Abstract
Introduction
Most intraocular T-cell lymphomas arise from metastatic source. We are reporting a rare case of intraocular T-cell lymphoma masquerading as pseudo-hypopyon and vitritis. The eye involvement proved to represent a metastatic spread from a co-existing adrenal T-cell lymphoma, which was discovered after the initial ophthalmic presentation.
Presentation of case
Our patient was a 71-year-old Saudi man, who was admitted for workup of anemia and weight loss. He also noticed a gradual, painless decline in his vision of both eyes, for which he was referred to the ophthalmology unit. Ocular examination revealed left eye 3 mm pinkish hypopyon. A diagnosis of T-cell lymphoma was made based on careful microscopic examination of the left aqueous fluid, immunohistochemical (IHC) and Flow cytometry analysis. Computerized tomography showed a large invasive left adrenal mass, which has proven to be a primary adrenal lymphoma with multiple metastasis including the intraocular involvement.
Discussion
Primary intraocular lymphoma is the most common lymphoma in the eye. Intraocular T-cell lymphoma is rare and is mostly metastatic. On the other hand, primary adrenal lymphoma (especially T-cell lymphoma) is also rare. There are only 5 cases of primary adrenal lymphoma, two of which, resulted in eye metastasis similar to our case. Primary adrenal lymphoma is known to be aggressive. Our patient eventually passed away.
Conclusion
This report stresses the importance of referring patients with systemic lymphoma to an ophthalmologist to be evaluated for ocular involvement. Even though intraocular metastatic adrenal T cell lymphoma is rare, high clinical suspicion in patients who are presenting with pinkish hypopyon in the presence of other constitutional symptoms is essential.
Keywords: Intraocular T-cell lymphoma, Adrenal, Uveitis, Masquerade syndrome, Hypopyon
Highlights
-
•
Intraocular metastatic adrenal T-cell lymphoma is a rare condition.
-
•
Diagnosis is essentially histopathological and can be made through aqueous tap.
-
•
We report the rare occurrence of metastatic adrenal T-cell lymphoma to the eye.
-
•
Intraocular lymphoma may present with pinkish hypopyon as a masquerade syndrome.
1. Introduction
Primary intraocular lymphoma is the most common lymphoma in the eye, in which the most common type is B-cell lymphoma [1]. Intraocular non-B cell type is rare. It accounts only for 1–3% of all lymphoproliferative lesions in the eye [2]. Most intraocular T-cell lymphomas arise from metastatic systemic source and are known to have poor prognosis [1,3]. Only few case reports and series have been described [4,5]. Intraocular manifestations of metastatic T-cell lymphoma are rare [6]. It mostly presents with non-granulomatous anterior uveitis and vitritis [7]. Metastasis of systemic lymphomas usually occurs through hematogenous spread to the uvea [1]. Other ocular manifestations include, yellowish subretinal infiltrates and posterior uveitis with or without optic nerve involvement [6]. Primary adrenal lymphoma (PAL) is an extremely aggressive and rare in which majority of them present as a large B-cell lymphoma. Adrenal T-cell lymphoma is very rare [8,9]. Up to our knowledge, only 5 cases of PAL were reported, with only two cases of eye metastasis. This is a rare case of intraocular metastatic presumed adrenal T-cell lymphoma. This case report has been prepared in compliance with the updated SCARE 2018 criteria [10]. A general written informed consent was taken from the patient, which includes permission for anonymous use of information and photos for the purpose of publication.
2. Case presentation
A 71-year-old Saudi man, known case of rheumatic heart disease, hypertension and chronic kidney disease, was admitted for workup of anemia and weight loss. Four months prior to admission, he noticed a gradual, painless decline in his vision of both eyes. He did not report any history of eye redness, photophobia, floaters, flashes or scotoma. There was no previous history of eye trauma or surgery. During systemic review of the patient, he reported history of raw milk ingestion. The patient was given an informed consent to have a full medical care and treatment including surgical management and chemotherapy treatment and was referred to the ophthalmologist.
