Abstract
Background/aim
We try to investigate the association between patterns of imaging findings in patients who had a diagnosis of subchondral fracture around the knee, formerly known as SONK and their clinical outcome.
Materials and methods
We retrospectively identified 43 knees of 37 patients (28 males, 15 females) who had diagnosis of subchondral fractures around the knee. The mean age is 56-year-old (range 17–83). Musculoskeletal fellowship trained radiologist evaluated all 43 knee MRI in: 1)location of marrow edema 2)peri-osseous edema; 3) subchondral fracture line; 4) subchondral articular surface contour; 5)meniscal tear and extrusion; 6)adjacent soft tissue edema; 7) joint effusion. Independent clinical chart review was performed for clinical outcome with follow up time average of 13.3 months (range 0–88 months). Bad outcome was defined as worsening on imaging, continued complaint with surgical management and knee replacement or another episode of SONK. Chi-square analysis and Student's T tests were conducted to test the statistical significance of association between MR findings and outcomes. Statistical significance was set at p = 0.05 level.
Results
Of 43 knees, 6 patients had another episodes of SONK (14%), 11 patients were not improving or needed injection vs arthroscopy (26%), 4 patients required arthroplasty (9%), 22 patients had no negative outcome (51%). Gender, age, diabetic status, and location of the subchondral fracture show no influence on outcome. Worse outcome group had a significantly higher average BMI (31.7 vs. 28.0, P = 0.02). Positive change of subchondral articular surface contour is the only imaging finding with positive association with worse outcome (80% vs. 39.9%, P = 0.02). Presence of positive findings of above 3), 4), 5) and 6) had higher percentage of bad outcome (77.8%) compared to those with less positive findings (47.2%).
Conclusion
MR imaging findings may help at identifying SONK patient with potential risk of developing bad outcome.
Keywords: SONK, Insufficiency fracture, Avascular necrosis, MRI
1. Introduction
Spontaneous osteonecrosis of the knee (SONK) is a disorder first described in the literature by Ahlback in 1968 as a sudden onset of knee pain predominantly seen in middle aged or elderly female population.1 Although the etiology of SONK is still not fully understood, Yamamoto et has suggested that osteoporosis will result in subchondral insufficiency fractures, that will ultimately lead to osteonecrosis, corresponding to the series of histopathological finding, separating this entity from avascular necrosis, which appears to be a secondary cause rather than the primary inciting element.1, 2, 3, 4, 5, 6, 7 Patients usually present with acute knee pain, without history of trauma. The pain is accentuated with weight bearing, and if left untreated subchondral collapse will ensue, followed by secondary OA and immanent knee replacement.4,5
Although radiographs are used for the initial evaluation of SONK cases, it is usually normal in the acute phase. Nevertheless, with the progression of the disease, lesions can become conspicuous, manifested as radiolucent areas with sclerotic halo and subtle flattening of the articular surface. In advanced cases, subchondral collapse and secondary osteoarthritis can ensue.8,9 The Koshino grading system was the first to be implemented about this entity, in 1979. Based on the integrated clinical and radiographic findings, it consists of four stages: Stage 1: Symptomatic patients with normal radiographs. Stage 2: The presence of flattening of the bone and subchondral cysts with sclerotic margins. Stage 3: Resultant subchondral collapse and progression of the subchondral cysts. Stage 4: Development of osteoarthritis.8
On the other hand, as suggested by Aglietti et al. MR imaging is rendered higher in sensitivity than radiographs, offering high contrast resolution. The bone marrow edema is apparent on MRI within 48 h from the onset of the disease.9, 10, 11 Serpiginous subchondral low signal intensity band with intense surrounding bone marrow edema are the correspondence of the radiolucent areas with sclerotic halo seen on the radiographs. Similar to radiographs, subchondral collapse, resultant osteonecrosis, and saucerized defect of articular surface are the features of progressive disease.10,12,13 Despite the fact that MR imaging has been regarded as the superlative modality for early diagnosis, there has been limited data in the literature exploring useful imaging characteristics for outcome prediction.14, 15, 16 Although, the size of the lesions on T2 weighted images (T2WI) is the recognized predictor of outcome, its accuracy is abated by several other pathologies, compelling further research in this area.
