Highlights
-
•
Hematocolpos remains the main consequence of the transversal septums of vagina.
-
•
The management of transversal septum of vagina is essentially based on surgery.
-
•
The risk of vaginal stenosis after surgery remains high.
Keywords: Hematocolpos, Transverse vaginal septum, Primary amenorrhoea
Abstract
Introduction
The transverse septum of the vagina or vaginal septum is a rare abnormality of the female genital tract. The most frequently advanced etiology is a defect in the fusion and/or channelling of the urogenital sinus and Mullerian conductors. This structural obstruction can completely obstruct the vagina and thus can cause a haematocolpos associated with cyclic pelvic pain shortly after menarche in adolescent girls. The diagnosis of a vaginal septum is based on a careful clinical gynaecological examination and especially on ultrasound scan via the abdominal or transrectal (see Transperineal) and in more complex cases on MRI. The treatment is surgical and must be carried out as early as possible.
Case report
We report the management of a case of a 16 year old girl who presented a haematocolpos complicating a complete transverse vaginal septum. The treatment consisted of making a transverse incision in the centre of the transverse septum of the vagina, draining the hematocolpos and visualising the cervix. A circumferential excision of the septum was made and the remaining vaginal edges were then sutured by a simple tarring of the entire circumference with Vicryl 2.0. A sponge soaked in oestrogen cream was placed in her vagina to prevent stenosis and removed the day after the operation. The patient was followed in our department for 2 years without any recurrence of vaginal stenosis or hematocolpos.
Conclusion
The transverse vaginal septum remains a rare anomaly of the female genital tract, the reasons for its discovery are extremely variable according to its shape and location. Haematocolpos remains the main consequence of these septums. The management is essentially based on surgery while taking into account the risks of postoperative stenosis and the repercussions on the upper genital tract.
1. Introduction
The transverse vaginal septum or vaginal septum is a rare abnormality of the female genital tract with an incidence of between 1/2100 and 1/7200 [1]. The most common etiology is a defect in the fusion and/or channelling of the urogenital sinus and Mullerian conductors [2]. The transverse vaginal septum can develop anywhere in the vagina, and its most common locations are in the lower part of the vagina according to the latest publications, so 72% of the septums are in the lower part of the vagina, 22% in the central part and 6% in the upper part of the vagina [3]. These septa are usually no more than 1 cm thick and usually have an eccentric perforation which allows for vaginal discharge. These structural obstacles can completely obstruct the vagina and can cause haematocolpos associated with cyclic pelvic pain shortly after menarche in adolescent girls. Haematocolpos is defined as an accumulation of menstrual blood in the vaginal cavity [4]. The diagnosis of a vaginal septum is based on a careful clinical gynaecological examination and especially on ultrasound scan via the abdomen or transrectal or even transperineal ultrasound and in more complex cases an MRI scan. The treatment is surgical and should be carried out as early as possible, as its management after puberty is associated with a high rate of vaginal stenosis [5].
2. Presentation of case
This is a 16 year old patient with a history of congenital right kidney agenesis. Without other pathological history, was not taking any drugs and with no medical family history. She presents for consultation with cyclic chronic pelvic pain in a primary amenorrhea context. The patient reports that she has never had sex in her life.
