Highlights
-
•
Nutcracker syndrome is characterized by compression of the left renal vein between the abdominal aorta and the superior mesenteric artery, resulting in an obstruction of blood flow from the left renal vein into the inferior vena cava due to extrinsic compression.
-
•
The management of nutcracker syndrome depends on the clinical presentation and severity of hypertension in the left renal vein, ranging from simple monitoring to nephrectomy.
-
•
Surgical techniques used for the treatment of patients with severe symptoms.
Keywords: Nutcracker syndrome, Left renal vein, Aorto-mesenteric region, Surgery
Abstract
Nutcracker syndrome is a rare entity that corresponds to an abdominal pain following compression of the left renal vein during its passage between the aorta and the superior mesenteric artery, with a peak prevalence in adults between 20 and 30 years old, The typical clinical presentation includes hematuria, orthostatic proteinuria with or without flank pain. doppler ultrasound has a sensitivity of 78% and specificity of 100%, Both CT and MRI can show the compression of the left renal vein between the aorta and the superior mesenteric artery.
We report the case of a young patient admitted to the emergency room for abdominal pain mainly localized in the left hypochondrium, with microscopic hematuria, a CT scan was performed showing a reduced aorto mesenteric angle with a compression of the left renal vein and collateralization of venous circulation of left gonadal vein.
1. Introduction
Nutcracker syndrome is a rare entity that corresponds to a benign abdominal pain following compression of the left renal vein during its passage between the aorta and the superior mesenteric artery [1] often evoked in the presence of chronic hematuria. The diagnosis is confirmed by a CT scan of vascular reconstruction of the hilar region of the kidney and the study of the pressure gradient between the left renal vein and the inferior vena cava [2], we report the case of a young patient admitted to the emergency room for abdominal pain mainly localized in the left hypochondrium, with microscopic hematuria, a CT scan was performed showing a reduced aorto mesenteric angle with a compression of the left renal vein and collateralization of venous circulation of left gonadal vein.
1.1. Patient and observation
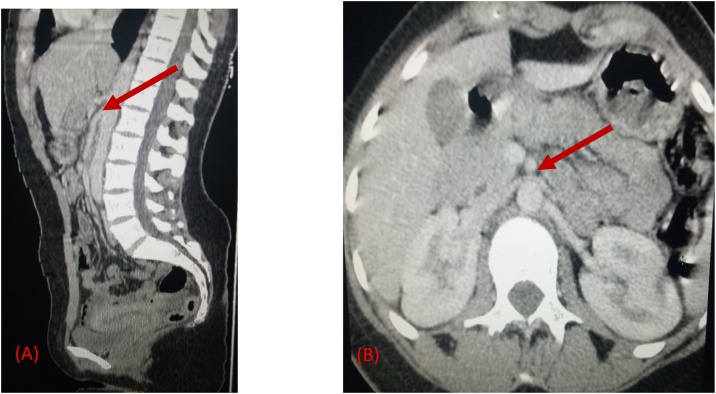
A 20-year-old woman with no particular pathological history admitted to the emergency room for abdominal pain in the left hypochondrium and epigastric region without any transit disorder or externalized digestive bleeding, and in whom the physical examination found a conscious patient who was hemodynamically and respiratory stable, the body mass index was 18 kg/m2 (underweight). The abdominal examination found an epigastric and left hypochondrium tenderness, an abdominal CT scan was performed showing an aorto-mesenteric angle measured at 14.2° with a narrowing of the left renal vein at this (Fig. 1), and varicose dilatation of the homolateral gonadal vein (Fig. 2).
Fig. 1.
(A) an axial CT showing the beak sign with an upper aorto-mesenteric angle measured at 14.2° (red arrow). (B) Curved image demonstrating Beak Sign at the aortomesenteric portion of the left renal vein.
Fig. 2.
CT scan showing a varicose dilatation of the left gonadal vein (arrow).
The biological check-up showed a microcytic hypochromic anemia with a hemoglobin level of 9 g/dl with a microscopic hematuria without proteinuria at the urinary analysis, the creatinine level is 7 mg/l and the urea level is 0.34 g/l. A conservative management was performed, The patient benefited from a clinical-biological monitoring with an hypercaloric diet, after 7 days of hospitalization the abdominal pain disappeared and the patient was advised to gain weight to increase in retroperitoneal adipose tissue, for reducing left renal vein tension, the patient was followed up every 6 months with a control examinations and if needed a intra venous CT scan.
