Abstract
Introduction
The original use of face masks was to help protect surgical wounds from staff-generated nasal and oral bacteria. Currently governments across the world have instituted the mandatory use of masks and other face coverings so that face masks now find much broader usage in situations where close contact of people is frequent and inevitable, particularly inside public transport facilities, shopping malls and workplaces in response to the COVID-19.
Objective
We conducted a rapid review to investigate the impact face mask use has had in controlling transmission of respiratory viral infections.
Method
A rapid review was conducted in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidance. Five electronic databases (CINAHL, Embase, Medline, PsycINFO and Global Health) were searched from database inception to date, using pre-defined search terms. We included all studies of any design and used descriptive analysis to report summary statistics of search results. Data were extracted including sample characteristics, study design, respiratory virus being controlled, type of face masks used and their effectiveness.
Results
58 out of 84 studies met the inclusion criteria, of which 13 were classified as systematic reviews and 45 were quantitative studies (comprising randomised controlled trials, retrospective cohort studies, case control, cross-sectional, surveys, observational and descriptive studies). N = 27 studies were conducted amongst healthcare workers wearing face masks, n = 19 studies among the general population, n = 9 studies among healthcare workers the general population and patients wearing masks, and n = 3 among only patients. Face masks use have shown a great potential for preventing respiratory virus transmission including COVID-19.
Conclusion
Regardless of the type, setting, or who wears the face mask, it serves primarily a dual preventive purpose; protecting oneself from getting viral infection and protecting others. Therefore, if everyone wears a face mask in public, it offers a double barrier against COVID-19 transmission.
Keywords: COVID-19, Face mask, Pandemic, Prevention, Respiratory viral infection, Rapid review
What is already known about the topic
-
•
The effectiveness of face masks for preventing respiratory virus transmission is still under debate
-
•
Despite face masks being cheaper and easier to use, more research has been carried out on the efficacy of respirators than on face masks
What this paper adds
-
•
Findings suggest that the correct and early use of facemask or face covering could prevent the spread respiratory virus transmission including COVID-19 than when it is not used
-
•
Regardless of the type, setting, or who wears the face mask, it serves primarily a dual preventive purpose of protecting oneself from getting viral infection and protecting others.
-
•
The prolong use of face masks may affect a person's oxygen concentration level and may lead to dizziness due to repeated rebreathing of carbon dioxide retention.
1. Introduction
Since Wells (Wells, 1934) first hypothesised droplet nuclei transmission of airborne infections in the 1930s, and many pathogens have been identified as transmittable through airborne routes (Fiegel et al., 2006, Eames et al., 2009). When a contagious person coughs or sneezes, droplets containing infectious particles (bacteria and viruses) are released (Nicas et al., 2005, Chao et al., 2009). Despite the potential public health implications or airborne transmission, it had not garnered serious global attention until the severe acute respiratory syndrome and human swine influenza pandemics in 2003 and 2009 respectively, which revealed the ramifications of such pandemics on global health and economy. After these pandemics, diverse studies have been conducted to investigate ways to control and reduce infections caused by airborne pathogens.
Respiratory infections can be transmitted by droplets of varying sizes: >5–10 μm in diameter (respiratory droplets), and <5 μm in diameter (droplet nuclei) (World Health Organization, 2014). Airborne transmission, which is the presence of microbes within droplet nuclei, is different from droplet transmission and can remain in the air for long periods of time and be transmitted to others over distances greater than 1 m. Although initial evidence suggested that COVID-19, which was declared a pandemic within three months of its emergence (World Health Organization, 2020), is primarily transmitted through respiratory droplets and contact routes (Liu et al., 2020, Chan et al., 2020, Li et al., 2020, Huang et al., 2020, Burke and Midgley, 2020), more recent research suggests that airborne transmission plays a very significant role in propagating the infection, similar to what was found in severe acute respiratory syndrome coronavirus 1 (SARS-COV1), its predecessor. There are different groups of approaches to control airborne diseases. Ventilation and air flow patterns have been widely investigated to study their influence on droplet transmission (Li et al., 2007, Strasser and Schlich, 2020). Active devices such as air cleaners may also be an effective control measure to reduce exposure when they are properly located relative to the infected person (Chen et al., 2010). Respiratory protective equipment such as facemasks and N95 respirators also provide personal protection against infection (Jefferson et al., 2009, van der Sande et al., 2008). Despite face masks being cheaper and easier to use, more research has been carried out on testing the efficacy of respirators than on face masks (Bałazy et al., 2006, Beest et al., 2010).
The original use of face masks was to help protect surgical wounds from staff-generated nasal and oral bacteria (Meleny and Stevens, 1926, Romney, 2001), among others. Currently governments across the world have instituted the mandatory use of masks and other face coverings so that face masks now find much broader usage in situations where close contact of people is frequent and inevitable, particularly inside public transport facilities, shopping malls and workplaces in response to the COVID-19 (GOV.UK, 2020). However, despite much research effort, the effectiveness of face masks for preventing the contraction of respiratory virus influenza is still under debate and the results presented are not viewed as conclusive (van der Sande et al., 2008, Cowling et al., 2008, Jacobs et al., 2009). Nevertheless, some recent research results have observed that face masks significantly reduce the risk of contracting influenza-like illnesses in households (Perski et al., 2020).
A rapid systematic review of randomised controlled trials using different interventions to assess the efficacy of face masks and respirators against respiratory virus transmission including coronaviruses found masks to be effective in the community; respirators worn by healthcare workers were also found to be effective, but only if worn continually; however, medical and cloth masks were less effective (MacIntyre and Chughtai, 2020). Owing to these varying medical and public perceptions of the impact of wearing face masks in preventing COVID-19, we aimed to conduct a rapid review of all study designs to investigate the impact face mask use has had in controlling transmission of respiratory viral infections.
2. Method
2.1. Review questions
-
1.
What useful lessons exist from the use of face masks in controlling respiratory virus transmission in the past?
-
2.
Which group of people would benefit the most from the use of face masks, to guide the efficient use and allocation of limited supplies and save cost?
2.2. Design
We conducted a rapid review in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (Moher et al., 2009).
2.3. Search strategy
Relevant studies were identified by searching electronic databases: CINAHL, Embase, Medline, PsycINFO and Global Health, and searching reference lists of included studies to identify additional studies. Studies published in English from inception of these databases to June 2020 were included.
The search strategy combined the keywords i) ‘Face mask’ OR ‘Respiratory protective equipment’ OR ‘face covering’ AND ii) ‘Severe Acute Respiratory Syndrome’ OR ‘Coronavirus/ COVID-19′ OR ‘Middle East Respiratory Syndrome’ OR ‘Respiratory virus’ OR ‘Influenza virus’ OR ‘Respiratory infection’ OR ‘Adult respiratory distress syndrome’ OR ‘Respiratory distress syndrome’ AND iii) ‘Cough’ OR ‘Sneeze’ OR ‘Droplet’ AND iv) ‘Impact’ OR ‘Effectiveness’. Multiple keywords were used including the abbreviated names of all respiratory viral infections (SARS-CoV-1, SARS-CoV-2, HIN1, among others) to broaden the search and increase sensitivity to the databases.
2.4. Inclusion and exclusion criteria
The inclusion criteria were primary and secondary studies of all designs including peer-reviewed research studies, review papers, dissertations and grey literature. Details of inclusion and exclusion criteria are listed in Table 1.
Table 1.
Inclusion and exclusion criteria.
| Inclusion | Exclusion |
|---|---|
| Qualitative, quantitative, mixed methods research, systematic reviews and randomised controlled trials, | Protocols, opinion, discussion and editorial papers, including letters. |
| All persons/study participants who have used face masks to prevent the transmission of respiratory viral infections. | Persons wearing face masks for purposes other than the prevention of the transmission of respiratory viral infections. |
| All countries and settings (health institutions, community settings, residential and care homes) |
Data selection and extraction.
The first reviewer (MA-O) imported all search results to Endnote reference manager version X9, de-duplicated, then screened titles and abstracts of all identified studies. Three authors (MA-O, BA, RO-P) screened retained studies against inclusion/ exclusion criteria, any article for which inclusion was unclear was discussed and adjudicated by authors (JB and YS). Full texts of the articles were obtained if abstracts did not contain sufficient information to determine the relevance of an article. We extracted variables such as sample size and characteristic, aims/objectives, design, respiratory virus being controlled by face mask, type of face mask used, impact/effectiveness of face mask controlling respiratory virus and sample size and final conclusions drawn to a common table (see Table 3). Studies not meeting the inclusion criteria were excluded from the analysis.
Table 3.
