Abstract
While surveillance can identify changes in COVID-19 transmission patterns over time and space, sections of the population at risk, and the efficacy of public health measures, reported cases of COVID-19 are generally understood to only capture a subset of the actual number of cases. Our primary objective was to estimate the percentage of cases reported in the general community, considered as those that occurred outside of long-term care facilities (LTCFs), in specific provinces and Canada as a whole. We applied a methodology using the delay-adjusted case fatality ratio (CFR) to all cases and deaths, as well as those representing the general community. Our second objective was to assess whether the assumed CFR (mean = 1.38%) was appropriate for calculating underestimation of cases in Canada. Estimates were developed for the period from March 11th, 2020 to September 16th, 2020. Estimates of the percentage of cases reported (PrCR) and CFR varied spatially and temporally across Canada. For the majority of provinces, and for Canada as a whole, the PrCR increased through the early stages of the pandemic. The estimated PrCR in general community settings for all of Canada increased from 18.1% to 69.0% throughout the entire study period. Estimates were greater when considering only those data from outside of LTCFs. The estimated upper bound CFR in general community settings for all of Canada decreased from 9.07% on March 11th, 2020 to 2.00% on September 16th, 2020. Therefore, the true CFR in the general community in Canada was likely less than 2% on September 16th. According to our analysis, some provinces, such as Alberta, Manitoba, Newfoundland and Labrador, Nova Scotia, and Saskatchewan reported a greater percentage of cases as of September 16th, compared to British Columbia, Ontario, and Québec. This could be due to differences in testing rates and criteria, demographics, socioeconomic factors, race, and access to healthcare among the provinces. Further investigation into these factors could reveal differences among provinces that could partially explain the variation in estimates of PrCR and CFR identified in our study. The estimates provide context to the summative state of the pandemic in Canada, and can be improved as knowledge of COVID-19 reporting rates and disease characteristics are advanced.
Keywords: SARS-CoV-2, Underestimation, Coronavirus disease, Long term care facilities, Case fatality ratio
1. Introduction
Surveillance is critical to inform the global public health response to the Coronavirus disease (COVID-19) pandemic; COVID-19 is caused by infection with the SARS-CoV-2 virus. Surveillance can identify changes in COVID-19 transmission patterns over time and space, sections of the population at risk (Paquette et al., 2020), and the efficacy of public health measures (Lai et al., 2020). Disease underestimation (the combination of under-ascertainment and under-reporting) occurs when a surveillance system is unable to capture all the cases and deaths associated with a disease in a given population (Gibbons et al., 2014). All human infectious disease surveillance systems are burdened with some degree of underestimation (Gibbons et al., 2014). When underestimation associated with a surveillance system is constant over time and among sub-populations, trends can be detected and extrapolated to the entire population. When underestimation is not constant, trend and extrapolation analyses can be applied if inequalities are known or adjusted for (MacDougall et al., 2008; Majowicz et al., 2005).
Reported cases of COVID-19 are generally understood to only capture a subset of the actual number of cases. There are several reasons for this. Surveillance systems can only capture those cases that sought medical care (or at least sought testing), and received a diagnostic test that was determined to be “positive”, that was subsequently reported back to the surveillance system. Many cases of COVID-19 are mild in severity (Gandhi, Lynch, & del Rio, 2020; Wu & McGoogan, 2020), which reduces the likelihood that they would seek medical care and testing (Peppa et al., 2017). Policies that restrict who can be tested (to, for example, healthcare workers, or those that exhibit a specific set of symptoms) can also cause under-ascertainment of cases. Additionally, a low percentage of individuals with COVID-19 may falsely test negative in diagnostic tests (Kim, Hong, & Yoon, 2020).
Russell et al. (2020) developed a methodology to estimate the underestimation of COVID-19 using a delay-adjusted case fatality ratio (CFR) (Russell et al., 2020). A CFR is defined as the ratio of deaths to symptomatic cases over a specified time period. The authors assumed that if a country had a CFR greater than 1.38, the cause of the deviation was the result of underestimation. However, factors other than underestimation could result in deviations from this CFR, and some variables may affect both underestimation and CFR. For example, population age demographics, socio-economic factors, and regional variation in access or availability of medical care and/or testing can all play a role. Contact tracing and expansive testing policies can have a large effect on bridging the gap between detected cases and the true number of cases, particularly if cases are mild or asymptomatic.
