical and social factors with excess hypertension risk in black compared with white US adults. JAMA. 2018;320:1338–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nordmann AJ, Suter-Zimmermann K, Bucher HC, et al. Meta-analysis comparing Mediterranean to low-fat diets for modification of cardiovascular risk factors. Am J Med. 2011;124:841–851.e2. [DOI] [PubMed] [Google Scholar]
- 74.Estruch R, Ros E, Salas-Salvadó J, et al. Retraction and republication: primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–90. N Engl J Med. 2018;378:2441–2. [DOI] [PubMed] [Google Scholar]
- 75.Bazzano LA, Hu T, Reynolds K, et al. Effects of low-carbohydrate and low-fat diets: a randomized trial. Ann Intern Med. 2014;161:309–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.He J, Wofford MR, Reynolds K, et al. Effect of dietary protein supplementation on blood pressure: a randomized, controlled trial. Circulation. 2011;124:589–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yokoyama Y, Nishimura K, Barnard ND, et al. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med. 2014;174:577–87. [DOI] [PubMed] [Google Scholar]
- 78.Sepucha KR, Scholl I. Measuring shared decision making: a review of constructs, measures, and opportunities for cardiovascular care. Circ Cardiovasc Qual Outcomes. 2014;7:620–6. [DOI] [PubMed] [Google Scholar]
- 79.Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. J Gen Intern Med. 2012;27:1361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Appel LJ, Champagne CM, Harsha DW, et al. Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA. 2003;289:2083–93. [DOI] [PubMed] [Google Scholar]
- 81.Appel LJ, Moore TJ, Obarzanek E, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 82.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med. 2001;344:3–10. [DOI] [PubMed] [Google Scholar]
- 83.Aburto NJ, Ziolkovska A, Hooper L, et al. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Graudal NA, Hubeck-Graudal T, Jürgens G. Effects of low-sodium diet vs. high-sodium diet on blood pressure, renin, aldosterone, catecholamines, cholesterol, and triglyceride (Cochrane Review). Am J Hypertens. 2012;25:1–15. [DOI] [PubMed] [Google Scholar]
- 85.He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ. 2013;346:f1325. [DOI] [PubMed] [Google Scholar]
- 86.Mozaffarian D, Fahimi S, Singh GM, et al. Global sodium consumption and death from cardiovascular causes. N Engl J Med. 2014;371:624–34. [DOI] [PubMed] [Google Scholar]
- 87.Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE). TONE Collaborative Research Group. JAMA. 1998;279:839–46. [DOI] [PubMed] [Google Scholar]
- 88.Aburto NJ, Hanson S, Gutierrez H, et al. Effect of increased potassium intake on cardiovascular risk factors and disease: systematic review and meta-analyses. BMJ. 2013;346:f1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Geleijnse JM, Kok FJ, Grobbee DE. Blood pressure response to changes in sodium and potassium intake: a metaregression analysis of randomised trials. J Hum Hypertens. 2003;17:471–80. [DOI] [PubMed] [Google Scholar]
- 90.Whelton PK, He J. Health effects of sodium and potassium in humans. Curr Opin Lipidol. 2014;25:75–9. [DOI] [PubMed] [Google Scholar]
- 91.Whelton PK, He J, Cutler JA, et al. Effects of oral potassium on blood pressure. Meta-analysis of randomized controlled clinical trials. JAMA. 1997;277:1624–32. [DOI] [PubMed] [Google Scholar]
- 92.World Health Organization. Potassium intake for adults and children: guideline. Geneva: World Health Organization; 2012. Available at: https://www.who.int/nutrition/publications/guidelines/potassium_in-take/en/. Accessed July 15, 2019. [Google Scholar]
- 93.Dickinson HO, Mason JM, Nicolson DJ, et al. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–33. [DOI] [PubMed] [Google Scholar]
- 94.Lang T, Nicaud V, Darné B, et al. Improving hypertension control among excessive alcohol drinkers: a randomised controlled trial in France. The WALPA Group. J Epidemiol Community Health. 1995;49:610–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Roerecke M, Kaczorowski J, Tobe SW, et al. The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e108–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stewart SH, Latham PK, Miller PM, et al. Blood pressure reduction during treatment for alcohol dependence: results from the Combining Medications and Behavioral Interventions for Alcoholism (COMBINE) study. Addiction. 2008;103:1622–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wallace P, Cutler S, Haines A. Randomised controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:663–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Xin X, He J, Frontini MG, et al. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–7. [DOI] [PubMed] [Google Scholar]