Studies included on face mask use to prevent respiratory virus transmission n = 58.
| No. | Author/ Year/ Country | Sample size | Sample characteristics | Study aim | Design | Respiratory virus being controlled by face mask | Type of face mask used | Impact/ Effectiveness of face mask controlling respiratory virus | Conclusion/ Comments |
|---|---|---|---|---|---|---|---|---|---|
| 1 | (Aiello et al., 2010) USA |
1437 | College students | To examine whether use of face masks and hand hygiene reduced the incidence of influenza-like illness | Randomised controlled trial | Seasonal Influenza-like illness | Masks + hand washing Control | We observed significant reductions in influenza-like illness during weeks 4–6 in the mask and hand hygiene group, compared with the control group, ranging from 35% (confidence interval 9%−53%) to 51% (Confidence Interval 13%−73%), after adjusting for vaccination and other covariates. Face mask use alone showed a similar reduction in influenza-like illness compared with the control group, but adjusted estimates were not statistically significant. | These findings suggest that face masks and hand hygiene may reduce respiratory illnesses in shared living settings and mitigate the impact of the influenza A pandemic. |
| 2 | (Aiello et al., 2012) USA |
1178 | College students | To examine if the use of face masks and hand hygiene reduced rates of influenza-like illness and laboratory-confirmed influenza in the natural setting. | Randomised controlled trials | influenza-like illness and laboratory-confirmed influenza | Masks Masks + hand hygiene Control |
A significant reduction in the rate of influenza-like illness was observed in weeks 3 through 6 of the study, with a maximum reduction of 75% during the final study week (rate ratio = 0.25, [95% Confidence Interval, 0.07 to 0.87]). Both intervention groups compared to the control showed cumulative reductions in rates of influenza over the study period, although results did not reach statistical significance. | Face masks and hand hygiene combined may reduce the rate of influenza-like illness and confirmed influenza in community settings. These non- pharmaceutical measures should be recommended in crowded settings at the start of an influenza pandemic. |
| 3 | (Barasheed et al., 2014) Saudi Arabia |
164 | Hajj pilgrims | To test the effectiveness of face masks against syndromic and laboratory-confirmed infections among Australian pilgrims to assess the feasibility of such a large-scale trial in the coming years. | A randomised pilot study | Influenza and other respiratory infections | Mask and control | Mask use compliance was 76% in the ‘mask’ group and 12% in the ‘control’ group. Based on developing syndromic influenza-like illness, less contacts became symptomatic in the ‘mask’ tents compared to the ‘control’ tents (31% versus 53%, p = 0.04). However, laboratory results did not show any difference between the two groups. | This pilot study shows that a large trial to assess the effectiveness of face masks use at Hajj is feasible. |
| 4 | (Bartoszko et al., 2020) | 4 studies | Healthcare workers | To compare medical masks to N95 respirators in preventing viral respiratory infections | Systematic review and meta-analysis | SARS-CoV, SARS-CoV-2, influenza | Surgical mask, N95 mask | Medical masks are as good as N95 masks in protecting healthcare workers against laboratory confirmed viral respiratory infections when performing routine care including non-aerosol-generating care. | N95 masks required during aerosol-generating care |
| 5 | (Benkouiten and Brouqui, 2014) | 17 studies | General population on Hajj pilgrimage | To summarize evidence related to the effectiveness of non-pharmaceutical measures in preventing spread of respiratory diseases during Hajj | Systematic review | Respiratory infection | Surgical mask | 3 studies showed significant reduction in respiratory symptoms with surgical mask use. Several other studies found no significant effect of surgical mask use on respiratory symptoms. |
None of the studies established conclusively any relationship between mask use and prevention of respiratory infection. |
| 6 | (Bin-Reza et al., 2012) | 17 studies | Healthcare workers and general population | To review face mask and respirator use in an influenza pandemic | Systematic review | Influenza Virus | Surgical mask, N95 mask/respirator | None of the studies provided conclusive evidence of a relationship between mask or respirator use and prevention of influenza transmission. | Evidence on influenza transmissibility is limited and conflicting. |
| 7 | (Bischoff et al., 2007) USA |
10 | Healthcare workers | Exploring the efficacy of the barrier precautions currently used in the healthcare setting for preventing airborne dispersal, as well as in how a common cold might impact the efficacy of these precautions. | Quantitative study | Rhinovirus induced common cold | N95 | Decrease in airborne spread when participants wear facemasks. | Wearing a face mask can prevent the spread of some microorganisms to some extent. |
| 8 | (Canini et al., 2010) France |
306 | Household subjects | To evaluate the effectiveness of surgical face masks for limiting influenza transmission by large droplets produced during coughing. | A cluster randomised controlled trial | Influenza | Surgical masks | influenza-like illness was reported in 24/148 (16.2%) of the contacts in the intervention arm and in 25/158 (15.8%) of the contacts in the control arm and the difference between arms was 0.40% (95%CI: −10% to 11%, P = 1.00). We observed a good adherence to the intervention. In various sensitivity analyses, we did not identify any trend in the results suggesting effectiveness of face masks | This study should be interpreted with caution since the lack of statistical power prevents us from drawing formal conclusions regarding effectiveness of facemasks in the context of a seasonal epidemic. |
| 9 | (Cheng et al., 2020) China |
10,050 | General population | To assess the effect of community-wide mask usage in controlling COVID-19 | Observational study | SARS-CoV-2 | Any mask | 961/10,050 infected with COVID-19. 113/infected 961 were engaged in mask-off activities in recreational settings. 11/961 were engaged in mask-on settings at the workplace. The number of people infected with SARS-CoV-2 were significantly higher amongst those engaged in mask-off activities in public. |
Compliance with mask wearing in public settings significantly reduces the incidence of COVID-19. |
| 10 | (Christie et al., 1995) USA |
206 | Hospital employees and patients | This study aims to describe methods of preventing nosocomial pertussis in patients, employees, and visitors to a hospital during a communitywide epidemic in greater Cincinnati. | Descriptive Study | Nosocomial Bordetella pertussis |
Surgical mask | The wearing of surgical masks for all persons who entered this area prevented potential pertussis exposures | The use of surgical masks prevented the spread of the bacteria. |
| 11 | (Chu et al., 2020) | 44 studies | Healthcare workers and general population | To evaluate the effect of face mask on transmission of coronavirus | Systematic review and meta-analysis | SARS-CoV-2, SARS-CoV, MERS-CoV | N95 mask, surgical mask, other mask types (paper, reusable cotton) | Use of face masks associated with protective benefits for both health care workers and general population | Optimum use of face masks, respirators and eye protection in public and health-care settings should be informed by these findings. |
| 12 | (Condon and Sinha, 2009) Mexico |
5200 | Anyone that visited the Metro station (study site) with the 13 days when study was conducted | To investigate the prevalence of using face\. mask in public venues when having influenza- like illness | Observational study | Influenza A H1N1 | Surgical masks, and the rest used the N95 respirators | Face mask usage peaked corresponded approximately with when the severity of the public health measures was announced. Females were observed to use the face masks frequently as compared to males. Taxi drivers were interested in wearing face masks during the pandemic because they feared their vehicles will be seized or passengers not patronize their vehicles. |
Gender differences in the use of the face mask during a pandemic. Public health preventive measures campaigns were very effective to compliance of using the face mask. The economic loss associated with non-compliance to wearing a face mask during a pandemic is crucial. |
| 13 | (GOV.UK 2020) Hong Kong |
198 | Households | To test whether two such non-pharmaceutical interventions can reduce transmission of inter-pandemic influenza in households. | A cluster randomised controlled trial | Influenza | Medical masks | There was no significant change in those wearing masks and those who did not wear masks | In conclusion, there remains a serious deficit in the evidence base of the efficacy of non-pharmaceutical interventions. |
| 14 | (Cowling et al., 2009) Hong Kong |
407 | Households | To investigate whether hand hygiene and use of face masks prevents household transmission of influenza | A cluster randomised controlled trial | Influenza | Hand hygiene masks + hand hygiene control | Sixty (8%) contacts in the 259 households had confirmed influenza virus infection in the 7 days after intervention. Hand hygiene with or without face masks seemed to reduce influenza transmission, but the differences compared with the control group were not significant. In 154 households in which interventions were implemented within 36 h of symptom onset in the index patient, transmission of confirmed infection seemed reduced, an effect attributable to fewer infections among participants using face masks plus hand hygiene | Hand hygiene and face masks seemed to prevent household transmission of influenza virus when implemented within 36 h of index patient symptom onset. These findings suggest that non-pharmaceutical interventions are important for mitigation of pandemic and inter-pandemic influenza. |
| 15 | (Heinzerling et al., 2020) USA |
43 | Healthcare workers | To investigate risk factors for covid-19 infection | Retrospective cohort study | SARS-CoV-2 | No face mask | All healthcare workers wore no masks during routine care and aerosol generating procedures. 3/43 got infected. | Sample size too small to draw any conclusion. However, wearing a mask is better than not wearing one. |
| 16 | (Hogg et al., 2006) Canada |
163 | 53 participating offices. 110 physicians |
The study aims to assess whether a short-term outreach facilitated intervention could be effective in improving practices for control of respiratory infections in family physicians’ offices. |
Quantitative study | SARS |
Specific type of face masks was not mentioned | Before the intervention, Physicians barely (17%) offered masks to patients presenting with symptoms of fever and cough. However, after the intervention this increased (66%). | Enforcing preventive measures amongst health care professionals is effective for control of respiratory infections. |
| 17 | (Inouye et al., 2006) Japan |