In Canada, outbreaks of COVID-19 in long term care facilities (LTCFs) have contributed substantially to deaths due to COVID-19 (Comas-Herrera et al., 2020). As of September 8th, 2020, approximately 31% of reported COVID-19 cases and 79% of deaths have been linked to LTCFs (Health Portfolio Operations Centre Health Surveilance and Epidemiology Division, 2020). Residents of these facilities are typically elderly and are more likely to have comorbidities than the average Canadian, and thus are particularly susceptible to severe and fatal effects of SARS-CoV-2 infection (Comas-Herrera et al., 2020; Zhou et al., 2020). Also, the rate of transmission of COVID-19 within and among LTCFs was much higher than observed for the general population (Bigelow et al., 2020; Holroyd-Leduc & Laupacis, 2020), as has been observed in outbreaks of other respiratory infections (Childs et al., 2019). These factors result in both a relatively high case incidence and CFR in LTCF residents compared to the remainder of the population (herein referred to as the “general community” for simplicity), which has had a large influence on the average CFR observed in Canada.
In this study, the objective was to estimate the percentage of cases reported in the general community in Canada. To meet this objective, we used the analysis and CFR from Russell et al. (2020) and additionally excluded cases and deaths that occurred in LTCFs from the national and provincial COVID-19 data. The CFR associated with COVID-19 is highly uncertain, with substantial variation in reported estimates in the literature. Hence, our second objective was to assess whether the assumed CFR was appropriate for estimating the percentage of cases reported of cases in Canada.
2. Methods
We used the delay-adjusted CFR to estimate the percentage of cases reported over time, for each province, and at the national-level in Canada.
2.1. Data sources and modifications to estimate the number of cases and deaths in the general community
Daily provincial cumulative case and death counts were downloaded from the Government of Canada’s website (Government of Canada, 2020). Information regarding cumulative cases and deaths that occurred in LTCFs were collected from news articles and publicly available provincial data sources by a team of Canadian federal government epidemiologists and data scrapers (Health Portfolio Operations Centre Health Surveilance and Epidemiology Division, 2020). We extracted this information from daily reports produced since May 1st, 2020 and April 14th, 2020 for cases and deaths, respectively.
To estimate LTCF cases that occurred prior to May 1st, the number of cases reported in LTCFs on May 1st were divided by the total number of cases reported the same day, to derive province- and territory-specific ratios. These ratios were then multiplied by the respective daily cumulative number of reported cases to derive cumulative LTCF case estimates from March 11th through April 30th for each province and territory. This same approach was applied for deaths, but data reported on April 14th were used to derive the ratios.
In some instances, case and death counts were not reported on weekends and holidays. Linear interpolation was used to derive counts where no reported data were available.
Cumulative cases that occurred in LTCFs in Québec were not available in datasets collected by data scrapers at the Health Surveillance and Epidemiology Division in the Health Portfolio Operations Centre. Therefore, we divided the total number of deaths in LTCFs excluding Québec by the corresponding total number of cases to determine the crude CFR specific to LTCFs elsewhere in Canada, using the most recent data available (September 29th, 2020). The Québec LTCF death counts were then divided by the calculated crude CFR to generate time-series data for the daily cumulative cases in Québec LTCFs.
2.2. Estimating the number of cases and deaths in the general community
We subtracted the daily estimated cumulative cases and deaths in LTCFs from the corresponding totals reported for each province or territory and for Canada. This yielded adjusted estimates to approximate the number of cases and deaths in the general community.
2.3. Estimating the percentage of cases reported compared to the expected number of cases
To obtain estimates for the percentage of cases reported (PrCR) on each day (dayx), we used Eq. (1):
| (1) |
where CFL and CFR represent the case fatality lag and case fatality ratio, respectively.
We used a stochastic approach to incorporate uncertainty and variability associated with the CFR and CFL. The CFR was parameterized as a normal distribution with 5th and 95th percentiles of 1.23% and 1.53%, respectively, and a mean value of 1.38% (Verity et al., 2020).
The CFL represents the estimated number of days between a reported case resulting in a reported death (assuming the case was fatal). The CFL was represented as a lognormal distribution with a mean of 10 days and a standard deviation of 2 days (Imperial College COVID-19 response team, 2020).
The model incorporated daily cumulative data reported from March 11th, 2020 (the date Canada reported its 100th case) through September 29th, 2020. Results were generated for each province and territory, as well as for all of Canada. The model was run using both unadjusted cumulative counts (to develop raw estimates that include cases and deaths in LTCFs) and general community cumulative counts (to develop adjusted estimates that describe the general community setting, and exclude cases and deaths in LTCFs). Estimates were developed for the period from March 11th, 2020 to September 16th, 2020.