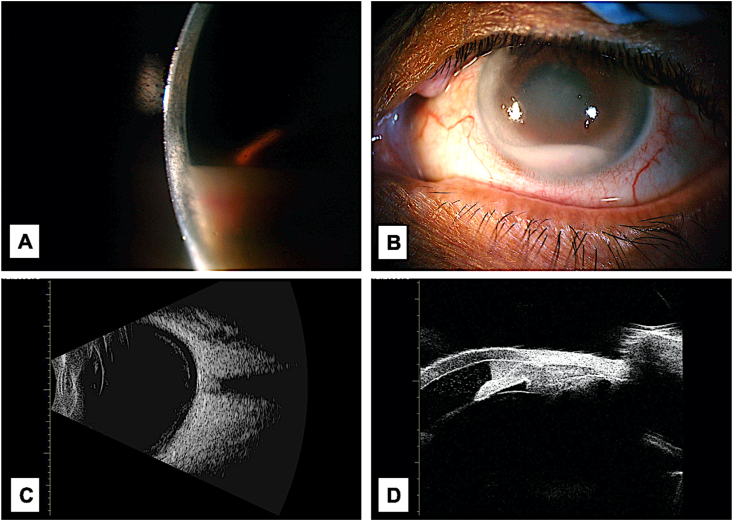
His ophthalmic examination revealed visual acuity measuring 6/200 on the right and 20/200 on the left, while his intraocular pressure was 13 and 15 mmHg in both eyes. His external examination and extra-ocular movements were normal. Pupils were both reactive to light, with no relative afferent pupillary defect. Slit lamp examination of the right eye showed deep and quite anterior chamber (AC). Left eye exam showed a 3 mm pinkish hypopyon, iris pigments on the surface of the lens, and irregular pupil with posterior synechiae (Fig. 1a & b). A visually significant nuclear sclerotic cataract along with multiple corneal scars in both eyes were obscuring the dilated fundus exam.
Fig. 1.
A: Left eye slit lamb examination showing a 3 mm pinkish hypopyon. B: Another clinical photo of the left eye showing the hypopyon, hazy view of the irregular pupil with posterior synechiae and iris pigments on the surface of the lens. C: Ultrasound Biomicroscopy of the left eye indicating flat retina, no vitritis or subretinal infiltrate in the posterior cavity of the left eye. D: Ultrasound Biomicroscopy showing floating cells in the anterior chamber and hypopyon in the same eye.
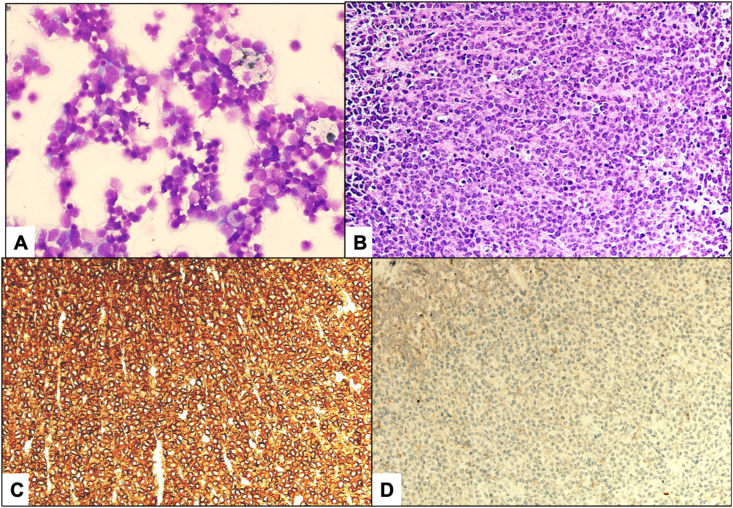
Extensive systemic work-up for infectious and inflammatory etiologies of possible pan-uveitis was ordered by his treating ophthalmologist. Three sets of blood, sputum and urine culture were all negative. Repeated cultures for acid fast bacilli were negative. Brucella titer was negative for brucellosis infection. B-Scan ultrasonography showed flat retina, no vitritis or subretinal infiltrate (Fig. 1c). Fundus photos and fundus Fluorescein angiography were done and had poor view due to the very dense cataract. Ultrasound Biomicroscopy showed floating cells in the AC and hypopyon (Fig. 1d). The ophthalmologist who has experience in treating uveitis cases started the patient on prednisolone acetate 1% drops 4 times a day and cyclopentolate 0.5% drops 3 times a day. The patient underwent left cataract extraction and intraoperative diagnostic paracentesis successfully by an experienced anterior segment ophthalmic surgeon. Microscopic examination of the left aqueous fluid showed atypical small to medium lymphoid cells with blastoid morphology with immunohistochemical (IHC) staining consistent with T-cell lymphoma (Fig. 2a). Flow cytometry analysis of the aqueous fluid demonstrated a positive lymphocytic subpopulation of CD5, CD3, CD2, CD8 and CD56 markers, but aberrant loss of CD4 and CD7 and no expression of CD10 and CD34. The alpha and beta T-cell receptor (TCR) were positive but gamma was negative. The overall features were consistent with T-cell lymphoma. On postoperative follow up, his visual acuity dropped to counting fingers at 3 feet in both eyes. Intraocular pressure of both eyes was normal. Anterior segment examination showed reforming pinkish hypopyon in the left AC and IOL was in place. Dilated fundus exam of the right eye showed hazy view due to cataract. Left eye fundus exam showed whitish retinal infiltrate in multiple areas.