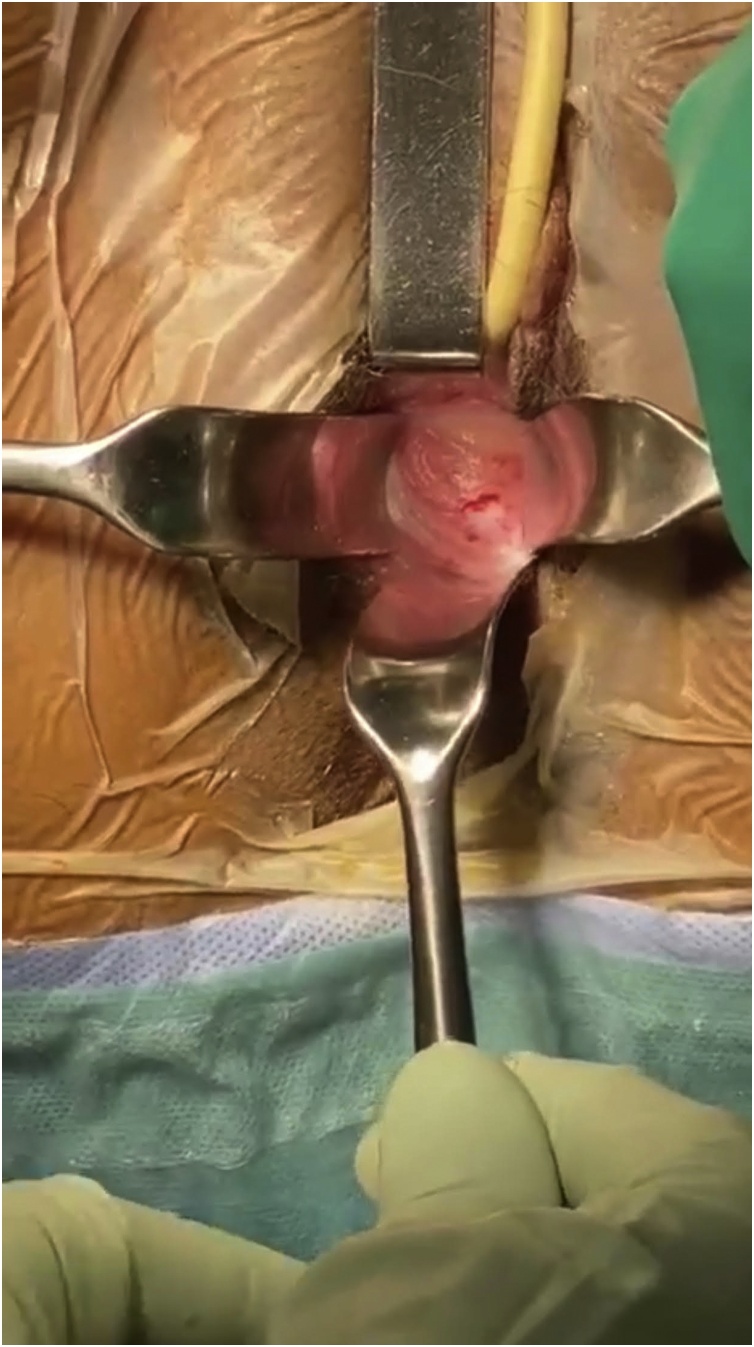
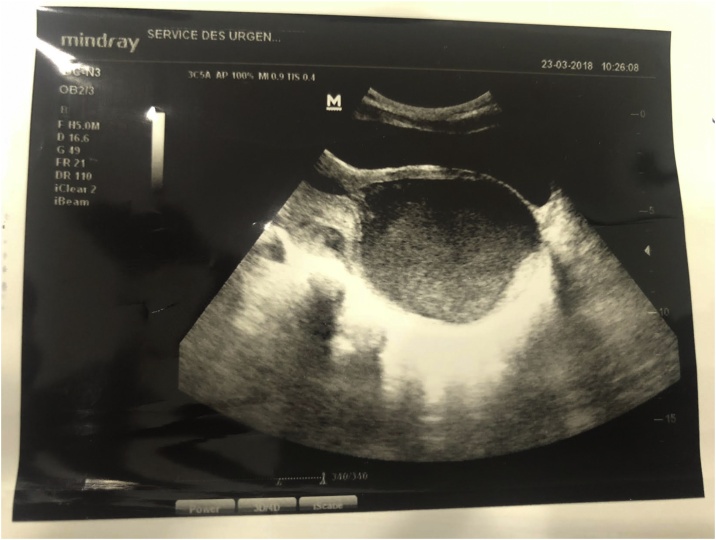
The clinical examination found normal secondary sexual characteristics. A soft, depressed abdomen and sensitivity in the hypogastric area. The vagina examination found a vagina totally obstructed by a transverse septum in the form of a vaginal diaphragm 1 cm from the hymen (Fig. 1). Pelvic and perineal ultrasound found a normal sized uterus with a large haematocolpos of 10 × 12 cm with the presence of a low transverse vaginal septum located 1 cm thick (Fig. 2).