2.4. Estimating the case fatality ratio
To check that an assumed CFR of 1.38% is appropriate for calculating the percentage of cases reported in Canada, we obtained an estimate for the CFR for reported cases on a given day (dayx) using Eq. (2):
| (2) |
This provided an upper-bound estimate for CFR by assuming that PrCR = 100%. The CFL, study period, and geographic area were defined as above. These upper-bound CFRs were calculated using both unadjusted cumulative counts and general community cumulative counts.
2.5. Model implementation
The model was implemented in Microsoft Excel using the @Risk version 7.6 add-on (Palisade Corporation, New York, USA) to allow for Monte Carlo simulation using Latin Hypercube sampling, using a randomly selected static seed value. Results were obtained using 1000 iterations for each simulated day.
3. Results
The PrCR and CFR estimates were calculated for provinces and territories that had reported at least one death outside of LTCFs prior to September 16th. Therefore, estimates were not generated for the following provinces/territories: New Brunswick, Northwest Territories, Nunavut, Prince Edward Island, and the Yukon. The number of unadjusted and adjusted cumulative deaths reported in each province studied are provided in Table 1.
Table 1.
The number of cumulative deaths and cumulative deaths in the general community in each province included in this study, as well as the total in Canada, as of September 29th, 2020.
| Jurisdiction | Cumulative deaths | Cumulative deaths in the general community (excluding deaths in LTCFs) |
|---|---|---|
| Alberta | 266 | 96 |
| British Columbia | 234 | 68 |
| Manitoba | 20 | 12 |
| Newfoundland and Labrador | 3 | 3 |
| Nova Scotia | 65 | 8 |
| Ontario | 2844 | 799 |
| Québec | 5833 | 945 |
| Saskatchewan | 24 | 22 |
| Canada | 9291 | 1953 |
LTCFs: Long term care facilities.
3.1. Percentage of cases reported
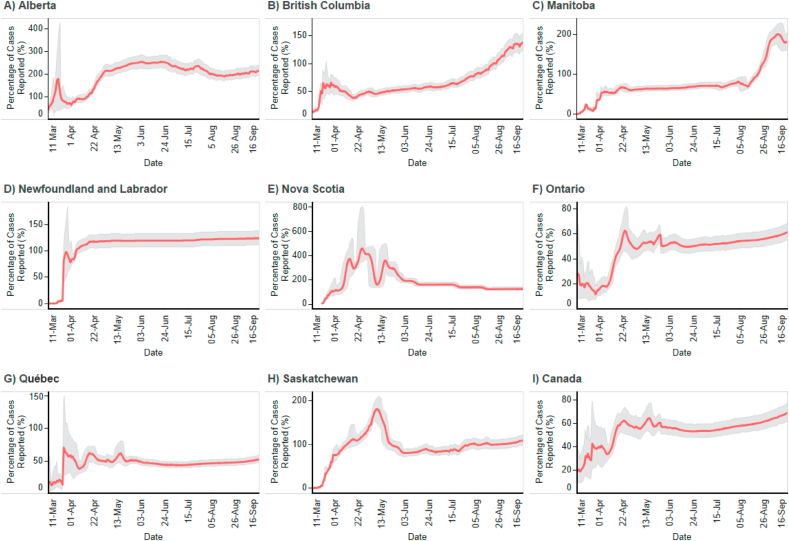
For the majority of provinces, and for Canada as a whole, the PrCR for the general community increased through the early stages of the pandemic (March through April; Fig. 1). Estimates were consistently greater than the estimates from the models unadjusted for LTCF cases and deaths (Supplementary Materials). For example, on September 16th, 2020, the general community and unadjusted models estimated a PrCR of 69.0% (90% CrI: 61.6%–76.7%), and 20.8% (90% CrI: 18.6%–23.1%), respectively, for all of Canada.
Fig. 1.
Estimates (mean and 90% credible interval band) for the percentage of cases reported in the general community (defined as all people in Canada that reside outside of long term care facilities) for eight provinces (A–H) and Canada (I) over time, assuming a mean case fatality ratio of 1.38%.
Unadjusted and adjusted PrCRs calculated as of September 16th, 2020 for each studied province are provided in Table 2. The estimated PrCR in general community settings for all of Canada increased from 18.1% to 69.0% throughout the entire study period. At varying stages of the pandemic, the model produced mean PrCR estimates for the general community greater than 100% for British Columbia, Alberta, Manitoba, Newfoundland and Labrador, Nova Scotia, and Saskatchewan (Fig. 1).