Not Stated | Patients | The aim of the study is to use an ultrasonic anemometer to measure the velocity of the airflow from the mouth in coughing, and compare three kinds of masks of various prices with regards to their ability to reduce the airspeed | Quantitative study | Influenza virus |
Three types of masks a. Made of paper b. Made of cotton gauze c. Made of polypropylene nonwoven fabric |
It was found that all the masks were able to reduce the air speed when a patient cough, even the cheapest face masks. |
There was a decrease in the virus spread from the patients irrespective of the type of mask used |
| 18 |
Jacobs et al. 2009 Japan |
2464 |
Healthcare workers in a tertiary care hospital | Use of surgical face masks to reduce the incidence of the Common Cold among healthcare workers |
Randomised controlled trial | Common Cold |
Surgical masks vs Control |
There were 2 colds during this time period, 1 in each group. Of the 8 symptoms recorded daily, subjects in the mask group were significantly more likely to experience headache during the study period (P < 0.05). Subjects living with children were more likely to have high cold severity scores over the course of the study. | Face mask use has not been demonstrated to provide benefits in terms of common cold symptoms \. or getting cold. |
| 19 | Jim et al., 2009 |
67 studies | Healthcare workers and general population | To review the evidence of effectiveness of physical interventions to interrupt or reduce the spread of acute respiratory viruses | Systematic review and meta-analysis | Viral respiratory viruses | N95 and surgical masks | Masks found to be the best intervention across populations and settings for prevention of transmission of respiratory viruses. Evidence to support the greater efficacy of N95 respirators over surgical mask limited. |
N95 has potential superior benefit in high-risk situations but further studies are needed to establish it and identify high-risk situations. |
| 20 | (Johnson et al., 2009) Australia |
9 | Patients | To assess the efficacy of both standard surgical masks and N95 masks to adequately filter influenza virus among patients with laboratory-proven acute influenza A and B to determine which was more appropriate to prevent spread. |
Quantitative assessment | Acute influenza infection | Surgical mask N95 (participants coughed 5 times onto a Petri dish wearing each device) |
Surgical and N95 masks appeared to be equally effective in filtering influenza, given that no influenza could be detected by RT-PCR of the ISP viral transport medium in any of the 9 participants for either mask. |
Both surgical and N95 masks appear equally effective in preventing influenza dissemination from patients with confirmed influenza. |
| 21 | (Ki et al., 2019) South Korea |
446 | Healthcare workers | To evaluate Middle East Respiratory Syndrome transmission and the role of routine infection prevention and control policies in reducing nosocomial outbreaks | Retrospective care-cohort study | MERS-CoV | Surgical mask | Surgical masks worn by 93% in the emergency department, 1.8% in the general ward. Although the percentage of high-risk individuals in the emergency department was higher than in the general ward (14.5% vs. 2.8%), the rate of infection was higher in the general ward (16.7%; 1/6) than the emergency department (3%; 1/33). |
Routine wearing of surgical masks can help reduce the transmission of MERS-CoV. |
| 22 | (Kim et al., 2015) South Korea |
9 | Healthcare workers | To investigate MERS-CoV transmission among contacts of healthcare workers | Retrospective case-cohort study | MERS-CoV | N95, Surgical mask | 6 wore surgical masks, 1 wore N95 masks, 2 wore no masks. None of those who wore a mask got infected. The two who wore no mask got infected. | N95 and surgical and surgical masks provide adequate protection from MERS-CoV. |
| 23 | (Kim et al., 2016) South Korea |
737 | Healthcare workers | To evaluate the prevalence and incidence of MERS-CoV in healthcare workers exposed to MERS-CoV patients | Survey | MERS-CoV | N95, Powered Air-Purifying Respirator | Almost all MERS-CoV infected healthcare workers did not wear an N95 mask during contact with Middle East Respiratory Syndrome positive patients. However, 2 wore N95 during aerosol-generating care and were infected. The authors were of the view that N95 masks are not totally effective in preventing MERS-CoV infection during aerosol-generating care due to the associated micro droplets. | Appropriate use of N95 masks is important in preventing MERS-CoV transmission. |
| 24 | (Larson et al., 2010) USA |
617 | Households, | To compare the impact of three household interventions: education, education with alcohol-based hand sanitizer, and education with hand sanitizer and face masks on incidence and secondary transmission of upper respiratory infections (URIs) and influenza, knowledge of transmission of URIs, and vaccination rates. | A Randomized Intervention Trial |
Upper respiratory tract infection and Influenza |
Health education Hand hygiene + health education Masks + hand hygiene +health education |
Despite the fact that compliance with mask wearing was poor, mask wearing as well as increased crowding, lower education levels of caretakers, and index cases 0–5 years of age (compared with adults) were associated with significantly lower secondary transmission rates (all p<0.02). |
There was no detectable additional benefit of hand sanitizer or face masks over targeted education on overall rates of upper respiratory tract infection, but mask wearing was associated with reduced secondary transmission and should be encouraged during outbreak situations. |
| 25 | (Lau et al., 2008a) Hong Kong |
1214 | Adults (18–60) General population including persons with influenza-like illness |
To investigate use of face mask and exposure to live birds and perceptions related to bird-to-human H5N1 avian influenza. | Quantitative, Cross Sectional telephone survey. Structured Questionnaires were used. |
H5N1 avian influenza Flu. |
Type of mask not mentioned | 36% said the use of the face masks when they had influenza-like illness symptoms. 92.1% of the respondents believed that wearing face mask in public places could prevent contracting bird-to-human H5N1. Factors associated with the use of face masks when having influenza-like illness symptoms include exposure to live birds, perceived similar symptoms between influenza and bird-to-human H5N1 avian influenza. |
The use of face masks can prevent the transmission of a respiratory viral infection through droplets spread in public places, and from the bird (carrier) to humans. |
| 26 | (Lau et al., 2004) Hong Kong |
1097 | General population | To investigate the risk factors associated with household attack rates and the household member attack rate for different categories of SARS patients | Case-control study | SARS-CoV | Mask type unspecified | The risk of transmission higher when the infected person and the household member were both not wearing mask | Transmission rates may be greatly reduced with precautionary measures taken by household members of SARS patients |
| 27 | (Liang et al., 2020) |
21 studies | Healthcare workers and general population | To evaluate the effectiveness of mask-use to prevent transmission of laboratory-confirmed respiratory virus | Systematic review and meta-analysis | Influenza, SARS-CoV, SARS-CoV-2 | N95 mask, surgical mask, other mask types (paper, reusable cotton) | Masks significantly reduce the risk of transmission of respiratory viruses in both hospital and community settings. | Appropriate use of masks in healthcare and community settings might help mitigate transmission of respiratory virus infections. |
| 28 | (Liu et al., 2009) China |
477 | Healthcare workers | To investigate risk factors for SARS transmission | Retrospective case-control study | SARS-CoV | Multiple layered mask, 16-layer cotton mask, 12-layer cotton mask | 27.3% wore one-layered cotton mask, 7.0% wore multiple layered masks | Any mask found to be better than no mask in preventing infection. However, a multiple-layered mask is better. |
| 29 | (Liung et al., 2020) Hong Kong |
246 | Children and adults |
To determine the potential efficacy of surgical face masks to prevent respiratory virus transmission. |
Randomised controlled trial | Respiratory virus infections |
Mask and control | Surgical face masks significantly reduced detection of influenza virus RNA in respiratory droplets and coronavirus RNA in aerosols, with a trend toward reduced detection of coronavirus RNA in respiratory droplets. | Our results indicate that surgical face masks could prevent transmission of human coronaviruses and influenza viruses from symptomatic individuals. |
| 30 | (Loeb et al., 2004) Canada |
43 | Healthcare workers | To determine risk factors for SARS transmission | Retrospective cohort study | SARS | Surgical mask, N95 mask | 3/23 who consistently wore either of the masks got infected. 5/9 did not consistently wear a mask and got infected. |
Risk of infection reduced by 80% when one wore either of the masks consistently. Risk of infection was associated with N95 half that of the surgical mask. |
| 31 | (Loeb et al., 2009) Canada |
446 | Healthcare workers | To compare the surgical mask with the N95 respirator in protecting health care workers against influenza | Non-inferiority randomized controlled trial | Influenza | Medical masks, targeted N95 | 225 were allocated to receive surgical masks and 221 to N95 respirators. Influenza infection occurred in 50 nurses (23.6%) in the surgical mask group and in 48 (22.9%) in the N95 respirator group (absolute risk difference, −0.73%; 95% CI, −8.8% to 7.3%; P = 0.86), the lower confidence limit being inside the non-inferiority limit of −9%. |
Use of a surgical mask compared with an N95 respirator resulted in non-inferior rates of laboratory-confirmed influenza |
| 32 | (Maclntyre et al., 2009) Australia. |
143 | Households | To test the effectiveness of using face masks to prevent or reduce transmission of influenza-like illness. |
A cluster-randomised household study | Influenza-like illness | Medical masks P2 masks Control |
1. Samples were collected from 141 children; respiratory viruses were detected in 90 (63.8%) children. In 79 (56.0%) of 141 cases, a single pathogen was detected: influenza A in 19/141 (13.5%); influenza B in 7/141 (4.9%). | Masks may therefore play an important role in reducing transmission. |
| 33 | (MacIntyre et al., 2011) China |
1441 |
Healthcare workers | To compare the efficacy of medical masks, N95 respirators (fit tested and non-fit tested), in healthcare workers. |
A cluster randomised controlled trials |
Clinical respiratory illness, influenza-like illness, laboratory- confirmed respiratory virus infection and influenza. |
Masks N95 respirators, fit tested N95 respirators, non-fit tested Control |
The rates of clinical respiratory illness N95 group compared to medical masks. By intention- to-treat analysis, when p-values were adjusted for clustering, non- fit-tested N95 respirators were significantly more protective than medical masks against clinical respiratory illness, but no other outcomes were significant. The rates of all outcomes were higher in the convenience no-mask group compared to the intervention arms. There was no significant difference in outcomes between the N95 arms with and without fit testing. |