- 99.The effects of nonpharmacologic interventions on blood pressure of persons with high normal levels. Results of the Trials of Hypertension Prevention, Phase I. JAMA. 1992;267:1213–20. [DOI] [PubMed] [Google Scholar]
- 100.Effects of weight loss and sodium reduction intervention on blood pressure and hypertension incidence in overweight people with high-normal blood pressure. The Trials of Hypertension Prevention, phase II. The Trials of Hypertension Prevention Collaborative Research Group. Arch Intern Med. 1997;157:657–67. [PubMed] [Google Scholar]
- 101.Carlson DJ, Dieberg G, Hess NC, et al. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:327–34. [DOI] [PubMed] [Google Scholar]
- 102.Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.García-Hermoso A, Saavedra JM, Escalante Y. Effects of exercise on resting blood pressure in obese children: a meta-analysis of randomized controlled trials. Obes Rev. 2013;14:919–28. [DOI] [PubMed] [Google Scholar]
- 104.Rossi AM, Moullec G, Lavoie KL, et al. The evolution of a Canadian Hypertension Education Program recommendation: the impact of resistance training on resting blood pressure in adults as an example. Can J Cardiol. 2013;29:622–7. [DOI] [PubMed] [Google Scholar]
- 105.Whelton SP, Chin A, Xin X, et al. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. [DOI] [PubMed] [Google Scholar]
- 106.Neter JE, Stam BE, Kok FJ, et al. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84. [DOI] [PubMed] [Google Scholar]
- 107.Whelton PK, Kumanyika SK, Cook NR, et al. Efficacy of nonpharmacologic interventions in adults with high-normal blood pressure: results from phase 1 of the Trials of Hypertension Prevention. Trials of Hypertension Prevention Collaborative Research Group. Am J Clin Nutr. 1997;65:652S–660S. [DOI] [PubMed] [Google Scholar]
- 108.Artinian NT, Fletcher GF, Mozaffarian D, et al. Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: a scientific statement from the American Heart Association. Circulation. 2010;122:406–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Eckel RH, Jakicic JM, Ard JD, et al. 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(suppl 2):S76–99. [DOI] [PubMed] [Google Scholar]
- 110.Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202:1028–34. [PubMed] [Google Scholar]
- 111.Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. Hypertension Detection and Follow-up Program Cooperative Group. JAMA. 1979;242:2562–71. [PubMed] [Google Scholar]
- 112.Prevention of stroke by antihypertensive drug treatment in older persons with isolated systolic hypertension. Final results of the Systolic Hypertension in the Elderly Program (SHEP). SHEP Cooperative Research Group. JAMA. 1991;265:3255–64. [PubMed] [Google Scholar]
- 113.Elliott WJ. What factors contribute to the inadequate control of elevated blood pressure? J Clin Hypertens (Greenwich). 2008;10:20–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.van der Laan DM, Elders PJM, Boons CCLM, et al. Factors associated with antihypertensive medication non-adherence: a systematic review. J Hum Hypertens. 2017;31:687–94. [DOI] [PubMed] [Google Scholar]
- 115.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310. [DOI] [PubMed] [Google Scholar]
- 116.Iskedjian M, Einarson TR, MacKeigan LD, et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther. 2002;24:302–16. [DOI] [PubMed] [Google Scholar]
- 117.Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill-Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15:90–6. [DOI] [PubMed] [Google Scholar]
- 118.Pharmacy Quality Alliance. Available at: https://www.pqaalliance.org/. Accessed July 15, 2019.
- 119.National Center for Chronic Disease Prevention and Health Promotion. Calculating proportion of days covered (PDC) for antihypertensive and antidiabetic medications: an evaluation guide for grantees. Available at: https://www.cdc.gov/dhdsp/docs/med-adherence-evaluation-tool.pdf. Accessed July 15, 2019.