Table 2.
The estimated unadjusted and general community percentage of cases reported (PrCR) with 90% credible interval (CrI) for each studied province and Canada, as of September 16th, 2020.
| Jurisdiction | Unadjusted PrCR (90% CrI) | General community PrCR (90% CrI) |
|---|---|---|
| Alberta | 85.1 (75.9–94.5) | 215 (192–240) |
| British Columbia | 45.0 (40.2–50.0) | 138 (123–153) |
| Manitoba | 108 (95.2–121) | 182 (160–204) |
| Newfoundland and Labrador | 125 (111–138) | 124 (111–138) |
| Nova Scotia | 23.1 (20.5–25.6) | 125 (111–139) |
| Ontario | 22.1 (19.7–24.4) | 61.4 (54.8–68.2) |
| Québec | 15.6 (13.9–17.3) | 52.4 (46.7–58.2) |
| Saskatchewan | 101 (89.7–112) | 109 (97.5–122) |
| Canada | 20.8 (18.6–23.1) | 69.0 (61.6–76.7) |
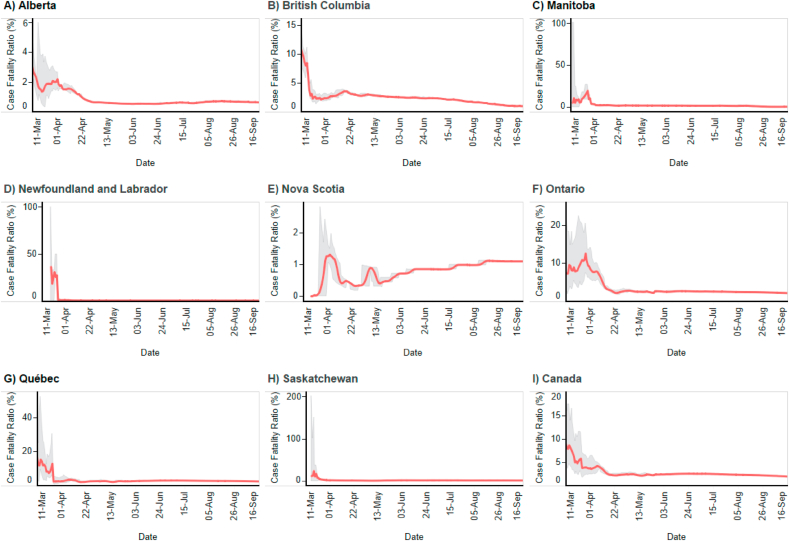
3.2. Case fatality ratio
Fig. 2 displays the model results for CFR using reported cases for each province and Canada as a whole. Given that Eq. (2) is a simple rearrangement of Eq. (1), the inverse trend is observed compared to Fig. 1.
Fig. 2.
Estimates (mean and 90% credible interval band) for the case fatality ratio in the general community (defined as all people in Canada that reside outside of long term care facilities) for eight provinces (A–H) and Canada (I) over time, assuming no underestimation (i.e., 100% reporting) of cases.
Unadjusted and adjusted CFRs calculated as of September 16th, 2020 for each studied province are provided in Table 3. These CFRs are the estimated maximum CFRs in the general community for each province and Canada. The lowest mean CFR in general community settings on September 16th, 2020 was 0.64% (90% CrI: 0.64%–0.65%), in Alberta. The highest mean CFR in general community settings on this date was 2.63% (90% CrI: 2.62%–2.65%), in Québec. The estimated CFR in general community settings for all of Canada decreased from 9.07% on March 11th, 2020 to 2.00% on September 16th, 2020. Therefore, the true CFR in the general community in Canada was likely <2.00% on September 16th according to this method. Distributions of CFR in all models reflected a wide range of credible intervals and fluctuated substantially in the first 30 days studied using the model. At later dates, the models typically stabilized and credible intervals narrowed considerably (Fig. 2).
Table 3.