Rates of infection in the medical mask group were double that in the N95 group. A benefit of respirators is suggested but would need to be confirmed by a larger trial, as this study may have been underpowered. |
| 34 | (MacIntyre et al., 2013) China |
1669 | Healthcare workers | To compare three policy options for the use of medical masks and N95 respirators in healthcare workers |
Randomised controlled trial |
Clinical respiratory illness and laboratory-confirmed respiratory pathogens in symptomatic subjects. |
Medical Mask N95 (continuous) N95 (targeted) |
N95 Bacterial respiratory tract colonization in subjects with clinical respiratory illness was highest in the medical mask arm (14.7%; 84 of 572), followed by the targeted N95 arm (10.1%; 52 of 516), and lowest in the N95 arm (6.2%; 36 of 581) (P 1⁄4 0.02). After adjusting for confounders, only continuous use of N95 remained significant against CRI and bacterial colonization, and for just CRI compared with targeted N95 use. Targeted N95 use was not superior to medical masks. |
Continuous use of N95 respirators was more efficacious against clinical respiratory illness than intermittent use of N95 or medical masks. |
| 35 | (MacIntyre et al., 2015) Vietnam |
1607 | Healthcare workers | To compare the efficacy of cloth masks to medical masks in hospital healthcare workers. The null hypothesis is that there is no difference between medical masks and cloth masks. |
A cluster randomised controlled trial |
Clinical respiratory illness, influenza-like illness and laboratory- confirmed respiratory virus infection. |
Medical masks, cloth masks, control | The rates of all infection outcomes were highest in the cloth mask arm, with the rate of influenza-like illness statistically significantly higher in the cloth mask arm compared with the medical mask arm. Cloth masks also had significantly higher rates of influenza-like illness compared with the control arm. An analysis by mask use showed influenza-like illness and laboratory- confirmed virus were significantly higher in the cloth masks group compared with the medical masks group. Penetration of cloth masks by particles was almost 97% and medical masks 44%. | This study is the first randomised controlled trial of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Further research is needed to inform the widespread use of cloth masks globally. However, as a precautionary measure, cloth masks should not be recommended for healthcare workers, particularly in high-risk situations, and guidelines need to be updated. |
| 36 | (MacIntyre and Chungtai, 2015) |
13 randomised controlled trials, 33 Non-randomised controlled trials | Healthcare workers and general population | To summarize available evidence on efficacy of face masks and respirators | Systematic review | Respiratory infections | Surgical masks, N95 mask, any face mask (paper mask, reusable cotton mask) | Respirators offer greater protection to healthcare workers than surgical masks. Use of any facemask in community settings associated with reduced community transmission of respiratory infections. | There is a lack of randomised controlled trials on reusable cloth masks. |
| 37 | (MacIntyre et al., 2016) China |
245 | Household | To determine whether medical mask use by sick individuals with influenza-like illness protects well contacts from related respiratory infections |
A cluster randomised controlled trial |
Influenza-like illness | Medical mask worn by sick case Control (no mask) Household contacts Followed for infection. |
Rates of clinical respiratory illness (relative risk (RR) 0.61, 95% CI 0.18 to 2.13), influenza-like illness (RR 0.32, 95% CI 0.03 to 3.13) and laboratory-confirmed viral infections (RR 0.97, 95% CI 0.06 to 15.54) were consistently lower in the mask arm compared with control, although not statistically significant. A post hoc comparison between the mask versus no-mask groups showed a protective effect against clinical respiratory illness, but not against influenza-like illness and laboratory-confirmed viral respiratory infections. | The study indicates a potential benefit of medical masks for source control but is limited by small sample size and low secondary attack rates. Larger trials are needed to confirm efficacy of medical masks as source control. |
| 38 | (MacIntyre et al., 2017) |
2 Randomised control trials, | Healthcare workers | To examine the efficacy of medical masks and N95 masks against respiratory infections | Systematic review | Respiratory infections | N95 mask, surgical mask | Viral respiratory infections significantly lower in the continuous N95 arm and targeted N95 arm. | N95 masks are more beneficial either for use (continuous or targeted). Medical masks do not appear to offer significant protection. |
| 39 | (MacIntyre and Chughtai, 2020) |
19 Randomised controlled trials | Healthcare workers, sick patients and the general public | To review the evidence around the efficacy of masks and respirators for healthcare workers, sick patients and the general public. | A systematic review of randomised controlled trial | Coronaviruses and other respiratory transmissible viruses |
Masks and respirators | Most of these randomised controlled trials used different interventions and outcome measures. In the community, masks appeared to be effective with and without hand hygiene, and both together are more protective. Randomised controlled trials in health care workers showed that respirators, if worn continually during a shift, were effective but not if worn intermittently. Medical masks were not effective, and cloth masks even less effective. When used by sick patients randomised controlled trials suggested protection of well contacts. | The study suggests that community mask use by well people could be beneficial, particularly for COVID-19, where transmission may be pre-symptomatic. The studies of masks as source control also suggest a benefit and may be important during the COVID-19 pandemic in universal community face mask use as well as in health care settings. |
| 40 | (Milton et al., 2013) USA |
38 | Patients | To report the culturalbility of virus in fine particle fraction and the effect of surgical mask |
Quantitative Study |
Seasonal Influenza | Surgical mask | a. Wearin Surgical mask nearly eliminated viral RNA detection in the coarse aerosol fraction. When not wearing mask viral RNA in coarse particles exhaled by 43% and in fine particles exhaled by 92% of influenza patients was detected. |
Wearing of surgical masks reduces the spread of the virus from infected persons to others. |
| 41 | (Offeddu et al., 2017) |
29 studies | Healthcare workers | To assess the effectiveness of medical masks and respirators in protecting healthcare workers from respiratory infections | Systematic review and meta-analysis | Viral respiratory infections | N95 respirator, surgical mask, paper mask, reusable cotton mask | Meta-analysis of randomised controlled trials - masks and respirators are protective against clinical respiratory illness and influenza-like illness but not laboratory confirmed infection. N95 confers greater protection. Meta-analysis of observational studies - both respirators and masks confer protection against SARS but not HINI influenza |
Both respirators and masks are effective in preventing healthcare workers from SARS-CoV infection but not HINI influenza. Paper masks and reusable cotton masks offer no protective benefit and may harbor infections that are not decontaminated appropriately. |
| 42 |
(Park et al., 2004) USA |
110 | Healthcare workers | To determine the extent of SARS transmission | Survey | SARS-CoV | N95 mask or higher respirators | 44/110 had at least one exposure without a respirator (N95 mask or higher respirators). |
None of the healthcare workers got infected. Lack of infection may have resulted from relative absence of highly infectious patients or high-risk procedures. |
| 43 | (Radonovich et al., 2019) USA |
2371 | Healthcare workers | To compare the effect of N95 respirators vs medical masks for prevention of influenza and other viral respiratory infections among healthcare workers | A cluster randomized pragmatic effectiveness study | Incidence of laboratory-confirmed influenza; incidence of acute respiratory illness, laboratory-detected respiratory infections, laboratory-confirmed respiratory illness, and influenza-like illness. | Medical masks, targeted N95 (when 2 m from confirmed respiratory infection) in Outpatient setting. |
There were 207 laboratory-confirmed influenza infection events in the N95 respirator group and 193 in the medical mask group There were 1556 acute respiratory illness events in the respirator group vs 1711 in the mask group; 679 laboratory-detected respiratory infections in the respirator group vs 745 in the mask group; 371 laboratory-confirmed respiratory illness events in the respirator group vs 417 in the mask group; and 128 influenza-like illness events in the respirator group vs 166 in the mask group. In the respirator group, 89.4% of participants reported “always” or “sometimes” wearing their assigned devices vs 90.2% in the mask group. | N95 respirators vs medical masks as worn by participants in this trial resulted in no significant difference in the incidence of laboratory-confirmed influenza. |
| 44 | (Ryu et al., 2019) South Korea |
34 | Public health workers | To determine degree of exposure of public health workers and whether they were infected | Cross-sectional study | MERS-CoV | N95 mask | All wore N95 masks. 1 in full personal protective equipment developed fever. None was infected with laboratory confirmed MERS-CoV. |
Risk of transmission of MERS-CoV outside hospitals is low. |
| 45 | (Saunders-Hastings et al., 2017) Canada |
16 studies | Healthcare workers and general population | To assess the effectiveness of personal protective measures in reducing risk of influenza transmission | Systematic review and meta-analysis | Influenza | Surgical mask | 8/16 studies measured effectiveness of face mask use. They found face mask use to be not significantly protective | Surgical masks have demonstrated mixed results in various studies. A randomised controlled trial has suggested it is effective. |
| 46 | (Scales et al., 2003) Canada |
69 | Healthcare workers | To investigate risk associated with SARS transmission after exposure infected patients | Retrospective survey | SARS-CoV | Surgical mask, N95 mask | 7/69 developed SARS. 6/31 who entered the patient's room got infected. 6 wore surgical masks and 2 got infected. 6 wore N95 masks and 1 got infected. 8 observed no precautions and 1 got infected. |
Airborne transmission may have occurred in some of the situations. |
| 47 | (Seto et al., 2003) China |
254 | Healthcare workers | To assess the effectiveness of droplet precautions for prevention of nosocomial transmission | Case-control study | SARS | Paper mask, N95 Mask, surgical mask | 13 infected; 241 control 2/13 infected used paper masks. None of those infected used surgical masks or N95 masks. |
Mask use was the significant predictor of prevention from being infected. Paper mask did not significantly reduce the risk of infection because it easily gets wet with saliva. |
| 48 | (Smith et al., 2016) |
