Highlights
-
•
Accelerated femoral head osteonecrosis after a single dose intra-articular steroid injection is rare with few cases reported in the literature.
-
•
Two patients developed rapid femoral head destruction at 14 and 11 weeks following a single intra-articular steroid injection, respectively.
-
•
Cases of accelerated femoral head osteonecrosis with subsequent resorption can be treated successfully with total hip arthroplasty.
Keywords: Avascular, Necrosis, Osteonecrosis, Femoral, Head
Abstract
Introduction
Accelerated femoral head avascular necrosis after a single dose intra-articular steroid injection is a rare pathology. Few cases were reported in the literature. Most cases were managed with total hip arthroplasty.
Case presentation
In this study, we report two rare cases of destructive osteonecrosis of the femoral head. Both patients presented with hip osteoarthritis that failed nonoperative measures. A single intra-articular corticosteroid injection was administered for each patient. Both patients had femoral head destruction and significant resorption at 14 and 11 weeks, respectively. Septic arthritis was ruled out by blood tests and joint aspiration. Total hip arthroplasty (THA) was undertaken and histology reports confirmed the osteonecrosis. The postoperative follow-up was uneventful with satisfactory hip function.
Discussion and conclusion
Destructive osteonecrosis of the femoral head is a rare catastrophic potential complication of intra-articular corticosteroid injection. Hence, physicians must consider this complication when counseling patients before an intra-articular corticosteroid hip injection.
1. Introduction
The incidence of femoral head osteonecrosis has been estimated to reach up to 30,000 cases annually, and it accounts for 10% of the indications for total hip arthroplasty (THA) [1], [2].
Femoral head osteonecrosis can develop following direct factors such as femoral neck fracture, hip dislocations, radiation. Whereas, indirect factors consist of corticosteroids, alcohol intake, smoking, hypercoagulable states, marrow-replacing disease (e.g., Gaucher disease), systemic lupus erythematosus (SLE), Caisson disease and viral infections (e.g., hepatitis, human immunodeficiency) [3], [4].
It is noteworthy that up to 40% of hip osteonecrosis are attributed to the use of corticosteroids [5]. The risk of osteonecrosis is most significant with prolonged and high dose corticosteroid treatment [5], [6]. In addition, short-term exposure has been described in several reports as well. However, only a few cases of osteonecrosis of the femoral head have been reported following a single intra-articular injection [7]. In this report, we describe two rare cases of destructive osteonecrosis of the femoral head after a single corticosteroid injection.
The patients were informed that data concerning their cases would be submitted for publication, and they provided consent.
2. Case presentation
The Surgical Case Report (SCARE) statement guidelines were utilized in the reporting of the two cases [8].
Case 1. A 58-years-old female presented with left hip post-traumatic osteoarthritis two years after open reduction and internal fixation for left acetabulum posterior wall fracture-dislocation (Fig. 1). The pain was exacerbated with activity and relieved by rest. She had a past medical history of hypertension and hypothyroidism, however no history of cancer, blood coagulation disorders, or inflammatory arteriopathies. No previous intake of corticosteroids. No history of smoking or alcohol consumption.
Fig. 1.
Case 1; Anteroposterior and lateral pelvis radiographs demonstrating left hip post-traumatic arthritis.
Initially she was treated with nonoperative measures such as self-directed exercises, weight loss, and analgesia. The left hip pain was refractory to the aforementioned conservative modalities, which impaired her daily living activities. Subsequently, a fluoroscopy-guided intra-articular corticosteroid injection of methylprednisolone acetate 80 mg and 3 mL of bupivacaine 0.5% was administered and the pain was improved for six weeks. At 14 weeks following the injection, she presented with further deterioration in left hip pain with the inability to perform any sort of weight-bearing. Physical examination demonstrated inability of weight-bearing ambulation, left lower limb shortening of approximately 2 cm, and a painful global range of motion.
Infection laboratory workup, including the hip joint aspiration and triphasic bone scan, were negative. Left hip plain radiographs and CT scan demonstrated destruction and resorption of the left femoral head (Fig. 2).
Fig. 2.
Case 1; Anteroposterior and lateral pelvis radiograph displaying left femoral head resorption following an intra-articular corticosteroid injection.
Subsequently, a cementless left THA with ceramic on ceramic bearings was performed through the posterior hip approach, and the implants from the previous acetabulum ORIF were retained. A bone biopsy was taken from the remnant of the femoral head which confirmed the diagnosis of osteonecrosis and ruled out the presence of infection (Fig. 3).
