Abstract
Objective:
To assess U.S. pediatricians’ preparedness, motivation, and barriers related to educating parents about corporal punishment (CP) and effective child discipline.
Methods:
A random sample of 1,500 pediatricians was drawn from a nationwide database in the U.S. A self-administered questionnaire was sent via mail in 2016. The response rate (53%; n = 787) was maximized via repeated survey mailings and use of cash incentives.
Results:
The majority of respondents were White (69%), female (59%) and were members of the American Academy of Pediatrics (85%). Most pediatricians felt somewhat prepared to advise parents about child discipline, particularly CP, and perceived their colleagues to be slightly less prepared than themselves. Although most (72%) respondents believed it was “extremely/very” likely that parents valued their advice about child discipline, only 36% believed parents were “extremely/very” likely to follow their advice. Most respondents were highly motivated to participate in activities designed to change norms regarding CP. The most common strategy pediatricians identified for improving child behavior was being consistent with rules (71%). Perceived barriers to providing child discipline advice to parents included lack of time (90%), lack of insurance reimbursement (48%) and lack of training and educational resources (47%).
Conclusions:
Pediatricians are a key source of professional advice for parents about how to discipline children safely. Given this, along with strong approval and use of CP in the U.S. and its harm for children, the current findings suggest a strong need for pediatricians to receive additional training on how to advise parents about child discipline along with removal of barriers to providing such advice.
Keywords: corporal punishment, child discipline, preparedness, norms, child physical abuse
A large body of empirical evidence has emerged regarding the harms of corporal punishment (CP) including risk for child physical abuse, effects on brain development, mental and emotional health problems in childhood,1 and mental and physical health problems in adulthood.2–5 CP, also known as physical discipline or punishment, and spanking, among other terms, is used to correct or punish a child’s behavior and includes the use of physical force intended to cause pain or discomfort to the child without injury.6 The effects of CP on mental health problems are on the same scale as other adverse childhood experiences including physical and emotional abuse.2 Despite substantial evidence indicating the harmful effects of CP, there is still widespread approval of CP in the U.S. with approximately 71% of adults agreeing that CP use is sometimes necessary to discipline a child.7 Further, although there has been a decline in the use of CP nationally and rates vary regionally, more than 60% of parents report using CP with their children by the time they have turned 5 years of age.8,9 The harmful effects of CP, combined with its widespread approval and use, highlight CP as an important public health issue to address. Therefore, potential avenues for interventions to shift norms regarding CP use are needed.
The Theory of Planned Behavior posits that perceived norms of influential groups regarding a behavior are strong predictors for attitudes toward and use of the behavior.10 For example, parental attitudes toward CP and use of CP are directly linked to their perceived norms regarding CP of family, friends, neighbors, and family service providers.11–13 Specifically, perceived approval of CP by pediatricians is a strong predictor for parental attitudes supportive of CP.14 Pediatricians have also been identified by parents as an extremely credible and influential source of advice regarding parenting and child discipline.15,16
Recent findings from a representative sample of U.S. pediatricians demonstrated that the majority of pediatricians (79%) disapprove of CP use and believe that it is harmful for children.17 However, pediatricians perceived their colleagues as having slightly more positive attitudes toward CP compared to their own attitudes. Further, over 75% of pediatricians identified no positive expected outcomes of CP use and instead identified several negative expected outcomes.17 Compared to earlier studies of medical professionals’ attitudes regarding CP use, this study reflects a meaningful trend toward less approval and support of CP use.18–20 Additionally, the release of a policy statement in 2018 by the American Academy of Pediatrics strongly condemning CP use,21 and release of training resources for pediatricians to engage with parents regarding CP use,22 have potentially influenced pediatricians’ approval ratings and support of CP since their emergence.
While pediatricians serve as a promising entry point for shifting parental norms regarding CP, there is a need to examine the specific training gaps and barriers for pediatricians to more effectively provide advice regarding child discipline to parents. Further, it would be useful to understand pediatricians’ motivation to help change norms regarding CP amongst their colleagues and with parents. The current study is designed to examine U.S. pediatricians’: 1) preparedness for and perceived value of addressing child discipline with parents, 2) perceptions of their colleagues’ preparedness for addressing child discipline with parents, 3) motivations to change norms regarding CP with parents and colleagues, 4) beliefs about various discipline strategies, and 5) perceived barriers to educating parents about safe child discipline. Examining these key variables will allow for development of targeted training interventions to provide pediatricians with the additional skills and tools needed to effectively advise parents about child discipline.
METHODS
Study Procedure
A national database of U.S. physicians purchased from SK&A Information (now IQVIA) was utilized to draw a random sample of pediatricians for the current study. The inclusion criteria for the sample frame included physicians who: 1) indicated pediatrics as their primary specialty, 2) currently practiced in the U.S., and 3) had a valid mailing address. In February 2016, a random sample of 1,500 records was pulled from pediatricians in the sampling frame (N=33,476). The University of Wisconsin Survey Center (UWSC) acquired the sample and directed mailings of surveys and data collection.