- 120.Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med. 2004;164: 722–32. [DOI] [PubMed] [Google Scholar]
- 121.Xu W, Goldberg SI, Shubina M, et al. Optimal systolic blood pressure target, time to intensification, and time to follow-up in treatment of hypertension: population based retrospective cohort study. BMJ. 2015;350:h158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Czernichow S, Zanchetti A, Turnbull F, et al. The effects of blood pressure reduction and of different blood pressure-lowering regimens on major cardiovascular events according to baseline blood pressure: meta-analysis of randomized trials. J Hypertens. 2011;29:4–16. [DOI] [PubMed] [Google Scholar]
- 123.Thompson AM, Hu T, Eshelbrenner CL, et al. Antihypertensive treatment and secondary prevention of cardiovascular disease events among persons without hypertension: a meta-analysis. JAMA. 2011;305:913–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.SPRINT Research Group Wright JT Jr, Williamson JD, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373:2103–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Blood Pressure Lowering Treatment Trialists’ Collaboration. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384:591–8. [DOI] [PubMed] [Google Scholar]
- 126.Kassaï B, Boissel J-P, Cucherat M, et al. Treatment of high blood pressure and gain in event-free life expectancy. Vasc Health Risk Manag. 2005;1:163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Montgomery AA, Fahey T, Ben-Shlomo Y, et al. The influence of absolute cardiovascular risk, patient utilities, and costs on the decision to treat hypertension: a Markov decision analysis. J Hypertens. 2003;21:1753–9. [DOI] [PubMed] [Google Scholar]
- 128.van Dieren S, Kengne AP, Chalmers J, et al. Effects of blood pressure lowering on cardiovascular outcomes in different cardiovascular risk groups among participants with type 2 diabetes. Diabetes Res Clin Pract. 2012;98:83–90. [DOI] [PubMed] [Google Scholar]
- 129.Bangalore S, Kamalakkannan G, Parkar S, et al. Fixed-dose combinations improve medication compliance: a meta-analysis. Am J Med. 2007;120:713–9. [DOI] [PubMed] [Google Scholar]
- 130.Yang W, Chang J, Kahler KH, et al. Evaluation of compliance and health care utilization in patients treated with single pill vs. free combination antihypertensives. Curr Med Res Opin. 2010;26:2065–76. [DOI] [PubMed] [Google Scholar]
- 131.Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension. 2010;55:399–407. [DOI] [PubMed] [Google Scholar]
- 132.Sherrill B, Halpern M, Khan S, et al. Single-pill vs free-equivalent combination therapies for hypertension: a meta-analysis of health care costs and adherence. J Clin Hypertens (Greenwich). 2011;13:898–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Muntner P, Einhorn PT, Cushman WC, et al. Blood pressure assessment in adults in clinical practice and clinic-based research: JACC Scientific Expert Panel. J Am Coll Cardiol. 2019;73:317–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Roerecke M, Kaczorowski J, Myers MG. Comparing automated office blood pressure readings with other methods of blood pressure measurement for identifying patients with possible hypertension: a systematic review and meta-analysis [published online ahead of print Feb 4, 2019]. JAMA Intern Med. DOI: 10.1001/jamainternmed.2018.6551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–219. [DOI] [PubMed] [Google Scholar]
- 136.Weir MR. In the clinic: hypertension. Ann Intern Med. 2014;161:ITC1–15; quiz ITC6. [DOI] [PubMed] [Google Scholar]
- 137.Kantola I, Vesalainen R, Kangassalo K, et al. Bell or diaphragm in the measurement of blood pressure? J Hypertens. 2005;23:499–503. [DOI] [PubMed] [Google Scholar]
- 138.Liu C, Griffiths C, Murray A, et al. Comparison of stethoscope bell and diaphragm, and of stethoscope tube length, for clinical blood pressure measurement. Blood Press Monit. 2016;21:178–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.American College of Cardiology. ASCVD Risk Predictor Plus. Available at: http://tools.acc.org/ASCVD-Risk-Estimator-Plus/#!/calculate/estimate/. Accessed July 15, 2019.