The prognosis of SONK can vary from complete recovery with conservative management to bone destruction requiring arthroplasty, rendering early diagnosis imperative.11 The size of the lesions appear to play a major role, thus lesions more than 5 cm2 on radiographs are considered as a poor prognostic sign and require surgical intervention as they are prone to condylar collapse, whereas lesions less than 3.5 cm are usually managed conservatively with non-steroidal anti-inflammatory drugs, analgesics, bisphosphonates and protected weight bearing.8,12 A cohort study of 40 patients of SONK, suggested that patients who had lesions greater than 40% of the affected femoral condyle on radiographs, tend to require a knee prosthesis, whereas none of patients whose lesion was less than 20% of the condyle, required surgery.13
Beside the lesions size and the percentage of bone involvement, surgical intervention is reserved for patients who failed the conservative treatment over the period of 3 months.8 Surgical options include: 1) Joint-preserving surgical techniques i.e. arthroscopic meniscal tear repairs, core decompression, and osteochondral autograft. 2) Joint arthroplasty.8 However, patients who have progressed to subchondral collapse may benefit more from osteochondral autograft as it aids in the restoration of the cartilage surface. While, osteochondral autografting is rendered useful in cases of subchondral collapse, high tibial osteotomy is preferred for the younger population as well as the uni-compartmental knee arthroplasty (UKA) for cases of uni-compartment osteoarthritis. Totally knee arthroplasty is reserved as the last resort when all methods have failed or in cases of multi-compartmental extensive disease.8
The purpose of this study is to investigate the relationship between the MRI patterns and clinical outcome of patients with subchondral fracture. The potential of MR Imaging at helping to gauge the risk of clinical progression in patients with SONK is valuable. Careful and close follow up with more aggressive treatment can help certain groups of patients to minimize their risk.
2. Material and method
This retrospective study was approved by the institutional review board approval. Written informed consent was waived owing to the retrospective nature of the study.
2.1. Study subjects
We retrospectively investigated subjects diagnosed with subchondral fractures from January 1, 2009 to August 20, 2014. The definition of subchondral fracture was bone marrow edema in the subchondral area around the knee regardless of the presence of a fracture line on knee MRI in a patient presented clinically with sudden onset of pain without a major trauma. Additional demographic information including age, gender, body mass index (BMI), and co-morbidity such as diabetic status was recorded. BMI was calculated by dividing the weight in kilograms by the height squared in meters (kg/m2).
2.2. MR imaging protocol
MR imaging were obtained at our institution on either 1.5T or 3T units. All MRI studies included the following sequences: Axial proton density (PD) with fat suppression (FS), coronal proton density with fat suppression, sagittal proton density, and sagittal T2 with fat suppression.
2.3. Image interpretation
Images were reviewed by a fellowship trained musculoskeletal radiologist with 6 years of experiences. The following MR features were evaluated: 1/location of marrow edema; 2/peri-osseous edema; 3/subchondral fracture line; 4/Subchondral articular surface contour; 5/meniscal tear and extrusion; 6/adjacent soft tissue edema and 7/joint effusion.
Peri-osseous edema was defined as a high signal intensity along the peri-osseous area on fluid sensitive sequences, while subchondral fracture line was considered to be present if there was a low signal intensity band in the subarticular area on any sequence. In addition, irregularity of the articular surface on any sequence was un articular surface contour irregularity. Meniscal extension beyond the tibial margin was regarded as an extrusion. High signal in soft tissues surrounding the knee and the presence of joint effusion were also evaluated. We classified the location of bone marrow edema (BME) to four anatomical sites (lateral and medial femoral condyles and medial and lateral tibial condyles) based on the most noted locations of the edema. We subsequently, investigated if the number of the involved areas in bone marrow edema had a significant impact on the clinical outcome (1 BME vs. ≥2 BME).
2.4. Clinical outcome
Clinical outcomes of all subjects were reviewed using their medical record independently. And the average follow-up time is about 13.3 months (range 0–88 months). The following scenarios were regarded as an unfavorable outcome: 1) Worsening pain or radiological progression of disease on subsequent imaging studies despite conservative treatment 2) Knee replacement 3) Development of a new subchondral fracture.
2.5. Statistical analysis
To test the statistical significance of the association with the outcomes. Student t-test was conducted for numerical variables and chi-square analysis was used for the MR imaging findings. We have set P value of less than 0.05 to be statistically significant.