27 studies | Healthcare workers | To review clinical and surrogate exposure data comparing N95 respirators and surgical face masks for the prevention of transmission of respiratory infections | Systematic review and meta-analysis | Influenza | Surgical facemask, N95 mask | Clinical studies - There was no significant difference between N95 and surgical facemasks in rate of infection. Surrogate exposure studies: N95 respirators were associated with less filter penetration, less face-seal leakage, and less total inward leakage |
Healthcare workers wearing N95 respirators are more likely to contaminate their faces while wearing the mask because it is generally uncomfortable to wear, may be worn improperly and may be adjusted more frequently. Thus, the potential benefits of N95 over surgical masks may be negated. |
| 49 | (Simmerman et al., 2011) Thailand |
465 | General population | To estimate the efficacy of handwashing and face mask use in decreasing influenza transmission | Randomised controlled trial | Influenza virus | Paper surgical mask | No statistically significant benefit found with the use of paper surgical masks in either secondary attack rate or multivariate analysis | There was a poor adherence to interventions - handwashing and face mask use. This may have contributed to the lack of efficacy seen. |
| 50 | (Suess et al., 2012) Germany |
84 index cases and 218 household contacts, | Index cases and household contacts, |
To test the efficacy, adherence and tolerability of facemasks and intensified hand hygiene to prevent influenza transmission in households. |
A cluster randomised controlled trial |
Influenza virus | Masks and Masks + hand hygiene Control |
There was no statistically significant effect of the Masks and Mask + Hand hygiene interventions on secondary infections. However, within households where intervention was implemented within 36 h of symptom onset of the index case, secondary infection in the pooled Mask and Mask+Hand hygiene groups was significantly lower compared to the control group. In a per-protocol analysis odds ratios were significantly reduced among participants of the Mask group. With the exception of Masks+Hand hygiene index cases in 2010/11 adherence was good for adults and children, contacts and index cases. |
Results suggest that household transmission of influenza can be reduced by the use of facemasks and intensified hand hygiene, when implemented early and used diligently. Concerns about acceptability and tolerability of the interventions should not be a reason against their recommendation. |
| 51 | (Teleman et al., 2004) Singapore |
86 | Healthcare workers | To determine risk factors for nosocomial SARS transmission | Case-control study | SARS-CoV | N95 mask | Whilst attending to patients with SARS, 3/36 infected staff wore masks, 23/50 wore no masks. Univariate analysis and logistic regression show significant reduction in odds of infection when wearing a N95 mask. |
Wearing N95 masks was associated with a 10-fold reduction in odds of infection when attending to patients infected with SARS. |
| 52 | (Tuan et al., 2007) Vietnam |
212 | General population | To investigate the risk factors for SARS-CoV transmission | Retrospective survey | SARS-CoV | Mask type not specified | 154/180 wore no mask. 9/180 had laboratory confirmed evidence of infection |
Risk of community transmission is low, requiring intimate unprotected contact. Mask use potentially minimizes risk of infection following exposure. |
| 53 | (Wang et al., 2020a) China |
120 infected healthcare workers | Healthcare workers | To assess the epidemiologic characteristics of COVID-19 in medical staff | Retrospective survey | SARS-CoV-2 | N95 mask, surgical mask | 89/120 used a surgical mask, 25/120 used no mask. 1/120 used N95 mask |
The risk of contracting SARS-CoV-2 was 36.9 times higher in those who used no mask than in those who used N95 masks. |
| 54 | (Wang et al., 2020b) China |
403 | Healthcare workers | To determine association between face mask usage and contracting the virus | Retrospective case-control study | SARS-CoV-2 | N95 | 278/493 wore a mask. None was infected. 213/493 did not wear a mask. 10/213 got infected |
Rate of infection significantly higher in the no mask group as compared to the mask group |
| 55 | (Wilder-Smith et al., 2005) Singapore |
80 | Healthcare workers | To investigate the incidence of asymptomatic SARS-CoV infection and associated factors | Cohort study | SARS-CoV | N95 masks | 50% of those who developed asymptomatic SARS had used masks. 8% of those who developed pneumonic SARS had used masks. |
Use of N95 masks associated with asymptomatic SARS. Non-use of masks associated with pneumonic SARS. Thus, mask use is better. |
| 56 | (Wu et al., 2004) China |
94 case-patients, 281 matched controls | General population | To assess the risk factors for SARS among persons without known contact to SARS patients | Matched case-control study | SARS-CoV | Masks type unspecified | There was a 70% reduction in the risk of infection with SARS when participants wore a mask consistently as compared to not wearing a mask. Intermittent wearing of masks was also found to offer some protection. |
Wearing a mask is significantly protective against development of clinical SARS. |
| 57 | (Xiao et al., 2020) |
10 radomised controlled trials | General population | To evaluate the effectiveness of personal protective measures on transmission of influenza virus | Systematic review and meta-analysis | Influenza | Surgical mask | There was no statistically significant reduction in influenza transmission with the use of surgical mask (RR 0.78, 95% Cl 0.51–1.20; I2=30%, P = 0.25) | Surgical mask use either by the infected or infected person does not affect influenza transmission significantly. |
| 58 | (Laosiritaworn, 2014) Thailand |
General Public (students and workers) | The study aimed to use an agent-based model to estimate influenza burden in Thailand and assess impact of control measures. | Quantitative study Dissertation | Influenza virus |
Surgical mask | The use of face masks is a non-pharmacological intervention that can spread the virus. The use of face masks is an effective strategy for countries that cannot afford vaccines. Face masks are used to limit influenza transmission by minimizing the distribution of large secretion droplets produced during sneezing or coughing. |
Wearing of face masks can be used to reduce the spread of the influenza virus. |
2.5. Analysis
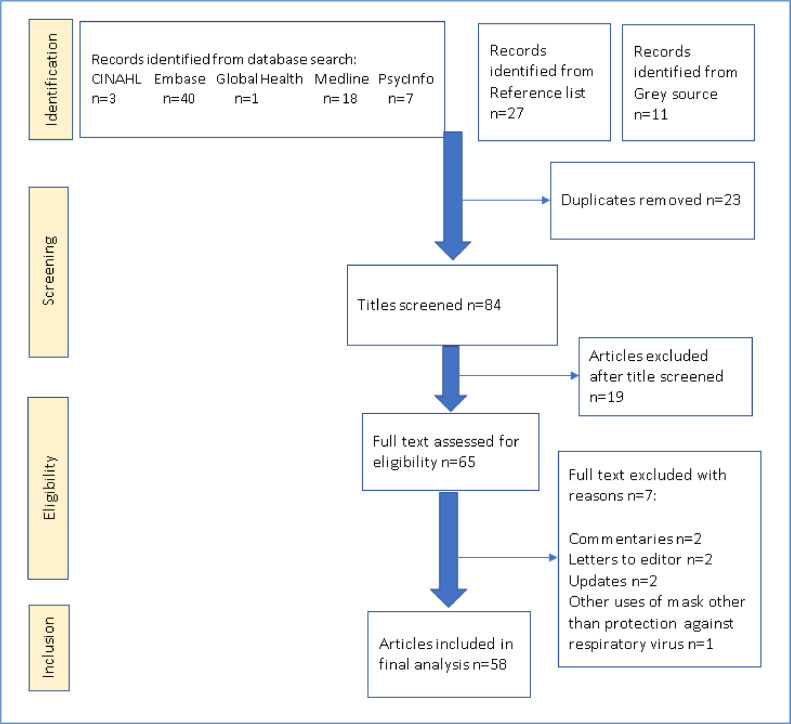
Summary statistics were used to report the number of published studies and presented in a PRISMA flow diagram in Fig. 1. We analysed descriptions of types of face masks by comparing masks vs. no masks, N95 vs. surgical/ medical face masks and other respirators; respiratory virus being controlled and effectiveness of face masks in controlling transmission of respiratory pathogens. All studies (qualitative, quantitative and systematic reviews) were analysed descriptively, and then findings synthesised. All studies addressing any type of respiratory virus/ infection and any type of face mask used were retained in the final analysis.
Fig. 1.
PRISMA flow diagram.
3. Results
3.1. Study characteristics
A total of 84 studies were retrieved through database and reference list search as shown in Fig. 1. Of the 84 studies, 19 irrelevant studies were excluded, leaving 65 studies for full-text review: 7 papers were excluded as they did not meet the inclusion criteria (reasons reported in Fig. 1) and 58 studies met the inclusion criteria. These 58 studies were retained for final analysis. Study designs included were mainly systematic reviews and quantitative studies (comprising randomised controlled trials, retrospective cohort studies, case control, cross-sectional, surveys, observational and descriptive studies). Of the 58 papers included in this review, 13 of them were systematic reviews and 45 were quantitative studies. Countries where these studies were conducted included Mainland China (n = 10); United States of America (USA) (n = 9); Canada (n = 4); Hong Kong (n = 4); South Korea (n = 4); Australia, Japan, Singapore, Thailand, and Vietnam each have two studies; and France, Germany, Mexico and Saudi Arabia each have one study. 13 systematic reviews were conducted by authors from multiple countries (see Table 3 for details of study designs and respective countries where the studies were conducted).
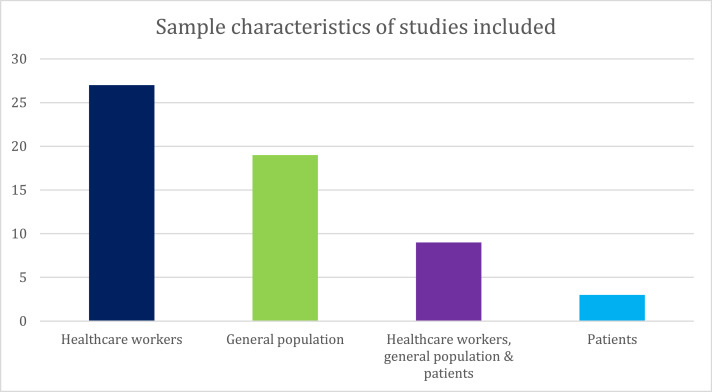
Fig. 2 represents the characteristics of the study samples in the various papers. n = 27 of the papers reported studies conducted amongst healthcare workers wearing face masks, n = 19 studies focused on wearing masks among the general population, n = 9 of the papers focused on a combination of studies of healthcare workers, the general population and patients wearing masks, and n = 3 focused on only patients wearing masks.
Fig. 2.
A plot showing the distribution of participant groups included in the studies reviewed.
Table 2 also represents the distribution of the types of face masks that were studied in the various studies reviewed. n = 14 studies did not mention the type of face masks used, n = 13 studies used surgical masks, n = 12 studies used both surgical and N95 masks, n = 10 used N95, n = 5 studied all types face masks (N95, Surgical Masks, Cotton, Paper, Fabrics etc.), n = 2 used paper, cotton and gauze masks, n = 1 used surgical masks and cloth mask, and n = 1 used N95, surgical masks and paper masks.
Table 2.
Types of face masks and corresponding number of studies that used them.
| Type of face mask used | Number of studies (n) |
|---|---|
| Specific mask not mentioned | n = 14 |
| Surgical masks | n = 13 |
| Both N95 and surgical mask | n = 12 |
| N95 | n = 10 |
| All types (N95, Surgical Masks, Cotton, Paper, Fabrics etc.) | n = 5 |
| Paper, cotton and gauze masks | n = 2 |
| Surgical masks and cloth mask | n = 1 |
| N95, surgical masks and paper masks | n = 1 |
4. Data synthesis
4.1. Types of face masks used to control various respiratory viruses
Majority of the studies (n = 55) included in the review reported the use of various types of face masks to control the transmission of respiratory viruses. Table 4 summarises the types of masks used to control the various respiratory viruses.
Table 4.
Types of face masks used in controlling respiratory virus.
5. Effectiveness of face masks in controlling transmission of respiratory pathogens
5.1. Masks vs. no masks
All studies that compared the use of face mask, irrespective of the type, to non-use of face mask observed a significantly higher rate of infection among the participants who did not use mask. For instance, Wang et al. (2020a) reported no SARS-CoV-2 infection among participants who wore a face mask whilst 10 participants in the no mask group were infected. In similar lines, the risk of contracting SARS-CoV-2 was reported to be 36.9 times higher in those who used no masks (Wang et al., 2020a). In addition, Kim et al. (2016) noted that two participants who did not wear a mask contracted MERS-CoV. Despite the findings above, two studies observed no significant change regarding the use or non-use of face masks in controlling influenza (GOV.UK 2020) or common cold (Cowling et al., 2008).