- 140.American Heart Association. ASCVD-Risk-Calculator. Available at: https://professional.heart.org/professional/GuidelinesStatements/ASCVDRiskCalculator/UCM_457698_ASCVD-Risk-Calculator.jsp. Accessed July 15, 2019.
- 141.Wilson PWF, Kannel WB, Silbershatz H, et al. Clustering of metabolic factors and coronary heart disease. Arch Intern Med. 1999;159:1104–9. [DOI] [PubMed] [Google Scholar]
- 142.Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Andersson C, Enserro D, Larson MG, et al. Implications of the US cholesterol guidelines on eligibility for statin therapy in the community: comparison of observed and predicted risks in the Framingham Heart Study Offspring Cohort. J Am Heart Assoc. 2015;4:e001888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Colantonio LD, Richman JS, Carson AP, et al. Performance of the atherosclerotic cardiovascular disease pooled cohort risk equations by social deprivation status. J Am Heart Assoc. 2017;6:e005676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129(suppl 2):S49–73. [DOI] [PubMed] [Google Scholar]
- 147.Mora S, Wenger NK, Cook NR, et al. Evaluation of the pooled cohort risk equations for cardiovascular risk prediction in a multiethnic cohort from the Women’s Health Initiative. JAMA Intern Med. 2018;178:1231–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Jung KJ, Jang Y, Oh DJ, et al. The ACC/AHA 2013 pooled cohort equations compared to a Korean Risk Prediction Model for atherosclerotic cardiovascular disease. Atherosclerosis. 2015;242:367–75. [DOI] [PubMed] [Google Scholar]
- 149.Yang X, Li J, Hu D, et al. Predicting the 10-year risks of atherosclerotic cardiovascular disease in Chinese population: the China-PAR Project (Prediction for ASCVD Risk in China). Circulation. 2016;134:1430–40. [DOI] [PubMed] [Google Scholar]
- 150.Kavousi M, Leening MJG, Nanchen D, et al. Comparison of application of the ACC/AHA guidelines, Adult Treatment Panel III guidelines, and European Society of Cardiology guidelines for cardiovascular disease prevention in a European cohort. JAMA. 2014;311:1416–23. [DOI] [PubMed] [Google Scholar]
- 151.Pylypchuk R, Wells S, Kerr A, et al. Cardiovascular disease risk prediction equations in 400 000 primary care patients in New Zealand: a derivation and validation study. Lancet. 2018;391:1897–907. [DOI] [PubMed] [Google Scholar]
- 152.D’Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: the Framingham Heart Study. Circulation. 2008;117:743–53. [DOI] [PubMed] [Google Scholar]
- 153.Ridker PM, Buring JE, Rifai N, et al. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: the Reynolds Risk Score. JAMA. 2007;297:611–9. [DOI] [PubMed] [Google Scholar]
- 154.Ridker PM, Paynter NP, Rifai N, et al. C-reactive protein and parental history improve global cardiovascular risk prediction: the Reynolds Risk Score for men. Circulation. 2008;118:2243–51, 4p following 2251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37:2999–3058. [DOI] [PubMed] [Google Scholar]
- 156.JBS3 Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart. 2014;100(suppl 2): ii1–67. [DOI] [PubMed] [Google Scholar]
- 157.Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol. 2016;32:1263–82. [DOI] [PubMed] [Google Scholar]
- 158.Bibbins-Domingo K, U.S. Preventive Services Task Force. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:836–45. [DOI] [PubMed] [Google Scholar]
- 159.Downs JR, O’Malley PG. Management of dyslipidemia for cardiovascular disease risk reduction: synopsis of the 2014 U.S. Department of Veterans Affairs and U.S. Department of Defense clinical practice guideline. Ann Intern Med. 2015;163:291–7. [DOI] [PubMed] [Google Scholar]
- 160.US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;316:1997–2007. [DOI] [PubMed] [Google Scholar]
- 161.Stergiou GS, Asayama K, Thijs L, et al. Prognosis of white-coat and masked hypertension. Hypertension. 2014;63:675–82. [DOI] [PubMed] [Google Scholar]