3. Results
Our study included 43 knee MR exams from 37 patients. Of the 37 patients, 22 were males while 15 were females, with an average of 56 years for age (range: 17–83 years). Of the 43 knees, 51.6% (22 of 43) had no negative outcome. As to the remaining 48.4% (21 of 43), 6 patients (14%) had another episode of subchondral fracture during the follow up period; 11 patients (26%) did not improve symptom wise or needed treatment in the form of steroid injection vs. arthroscopy, while 4 patients (9%) underwent total knee arthroplasty during the follow up period. These studies were labeled as with an unfavorable outcome.
Demographic summary of the studies and including the statistical differences between these two groups are shown in (Table 1). BMI was significantly higher in the group of unfavorable outcomes in comparison to the group with no negative outcome (28.0 vs 31.7, p = 0.02). Except for BMI, no other statistically significant demographic features were found.
Table 1.
Demographic summary of the studies and the statistical differences between the two groups.
| No Negative outcome (22) | Unfavorable outcome (21) | p value | |
|---|---|---|---|
| Age | 57.2 (±12.8) | 55.4 (±2.74) | 0.62 |
| Female | 8 (36.4%) | 7 (33.3%) | 0.84 |
| BMI (kg/m2) | 28.0 (±4.5) | 31.7 (±5.7) | 0.02 |
| Diabetes | 4 (18.2%) | 3 (14.3%) | 0.73 |
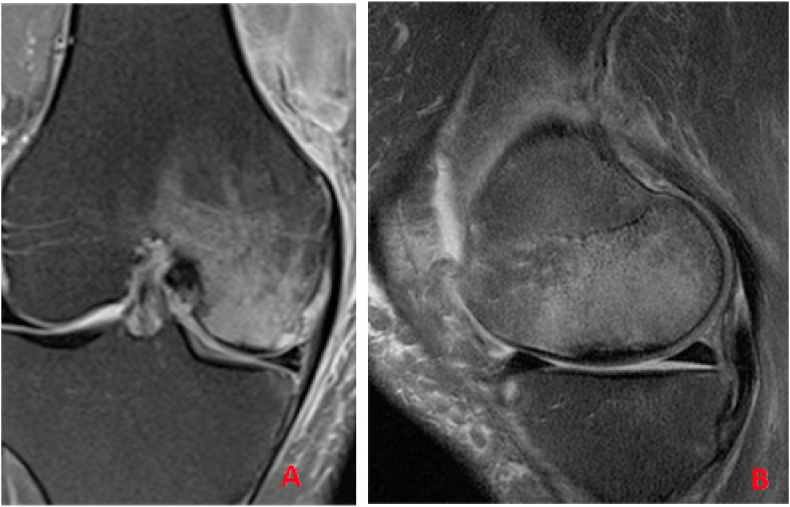
Of MR imaging features, all subjects had periosseous edema adjacent to the fractures site (Fig. 1, Fig. 2). BME was present at one site in 34 studies, while in 9 studies, it was involving two sites, of which 52.9% and 33.3%, progressed to have an unfavorable outcome respectively, delineating no significant difference between them (p = 0.30).
Fig. 1.
Coronal and Sagittal STIR images of the right knee showing extensive marrow edema, involving the medial condyle, and extending into the intercondylar region.
Fig. 2.
Coronal STIR image of the right knee, showing subchondral fracture of medial femoral condyle with extensive marrow edema of the medial femoral condyle and marrow edema around medial tibia.