5.2. N95 vs. surgical/ medical face mask
Mixed findings were reported by studies that compared N95 to surgical/ medical masks. Six studies observed that both forms of face mask offered similar levels of protection in controlling the transmission of respiratory pathogens (Benkouiten and Brouqui, 2014, Johnson et al., 2009, Ki et al., 2019, Kim et al., 2016, Radonovich et al., 2019, Smith et al., 2016). Despite the notion of both forms of face masks offering similar levels of protection in controlling the transmission of SARS-CoV, one study observed that this did not apply to H1N1 influenza (Offeddu et al., 2017). Four studies further highlighted that N95 offered a better form of protection when compared with surgical masks (Loeb et al., 2009, MacIntyre et al., 2017, Scales et al., 2003, Seto et al., 2003). Further, in this regard, MacIntyre et al. (2013) observed that it is the continuous use of N95, rather than the intermittent use that offered an effective protection against clinical respiratory illness. Although Inouye et al. (Jefferson et al., 2011) observed that face masks made from paper, cotton gauze or non-woven fabric provided some protection, Offeddu et al. (2017) highlighted that paper or reusable cotton face masks offered no protection and were associated with a higher risk of harbouring various pathogens when compared to N95 or medical masks. Similarly, MacIntyre et al. (2015) also noted that the use of a double-layered cloth face mask led to a high rate of influenza-like illness as compared to those who used other types of masks. These findings notwithstanding, the study findings by Smith et al. (2016) offers a caution to healthcare professionals as the authors noted that nurses/ physicians are more likely to contaminate their faces while wearing the N95 mask due to the discomfort associated with their use.
5.3. Other respirators
Beside N95 and surgical facemasks, the use of other advanced respirators were noted in the review. One study reported the enhanced efficacy of the Powered Air-Purifying Respirator in controlling/ preventing the transmission of MERS-CoV in comparison to N95 (Larson et al., 2010). The use of other advanced respirators also protected healthcare professionals from contracting SARS-CoV (Park et al., 2004).
5.4. Combined use of masks and hand hygiene
Five studies evaluated the combined effects of face masks and hand hygiene in reducing transmission (Aiello et al., 2012, Barasheed et al., 2014, Heinzerling et al., 2020, Lau et al., 2008a, Suess et al., 2012). Three studies observed that the utilization of mask and hand hygiene significantly lowered the transmission of influenza-like illness (Aiello et al., 2012, Barasheed et al., 2014, Heinzerling et al., 2020). Although Suess et al. (2012) did not observe a statistically significant difference on the combined effects of mask and hand hygiene, the authors noted that commencement of these interventions within 36hours of symptom onset of the index case led to lower rates of transmitting secondary infection among contacts.
6. Discussion
Findings suggest that the correct and early use of facemask or face covering could save many more lives than when it is not used. Mask use could lower the risk of COVID-19 transmission (MacIntyre and Chughtai, 2020, Christie et al., 1995, Hogg et al., 2006, Loeb et al., 2004), SARS (Inouye et al., 2006), Influenza (Ki et al., 2019, Laosiritaworn, 2014), MERS (Kim et al., 2015) and recommended for use in the public (Condon and Sinha, 2009). Additionally, N95 masks seem to provide a better form of protection from influenza-like illness than the other types of masks when used continuously, rather than intermittently (Maclntyre et al., 2009, MacIntyre et al., 2013, MacIntyre et al., 2017) and a multi-layered mask offered better protection (Liung et al., 2020). However, in a randomised controlled trial Smith et al. (2016) concluded that the process of wearing N95 respirators might lead to contamination due to the following factors; 1) N95 is mostly uncomfortable to wear, 2) may be worn improperly and 3) may be adjusted often. This will have implication for clinical practice where the setting could lead to transmission of disease to vulnerable patients, and therefore proper hand washing should be ensured in addition to mask use (Adhikari et al., 2020).
The use of cloth masks was cautioned as it has a greater moisture retention, likely to be reused and may have poor filtration that may result in increased risk of infection when not properly decontaminated (MacIntyre et al., 2015, Offeddu et al., 2017). Paper mask was identified as the worst of them all because they easily moisten and disintegrate (Seto et al., 2003). This, therefore, means that when people use cloth mask; it must be washed after each use and dried and or ironed to reduce the risk of contamination. The general use of face masks was recommended in several countries, such as Mainland China, Hong Kong Special Administrative Region, Singapore, Japan, USA, UK, and Germany in the early period of the outbreak of COVID-19 pandemic (Feng et al., 2020). Additionally, the review findings suggest a need to consider the utilisation of other adjunct measures such as hand hygiene in order to decrease the risk of transmission further. Taken together, the findings offer support to enforce the early and correct use of face masks and meticulous hand hygiene.
Our review shows that wearing a face mask has a great potential in controlling airborne transmitted viruses including COVID-19. This corroborate previous works that indicated that mask use is beneficial to prevent the transmission of COVID-19 (Greenhalgh et al., 2020). Greenhalgh et al. (2020) concluded that wearing a face mask in public should be encouraged regardless, even if the protection it offers is limited. This they argued, will limit transmission of COVID-19 and save some lives. In a narrative rebuttal to critics who disagreed with the contention by Greenhalgh et al. (2020) that face mask could be used as a ‘precautionary measure’ when in public, the author maintained that in time of global health and economic crises a reliance on only ‘perfect evidence’ such as randomised controlled trial evidence, may be the enemy of good policy. A recent rapid systematic review on face mask use and its efficacy against coronavirus and other respiratory viruses found that mask use in public could be beneficial within in the community and clinical settings for the prevention of COVID-19, especially those who have not yet started showing clinical symptoms (MacIntyre and Chughtai, 2020). Their study also indicated that mask use offered respiratory protection from patients (source control) to others. Although this review focused only on randomised controlled trial, which is widely believed to be the ‘gold standard’ for evidence, we contend that for people to accept the use of mask, they do not only need the evidence for its use, but also require the potential and actual problems associated with mask use to be addressed. This study addresses this loophole, since it included all study designs.
We are also cognisant of all the systematic reviews conducted on the use of face masks and other face-covering (MacIntyre and Chughtai, 2020, Bartoszko et al., 2020, Benkouiten and Brouqui, 2014, Bin-Reza et al., 2012, Chu et al., 2020, Jefferson et al., 2011, Liang et al., 2020, MacIntyre and Chungtai, 2015, MacIntyre et al., 2017, Offeddu et al., 2017, Saunders-Hastings et al., 2017, Smith et al., 2016, Xiao et al., 2020). These reviews have mainly focused on: (a) a combination of different primary study designs (Bartoszko et al., 2020, Benkouiten and Brouqui, 2014, Bin-Reza et al., 2012, Chu et al., 2020, Jefferson et al., 2011, Liang et al., 2020, Offeddu et al., 2017, Saunders-Hastings et al., 2017, Smith et al., 2016); (b) only randomised controlled trials (MacIntyre and Chughtai, 2020, MacIntyre and Chungtai, 2015, MacIntyre et al., 2017, Xiao et al., 2020); (c) studied multiple interventions in addition to face-covering (Bin-Reza et al., 2012, Chu et al., 2020, Liang et al., 2020, Offeddu et al., 2017); (d) only healthcare workers and general population (Bin-Reza et al., 2012, Chu et al., 2020, Jefferson et al., 2011, Liang et al., 2020, MacIntyre and Chungtai, 2015, Saunders-Hastings et al., 2017); (e) only healthcare workers (Bartoszko et al., 2020, MacIntyre et al., 2017, Offeddu et al., 2017, Smith et al., 2016); (f) only general population (Benkouiten and Brouqui, 2014, Xiao et al., 2020); and (g) a combination of healthcare workers, general population and patients (MacIntyre and Chughtai, 2020).
Therefore, the findings from this study which reviewed all study designs (including systematic reviews), focusing on all types of study population (healthcare workers, general population and patients), and using face mask to prevent all types of respiratory viral transmission will reinforce the evidence presented in the above reviews. Additionally, these findings could help in drawing a holistic conclusion of the impact of face masks in preventing the spread of respiratory viral infection in order to make policy recommendation for their use. Wearing face masks will not only protect lives but can protect the economy because people can engage in their work, less likely to be infected, are able to prevent possible future lockdowns, and ensure people stay healthy enough to work.
The study findings have significant bearing on nursing practice particularly, regarding the education of the populace and patients on the early and continuous use of appropriate face masks, in addition to other measures (such as hand hygiene) as we navigate the pandemic. As nurses continue to play critical roles as frontline workers, the findings of this review can enhance infection control measures instituted during the COVID-19 pandemic. As noted in the review, the efficacy of some face masks used such as those made from paper and cloth has not been established therefore, further research is required in this regard to strengthen the evidence base. Additionally, the effectiveness of reusable face masks after being washed is another area requiring more evidence. Despite the extensiveness of the current review, some limitations are noteworthy, including reviewing only studies published and reported in English thereby missing out on grey literature and studies published in other languages.
7. Conclusion
This rapid review highlights the impact of face mask use in preventing respiratory virus transmission among healthcare workers, patients and the general population. Findings demonstrate that, regardless of the type, setting, or who wears the face mask, it serves primarily a dual preventive purpose; protecting oneself from getting viral infection and protecting others. Therefore, if everyone wears a face mask in public, it offers a double barrier against COVID-19 transmission. In addition, this review reveal that the prolonged/ continuous use of face masks may affect a person's oxygen concentration level and may lead to dizziness due to repeated rebreathing of carbon dioxide retention. Consequently, we recommended that any future study conducted on the use of masks, investigates the length at which mask can be used at a particular time in order to mitigate these negative health effects.
Controlling the spread of COVID-19 could save lives, prevent possible reintroduction of lockdowns, and ensure that health systems are not overwhelmed with severe cases of COVID-19.