Fig. 3.
Case 1; Histological photomicrographs of the intraoperative femoral head fragments demonstrating A) Necrotic bony trabeculae with empty lacunae (arrows) adjacent to fibrotic bone marrow (hematoxylin and eosin ×100). B) Significant bone marrow fibrosis (hematoxylin and eosin ×200).
Postoperatively, the patient had a smooth recovery and was discharged with a postoperative physical therapy plan. At the latest follow-up of five years, she was satisfied with the left hip function, and no postoperative complications were noted (Fig. 4).
Fig. 4.
Case 1; post-operative anteroposterior and lateral hip radiographs following total hip arthroplasty.
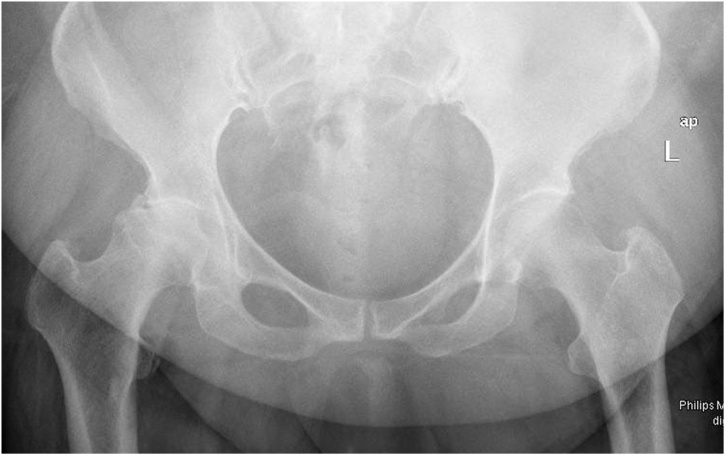
Case 2. A 47-year-old female who is a known case of psoriasis complained of right hip worsening pain and difficulty in performing daily life activities. She is known to have right hip osteoarthritis (Fig. 5), which failed conservative measures such as non-steroidal anti-inflammatories, and physical therapy. No past surgical history, however, she has a past medical history of coronary artery disease, morbid obesity and modulating immunotherapy for psoriasis. No relevant family history, and no alcohol intake or smoking.
Fig. 5.
Case 2; Anteroposterior pelvis radiograph demonstrating right hip osteoarthritis.
A right hip ultra-sound guided intra-articular injection with 3 mL levobupivacaine 0.5% and triamcinolone acetonide 40 mg was performed by a pain specialist, with immediate pain relief. Eleven weeks later she presented with worsening right hip pain with the inability to perform any sort of weight-bearing. Physical examination showed inability of weight-bearing ambulation, right lower limb shortening of 3 cm, and painful global range of motion.
The infection workup revealed a white cell count of 5.5 × 10^3/μL and a C-reactive protein of 1.3 mg/L with negative joint aspiration. Right hip plain radiographs displayed right femoral head destruction and resorption (Fig. 6).
Fig. 6.
Case 2; Anteroposterior and lateral hip radiographs displaying right femoral head resorption following an intra-articular corticosteroid injection.
Thereafter, a cementless right THA with ceramic on ceramic bearings was performed through the posterior hip approach (Fig. 7). Bone biopsy was taken from the remnant of the femoral head which ruled out infection and confirmed the diagnosis of osteonecrosis (Fig. 8).
Fig. 7.
Case 2; post-operative anteroposterior and lateral hip radiographs following a total hip arthroplasty.
Fig. 8.
Case 2; A) Macroscopic photo showing femoral head fragmentation B) Histological photomicrograph (hematoxylin and eosin stain ×40) of the intraoperative femoral head fragments demonstrating bony erosion with subchondral cysts surrounded by fibrosis.
Postoperatively, the patient had an uneventful course and was discharged within eight days after achieving physical therapy discharge milestones. At the latest follow-up point 1 year postoperatively, she was ambulating independently with a profound improvement in pain and hip function with no postoperative complications.
3. Discussion
This study reported two cases with destructive osteonecrosis of the femoral head after single intra-articular corticosteroid injection. The osteonecrosis in both cases was destructive, occurring within 14 and 11 weeks of intraarticular steroid injection in each case, respectively.
In the first case, the patient had a posttraumatic osteoarthritis and in the second case, the patient is known to be obese, psoriatic with osteoarthritis.