Fig. 1.
Transverse septum obstructing the vagina.
Fig. 2.
Suprapubic ultrasound image showing the haematocolpos in the form of a large anechogenic mass.
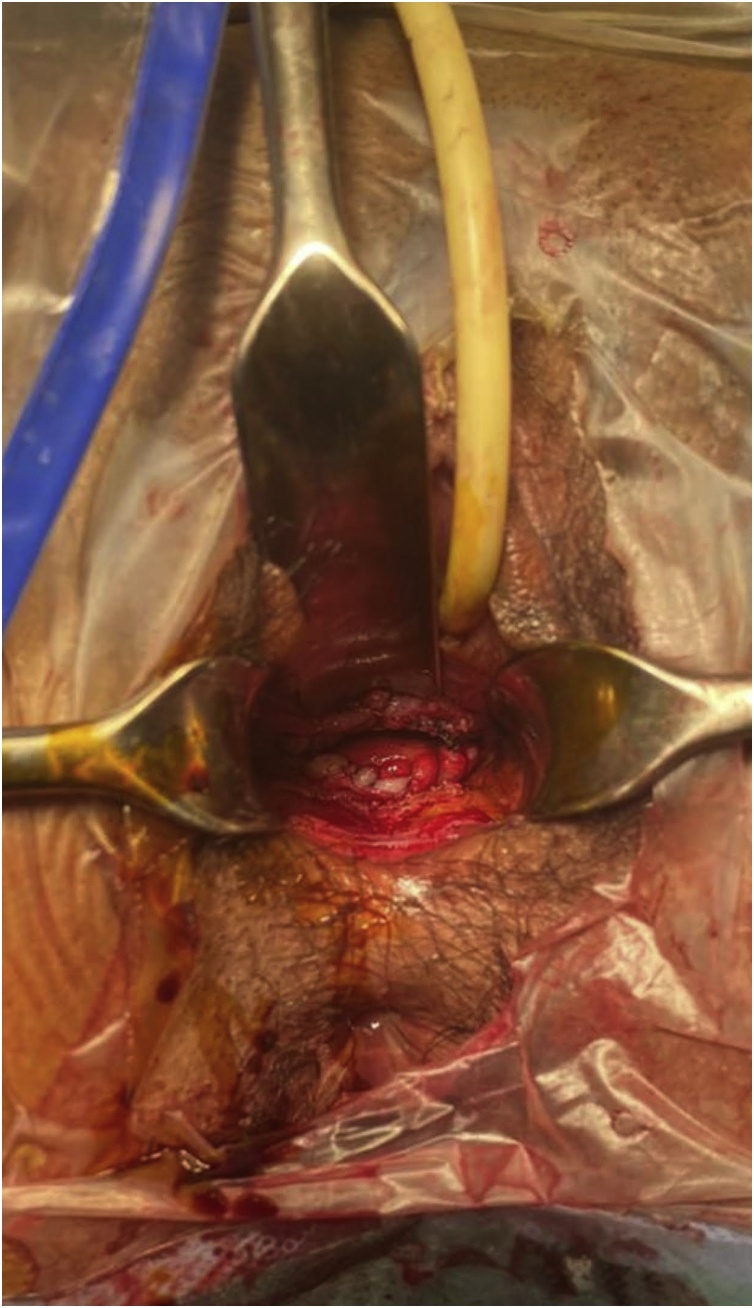
The treatment consisted of making a transverse incision, who was performed bu junior resident with 5 years of specialised training, in the centre of the transverse septum of the vagina, draining the hematocolpos (Fig. 3) and visualising the cervix. A circumferential excision of the septum was made and the remaining vaginal edges were then sutured by a simple tarring of the entire circumference with Vicryl 2.0 (Fig. 4). A sponge soaked in oestrogen cream was placed in her vagina to prevent stenosis and removed the day after the operation. T
Fig. 3.