- 162.Sheridan S, Pignone M, Donahue K. Screening for high blood pressure: a review of the evidence for the U.S. Preventive Services Task Force. Am J Prev Med. 2003;25:151–8. [DOI] [PubMed] [Google Scholar]
- 163.Wolff T, Miller T. Evidence for the reaffirmation of the U.S. Preventive Services Task Force recommendation on screening for high blood pressure. Ann Intern Med. 2007;147:787–91. [DOI] [PubMed] [Google Scholar]
- 164.Piper MA, Evans CV, Burda BU, et al. Screening for high blood pressure in adults: a systematic evidence review for the US Preventive Services Task Force. Evidence Synthesis No. 121 Rockville, MD: Agency for Healthcare Research and Quality; 2014. [PubMed] [Google Scholar]
- 165.Elwyn G, O’Connor A, Stacey D, et al. Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. BMJ Open. 2006;333:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Buhse S, Mühlhauser I, Heller T, et al. Informed shared decision-making programme on the prevention of myocardial infarction in type 2 diabetes: a randomised controlled trial. BMJ Open. 2015;5:e009116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Cooper LA, Roter DL, Carson KA, et al. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med. 2011;26:1297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Olomu A, Hart-Davidson W, Luo Z, et al. Implementing shared decision making in federally qualified health centers, a quasi-experimental design study: the Office-Guidelines Applied to Practice (Office-GAP) program. BMC Health Serv Res. 2016;16:334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8: 410–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Elwyn G, Laitner S, Coulter A, et al. Implementing shared decision making in the NHS. BMJ. 2010;341:c5146. [DOI] [PubMed] [Google Scholar]
- 171.Edwards A, Elwyn G, Hood K, et al. The development of COMRADE–a patient-based outcome measure to evaluate the effectiveness of risk communication and treatment decision making in consultations. Patient Educ Couns. 2003;50:311–22. [DOI] [PubMed] [Google Scholar]
- 172.Montori VM, Breslin M, Maleska M, et al. Creating a conversation: insights from the development of a decision aid. PLoS Med. 2007;4:e233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Barr PJ, Thompson R, Walsh T, et al. The psychometric properties of CollaboRATE: a fast and frugal patient-reported measure of the shared decision-making process. J Med Internet Res. 2014;16:e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kriston L, Scholl I, Hölzel L, et al. The 9-item Shared Decision Making Questionnaire (SDM-Q-9). Development and psychometric properties in a primary care sample. Patient Educ Couns. 2010;80:94–9. [DOI] [PubMed] [Google Scholar]
- 175.Légaré F, Kearing S, Clay K, et al. Are you SURE?: Assessing patient decisional conflict with a 4-item screening test. Can Fam Physician. 2010;56:e308–14. [PMC free article] [PubMed] [Google Scholar]
- 176.Scholl I, Kriston L, Dirmaier J, et al. Development and psychometric properties of the Shared Decision Making Questionnaire–physician version (SDM-Q-Doc). Patient Educ Couns. 2012;88:284–90. [DOI] [PubMed] [Google Scholar]
- 177.Billioux A, Verlander K, Anthony S, et al. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. NAM Perspectives Discussion Paper, National Academy of Medicine, Washington, DC: Available at: https://nam.edu/wp-content/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pdf. Accessed July 15, 2019. [Google Scholar]
- 178.Khaing W, Vallibhakara SA, Attia J, et al. Effects of education and income on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24:1032–42. [DOI] [PubMed] [Google Scholar]