In the literature, few cases have been previously reported with femoral head osteonecrosis following single intra-articular corticosteroid injections (Table 1) [7], [9], [10], [11]. It was first reported in 2006 on a 50-year-old female with left hip osteoarthritis following a single intra-articular injection with 80 mg of methylprednisolone [9]. In previous case reports, patients presented initially with mild hip osteoarthritis, which deteriorated rapidly into severe hip pain and disability. The period from an intra-articular corticosteroid injection to deterioration ranged from 4 to 12 weeks. The radiographs in all cases were notable for femoral head collapse and flattening. The underlying etiology of osteonecrosis was confirmed with histology, and infectious processes were ruled out. Hip replacement in the form of THA was performed in all reports, except in the case report by Vanushkina et al., who implemented a hip hemiarthroplasty instead.
Table 1.
Summary of reported cases of rapidly-progressive osteonecrosis of the femoral head following a single intra-articular corticosteroid injection.
| Author, year | Age | Sex | Diagnosis | Corticosteroid Injection | Time | Treatment |
|---|---|---|---|---|---|---|
| Yamamoto, 2006 | 50 | Female | Osteoarthritis | Methylprednisolone acetate 80 mg | 12 weeks | THA |
| Kassam, 2010 | 79 | Male | Osteoarthritis | Triamcinolone acetonide 2 mL | 5 weeks | THA |
| Thompson and Ensrud, 2019 | 72 | Female | Osteoarthritis | Triamcinolone acetonide 80mg | 4 weeks | THA |
| Al-Omari, 2019 | 78 | Male | Osteoarthritis | Unspecified | 7.25 weeks | THA |
In the evaluation of the destruction of the femoral head, several differential diagnoses should be considered. Septic hip infection following intra-articular injections is a potentially devastating complication. The incidence of iatrogenic joint infection is rare with an incidence 2–10 cases per 100,000 injections [12]; however, its prevalence has increased given the frequent use of intra-articular corticosteroids and viscosupplements in the management of osteoarthritis. Risk factors for iatrogenic joint infections include immunocompromised states (e.g., diabetes mellitus, HIV, immunosuppressants), excessive alcohol intake, previous joint or skin infections, presence of joint prosthesis and previous joint surgery [13]. It is paramount to rule out any infectious processes. A proper history and physical examination in combination with inflammatory markers and intraoperative tissue cultures are necessary for the process of evaluation.
Another differential diagnosis is rapidly-progressive osteoarthritis, which is defined as loss of > 50% of joint space within 12 months [14]. It can occur following trauma such as acetabular fracture, which is more prevalent in elderly males. However, non-traumatic cases have been reported in elderly female [15]. The clinical presentation resembles that of rapidly-progressive osteonecrosis; therefore, further investigations are useful in differentiating one condition from another. In early stages, the subchondral fractures in rapidly progressive osteoarthritis appear as a curvilinear band of low signal on all MRI sequences [16]. Whereas, the MRI findings in osteonecrosis display edema with serpentine-like pattern and the subchondral fracture is concave to the articular surface [17]. In late stages where the femoral head is destroyed, MRI findings and histopathology offer little to no value in differentiating between both conditions. Histology in rapidly-progressive osteoarthritis shows synovitis that is consistent with reactive and hypervascularity changes [15]. However, osteonecrosis histology is evident in bone marrow edema and necrosis with appositional bone formation [18].
In summary, destructive osteonecrosis of the femoral head is a rare catastrophic potential complication of intra-articular corticosteroid injection. Hence, physicians must consider this complication when counseling patients before an intra-articular corticosteroid hip injection. In addition, such cases can be treated effectively with THA.
Conflicts of interest
No conflict of interest to declare.
Funding
No funding was obtained for this case report.
Ethical approval
The case report was approved by the medical research centre at Hamad Medical Corporation, Doha, Qatar. Reference number: MRC-04-20-188.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
AA, MH and MS wrote the manuscript and consented the patients. GA was the senior author who provided supervision for writing this case report.
Registration of research studies
The study is a case report and has no registries.