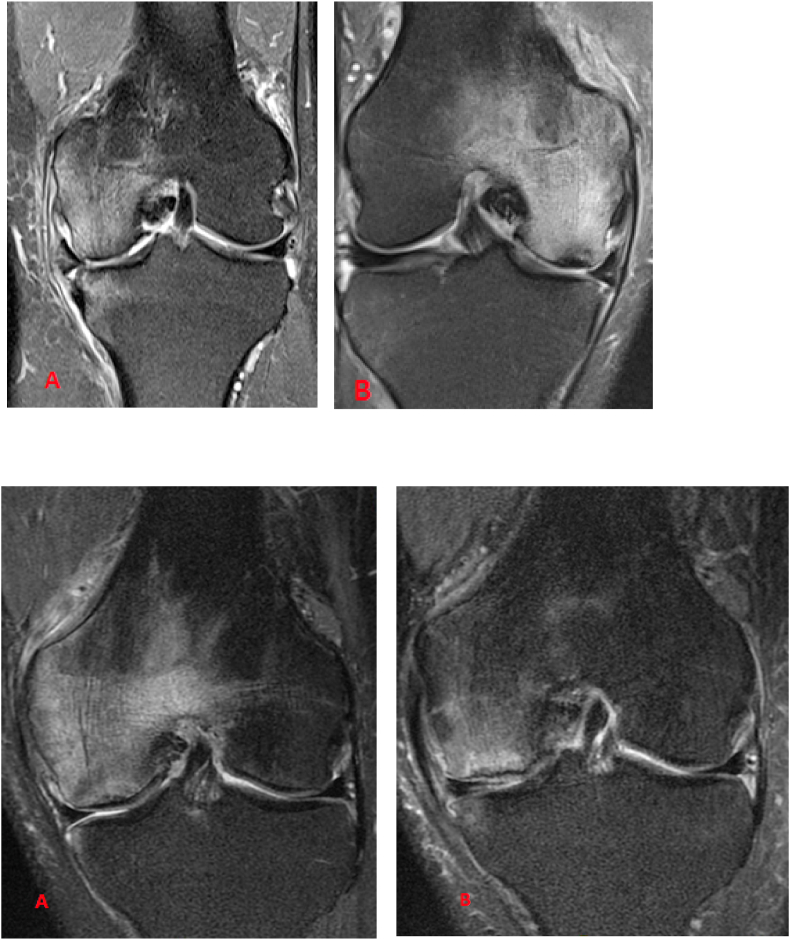
Only subarticular contour irregularity had a positive association with the unfavorable outcome (39.4% vs 80.0%, p = 0.02) (Fig. 3). No other MRI findings were found to have significant differences between the two groups (Table 2).
Fig. 3.
The change of the subchondral articular surface contour was the only imaging finding in isolation associated with poor outcome.
Table 2.
Summary of the MRI findings in both groups.
| MRI findings | negative | positive | p value |
|---|---|---|---|
| subchondral low signal band | 37.5 (3/8) | 51.4 (18/35) | 0.48 |
| subchondral articular contour irregularity | 39.4 (13/33) | 80.0 (8/10) | 0.02 |
| meniscal tear/extrusion | 42.9 (6/14) | 51.7 (15/29) | 0.59 |
| soft tissue edema | 57.1 (4/7) | 47.2 (17/36) | 0.63 |
| joint effusion | 42.1 (8/19) | 54.2 (13/24) | 0.43 |
| ≥2 bone marrow edema | 52.9 (18/34) | 33.3 (3/9) | 0.3 |
Numbers represent unfavorable outcome percentage of each MR imaging findings.
Numbers in parenthesis indicate actual number of cases.
Upon combining the four MR imaging findings: subchondral low signal intensity band (fracture line), subchondral articular contour irregularity, meniscal tear and soft tissue edema in one knee, a higher percentage of poor outcome has resulted; (77.8%) compared to those with less positive findings (47.2%) (Fig. 4).
Fig. 4.
Power of Combination of MR findings at predicating outcome: Subchondral fracture line, Subchondral articular surface contour change, meniscal tear/extrusion, Soft tissue edema.
4. Discussion
In our study, we have found that when we combine multiple key MR features of subchondral fracture, change of subchondral articular surface contour, presence of meniscal tear/extrusion and adjacent soft tissue edema (Fig. 1, Fig. 2), there is higher percentage of unfavorable outcomes (77.8%), compared to those with less positive findings (47.2%). A higher BMI was another significant negative prognostic factor.
In the literature, approximately 80% of SONK patients recover clinically with conservative treatment, while some require surgical interventions.11 In our study 16.3% (7 of 43 knees) had total knee arthroplasty.
Subchondral insufficiency fracture has been recognized as an early pathological finding along with marrow edema that can result in osteonecrosis due to the ischemia. Histological evidence of fractures and new bone formation within the lesion implies that osteonecrosis does not seem to be the cause of the disease.2,17 This theory makes it easier to understand the reason why prognosis of SONK can be diverse, differentiating it from avascular necrosis which usually mandates surgical intervention.