Haematocolpos drainage after incision of the transverse spetum of the vagina.
Fig. 4.
The final result obtained after suturing the edges of the incision.
Postoperative evolution was favourable. the patient was followed in our department for 2 years without any recurrence of vaginal stenosis or hematocolpos.
3. Discussion
One of the main causes of haematocolpos is the transverse vaginal septum. This transverse vaginal septum results either from incomplete channelling of the vaginal plate or failure of the parameonephral ducts to meet the urogenital sinus [6].
Vaginal septum was first described in 1877 and since then other case series have been published. However, they remain rare due to the low frequency of this anomaly.
The diagnosis of transverse vaginal septum is made either pre-puberty or post-puberty.
In pre-pubertal patients, they present a hydrocolpos caused by an obstruction in the drainage of genital secretions produced by hypersecretion of the proximal reproductive glands which respond to maternal hormonal stimulation, in patients in post puberty, the clinical presentation is variable, depending, above all, on whether or not there is a perforation of the septum. If the septum is complete, as in our case, clinically, they present abdominal pain associated with primary amenorrhoea with the presence of a haematocolpos, haematometry or haematosalpinx depending on the location of the septum. If the septum is incomplete, the diagnosis is more difficult, as it may be asymptomatic with only dyspareunic or infertility symptoms [7].
The transverse vaginal septum is not a common mullerian abnormality. Similar to an imperforate hymen, it can present a diagnostic challenge, as the symptoms are often not gynaecological in nature, e.g. lower abdominal pain, low back pain, chronic constipation [8], or urinary retention [9]. An obstructive genital anomaly should be routinely sought in all young women with these symptoms associated with primary amenorrhea. An imperforate hymen is easily distinguished from a transverse vaginal septum on physical examination. The bluish appearance with a bulge is often observed between the lips in the case of an imperforated hymen. In addition, slight pressure applied suprapubically causes visible distension of the imperforated hymen. On the other hand, if a transverse septum is present, suprapubic pressure does not cause a visible bulge in the perineum. The thickness and exact location of a transverse vaginal septum is difficult to assess clinically unless a patient is willing to undergo a careful vaginal and/or rectoabdominal examination. Most young women before their first sexual activities do not undergo such an examination without general anaesthesia. Therefore, the thickness and location of the septum is most often assessed by abdominal ultrasound, trans perineal or transrectal ultrasound or MRI before attempting management [10].
Very little data is available in the literature on the surgical management of this condition.
In the experience of Dennie et al. [11], the septum should be removed when the girl reaches the age of first menstruation, and surgery is easier if the patient has a haematocolpos before drainage. Williams et al. [12] describe 46 patients with VSDs treated by 3 different routes: laparotomy abdomino-perineal vaginoplasty, simple vaginal excision and laparoscopic resection of the vaginal wall.
Another surgical approach is the Grünberger method, which consists of a cross-shaped incision in the caudal part of the septum and a cross incision in the other part with transverse closure [13,14].
Van Bijsterveldt et al. [15] proposed two new techniques for the treatment of the vaginal wall: push and pull techniques. The former requires a combined abdominal-vaginal approach, and is used in patients with a higher risk of restenosis after surgery. The traction technique is reserved for patients with a simple vaginal obstruction [15].
A modification of this technique was performed by Layman et al. [16] with traction through proximal distension of the vagina using an Olbert balloon catheter to facilitate surgical management and to limit postoperative narrowing of the vagina.