Guarantor
Dr. Ghalib Ahmed is the senior author and the guarantor.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Desforges J.F., Mankin H.J. Nontraumatic necrosis of bone (Osteonecrosis) N. Engl. J. Med. 1992;326(May (22)):1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 2.Moya-Angeler J., Gianakos A.L., Villa J.C., Ni A., Lane J.M. Current concepts on osteonecrosis of the femoral head. World J. Orthop. 2015;6(September (8)):590–601. doi: 10.5312/wjo.v6.i8.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lausten G.S. Non-traumatic necrosis of the femoral head. Int. Orthop. 1999;23(November (4)):193–197. doi: 10.1007/s002640050348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergman J., Nordström A., Nordström P. Epidemiology of osteonecrosis among older adults in Sweden. Osteoporos. Int. 2019;30(May (5)):965–973. doi: 10.1007/s00198-018-04826-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein R.S. Glucocorticoid-induced bone disease. N. Engl. J. Med. 2011;365(July (1)):62–70. doi: 10.1056/NEJMcp1012926. [DOI] [PubMed] [Google Scholar]
- 6.Mont M.A., Pivec R., Banerjee S., Issa K., Elmallah R.K., Jones L.C. High-dose corticosteroid use and risk of hip osteonecrosis: meta-analysis and systematic literature review. J. Arthroplasty. 2015;30(September (9)):1506–1512. doi: 10.1016/j.arth.2015.03.036. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Omari A.A., Aleshawi A.J., Marei O.A., Bani Younes H.M., Alawneh K.Z., ALQuran E. Avascular necrosis of the femoral head after single steroid intra-articular injection. Eur. J. Orthop. Surg. Traumatol. 2020;30:193–197. doi: 10.1007/s00590-019-02555-8. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T., Schneider R., Iwamoto Y., Bullough P.G. Rapid destruction of the femoral head after a single intraarticular injection of corticosteroid into the hip joint. J. Rheumatol. 2006;33(August (8)):1701–1704. [PubMed] [Google Scholar]
- 10.Kassam A.M. Accelerated avascular necrosis after single intra-articular injection of corticosteroid into the hip joint. Case Rep. 2010;2010 bcr1020092405. [Google Scholar]
- 11.Thompson A.R., Ensrud E.R. Rapid onset of femoral head osteonecrosis after a single intra-articular hip joint injection of corticosteroid. Am. J. Phys. Med. Rehabil. 2020;99(April (4)):e54–e55. doi: 10.1097/PHM.0000000000001202. [DOI] [PubMed] [Google Scholar]
- 12.Mathews C.J., Coakley G. Septic arthritis: current diagnostic and therapeutic algorithm. Curr. Opin. Rheumatol. 2008;20(July (4)):457–462. doi: 10.1097/BOR.0b013e3283036975. [DOI] [PubMed] [Google Scholar]
- 13.Kaandorp C.J.E., Van Schaardenburg D., Krijnen P., Habbema J.D., van de Laar M.A. Risk factors for septic arthritis in patients with joint disease. Arthritis Rheum. 1995;38(December (12)):1819–1825. doi: 10.1002/art.1780381215. [DOI] [PubMed] [Google Scholar]
- 14.Lequesne M. Rapidly progressing destructive diseases of the hip. Ann. Radiol. (Paris) 1993;36:62–64. [PubMed] [Google Scholar]
- 15.Flemming D.J., Gustas-French C.N. Rapidly progressive osteoarthritis: a review of the clinical and radiologic presentation. Curr. Rheumatol. Rep. 2017;19(July (7)):42. doi: 10.1007/s11926-017-0665-5. [DOI] [PubMed] [Google Scholar]
- 16.Boutry N., Paul C., Leroy X., Fredoux D., Migaud H., Cotton A. Rapidly destructive osteoarthritis of the hip: MR imaging findings. AJR Am. J. Roentgenol. 2002;179(September (3)):657–663. doi: 10.2214/ajr.179.3.1790657. [DOI] [PubMed] [Google Scholar]
- 17.Ikemura S., Yamamoto T., Motomura G., Nakashima Y., Mawatari T., Iwamoto Y. MRI evaluation of collapsed femoral heads in patients 60 years old or older: differentiation of subchondral insufficiency fracture from osteonecrosis of the femoral head. AJR Am. J. Roentgenol. 2010;195(1):W63–8. doi: 10.2214/AJR.09.3271. [DOI] [PubMed] [Google Scholar]
- 18.Chernetsky S.G., Mont M.A., LaPorte D.M., Jones L.C., Hungerford D.S., McCarthy E.D. Pathologic features in steroid and nonsteroid associated osteonecrosis. Clin. Orthop. Relat. Res. 1999:149–161. [PubMed] [Google Scholar]