On radiograph, the lesion's size correlates negatively with clinical outcome based on literature.8 However, radiograph has much low sensitivity of diagnosing SONK compared to MRI. Though, a recent article on use of tomosynthesis, has suggested a perilesional disorganized trabecular texture, to be associated with arthroplasty.17 Varus deformity was also reported as a poor prognostic factor.11
On the other hand, although MRI is widely used and recognized as useful tool for early diagnosis for SONK, there is relatively limited reported data on imaging findings relationship with clinical outcome.14, 15, 16 Lecouvet et al. reported that thick low signal intensity in subchondral area on T2 weighted image and focal epiphyseal contour depression were related to early irreversible osteonecrosis outcome.14 In another article evaluating 19 cases of transient recovery of SONK, Yates et al. found only 1 case to have focal epiphyseal contour depression and concluded absence of epiphyseal contour depression to be an indicator for benign prognosis.15 Both articles were consistent with our results that subchondral articular contour irregularity on MRI to be significantly associated with unfavorable outcome (Fig. 5, Fig. 6).
Fig. 5.
Examples of radiological progression of the disease. Theme 1: A new episode of SONK. Coronal STIR images showing: (A) Left knee medial femoral condyle subchondral fracture on 9/20/2013. (B) Right knee medial femoral condyle subchondral fracture on 5/21/2015. Theme 2: Worsening symptoms. Coronal STIR images showing: (A) Left knee medial femoral condyle subchondral fracture on November 7, 2011. (B) Left knee medial femoral condyle decreasing edema but worsening subchondral collapse and worsening osteoarthritis on September 3, 2012.
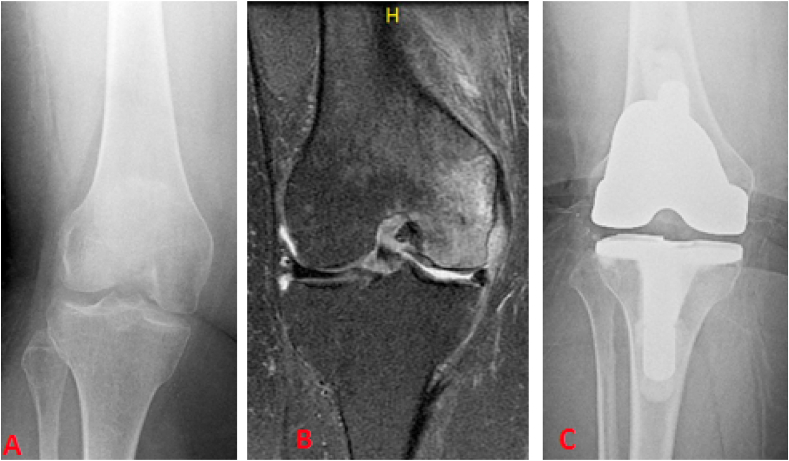
Fig. 6.
(A) A right knee radiograph on 12/18/2012. (B) Coronal STIR image of the right knee showing medial femoral condyle subchondral fracture on 12/20/2012. (C) A right knee radiograph on 2/25/2013, post total knee replacement due to continued pain.
In relatable studies involving the femoral head, articular surface collapse was considered as predictor for subchondral insufficiency fracture of the femoral head.18, 19, 20 Iwasaki et al. reported that all patients with a collapsed articular surface needed surgery18, while 50% of patients with less than 2 mm collapse to required surgical intervention as well.19 Hackney et al. has considered fracture morphology i.e. surface irregularity as a prognostic factor; thus loss of femoral head sphericity represents increased collapse and instability, leading to disease progression.19, 20 This could be applied to the knee joint and support our results. Loss of congruity of joint surface increase mechanical stresses at the site and may result in further collapse. Compared to radiographs, MRI is superior for morphological, 3-dimensional assessment of the articular contour of the knee joint, rendering it a better tool for outcome predictor for SONK cases.