2. Discussion
Nutcracker syndrome is characterized by compression of the left renal vein between the abdominal aorta and the superior mesenteric artery, resulting in an obstruction of blood flow from the left renal vein into the inferior vena cava due to extrinsic compression [3]. This is a rare situation whose prevalence is unknown [4]. It has been described as more common in women in the third or fourth decade, although a later study showed equal prevalence between men and women [5] with a peak prevalence in adults between 20 and 30 years old probably related to the rapid development of vertebral bodies during puberty, causing a narrowing of the angle between the abdominal aorta and the superior mesenteric artery [6] compression of the left renal artery is most often anterior, between the abdominal aorta and the superior mesenteric artery, more rarely compression is posterior when the left renal vein passes between the abdominal aorta and the spine, then we speak of a posterior nutcracker syndrome [7] the other etiologies: Pancreatic tumors, para-aortic adenopathy, retroperitoneal tumors, abdominal aortic aneurysm, duplication of the left renal vein, left renal ptosis, lordosis and decrease of retroperitoneal and mesenteric adipose tissue [8] the nutcracker syndrome can be clinically differentiated into 2 subtypes as follows: typical presentation (or renal presentation) and atypical presentation (or urological presentation). The typical clinical presentation includes hematuria, orthostatic proteinuria with or without flank pain. Atypical presentation includes Abdominal pain, varicocele, dyspareunia, dysmenorrhea, fatigue and orthostatic intolerance [3]. Positive diagnosis is based on imaging showing a renal cell recoil gradient ≥3 mmHg, an angle of less than 45° between the aorta and the superior mesenteric artery, a narrowing of the left renal vein, Collateral venous circulation, gonadal vein distension or pelvic congestion [6]. Doppler ultrasound has a sensitivity of 78% and specificity of 100%. Both CT and MRI can demonstrate compression of the left renal vein in the angle formed by the superior mesenteric artery and the abdominal aorta, gonadal vein distension and pelvic congestion. The most specific nutcracker syndrome CT result was a ratio of left renal vein diameter of hilar and aorto-mesenteric left renal vein ≥4.9 (100% specificity) and an axial CT image with a beak sign [3]. Phlebography is the standard gold test to confirm the diagnosis of nutcracker syndrome which shows a pressure gradient in the trapping zone. The reflux of contrast into the adrenal and gonadal veins from the peri-urethral and peri-renal venous collaterals, and the pooling of contrast in the left renal vein [9]. The management of nutcracker syndrome depends on the clinical presentation and severity of hypertension in the left renal vein, ranging from simple monitoring to nephrectomy. Mild and tolerable symptoms can be followed conservatively. However, recurrent coarse hematuria with anemia, severe flank pain, impaired renal function and ineffective or worsening conservative therapy, persistent orthostatic proteinuria after 24 months of follow-up may require surgical treatment [9,10]. The conservative approach with observation for at least 2 years without medication is the best option for patients under 18 years of age, 75% of patients with hematuria have complete resolution during this period [11]. Surgical techniques used for the treatment of patients with severe symptoms are Nephropexy, intravascular and extravascular stent implantation, transposition of the left renal vein or superior mesenteric artery, gonadal bypass surgery, renal auto transplantation and nephrectomy [3] to our patient, the therapeutic attitude was a clinical surveillance with an hypercaloric diet weight to increase in retroperitoneal adipose tissue, for reducing left renal vein tension. This case has been reported in line with the SCARE Guideline 2018 [12].
3. Conclusion
The nutcracker syndrome is defined as the compression of the left renal vein between the aorta and the superior mesenteric artery angle responsible for many clinical manifestations, often unknown and must be evoked in front of abdominal pain associated with micro o macroscopic hematuria, its management depends on the severity of clinical signs ranging from simple monitoring to nephrectomy.
Declaration of Competing Interest
The authors report no declarations of interest.
Funding
There is no sources of funding.
Ethical approval
It is a case report and not a study.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
This work was carried out in collaboration among all authors. All authors contributed to the conduct of this work. They also declare that they have read and approved the final version of the manuscript
Registration of research studies
N/A.
Guarantor
None.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Teyeb Z., Hamzaoui S., Larbi T., Abdallah M., Bouslema K., M’rad S. A rare etiology of chronic abdominal pain: nutcracker syndrome. Rev. Intern. Med. 2014;35(December):A162–A163. [Google Scholar]
- 2.Andrianne Robert, Limet Raymond, Waltregny David. Hematuria caused by nutcracker syndrome: peroperatory confirmation of its reality. Prog. Urol. 2002;12(6):1323–1326. [PubMed] [Google Scholar]
- 3.Gulleroglu K., Gulleroglu B., Baskin E. Nutcracker syndrome. World J. Nephrol. 2014;3(November (4)):277–281. doi: 10.5527/wjn.v3.i4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Penfold Dana, et Lotfollahzadeh Saran. 2020. Nutcracker Syndrome. StatPearls. [Internet] [PubMed] [Google Scholar]
- 5.Dunphy L., Penna M., Tam E., Jihene E.-K. Left renal vein entrapment syndrome: nutcracker syndrome! BMJ Case Rep. CP. 2019;12(9) doi: 10.1136/bcr-2019-230877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ananthan K., Onida S., Davies A.H. Nutcracker syndrome: an update on current diagnostic criteria and management guidelines. Eur. J. Vasc. Endovasc. Surg. 2017;53(6):886–894. doi: 10.1016/j.ejvs.2017.02.015. [DOI] [PubMed] [Google Scholar]
- 7.He Y., Wu Z., Chen S., Tian L., Li D., Li M. Nutcracker syndrome-how well do we know it? Urology. 2014;83(1):12–17. doi: 10.1016/j.urology.2013.08.033. [DOI] [PubMed] [Google Scholar]
- 8.Basile A., Tsetis D., Calcara G., Figuera M., Coppolino F., Patti M.T. Nutcracker syndrome due to left renal vein compression by an aberrant right renal artery. Am. J. Kidney Dis. 2007;50(2):326–329. doi: 10.1053/j.ajkd.2007.05.016. [DOI] [PubMed] [Google Scholar]
- 9.Noorani A., Walsh S.R., Cooper D.G. Entrapment syndromes. Eur. J. Vasc. Endovasc. Surg. 2009;37(2):213–220. doi: 10.1016/j.ejvs.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Wang Long, Yi Lu, Yang Luoyan. Diagnosis and surgical treatment of nutcracker syndrome: a single-center experience. Urology. 2009;73(4):871–876. doi: 10.1016/j.urology.2008.11.043. [DOI] [PubMed] [Google Scholar]
- 11.Kurklinsky Andrew K., et rooke Thom W. Mayo Clinic Proceedings. Elsevier; 2010. Nutcracker phenomenon and nutcracker syndrome; pp. 552–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]