Acknowledgements
I acknowledge all authors for their contribution to this rapid review.
This review was conceived and designed by ………………, and …………. The first reviewer imported all search results to Endnote reference manager version X9, de-duplicated, then all authors screened titles and abstracts of all identified studies, any article for which inclusion was unclear were discussed and if necessary adjudicated by the last reviewer. All authors critically appraised and contributed to the manuscript.
Declaration of Competing Interest
None.
Funding sources
No external funding
Contributor Information
Mary Abboah-Offei, Email: mary.abboah-offei@york.ac.uk.
Yakubu Salifu, Email: y.salifu@lancaster.ac.uk.
Bisi Adewale, Email: adewale@ualberta.ca.
Reference
- Adhikari S.P., Meng S., Wu Y.J., et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect. Dis. Poverty. 2020;9(1):1–12. doi: 10.1186/s40249-020-00646-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28 Aiello A.E., Murray G.F., Perez V. Mask use, hand hygiene, and seasonal influenza-like illness among young adults: a randomized intervention trial. J. Infect. Dis. 2010;201(4):491–498. doi: 10.1086/650396. [DOI] [PubMed] [Google Scholar]
- Aiello A.E., Perez V., Coulborn R.M., Davis B.M., Uddin M., Monto A.S., et al. Facemasks, hand hygiene, and influenza among young adults: a randomized intervention trial. PLoS One. 2012;7(1) doi: 10.1371/journal.pone.0029744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18 Bałazy A., Toivola M., Adhikari A., et al. Do N95 respirators pro- vide 95% protection level against airborne viruses, and how adequate are surgical masks? Am. J. Infect. Control. 2006;34:51–57. doi: 10.1016/j.ajic.2005.08.018. [DOI] [PubMed] [Google Scholar]
- Barasheed O., Almasri N., Badahdah A.M., et al. Pilot randomised controlled trial to test effectiveness of facemasks in preventing influenza-like illness transmission among Australian Hajj Pilgrims in 2011 Infect. Disord. Drug Targets. 2014;14(2):110–116. doi: 10.2174/1871526514666141021112855. [DOI] [PubMed] [Google Scholar]
- Bartoszko J.J., Farooqi M.A.M., Alhazzani W., et al. Medical masks vs N95 respirators for preventing COVID-19 in healthcare workers: a systematic review and meta-analysis of randomized trials. Influenza Other Respir. Viruses. 2020 doi: 10.1111/irv.12745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19 Beest D.E.T., van Boven M., Bos M.E.H., et al. Effectiveness of personal protective equipment and oseltamivir prophylaxis during avian influenza A (H1N1) epidemic, the Netherlands, 2003. Emerg. Infect. Dis. 2010;16:1562–1568. doi: 10.3201/eid1610.091412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benkouiten S., Brouqui G.P. Non-pharmaceutical interventions for the prevention of respiratory tract infections during Hajj pilgrimage. Travel Med. Infect. Dis. 2014;12:429–442. doi: 10.1016/j.tmaid.2014.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bin-Reza F., Lopez Chavarrias V., Nicoll A., et al. The use of masks and respirators to prevent transmission of influenza: a systematic review of the scientific evidence Influenza Other Respir. Viruses. 2012;6(4):257–267. doi: 10.1111/j.1750-2659.2011.00307.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischoff W.E., Tucker B.S., Brian K. Preventing the airborne spread of staphylococcus aureus by persons with the common cold: effect of surgical scrubs, gowns, and masks. Infect. Control Hosp. Epidermiol. 2007;28(10):1148–1154. doi: 10.1086/520734. [DOI] [PubMed] [Google Scholar]
- Burke R.M., Midgley C.M., et al. Active monitoring of persons exposed to patients with confirmed COVID-19 — United States, January-February 2020. MMWR Morb. Mortal Wkly. Rep. 2020 doi: 10.15585/mmwr.mm6909e1externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canini L., Andreoletti L., Ferrari P., et al. Surgical mask to prevent influenza transmission in households: a cluster randomized trial. PLoS One. 2010;5(11):e13998. doi: 10.1371/journal.pone.0013998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9 Chan J., Yuan S., Kok K., et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020 doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5 Chao C.Y.H., et al. Characterization of expiration air jets and droplet size distributions immediately at the mouth opening. J. Aerosol Sci. 2009;40:122–133. doi: 10.1016/j.jaerosci.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15 Chen C., Zhao B., Cui W.L., et al. The effectiveness of an air cleaner in controlling droplet/aerosol particle dispersion emitted from a patient's mouth in the indoor environment of dental clinics. J. R. Soc. Interface. 2010;7:1105–1118. doi: 10.1098/rsif.2009.0516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng V.C., Wong S., Chuang V., et al. The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J. Infect. 2020 doi: 10.1016/j.jinf.2020.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou R., Dana T., Jungbauer R., et al. Masks for prevention of respiratory virus infections, including SARS-CoV-2, in health care and community settings: a living rapid review. Ann. Intern. Med. 2020 doi: 10.7326/M20-3213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christie C.D., Glover A.M., Willke M.J., et al. Containment of pertussis in the regional hospital during the Greater Cincinnati epidermic of 1993. Infect. Control Hosp. Epidiomil. 1995;16(10):556–563. doi: 10.1086/647008. [DOI] [PubMed] [Google Scholar]
- Chu D.K., Akl E.A., Duda S., et al. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020 doi: 10.1016/S0140-6736(20)31142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Condon B.J., Sinha T. Who is that masked person: the use of facemasks on Mexico City public transportation during the Influenza A (H1NI) outbreak. Health Policy. 2009 doi: 10.1016/j.healthpol.2009.11.009. [DOI] [PubMed] [Google Scholar]
- Cowling B.J., et al. Preliminary findings of a ran- domized trial of non-pharmaceutical interventions to prevent influenza transmission in households. PLoS One. 2008;3:e2101. doi: 10.1371/journal.pone.0002101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40 Cowling B.J., Chan K.H., Fang V.J., et al. Facemasks and hand hygiene to prevent influenza transmission in households: a cluster randomized trial. Ann. Intern. Med. 2009;151(7):437–446. doi: 10.7326/0003-4819-151-7-200910060-00142. [DOI] [PubMed] [Google Scholar]
- 3 Eames, et al. Movement of airborne contaminants in a hospital isolation room. J. R. Soc. Interface. 2009;6:S757–S766. doi: 10.1098/rsif.2009.0319.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng S., Chen S., Nan X., et al. Rational use of face masks in the COVID-19 pandemic. Lancet Respir. Med. 2020;8(5):434–436. doi: 10.1016/S2213-2600(20)30134-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2 Fiegel J., Clarke R., Edwards D.A. Airborne infectious disease and the suppression of pulmonary bioaerosols. Drug Discov. Today. 2006;11:51–57. doi: 10.1016/S1359-6446(05)03687-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOV.UK. Coronavirus (COVID-19): safer travel guidance for passengers. GOV.UK. Updated July 2020. See https://www.gov.uk/guidance/coronavirus-covid-19-safer-travel-guidance-for-passengers#public-transport.
- 85 Greenhalgh T., Schmid M.B., Czypionka T., et al. Face masks for the public during the covid-19 crisis. BMJ. 2020;369:1435. doi: 10.1136/bmj.m1435. [DOI] [PubMed] [Google Scholar]
- Heinzerling A., Stuckey M.J., Scheuer T., et al. Transmission of COVID-19 to health care personnel during exposures to a hospitalized patient: solano County, California, February 2020. MMWR Morb. Mortal Wkly. Rep. 2020;69:472–476. doi: 10.15585/mmwr.mm6915e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogg W., Huston P., Martin C., et al. A process evaluation of an intervention to improve respiratory infection contro practices in family physician offices. Can. J. Public Health. 2006;97(5):475–479. doi: 10.1007/BF03405231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11 Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inouye S., Matsudaira Y., Sugihara Y. Masks for influenza patients: measurement of airflow from the mouth. Jpn. J. Infect. Dis. 2006;59(3):179–181. [PubMed] [Google Scholar]
- 24 Jacobs J.L., Ohde S., Takahashi O., et al. Use of surgical face masks to reduce the incidence of the common cold among health care workers in Japan: a randomized controlled trial. Am. J. Infect. Control. 2009;39:417–419. doi: 10.1016/j.ajic.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 16 Jefferson T., Del Mar C., Dooley L., et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2009;339:3675. doi: 10.1136/bmj.b3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson T., Del Mar C.B., Dooley L., et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst. Rev. 2011;(7) doi: 10.1002/14651858.CD006207.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45 Johnson D., Druce J.D., Birch C., et al. A quantitative assessment of the efficacy of surgical and N95 masks to filter influenza virus in patients with acute influenza infection Clin. Infect. Dis. 2009;49(2):275–277. doi: 10.1086/600041. [DOI] [PubMed] [Google Scholar]
- Ki H.K., Han S.K., Son J.S., et al. Risk of transmission via medical employees and importance of routine infection-prevention policy in a nosocomial outbreak of Middle East respiratory syndrome (MERS): a descriptive analysis from a tertiary care hospital in South Korea. BMC Pulm. Med. 2019;19:190. doi: 10.1186/s12890-019-0940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim T., Jung J., Kim S.M., et al. Transmission among healthcare worker contacts with a Middle East respiratory syndrome patient in a single Korean centre. Clin. Microbiol. Infect. 2015;22:e11–e13. doi: 10.1016/j.cmi.2015.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim C.J., Choi W.S., Jung Y., et al. Surveillance of the Middle East respiratory syndrome (MERS) coronavirus (CoV) infection in healthcare workers after contact with confirmed MERS patients: incidence and risk factors of MERS-CoV seropositivity. Clin. Microbiol. Infect. 2016;22:880–886. doi: 10.1016/j.cmi.2016.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82 Laosiritaworn Y. University of Pittsburgh, Graduate School of Public Health; 2014. Computational Modelling to Address the Burden of Influenza and Strategies of Control Measures in Thailand. (Thesis) [Google Scholar]