Subchondral low signal intensity band has been regarded as a fracture line, though this is not required for diagnosis of subchondral fracture. In our study, the presence or absence of a fracture line had no major impact on prognosis. Also, the relationship between meniscal tear and SONK was well reported but the effect on prognosis has not been well understood. A recent study suggested over 95% of patients who suffer from SONK had coexisting meniscal tear,21 especially of large radial and root tears.4 However, our study showed that just the presence of a meniscal tear or extrusion was not statistically significant factor in predicting clinical outcome. In the literature, soft tissue edema has been suggested to play a vital role for early diagnosis, such as edema abutting the vastus lateralis often seen with subchondral fracture of lateral femoral condyle.22 In our study, soft tissue edema was common (83.7%) yet with no significant influence on clinical outcome, like joint effusion. This is similar in subchondral insufficiency fractures of the femoral head, where joint effusion and synovitis were common, but proved to have no significant impact on the clinical outcome in the literature.20 BME in the knee had no significant association with clinical outcome either, concurring to the findings in the literature, which also stated that the size of BME does not affect the outcome.11,14 Similarly, gender appeared to have no impact on clinical outcome, despite the fact that, SONK was initially reported to be more common in females, coinciding with the data in recent literature.22 Conversely, BMI was inversely associated with unfavorable outcome in our study, contradicting with an article stating that there is no significant differences of BMI between the groups that required conservative therapy versus intervention, however, the number of subjects included in the study was small [i.e.10 in each group].16
Based on the findings, it is evident that it is crucial to combine all the prognostic factors, in order to decide upon a precise prognosis.
In general, our study had several limitations; it is a retrospective study; the follow-up duration was not constant, and the number of subjects was relatively small.
5. Conclusion
In conclusion, subchondral articular contour irregularity on MR imaging was found to be significantly related to unfavorable outcome of subchondral fractures around the knee. And combination of several key MR features of subchondral fracture around the knee also lead to unfavorable clinical outcome. Thus, careful imaging evaluation can help a certain group of patients to minimize their risk.
Funding
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Declaration of competing interest
No authors have conflict of interest or financial relationship with any commercial organization that may have a direct or indirect interest in the content.
Contributor Information
Rola Husain, Email: rola.mahmood@gmail.com.
Jared Nesbitt, Email: jared.nesbitt@gmail.com.
Dharmesh Tank, Email: dharmesh.tank@gmail.com.
Marco Oriundo Verastegui, Email: m.oriundo@gmail.com.
Elaine S. Gould, Email: elaine.gould@stonybrookmedine.edu.
Mingqian Huang, Email: mingqian.huang@mountsinai.org.
References
- 1.Ahlback S, Bauer GC, Bohne WH. Spontaneous osteonecrosis of the knee. Arthritis Rheum. 1968;11(6):705–733. doi: 10.1002/art.1780110602. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto T, Bullough PG. Spontaneous osteonecrosis of the knee: the result of subchondral insufficiency fracture. J Bone Joint Surg Am. 2000;82(6):858–866. doi: 10.2106/00004623-200006000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Akamatsu Y, Mitsugi N, Hayashi T, Kobayashi H., Saito T. Low bone mineral density is associated with the onset of spontaneous osteonecrosis of the knee. Acta Orthop. 2012;83(3):249–255. doi: 10.3109/17453674.2012.684139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gil HC, Levine SM, Zoga AC. MRI findings in the subchondral bone marrow: a discussion of conditions including transient osteoporosis, transient bone marrow edema syndrome, SONK, and shifting bone marrow edema of the knee. Semin Musculoskelet Radiol. 2006;10(3):177–186. doi: 10.1055/s-2006-957171. [DOI] [PubMed] [Google Scholar]