Sardesai et al. [17] described double cross-plasty/Z-plasty for vaginal wall management after 20 years experience as the best technique compared to other surgical methods.
Vaginal stenosis at the resection site remains the most common complication [18]. Postoperative vaginal dilation may help to reduce scarring and stenosis at the surgical site [19]. This postoperative dilation is essential to the success of the procedure.
Other less common complications are described after surgery, such as dyspareunia, menstrual irregularities and fertility problems.
Management of the vaginal septum with drainage of the haematocolpos at an early age is necessary to preserve fertility and reduce the risk of endometriosis.
Therefore, these patients and their parents need to be informed about these potential long-term complications and the importance of regular follow-up [19,20].
We all know that the various surgeries of the transverse septum of the vagina, despite their complexity, are complicated by vaginal stenosis and recurrences. In this context we report a simple and safe technique that allows us to treat this kind of pathologies using a simple technique and which gives us a good result and without recurrence of vaginal obstruction. This surgical technique is based on a transverse incision of the vaginal septum with a tarring of the edges by a VICRYL 2.0 file associated with a sponge containing ostrogen left two days from the postop.
This work has been reported in line with the SCARE 2018 criteria [21].
4. Conclusion
the transverse vaginal septum remains a rare anomaly of the female genital tract, the reasons for its discovery are extremely variable according to its shape and location. haematocolpos remains the main consequence of these septums. the managementis essentially based on surgery while taking into account the risks of postoperative stenosis and the repercussions on the upper genital tract.
Declaration of Competing interest
The authors report no declarations of interest.
Funding
There are no funding sources to be declared.
Ethical approval
Ethics approval has been obtained to proceed with the current study. Consent to participate not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
KE made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; he has been involved in drafting the manuscript and revising it critically for important intellectual content. AL made substantial contributions to interpretation of data and she has been involved in drafting the manuscript and revising it critically for important intellectual content. AB and AL made substantial contributions to conception and design and acquisition of data; they has been involved in drafting the manuscript.
Registration of research studies
N/A.
Guarantor
Corresponding author: Dr Kamal el Moussaoui.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgements
None.
References
- 1.Saks E.K., Vakili B., Steinberg A.C. Primary amenorrhea with an abdominal mass at the umbilicus. J. Pediatr. Adolesc. Gynecol. 2009;22(1):e1–3. doi: 10.1016/j.jpag.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 2.Breech L.L., Laufer M.R. Müllerian anomalies. Obstet. Gynecol. Clin. North Am. 2009;36(1):47–68. doi: 10.1016/j.ogc.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 3.Williams C.E., Nakhal R.S., Hall-Craggs M.A., Wood D. Transverse vaginal septae: management and long-term outcomes. BJOG. 2014;121(13):1653–1658. doi: 10.1111/1471-0528.12899. [DOI] [PubMed] [Google Scholar]
- 4.Deligeoroglou E., Iavazzo C., Sofoudis C., Kalampokas T., Creatsas G. Management of hematocolpos in adolescents with transverse vaginal septum. Arch. Gynecol. Obstet. 2012;285(04):1083–1087. doi: 10.1007/s00404-011-2114-4. [DOI] [PubMed] [Google Scholar]
- 5.Rock J.A. Surgery for anomalies of the müllerian ducts. In: En Rock J.A., Thompson J.D., editors. Telinde’s Operative Gynecology. 8th ed. Lippincott-Raven; Philadelphia: 1997. pp. 687–729. [Google Scholar]