Fig. 2.
A: Microscopic appearance of the left aqueous fluid obtained by paracentesis at the time of surgery showing atypical lymphoid cells with blastoid morphology (Original magnification X 400 Hematoxylin and Eosin). B: The adrenal mass biopsy from the patient showing infiltration by atypical small to medium lymphoid cells with blastoid features (Original magnification X 200 Hematoxylin and Eosin). C: T-lymphocytes showing diffuse strong expression with CD3 marker (Original magnification X 200 CD3). E: The non-B-lymphocytes showing lack of expression with CD20 marker (Original magnification X 200 CD20).
Meanwhile, multiple radiologic investigations were ordered by the oncology team. Chest x-ray showed signs of pulmonary edema otherwise was unremarkable for tuberculosis or sarcoidosis. Liver ultrasound showed heterogeneous liver with no definite mass lesion noted. Computed tomography of chest, abdomen, and pelvis (CAP) showed large heterogeneous left adrenal mass, with features that are suspicious for invasion, and consistent with malignancy. No other suspicious lesions were found at that time. Ultrasound guided biopsy was taken from the adrenal mass and microscopic examination, which showed infiltration with atypical small to medium lymphoid cells with blastoid features similar to the intraocular involvement (Fig. 2b). The tumor cells strongly expressed T-lymphocytes marker: CD3 while failed to express the B-lymphocytic marker: CD20 (Fig. 2c and d). Along with other extensive IHC battery the diagnosis of T-cell lymphoma was further confirmed. The haemato-oncology team were consulted to start treatment for his adrenal mass and retinal infiltrate. Lumber puncture and Positron Emission Tomography (PET) scan of the brain and orbit to rule out central nervous system (CNS) involvement was also recommended.
The disease extent and process were explained to the patient who agreed on the chemotherapy regimen for T-cell lymphoma and was treated with cyclophosphamide, oncovin [vincristine], and prednisolone (CVP). He was also further investigated by the treating oncology team in the same tertiary care hospital. Lumbar puncture was done, and cerebrospinal fluid was negative for malignancy. Bone marrow biopsy was also negative for malignancy.
PET scan of the brain and orbit showed increase uptake in right nasal and ethmoidal sinuses, most likely lymphoma related. PET scan of the pelvis was also done and showed high uptake in scrotum and testicles and the metastatic involvement of this area by lymphoma was further supported by ultrasonography of scrotum and testicles. Therefore, local radiotherapy to orbits and testicles was added to his treatment plan. The fact that the lymphoproliferative disease was considered to be disseminating was challenging and the guarded prognosis was explained to the patient. However, chemotherapy was continued.