The estimated unadjusted and general community case fatality ratio (CFR) with 90% credible interval (CrI) for each studied province and Canada assuming no underestimation, as of September 16th, 2020.
| Jurisdiction | Unadjusted CFR (90% CrI) | General community CFR (90% CrI) |
|---|---|---|
| Alberta | 1.62 (1.61–1.65) | 0.64 (0.64–0.65) |
| British Columbia | 3.07 (3.03–3.12) | 1.00 (0.97–1.01) |
| Manitoba | 1.28 (1.21–1.34) | 0.76 (0.75–0.82) |
| Newfoundland and Labrador | 1.11 (1.11–1.11) | 1.11 (1.11–1.11) |
| Nova Scotia | 5.99 (5.99–5.99) | 1.11 (1.11–1.11) |
| Ontario | 6.25 (6.25–6.27) | 2.25 (2.24–2.25) |
| Québec | 8.84 (8.82–8.86) | 2.63 (2.62–2.65) |
| Saskatchewan | 1.37 (1.37–1.37) | 1.26 (1.26–1.26) |
| Canada | 6.63 (6.62–6.65) | 2.00 (1.99–2.01) |
4. Discussion
4.1. Percentage of cases reported and case fatality ratios
Our unadjusted estimates for the PrCR for Canada are comparable to the estimates developed earlier in the pandemic by Russel et al. (2020) and Zhao (2020). Russel et al. (2020) estimated that on June 6th, 2020, Canada reported 26.1% (95% CrI: 20.8%–31.7%) of COVID-19 cases, compared to our unadjusted estimate of 16.0% (90% CrI: 14.2%–17.7%) on that same date (Supplementary Materials). The disparity is the result of different data sources used to inform the number of reported cases and deaths, as well as model parameterization of case fatality lag. For the former, Russell et al. (2020) used data from the European Centre for Disease Prevention and Control (2020), while we used the officially reported data from the Government of Canada (2020). Russell et al. (2020), used a mean value of 13 days for CFL whereas our model used a mean value of 10 days derived by the Imperial College COVID-19 response team (2020). Of the 140 countries included in the analysis by Russell et al. (2020) Canada had the 118th highest proportion of cases reported. If our unadjusted estimate had been used, Canada would have been ranked 135th out of the 140 countries assessed. However, after removing LTCF cases and deaths, our adjusted general community estimate of 56.2% (90% CrI: 50.0%–62.6%) for June 6th would have improved Canada’s ranking to be 68th of the 140 countries. The difference between our unadjusted and adjusted estimates highlights the impact that outbreaks in LTCFs had on Canada’s apparent CFR.
Estimates of PrCR and CFR varied spatially and temporally across Canada. The PrCR for the general population increased from March 11th through approximately mid-April for all provinces. This increase was likely the result of improved availability of testing, relaxing of criteria of who qualified for a test, contact tracing, changes in behaviour regarding seeking medical care/testing, or a combination of these. According to our analysis, some provinces, such as Alberta, Manitoba, Newfoundland and Labrador, Nova Scotia, and Saskatchewan reported a greater percentage of cases as of September 16th compared to other jurisdictions such as Ontario, and Québec. This could be due to differences in testing rates and criteria, and differences in the epidemics among the provinces. Mean PrCR estimates for the general community were sometimes greater than 100% for these provinces. In these instances, it is possible that the CFR in the study population was lower than the assumed mean of 1.38%.
Throughout the early stages of the COVID-19 pandemic, testing capacities and supplies were in limited supply across the globe. This is likely to have had an impact on the number of tests performed across Canada. Provinces that tested a greater proportion of the population might have been more likely to report a relatively greater number of cases, increasing the numerator in Eq. (1) and thereby the PrCR. If the estimated PrCR could be explained on the basis of per capita testing alone, one would expect that the ranking of PrCR and per capita testing would coincide. As of September 16th, 2020, per capita testing rates in the provinces reported on in our study here ranged from 6.92% to 22.6% (in Newfoundland and Labrador and Ontario, respectively) (Government of Canada, 2020), and the rankings do not correspond with estimated PrCRs. Therefore, the differences among estimated PrCRs are not fully explained by reported per capita testing rates. Inter- and intra-provincial differences among testing policies and criteria over time could account for this. Each province implemented distinct rules for test qualification at different dates throughout the pandemic. For example, some provinces implemented universal testing (i.e., testing anyone with symptoms) in early April, while others restricted testing to only individuals with a known exposure event or members of priority groups (e.g., healthcare workers) until mid May. A less restrictive testing policy would be expected to result in capture of a higher number of cases. In Alberta and Saskatchewan, asymptomatic testing has occurred since May, so the CFR estimated for these provinces may more likely approach the infection fatality rate (IFR). Community-transmission of COVID-19 has been greatly reduced in the Atlantic provinces since June, with many reported cases identified by routine screening of travellers, or associated with small outbreaks in which contacts would be tested whether or not they were asymptomatic. Therefore, the CFR is perhaps closer to the IFR in the Atlantic provinces.