- 179.Schultz WM, Kelli HM, Lisko JC, et al. Socioeconomic status and cardiovascular outcomes: challenges and interventions. Circulation. 2018;137:2166–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Beauchamp A, Peeters A, Tonkin A, et al. Best practice for prevention and treatment of cardiovascular disease through an equity lens: a review. Eur J Cardiovasc Prev Rehabil. 2010;17:599–606. [DOI] [PubMed] [Google Scholar]
- 181.Pollitt RA, Rose KM, Kaufman JS. Evaluating the evidence for models of life course socioeconomic factors and cardiovascular outcomes: a systematic review. BMC Public Health. 2005;5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Malambo P, Kengne AP, De Villiers A, et al. Built environment, selected risk factors and major cardiovascular disease outcomes: a systematic review. PLoS ONE. 2016;11:e0166846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.DeFilippis AP, Young R, McEvoy JW, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic cardiovascular disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38:598–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Berkowitz SA, Hulberg AC, Standish S, et al. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med. 2017;177:244–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–98. [DOI] [PubMed] [Google Scholar]
- 186.Carnethon MR, Pu J, Howard G, et al. Cardiovascular health in African Americans: a scientific statement from the American Heart Association. Circulation. 2017;136:e393–423. [DOI] [PubMed] [Google Scholar]
- 187.Rodriguez CJ, Allison M, Daviglus ML, et al. Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation. 2014;130: 593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in south Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018;138:e1–34. [DOI] [PubMed] [Google Scholar]
- 189.Backholer K, Peters SAE, Bots SH, et al. Sex differences in the relationship between socioeconomic status and cardiovascular disease: a systematic review and meta-analysis. J Epidemiol Community Health. 2017;71:550–7. [DOI] [PubMed] [Google Scholar]
- 190.IOM (Institute of Medicine). 2014. Capturing social and behavioral domains and measures in electronic health records: Phase 2. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 191.Vilhelmsson A, Östergren P-O. Reducing health inequalities with interventions targeting behavioral factors among individuals with low levels of education - a rapid review. PloS ONE. 2018;13:e0195774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Elo AL, Leppanen A, Jahkola A. Validity of a single-item measure of stress symptoms. Scand J Work Environ Health. 2003;29:444–51. [DOI] [PubMed] [Google Scholar]
- 193.Smith CD, Balatbat C, Corbridge S, et al. Implementing optimal team-based care to reduce clinician burnout. Available at: https://nam.edu/implementing-optimal-team-based-care-to-reduce-clinician-burnout/. Accessed July 15, 2019.
- 194.Carter BL, Rogers M, Daly J, et al. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169:1748–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Clark CE, Smith LFP, Taylor RS, et al. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ. 2010;341:c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3:e000718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Shaw RJ, McDuffie JR, Hendrix CC, et al. Effects of nurse-managed protocols in the outpatient management of adults with chronic conditions: a systematic review and meta-analysis. Ann Intern Med. 2014;161:113–21. [DOI] [PubMed] [Google Scholar]
- 198.Brownstein JN, Chowdhury FM, Norris SL, et al. Effectiveness of community health workers in the care of people with hypertension. Am J Prev Med. 2007;32:435–47. [DOI] [PubMed] [Google Scholar]
- 199.Proia KK, Thota AB, Njie GJ, et al. Team-based care and improved blood pressure control: a community guide systematic review. Am J Prev Med. 2014;47:86–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.TeamSTEPPS® Long-Term Care Implementation Guide. Available at: https://www.ahrq.gov/teamstepps/longtermcare/implement/implguide.html. Accessed July 15, 2019.