After two cycles of chemotherapy, the patient's condition started deteriorating and he developed atrial fibrillation. The patient was stabilized and transferred to Medical Intensive Care Unit with regular ophthalmic bedside follow up visits. Few days later, he collapsed, became unresponsive, and had impalpable pulse. Cardiopulmonary resuscitation and Advanced trauma life support protocols were started. The patient was intubated, and deeply comatose, with a Glasgow Coma scale (GCS) of 6/15. Furthermore, he developed sepsis, which was treated with proper antibiotics. Meanwhile, his chemotherapy and radiation were kept on hold because of his clinical condition. The patient continued to deteriorate, GCS became 3/15, and he was put on Do not attempt resuscitation and he eventually passed away.
3. Discussion
Adrenal T-cell lymphoma is a rare disease that is known to be more common in men above 60 years old [11]. It mostly affects both adrenal glands in 60%–75% of the cases [8,9]. The main clinical symptoms are lumber pain, fever, and weight loss [8,12]. On the other hand, most metastatic intraocular lymphomas are B-cell in origin. Intraocular T-cell metastatic lymphoma is very rare and very difficult to be distinguished clinically from B cell lymphoma [13,14]. Nearly, all patients have vitreoretinal involvement [14]. Metastatic B-cell lymphoma usually have uveal involvement, in contrast to metastatic T-cell lymphoma, which usually presents with anterior uveitis (71%) and subretinal/retinal infiltrate (57%) [14]. Only few case reports and series in the English-written literature have documented this presentation [4,5].
In general, metastases to the eye and ocular adnexa from T-cell lymphomas are uncommon relative to B-cell lymphomas [[15], [16], [17], [18]]. The histologic appearance of the aqueous tap fluid and the flowcytometry analysis of the aqueous fluid in our patient demonstrated overall features consistent with T-cell lymphoma. However, in view of his co-existing large adrenal T-cell lymphoma, the eye involvement was not considered to be a primary intraocular lymphoma.
Paracentesis was very helpful in reaching the diagnosis, which is of paramount importance since some patients can solely present to the ophthalmologist with masquerade syndrome and pseudo-hypopyon. This is also helpful in the absence of a clear view to the posterior pole because of lens opacities such as in our case. However, after the cataract extraction, the subretinal infiltrates caused by the intraocular metastatic T-cell lymphoma became apparent. This additional new finding was helpful to support his involvement by intraocular T-cell rather than B-cell lymphoma, which usually spreads to the uveal tissue [19].
Sfaxi reported a case of 33 years old male with bilateral adrenal T-cell lymphoma who presented with weight loss, fever and vomiting. No metastasis was detected. Patient was successfully treated with chemotherapy [20]. Pimentel reported as well a 42-years-old male with large, bilateral adrenal extra-nodal T cell lymphoma who same symptoms as the previous patient. CSF was positive for malignant cell and metastasis to rectus muscle sheath of both eyes. Patient was expired after 4 months [21]. Bommannan reported a case of 26 years old male with bilateral adrenal T cell lymphoma who presented with weight loss and blurred vision. Aqueous aspirate from the pseudo-hypopon of the right eye showed infiltration of lymphoid cells. Patient expired due to intra-abdominal hemorrhage [22].
Unfortunately, the patient died, and he could not share his perspective for treatment and his disease prognosis. Also, autopsy was not done due to cultural issues and hospital policy.
4. Conclusion
Intraocular metastatic primary adrenal T-cell lymphoma is rare. The diagnosis is essentially histological. It is desirable to obtain a biopsy early on in the diagnostic workup of adrenal masses. To our knowledge, we are the first in Saudi Arabia to report intraocular metastatic T-cell lymphoma arising from the adrenal gland. Patients with systemic lymphoma should be referred to an ophthalmologist to be evaluated for intraocular and periocular involvement. High clinical suspicion in patients presenting with pinkish hypopyon is required, especially if associated with other constitutional symptoms such as chronic anemia and weight loss.
Declaration of competing Interest
The authors have no conflict of interest or financial disclosures in relation to this work.