It is also possible that the true CFR varies across Canadian jurisdictions, which would impact the estimates of PrCR. The observed CFR is in partially dependent on the underlying age-distribution of cases among provinces. Age has been found to be strongly linked with severity of COVID-19 cases, with old age associated with more severe outcomes including death (Onder et al., 2020), and higher CFRs (Botly et al., 2020). Available data provide evidence of differential age-distributions of people across the provinces and territories in Canada. As of September 10th, 2020, 8.0%, 12.5%, 20.4%, and 25.2% of reported COVID-19 cases were 70 years of age or older in Alberta, British Columbia, Ontario, and Québec, respectively (Alberta Health, 2020; BC Centre for Disease Control, 2020; Institut national de santé publique du Institut national de santé publiquedu Québec, 2020; Public Health Ontario, 2020). This ranking corresponds with the inverse relative ranking of PrCR for these four provinces (which constitute the majority of cases reported in Canada). However, these proportions include cases linked to LTCFs, and it is therefore possible that these differences do not reflect age-distributions of general community cases. The severity of illness (and therefore CFR and estimated PrCR) could be affected by other factors including socioeconomic factors, race, and access to healthcare (Galea & Abdalla, 2020; Lazzerini et al., 2020); the prevalence of these factors are expected to vary across provinces and territories. Further investigation into these factors could reveal differences among provinces that could partially explain the variation in estimates of PrCR identified in our study.
The CFR estimated for the general community in Canada was 2.00% (90% CrI: 1.99%–2.01%) on September 16th, 2020. Therefore, the true CFR in the general community in Canada was less than 2%, and an assumption of an overall CFR of 1.38% seems reasonable. The high CFR in the early months of the epidemic is consistent with estimates by others (Abdollahi et al., 2020; Zhao, 2020). The estimated CFR for the general community in Ontario in June is consistent with the overall 3.3% obtained from a subset of resolved cases (i.e., recovered or died) calculated from data on cases reported from January to June in Ontario by Papst et al. (2020).
4.2. Limitations
To adjust for the lack of available data in Québec for cases that occurred in LTCFs, we applied the CFR derived from case and death counts in LTCFs from all the other provinces/territories to retroactively calculate cases in Québec LTCFs. This could have resulted in under- and overestimated general community PrCRs and CFRs, respectively for this province. Additionally, the lack of LTCF data prior to May 1st, 2020 required us to estimate this missing data. Due to this, the results of our model prior to May 1st, 2020 should be interpreted with caution.
Estimates for both PrCR and CFR were based on the assumption that deaths from COVID-19 were always reported (i.e., no underestimation). While we expect that the majority of causes for underestimation previously described are less likely to impact fatality reports, it is possible that on rare occasions a COVID-19 death was unreported. An unreported death would have a minimal impact on our estimates in jurisdictions with numerous deaths attributed to COVID-19. However, the impact would be substantial in provinces that have reported very few deaths such as Manitoba, Newfoundland and Labrador, and Saskatchewan. Conversely, it was also assumed that the impact of incorrect attribution of COVID-19 to cause of death was negligible.
An additional limitation of this study was the limited availability of data to characterize the two parameters used in our models, CFR and CFL. Many studies have attempted to determine the CFR of COVID-19, but there is substantial variation in the findings of these studies for many reasons (Rajgor et al., 2020). In this study, we used a distribution around the mean estimate of 1.38% that was developed by Verity et al. (2020). This estimate incorporated adjustments for demography and under-ascertainment, which are factors that can influence CFR. Given that our analysis excluded cases and deaths linked to LTCFs, it was deemed also appropriate to select a CFR estimate that is on lower end of the range of estimates reported in the literature. This approach was supported by our finding that in some jurisdictions the estimated mean PrCR exceeded 100%, which indicated that the true CFR was even lower than 1.38%. We also assumed a CFL following a lognormal distribution of 10 ± 2 days, as in Imperial College COVID-19 response team (2020). This is lower than the mean value of 13.59 ± 2 days used in another Canadian study (Abdollahi et al., 2020). Our model was rerun using this longer CFL and there were no appreciable differences in the model outputs. A comprehensive Canadian retrospective study is required to reduce the uncertainty in this parameter for future modelling studies.
While our model is structured to estimate either PrCR or CFR, the accuracy of the absolute estimates for one variable are dependent on the quality of data for the other. If better information become available about CFR, then confidence in the absolute estimates of PrCR is improved, and vice versa. In the near-term, is more likely that the CFR can be better informed through province- and territory-specific observational studies. Nevertheless, the current estimates can provide essential information on the relative differences across Canada with respect to the percentage of cases reported and CFRs.