- Larson E.L., Ferng Y.-.H., Wong-McLoughlin J., et al. Impact of non-pharmaceutical interventions on URIs and influenza in crowded, urban households. Public Health Rep. 2010;125(2):178–191. doi: 10.1177/003335491012500206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T.F., Lau M., Kim J.H., et al. Probable secondary infections in households of SARS patients in Hong Kong. Emerg. Infect. Dis. 2004;10:235–243. doi: 10.3201/eid1002.030626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T.F., Kim J.H., Tsui H.Y., et al. Perceptions related to bird-to-human avian influenza, influenza vaccination, and use of face mask. Infection. 2008;36(5):434–443. doi: 10.1007/s15010-008-7277-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., et al. Role of ventilation in airborne trans- mission of infectious agents in the built environment: a multidisciplinary systematic review. Indoor Air. 2007;17:2–18. doi: 10.1111/j.1600-0668.2006.00445.x. [DOI] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang M., Gao L., Cheng C., et al. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu W., Tang F., Fang L.Q., et al. Risk factors for SARS infection among hospital healthcare workers in Beijing: a case control study. Trop. Med. Int. Health. 2009;14(suppl 1):52–59. doi: 10.1111/j.1365-3156.2009.02255.x. [DOI] [Google Scholar]
- Liu J., Liao X., Qian S., et al. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China. Emerg. Infect. Dis. 2020 doi: 10.3201/eid2606.200239. doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54 Liung N.H., Chu D.K., Shiu E.Y., et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat. Med. 2020:1–5. doi: 10.1038/s41591-020-0843-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb M., McGeer A., Henry B., et al. SARS among critical care nurses, Toronto. Emerg. Infect. Dis. 2004;10:251–255. doi: 10.3201/eid1002.030838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeb M., Dafoe N., Mahony J., et al. Surgical mask vs N95 respirator for preventing influenza among health care workers: a randomized trial. JAMA. 2009;302:1865–1871. doi: 10.1001/jama.2009.1466. [DOI] [PubMed] [Google Scholar]
- MacIntyre C.R., Chughtai A.A. A rapid systematic review of the efficacy of face masks and respirators against coronaviruses and other respiratory transmissible viruses for the community, healthcare workers and sick patients. Int. J. Nurs. Stud. 2020;108 doi: 10.1016/j.ijnurstu.2020.103629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61 MacIntyre C.R., Chungtai A.A. Facemasks for the prevention of infection in healthcare and community settings. BMJ. 2015:350. doi: 10.1136/bmj.h694. [DOI] [PubMed] [Google Scholar]
- 58 MacIntyre C.R., Wang Q., Cauchemez S., et al. A cluster randomized clinical trial comparing fit-tested and non-fit-tested N95 respirators to medical masks to prevent respiratory virus infection in health care workers. Influenza Other Respir. Viruses. 2011;5(3):170–179. doi: 10.1111/j.1750-2659.2011.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Wang Q., Seale H., et al. A randomized clinical trial of three options for N95 respirators and medical masks in health workers. Am. J. Respir. Crit. Care Med. 2013;187:960–966. doi: 10.1164/rccm.201207-1164OC. [DOI] [PubMed] [Google Scholar]
- MacIntyre C.R., Seale H., Dung T.C., et al. A cluster randomised trial of cloth masks compared with medical masks in healthcare workers. BMJ Open. 2015;5(4) doi: 10.1136/bmjopen-2014-006577. Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Zhang Y., Chughtai A.A., et al. Cluster randomised controlled trial to examine medical mask use as source control for people with respiratory illness. BMJ Open. 2016;6(12) doi: 10.1136/bmjopen-2016-012330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacIntyre C.R., Chughtai A.A., Rahman B., et al. The efficacy of medical masks and respirators against respiratory infection in healthcare workers. Influenza Other Respir. Viruses. 2017;11(6):511–517. doi: 10.1111/irv.12474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57 Maclntyre C.R., et al. Face mask use and control of respiratory virus transmission in households. Emerg. Infect. Dis. 2009;15:233–241. doi: 10.3201/eid1502.081167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20 Meleny F.L., Stevens F.A. Postoperative haemolytic streptococcus wound infections and their relation to haemolytic streptococcus carriers among the operating personel. Surg. Gynecol.Obstet. 1926;43:338–342. [Google Scholar]
- Milton D.K., Fabian M.P., Cowling B.J., et al. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog. 2013;9(3) doi: 10.1371/journal.ppat.1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P... Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2707599/pdf/pmed.1000097.pdf Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4 Nicas M., Nazaroff W.W., Hubbard A. Toward understanding the risk of secondary airborne infection: emission of respirable pathogens. J. Occup. Environ. Hyg. 2005;2:143–154. doi: 10.1080/15459620590918466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Offeddu V., Yung C.-.F., Low M.S.F., et al. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin. Infect. Dis. 2017;65:1934–1942. doi: 10.1093/cid/cix681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park B.J., Peck A.J., Kuehnert M.J., et al. Lack of SARS transmission among healthcare workers, United States. Emerg. Infect. Dis. 2004;10:244–248. doi: 10.3201/eid1002.030793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perski O., Simons D., West R., Michie S. Face masks to prevent community transmission of viral respiratory infections: a rapid evidence review using Bayesian analysis. Qeios. 2020 doi: 10.32388/1SC5L4. [DOI] [Google Scholar]
- Radonovich L.J., Jr., Simberkoff M.S., Bessesen M.T., et al. N95 respirators vs medical masks for preventing influenza among health care personnel: a randomized clinical trial. JAMA. 2019;322(9):824–833. doi: 10.1001/jama.2019.11645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21 Romney M.G. Surgical face masks in the operating theatre: re-examining the evidence. J. Hosp. Infect. 2001;47:251–256. doi: 10.1053/jhin.2000.0912. [DOI] [PubMed] [Google Scholar]
- 68 Ryu B., Cho Sung-Il, Oh Myoung-don, et al. Seroprevalence of Middle East respiratory syndrome coronavirus (MERS-CoV) in public health workers responding to a MERS outbreak in Seoul, Republic of Korea, in 2015. WPSAR. 2019;10(2) doi: 10.5365/wpsar.2018.9.3.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders-Hastings P., Crispo J.A.G., Sikora L., et al. Effectiveness of personal protective measures in reducing pandemic influenza transmission: a systematic review and meta-analysis. Epidemics. 2017;20:1–20. doi: 10.1016/j.epidem.2017.04.003. [DOI] [PubMed] [Google Scholar]
- Scales D.C., Green K., Chan A.K., et al. Illness in intensive care staff after brief exposure to severe acute respiratory syndrome. Emerg. Infect. Dis. 2003;9(10) doi: 10.3201/eid0910.030525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71 Seto W.H., Tsang D., Yung R.W.H., et al. Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS) Lancet. 2003;361:1519–1520. doi: 10.1016/s0140-6736(03)13168-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73 Simmerman J.M., Suntarattiwong P., Levy J., et al. Findings from a household randomized controlled trial of hand washing and face masks to reduce influenza transmission in Bangkok, Thailand. Influenza Other Respir. Viruses. 2011;5:256–267. doi: 10.1111/j.1750-2659.2011.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72 Smith J.D., MacDougall C.C., Johnstone J., et al. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ. 2016;188(8) doi: 10.1503/cmaj.150835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14 Strasser B.J., Schlich T. A history of the medical mask and the rise of throwaway culture. Lancet. 2020;396(10243):19–20. doi: 10.1016/S0140-6736(20)31207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74 Suess T., Remschmidt C., Schink S.B., et al. The role of facemasks and hand hygiene in the prevention of influenza transmission in households: results from a cluster randomised trial; Berlin, Germany, 2009-2011. BMC Infect. Dis. 2012;12:26. doi: 10.1186/1471-2334-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teleman M.D., Boudville I.C., Heng B.H., et al. Factors associated with transmission of severe acute respiratory syndrome among health-care workers in Singapore. Epidemiol. Infect. 2004;132:797–803. doi: 10.1017/s0950268804002766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuan P.A., Horby P., Dinh P.N., et al. SARS transmission in Vietnam outside of the health-care setting. Epidemiol. Infect. 2007;135:392–401. doi: 10.1017/S0950268806006996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Sande M., Teunis P., Sabel R. Pro- fessional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One. 2008;3:e2618. doi: 10.1371/journal.pone.0002618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Q., Huang, X., Bai, Y., et al. Epidemiological characteristics of COVID-19 in medical staff members of neurosurgery departments in Hubei province: a multicentre descriptive study. medRiv. 2020a. doi: 10.1101/2020.04.20.20064899. [DOI]
- Wang X., Pan Z., Cheng Z. Association between 2019-nCoV transmission and N95 respirator use. J. Hosp. Infect. 2020;105:104–105. doi: 10.1016/j.jhin.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 1 Wells W.F. On air-borne infection. Study II. Droplets and droplet nuclei. Am. J. Hyg. 1934;20:611–618. doi: 10.1093/oxfordjournals.aje.a118097. [DOI] [Google Scholar]
- Wilder-Smith A., Teleman M.D., Heng B.H., et al. Asymptomatic SARS coronavirus infection among healthcare workers, Singapore. Emerg. Infect. Dis. 2005;11:1142. doi: 10.3201/eid1107.041165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6 World Health Organization . World Health Organization; Geneva: 2014. Infection Prevention and Control of Epidemic- and Pandemic-Prone Acute Respiratory Infections in Health Care. [PubMed] [Google Scholar]
- World Health Organization. Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 [press release]. March 11, 2020.
- Wu J., Xu F., Zhou W., et al. Risk factors for SARS among persons without known contact with SARS patients, Beijing, China. Emerg. Infect. Dis. 2004;10:210–216. doi: 10.3201/eid1002.030730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao J., Shiu E.Y.C., Gao H., et al. Nonpharmaceutical measures for pandemic influenza in nonhealthcare settings – personal protective and environmental measures. Emerg. Infect. Dis. 2020;26(5):967–975. doi: 10.3201/eid2605.190995. [DOI] [PMC free article] [PubMed] [Google Scholar]