This case report was prepared in accordance with the ethical standards of the human ethics committee and with the Helsinki Declaration. A general informed written consent was taken from the patient, which includes permission for anonymous use of photos and reporting.
The authors have no conflict of interest or financial disclosures in relation to this work.
Funding
This Case report did not receive any funding from any resource.
Ethical approval
Case reports do not require Ethical approval in our institution.
This case report was prepared in accordance with the ethical standards and the Helsinki Declaration. No trial of new drugs or therapy is applicable in this case.
Consent
A written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal upon request.
Author contribution
First author: Review of chart, literature review and first draft of the case report.
Second author: Clinical diagnosis of the case and manuscript review.
Third author: Histopathological examination and final tissue diagnosis. Fourth author: Histopathological review of slides. Fifth author & Sixth author: Consultation to confirm the clinical retinal findings of the patient. Seventh author: Senior pathologist, taking images, and overall review for editing of the manuscript as the corresponding author.
Registration of research studies
-
1.
Name of the registry: This is a case report, which does not require a registry.
-
2.
Unique Identifying number or registration ID:
-
3.
Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Dr. Hind Manaa Alkatan.
Provenance and peer review
Not commissioned, externally peer reviewed.
Acknowledgements
The authors would like to thank the manpower and facilities support provided by King Faisal Specialist Hospital and Research Centre.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.11.066.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Cao X., Shen D., Callanan D.G., Mochizuki M., Chan C.C. Diagnosis of systemic metastatic retinal lymphoma. Acta Ophthalmol. 2011;89:e149–e154. doi: 10.1111/j.1755-3768.2009.01797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cimino L., Chan C.C., Shen D., Masini L., Ilariucci F., Masetti M., Asioli S., Sartori A., Cappuccini L. Ocular involvement in nasal natural killer T-cell lymphoma. Int. Ophthalmol. 2009;29:275–279. doi: 10.1007/s10792-008-9220-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu L.L., Yuen H.K., Chan C.K., Lai T.Y., Chan J.K., Cheuk W. Panuveitis as an initial presentation of extranodal NK/T-cell lymphoma. Leuk. Lymphoma. 2009;50:648–650. doi: 10.1080/10428190802713539. [DOI] [PubMed] [Google Scholar]
- 4.Alqahtani A., Touitou V., Cassoux N. More than a masquerade syndrome: atypical presentations of vitreoretinal lymphomas. Ocul. Immunol. Inflamm. 2014;22:189–196. doi: 10.3109/09273948.2013.835427. [DOI] [PubMed] [Google Scholar]
- 5.Foester H.C. Mycosis fungoides with intraocular involve- ment. Trans. Am. Acad. Ophthalmol. Otolaryngol. 1960;64:308–313. [PubMed] [Google Scholar]
- 6.Goeminne J.C., Brouillard A., Jaumain P., Ferrant A., Snyers B., De Potter P. Bilateral granulomatous panuveitis as initial presentation of diffuse systemic T cell lymphoma. Ophthalmologica. 1999;213:323–326. doi: 10.1159/000027447. [DOI] [PubMed] [Google Scholar]
- 7.Lin T.C., Lin P.Y., Wang L.C., Chen S.J., Chang Y.M., Lee S.M. Intraocular involvement of T-cell lymphoma presenting as inflammatory glaucoma, neurotrophic keratopathy, and choroidal detachment. J. Chin. Med. Assoc. 2014;77(7):385–388. doi: 10.1016/j.jcma.2014.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Tsukahara T., Takasawa A., Murata M., Okumura A., Nakayama M., Sato N., Hasegawa T. NK/T-cell lymphoma of bilateral adrenal glands in a patient with pyothorax. Diagn. Pathol. 2012;7:114. doi: 10.1186/1746-1596-7-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rashidi A., Fisher S.I. Primary adrenal lymphoma: a systematic review. Ann. Hematol. 2013;92:1583–1593. doi: 10.1007/s00277-013-1812-3. [DOI] [PubMed] [Google Scholar]