- 6.Rock J.A., Zacur H.A., Dlugi A.M., Jones H.W., Jr., TeLinde R.W. Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet. Gynecol. 1982;59(04):448–451. 8 Deligeoroglou. [PubMed] [Google Scholar]
- 7.Paredes Esteban R.M., Ocaña Losa J.M., Pizarro de Celis F., Gutiérrez Cantó M. Síndrome de McKusick-Kaufman: Aportación de cinco nuevos casos, incluido un varón. An. Esp. Pediatr. 1996;44(5):493–495. [PubMed] [Google Scholar]
- 8.Wang W., Chen M.H., Yang W., Hwang D.L. Imperforate hymen presenting with chronic constipation and lumbago: report of one case. Acta Paediatr. Taiwan. 2004;45:340–342. [PubMed] [Google Scholar]
- 9.Dane C., Dane B., Erginbas M., Cetin A. Imperforate hymen—a rare cause of abdominal pain: two cases and review of the literature. J. Pediatr. Adolesc. Gynecol. 2007;20:245–247. doi: 10.1016/j.jpag.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Miller R., Breech L. Surgical correction of vaginal anomalies. Clin. Obstet. Gynecol. 2008;51:223–236. doi: 10.1097/GRF.0b013e31816d2181. [DOI] [PubMed] [Google Scholar]
- 11.Dennie J., Pillay S., Watson D., Grover S. Laparoscopic drainage of hematocolpos: a new treatment option for the acute management of a transverse vaginal septum. Fertil. Steril. 2010;94(05):1853–1857. doi: 10.1016/j.fertnstert.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 12.Williams C.E., Nakhal R.S., Hall-Craggs M.A. Transverse vaginal septae: management and long-term outcomes. BJOG. 2014;121(13):1653–1658. doi: 10.1111/1471-0528.12899. [DOI] [PubMed] [Google Scholar]
- 13.Garcia R.F. Z-plasty for correction of congenital transferse vaginal septum. Am. J. Obstet. Gynecol. 1967;99(08):1164–1165. doi: 10.1016/0002-9378(67)90357-2. [DOI] [PubMed] [Google Scholar]
- 14.Blanton E.N., Rouse D.J. Trial of labor in women with transverse vaginal septa. Obstet. Gynecol. 2003;101(5 Pt 2):1110–1112. doi: 10.1016/s0029-7844(02)02623-6. [DOI] [PubMed] [Google Scholar]
- 15.van Bijsterveldt C., Willemsen W. Treatment of patients with a congenital transversal vaginal septum or a partial aplasia of the vagina. The vaginal pull-through versus the push-through technique. J. Pediatr. Adolesc. Gynecol. 2009;22(03):157–161. doi: 10.1016/j.jpag.2008.02.008. [DOI] [PubMed] [Google Scholar]
- 16.Layman L.C., McDonough P.G. Management of transverse vaginal septum using the Olbert balloon catheter to mobilize the proximal vaginal mucosa and facilitate low anastomosis. Fertil. Steril. 2010;94(06):2316–2318. doi: 10.1016/j.fertnstert.2009.12.061. [DOI] [PubMed] [Google Scholar]
- 17.Loscalzo I.L., Catapano M., Loscalzo J., Sama A. Imperforate hymen with bilateral hydronephrosis: an unusual emergency department diagnosis. J. Emerg. Med. 1995;13(03):337–339. doi: 10.1016/0736-4679(95)00008-x. [DOI] [PubMed] [Google Scholar]
- 18.Rink Richard C., Martin Kaefer. Surgical management of disorders of sexual differentiation, cloacal malformation and other abnormalities of the genitalia in girls. In: Wein A.J., editor. Campbell-Walsh Urology. 9th ed. Saunders; Philadelphia: 2007. [Google Scholar]
- 19.Ridhima Gupta, Bozzay Joseph D., Williams David L., DePond Robert T., Gantt Pickens A. Management of recurrent stricture formation after transverse vaginal septum excision. Case Rep. Obstet. Gynaecol. 2015 doi: 10.1155/2015/975463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rock J.A., Zacur H.A., Dlugi A.M., Jones H.W., Jr., TeLinde R.W. Pregnancy success following surgical correction of imperforate hymen and complete transverse vaginal septum. Obstet. Gynaecol. 1982;59(4):448–451. [PubMed] [Google Scholar]
- 21.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., pour le groupe SCARE The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;(60):132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.