5. Conclusion
The methodology used in this paper uses cumulative case and death data, having excluded cases and deaths that occurred in LTCFs, to develop estimates that aim to describe either the PrCR or CFR of a jurisdiction over time. The estimates are therefore helpful to provide context to the summative state of the pandemic in Canada, and can be improved as knowledge of COVID-19 reporting rates and disease characteristics are advanced. Exploring methods to understand the magnitude of the true number of cases of COVID-19 in the general community is critical to developing appropriate interventions. Identification of differences within Canada regarding the percentage of cases reported and case-fatality ratios, when combined with knowledge of differing existing interventions, provides important information for decision-making.
Authors’ statement
BD- Conceptualization, Methodology, Formal Analysis, Data curation, Writing – Original draft, Writing – Review & Editing, Visualization. BAS- Methodology, Writing – Review & Editing. CC- Writing – Review & Editing. NHO- Writing – Review & Editing.
Funding
This work was funded by the Public Health Agency of Canada.
Declaration of competing interest
None to report.
Handling editor: Dr. J Wu
Footnotes
Peer review under responsibility of KeAi Communications Co., Ltd.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.idm.2020.11.008.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- Abdollahi E., Champredon D., Langley J.M., Galvani A.P., Moghadas S.M. CMAJ; 2020. Temporal estimates of case-fatality rate for COVID-19 outbreaks in Canada and the United States. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberta Health COVID-19 Alberta statistics: Interactive aggregate data on COVID-19 cases in Alberta. 2020. https://www.alberta.ca/stats/covid-19-alberta-statistics.htm Retrieved from.
- BC Centre for Disease Control British Columbia COVID-19 dashboard. 2020. https://experience.arcgis.com/experience/a6f23959a8b14bfa989e3cda29297ded Retrieved from.
- Bigelow B.F., Tang O., Barshick B., Peters M., Sisson S.D., Peairs K.S., Katz M.J. Outcomes of universal COVID-19 testing following detection of incident cases in 11 long-term care facilities. JAMA Internal Medicine. 2020 doi: 10.1001/jamainternmed.2020.3738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Botly L.C.P., Martin-Rhee M., Kasiban A., Swartz R.H., Mulvagh S.L., Lindsay M.P., Goia C., Smith E.E., Hill M.D., Field T.S., Krahn A.D., Oudit G.Y., Zieroth S., Yip C.Y.Y. COVID-19 Pandemic: Global Impact and Potential Implications for Cardiovascular Disease in Canada. CJC Open. 2020, Jul;2(4):265–272. doi: 10.1016/j.cjco.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs A., Zullo A.R., Joyce N.R., McConeghy K.W., van Aalst R., Moyo P., Bosco E., Mor V., Gravenstein S. The burden of respiratory infections among older adults in long-term care: a systematic review. BMC Geriatr. 2019;19(1):210. doi: 10.1186/s12877-019-1236-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comas-Herrera A., Zalakaín J., Litwin C., Hsu A.T., Lane N., Fernández J.-L. LTCcovid. org, International Long-Term Care Policy Network; 2020. Mortality associated with COVID-19 outbreaks in care homes: Early international evidence. [Google Scholar]
- European Centre for Disease Prevention and Control Daily number of new reported cases of COVID-19 by country worldwide. 2020. https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide Retrieved from.
- Galea S., Abdalla S.M. COVID-19 pandemic, unemployment, and civil unrest: Underlying deep racial and socioeconomic divides. Jama. 2020;324(3):227–228. doi: 10.1001/jama.2020.11132. [DOI] [PubMed] [Google Scholar]
- Gandhi R.T., Lynch J.B., del Rio C. Mild or moderate COVID-19. New England Journal of Medicine. 2020;383(18):1757–1766. doi: 10.1056/NEJMcp2009249. [DOI] [PubMed] [Google Scholar]
- Gibbons C.L., Mangen M.J., Plass D., Havelaar A.H., Brooke R.J., Kramarz P., Peterson K.L., Stuurman A.L., Cassini A., Fèvre E.M., Kretzschmar M.E. Measuring underreporting and under-ascertainment in infectious disease datasets: a comparison of methods. BMC public health. 2014, Feb 11;14:147. doi: 10.1186/1471-2458-14-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada Interactive data visualizations of COVID-19. 2020. https://health-infobase.canada.ca/covid-19/ Retrieved from.