- 10.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 11.Salvatore J.R., Ross R.S. Primary bilateral adrenal lymphoma. Leuk. Lymphoma. 1999;34(1–2):111–117. doi: 10.3109/10428199909083386. [DOI] [PubMed] [Google Scholar]
- 12.Rizzo Christopher, James Camilleri David, Betts Alexandra, Gatt Andre’, Fava Stephen. Primary bilateral non-hodgkin’s lymphoma of the adrenal gland presenting as incidental adrenal masses. Case Reports in Medicine. 2015;2015 doi: 10.1155/2015/620381. 6 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santhosh S., Mittal B.R., Shankar P., Kashyab R., Bhattacharya A., Singh B., Das A., Bhansali A. 18)F-FDG PET/CT in bilateral primary adrenal T-cell lymphoma. Hellenic J. Nucl. Med. 2011;14:166–167. [PubMed] [Google Scholar]
- 14.Levy-Clarke G.A., Greenman D., Sieving P.C., Bymes G., Shen D., Nussenblatt R., Chan C.C. Ophthalmic manifestations, cytology, immunohistochemistry, and molecular analysis of intraocular metastatic T-cell lymphoma: report of a case and review of the literature. Surv. Ophthalmol. 2008;53:285–295. doi: 10.1016/j.survophthal.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coupland S.E., Foss H.D., Assaf C., Auw-Haedrich C., Anastassiou G., Anagnostopoulos I., Hummel M., Karesh J.W., Lee W.R., Stein H. T-cell and T/natural killer-cell lymphomas involving ocular and ocular adnexal tissues: a clinicopathologic, immunohistochemical, and molecular study of seven cases. Ophthalmology. 1999;106:2109–2120. doi: 10.1016/S0161-6420(99)90492-X. [DOI] [PubMed] [Google Scholar]
- 16.Jensen O.A., Johansen S., Kiss K. Intraocular T-cell lymphoma mimicking a ring melanoma. First manifestation of systemic disease. Report of a case and survey of the literature. Graefes Arch. Clin. Exp. Ophthalmol. 1994;232:148–152. doi: 10.1007/BF00176784. [DOI] [PubMed] [Google Scholar]
- 17.Levy-Clarke G.A., Greenman D., Sieving P.C., Byrnes G., Shen D., Nussenblatt R., Chan C.C. Ophthalmic manifestations, cytology, immunohistochemistry, and molecular analysis of intraocular metastatic T-cell lymphoma: report of a case and review of the literature. Surv. Ophthalmol. 2008;53:285–295. doi: 10.1016/j.survophthal.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saga T., Ohno S., Matsuda H., Ogasawara M., Kikuchi K. Ocular involvement by a peripheral T-cell lymphoma. Arch. Ophthalmol. 1984;102:399–402. doi: 10.1001/archopht.1984.01040030317027. [DOI] [PubMed] [Google Scholar]
- 19.Ozcan A.A., Paydas S., Soylu M., Yavuz S. Bilateral choroidal infiltration from indolent non-Hodgkin's lymphoma: a rapid course with poor prognosis. Leuk. Lymphoma. 2005;46:615–617. doi: 10.1080/10428190500032554. [DOI] [PubMed] [Google Scholar]
- 20.Sfaxi M., Bouzouita A., Bouasker I. Primary bilateral adrenal T-cell lymphoma. A case report rarer than B-cell lymphoma. Ann Endocrinol (Paris) 2008;69:249–253. doi: 10.1016/j.ando.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Pimentel M., Johnston J.B., Allan D.R., Greenberg H., Bernstein C.N. Primary adrenal lymphoma associated with adrenal in- sufficiency: a distinct clinical entity. Leuk. Lymphoma. 1997;24:363–367. doi: 10.3109/10428199709039025. [DOI] [PubMed] [Google Scholar]
- 22.Bommannan K., Sachdeva M.U., Sekar A., Kumar R., Dey P. Primary adrenal T-cell lymphoma in a young adult presented with pseudo-hypopyon: a case report and literature review. 2017 Sep;52(3):227–229. doi: 10.5045/br.2017.52.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.