- 201.Carter BL, Coffey CS, Ardery G, et al. Cluster-randomized trial of a physician/pharmacist collaborative model to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2015;8:235–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Shah BR, Thomas KL, Elliot-Bynum S, et al. Check it, change it: a community-based intervention to improve blood pressure control. Circ Cardiovasc Qual Outcomes. 2013;6:741–8. [DOI] [PubMed] [Google Scholar]
- 203.Bosworth HB, Olsen MK, Grubber JM, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med. 2009;151:687–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Bosworth HB, Powers BJ, Olsen MK, et al. Home blood pressure management and improved blood pressure control: results from a randomized controlled trial. Arch Intern Med. 2011;171:1173–80. [DOI] [PubMed] [Google Scholar]
- 205.Brennan T, Spettell C, Villagra V, et al. Disease management to promote blood pressure control among African Americans. Popul Health Manag. 2010;13:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299:2857–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Heisler M, Hofer TP, Schmittdiel JA, et al. Improving blood pressure control through a clinical pharmacist outreach program in patients with diabetes mellitus in 2 high-performing health systems: the adherence and intensification of medications cluster randomized, controlled pragmatic trial. Circulation. 2012;125:2863–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Liu S, Dunford SD, Leung YW, et al. Reducing blood pressure with Internet-based interventions: a meta-analysis. Can J Cardiol. 2013;29:613–21. [DOI] [PubMed] [Google Scholar]
- 209.Omboni S, Gazzola T, Carabelli G, et al. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: meta-analysis of randomized controlled studies. J Hypertens. 2013;31:455–467; discussion 467–8. [DOI] [PubMed] [Google Scholar]
- 210.Verberk WJ, Kessels AGH, Thien T. Telecare is a valuable tool for hypertension management, a systematic review and meta-analysis. Blood Press Monit. 2011;16:149–55. [DOI] [PubMed] [Google Scholar]
- 211.Agarwal R, Bills JE, Hecht TJW, et al. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011;57:29–38. [DOI] [PubMed] [Google Scholar]
- 212.Burke LE, Ma J, Azar KMJ, et al. Current science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. 2015;132:1157–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Institute of Medicine (US). Crossing the quality chasm: a new health system for the 21st century. Washington, DC: The National Academies Press; 2001. [PubMed] [Google Scholar]
- 214.O’Brien E, Stergiou GS. The pursuit of accurate blood pressure measurement: a 35-year travail. J Clin Hypertens (Greenwich). 2017;19:746–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Yi SS, Tabaei BP, Angell SY, et al. Self-blood pressure monitoring in an urban, ethnically diverse population: a randomized clinical trial utilizing the electronic health record. Circ Cardiovasc Qual Outcomes. 2015;8:138–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Banegas JR, Ruilope LM, de la Sierra A, et al. Relationship between clinic and ambulatory blood-pressure measurements and mortality. N Engl J Med. 2018;378:1509–20. [DOI] [PubMed] [Google Scholar]
- 217.Monitoring Your Blood Pressure at Home. Available at: https://www.heart.org/en/health-topics/high-blood-pressure/understanding-blood-pressure-readings/monitoring-your-blood-pressure-at-home#.WcQNfLKGMnM. Accessed July 15, 2019.
- 218.American Heart Association. At home blood pressure monitoring. Available at: https://newsroom.heart.org/file?fid=5b90209e2cfac208f5b46be0. Accessed July 15, 2019.
- 219.Standards of Medical Care in Diabetes—2016: summary of revisions. Diabetes Care. 2016;399(suppl 1):S4–5. [DOI] [PubMed] [Google Scholar]
- 220.Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2014;130:1749–67. [DOI] [PubMed] [Google Scholar]
- 221.Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012;126:e354–471. [DOI] [PubMed] [Google Scholar]
- 222.Jaffe MG, Young JD. The Kaiser Permanente Northern California story: improving hypertension control from 44% to 90% in 13 years (2000 to 2013). J Clin Hypertens (Greenwich). 2016;18:260–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Smith SC, Benjamin EJ, Bonow RO, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011;124:2458–73. [DOI] [PubMed] [Google Scholar]
- 224.Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;128:e240–327. [DOI] [PubMed] [Google Scholar]
- 225.Navar-Boggan AM, Shah BR, Boggan JC, et al. Variability in performance measures for assessment of hypertension control. Am Heart J. 2013;165:823–7. [DOI] [PubMed] [Google Scholar]
- 226.Powers BJ, Olsen MK, Smith VA, et al. Measuring blood pressure for decision making and quality reporting: where and how many measures? Ann Intern Med. 2011;154:781–8, W-289–90. [DOI] [PubMed] [Google Scholar]
- 227.de Lusignana S, Gallagher H, Jones S, et al. Audit-based education lowers systolic blood pressure in chronic kidney disease: the Quality Improvement in CKD (QICKD) trial results. Kidney Int. 2013;84: 609–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Svetkey LP, Pollak KI, Yancy WS, et al. Hypertension improvement project: randomized trial of quality improvement for physicians and lifestyle modification for patients. Hypertension. 2009;54:1226–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