- 5.Narvaez J, Narvaez JA, Rodriguez-Moreno J, Roig-Escofet D. Osteonecrosis of the knee: differences among idiopathic and secondary types. Rheumatology (Oxford) 2000;39(9):982–989. doi: 10.1093/rheumatology/39.9.982. [DOI] [PubMed] [Google Scholar]
- 6.Reddy AS, Frederick RW. Evaluation of the intraosseous and extraosseous blood supply to the distal femoral condyles. The American journal of sports medicine. 1998;26(3):415–419. doi: 10.1177/03635465980260031201. [DOI] [PubMed] [Google Scholar]
- 7.Strauss EJ, Kang R, Bush-Joseph C, Bach BR., Jr. The diagnosis and management of spontaneous and post-arthroscopy osteonecrosis of the knee. Bulletin of the NYU hospital for joint diseases. 2011;69(4):320–330. [PubMed] [Google Scholar]
- 8.Karim AR, Cherian JJ, Jauregui JJ, Pierce T, Mont MA. Osteonecrosis of the knee. Annals of translational medicine. 2015 Jan;3(1) doi: 10.3978/j.issn.2305-5839.2014.11.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jose J, Pasquotti G, Smith MK, Gupta A, Lesniak BP, Kaplan LD. Subchondral insufficiency fractures of the knee: review of imaging findings. Acta Radiol. 2015;56(6):714–719. doi: 10.1177/0284185114535132. [DOI] [PubMed] [Google Scholar]
- 10.Nakayama H, Iseki T, Kanto R, Daimon T, Kashiwa K, Yoshiya S. Analysis of risk factors for poor prognosis in conservatively managed early-stage spontaneous osteonecrosis of the knee. Knee. 2016;23(1):25–28. doi: 10.1016/j.knee.2015.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Aglietti P, Insall JN, Buzzi R, Deschamps G. Idiopathic osteonecrosis of the knee. Aetiology, prognosis and treatment. The Journal of bone and joint surgery British. 1983;65(5):588–597. doi: 10.1302/0301-620X.65B5.6643563. [DOI] [PubMed] [Google Scholar]
- 12.Jureus J, Lindstrand A, Geijer M, Robertsson O, Tagil M. The natural course of spontaneous osteonecrosis of the knee (SPONK): a 1- to 27-year follow-up of 40 patients. Acta Orthop. 2013;84(4):410–414. doi: 10.3109/17453674.2013.810521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lecouvet FE, van de Berg BC, Maldague BE, Lebon CJ, Jamart J, Saleh M. Early irreversible osteonecrosis versus transient lesions of the femoral condyles: prognostic value of subchondral bone and marrow changes on MR imaging. American Journal of Roentgenology. 1998;170(1):71–77. doi: 10.2214/ajr.170.1.9423603. [DOI] [PubMed] [Google Scholar]
- 14.Yates PJ, Calder JD, Stranks GJ, Conn KS, Peppercorn D, Thomas NP. Early MRI diagnosis and non-surgical management of spontaneous osteonecrosis of the knee. Knee. 2007;14(2):112–116. doi: 10.1016/j.knee.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Horikawa A, Miyakoshi N, Shimada Y, Kodama H. Spontaneous Osteonecrosis of the Knee: A Retrospective Analysis by Using MRI and DEXA. Open Orthop J. 2016;10(2):532–538. doi: 10.2174/1874325001610010532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacDessi SJ, Brophy RH, Bullough PG, Windsor RE, Sculco TP. Subchondral fracture following arthroscopic knee surgery. A series of eight cases. J Bone Joint Surg Am. 2008;90(5):1007–1012. doi: 10.2106/JBJS.G.00445. [DOI] [PubMed] [Google Scholar]
- 17.Nelson F, Bokhari O, Oravec D, Kim W, Flynn M, Lumley C. The Use of Tomosynthesis in the Global Study of Knee Subchondral Insufficiency Fractures. Acad Radiol. 2017;24(2):175–183. doi: 10.1016/j.acra.2016.09.015. [DOI] [PubMed] [Google Scholar]
- 18.Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y. Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fractures of the femoral head. AJR Am J Roentgenol. 2013;201(1) doi: 10.2214/AJR.12.9615. W97-103. [DOI] [PubMed] [Google Scholar]
- 19.Hackney LA, Lee MH, Joseph GB, Vail TP, Link TM. Subchondral insufficiency fractures of the femoral head: associated imaging findings and predictors of clinical progression. Eur Radiol. 2016;26(6):1929–1941. doi: 10.1007/s00330-015-3967-x. [DOI] [PubMed] [Google Scholar]
- 20.Nelson FR, Craig J, Francois H, Azuh O, Oyetakin-White P, King B. Subchondral insufficiency fractures and spontaneous osteonecrosis of the knee may not be related to osteoporosis. Arch Osteoporos. 2014;9:194. doi: 10.1007/s11657-014-0194-z. [DOI] [PubMed] [Google Scholar]
- 21.Wilmot AS, Ruutiainen AT, Bakhru PT, Schweitzer ME, Shabshin N. Subchondral insufficiency fracture of the knee: A recognizable associated soft tissue edema pattern and a similar distribution among men and women. Eur J Radiol. 2016;85(11):2096–2103. doi: 10.1016/j.ejrad.2016.08.016. [DOI] [PubMed] [Google Scholar]