- Health Portfolio Operations Centre Health Surveilance and Epidemiology Division . 2020. Rapid Web Scan: Estimated Deaths in LTC (residents and staff) based on press clippings. press conferences, and PT websites. [Google Scholar]
- Holroyd-Leduc J.M., Laupacis A. Continuing care and COVID-19: A Canadian tragedy that must not be allowed to happen again. Can Med Assoc. 2020;192(23):E632–E633. doi: 10.1503/cmaj.201017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imperial College COVID-19 response team . Imperial College London; 2020. Short-term forecasts of COVID-19 deaths in multiple countries.https://mrc-ide.github.io/covid19-short-term-forecasts/index.html [Google Scholar]
- Institut national de santé publique du Québec COVID-19 data in Quebec: Breakdown of confirmed cases by age group. 2020. https://www.inspq.qc.ca/covid-19/donnees Retrieved from.
- Kim H., Hong H., Yoon S.H. Diagnostic performance of CT and reverse transcriptase-polymerase chain reaction for coronavirus disease 2019: A meta-analysis. Radiology. 2020;296(3):E145–E155. doi: 10.1148/radiol.2020201343. 201343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai S., Ruktanonchai N.W., Zhou L., Prosper O., Luo W., Floyd J.R., Wesolowski A., Santillana M., Zhang C., Du X., Yu H., Tatem A.J. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–413. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. The Lancet Child & Adolescent Health. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDougall L., Majowicz S., Dore K., Flint J., Thomas K., Kovacs S., Sockett P. Under-reporting of infectious gastrointestinal illness in British Columbia, Canada: Who is counted in provincial communicable disease statistics? Epidemiology and Infection. 2008;136(2):248–256. doi: 10.1017/S0950268807008461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majowicz S.E., Edge V.L., Fazil A., McNab W.B., Doré K.A., Sockett P.N., Flint J.A., Middleton D., McEwen S.A., Wilson J.B. Estimating the under-reporting rate for infectious gastrointestinal illness in Ontario. Can J Public Health. 2005, May-Jun;96(3):178–181. doi: 10.1007/bf03403685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama. 2020;323(18):1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- Papst I., Li M., Champredon D., Bolker B.M., Dushoff J., Earn D.J. Canada. medRxiv; 2020. Age-dependence of healthcare interventions for SARS-CoV-2 infection in Ontario. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paquette D., Bell C., Roy M., Whitmore L., Currie A., Archibald C., MacDonald D., Pennock J. Laboratory-confirmed COVID-19 in children and youth in Canada, January 15-April 27, 2020. Can Commun Dis Rep. 2020, May 7;46(5):121–124. doi: 10.14745/ccdr.v46i06a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peppa M., Edmunds W.J., Funk S. Disease severity determines health-seeking behaviour amongst individuals with influenza-like illness in an internet-based cohort. BMC Infectious Diseases. 2017;17(1):238. doi: 10.1186/s12879-017-2337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public Health Ontario Ontario COVID-19 data tool: Counts of COVID-19 cases by age group in Ontario. 2020. https://www.publichealthontario.ca/en/data-and-analysis/infectious-disease/covid-19-data-surveillance/covid-19-data-tool Retrieved from.
- Rajgor D.D., Lee M.H., Archuleta S., Bagdasarian N., Quek S.C. The many estimates of the COVID-19 case fatality rate. The Lancet Infectious Diseases. 2020;20(7):776–777. doi: 10.1016/S1473-3099(20)30244-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell T.W., Hellewell J., Abbott S., Jarvis C., van Zandvoort K., Jarvis C.I., Gibbs H., Liu Y., Eggo R.M., Edmunds W.J., Kucharski A.J. Using a delay-adjusted case fatality ratio to estimate under-reporting. BMC Med. 2020, Oct 22;18(1):332. doi: 10.1186/s12916-020-01790-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verity R., Okell L.C., Dorigatti I., Winskill P., Whittaker C., Imai N., Cuomo-Dannenburg G., Thompson H., Walker P.G.T., Fu H., Dighe A., Griffin J.T, Baguelin M., Bhatia S., Boonyasiri A., Cori A., Cucunubá Z., FitzJohn R., Gaythorpe K. Estimates of the severity of coronavirus disease 2019: A model-based analysis. The Lancet Infectious Diseases. 2020, Jun;20(6):669–677. doi: 10.1016/s1473-3099(20)30243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese center for disease Control and prevention. Jama. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- Zhao S. A simple approach to estimate the instantaneous case fatality ratio: Using the publicly available COVID-19 surveillance data in Canada as an example. Infectious Disease Modelling. 2020;5:575–579. doi: 10.1016/j.idm.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/s0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.