Surveys were mailed from March to May of 2016, with data collection finalized on June 2016. UWSC conducted four mailings to maximize survey response rates: 1) a full mailing (including a cover letter, a questionnaire, a cash incentive, and a business reply envelope) to all 1,500 participants, 2) a postcard reminder sent one week later (N=1500), 3) a full mailing at one month (N=947), and 4) a final full mailing seven weeks (N=757) later to participants who had not responded. Instructions providing a description of the survey, the voluntary and confidential nature of the survey, and how to return responses were included in the full mailings.
The current study was approved by Tulane University’s Institutional Review Board. Participants received anywhere from $5 to $20 in incentives across two survey mailings, for total of $17,530 in incentive costs. (Note: findings from the incentive level experiment are reported elsewhere.23) All responses remained anonymous. No personally identifying information was collected. In total, 787 respondents completed the survey yielding a response rate of 53%. The response rate is similar to the average rate of 50% reported in a meta-analysis of healthcare professional surveys.24
Measures
Instructions were given to participants asking them to respond to questions as follows: “Please rate the following statements with regard to advising parents about using discipline that does not involve spanking or hitting a child with a hand or an object.” All answers were scored on a 5-point Likert scale ranging from 1=not at all, 2=a little, 3=somewhat/moderately, 4=very, to 5= extremely, then averaged so that final scores ranged from 1 to 5.
Preparedness for and value of advising parents about child discipline.
Professional preparedness beliefs included: (1) How strongly do you believe that this is part of your job? (2) How well-trained do you feel you were to provide such advice? (3) How confident do you feel about your ability to provide such advice? and (4) How supported do you feel in your workplace to provide such advice? Perceived value beliefs included: (1) Do you give a high priority to providing such advice? (2) How highly do you think parents value such advice when you provide it? and (3) How likely do you think parents are to follow such advice when you provide it?
Perceived professional norms of preparedness about advising parents about child discipline.
Respondents were asked four questions regarding their perceived professional environment on this topic: (1) How well-trained do you think most people in your profession are to provide advice about using discipline that does not involve spanking or hitting a child with a hand or an object? (2) How confident do you think most people in your profession are to provide advice about using discipline that does not involve spanking or hitting a child with a hand or an object? (3) Was learning how to prevent child physical abuse before it occurs emphasized in your professional training or education? As a point of comparison, we also asked, “Was learning how to respond to child physical abuse cases after they occur emphasized in your professional training or education?”
Motivation to change norms regarding corporal punishment of children.
Respondents were asked their level of motivation to participate in seven items: (1) Learn more about research findings on the effects of spanking on children, (2) Talk to parents about using discipline techniques that do not involve spanking, (3) Challenge parents’ viewpoints that support the use of spanking, (4) Challenge colleagues’ viewpoints that support the use of spanking, (5) Work with your employer to change policies related to the use of spanking (e.g., no hit zones), (6) Discuss with your colleagues discipline techniques that do not involve spanking, and (7) Learn about ways you can best intervene with parents when they spank children in your presence.
Beliefs about alternative child discipline strategies.
Participants were asked: “How effective are the following disciplinary strategies at improving a child’s behavior, assuming age-appropriate application?” regarding fifteen child discipline strategies. The fifteen items included: (1) being consistent with rules, (2) praising, (3) applying awareness of a child’s developmental capabilities, (4) redirection, (5) rewards for good behavior, (6) setting future expectations, (7) time out, (8) removing privileges, (9) explanation of rules, (10) warning, (11) grounding of adolescents, (12) shaming, (13) yelling, (14) spanking, and (15) assigning chores as punishment.
Statistical Analysis
All analyses were conducted using STATA 15. Summary and descriptive statistics, including frequency distributions, means, and standard deviations, were conducted. Bivariate analysis including a correlation matrix to assess collinearity amongst the main variables of interest. Multivariable linear regression analyses were conducted to determine the association between preparedness and perceived professional norms of preparedness about advising parents about child discipline, and motivations to change norms regarding CP and key respondent characteristics. In linear regression, the unstandardized beta coefficient (B) is the degree of change in the outcome variable for every 1-unit change in the predictor variable. The standard error (SE B) is similar to the standard deviation for a mean, with a larger number indicating greater spread of points from the regression line. The standardized beta coefficient (β) ranges from −1 to 0 or 0 to 1 depending on the direction of the relationship between the outcome and predictor, with a value closer to −1 or 1 indicating a stronger relationship. A p-value <0.05 was used to define statistically significant associations.
RESULTS
Respondent characteristics are presented in Table 1. All survey respondents were pediatricians, and the majority were members of the American Academy of Pediatrics (85.0%). All regions of the U.S. were represented including the Northeast (31.0%), the South (28.0%), the West (23.4%), and the Midwest (15.3%). Racial and ethnic demographics included White (69.3%), Asian (14.9%), Hispanic/White (6.5%), Black (3.4%), and other (4.2%). Most respondents were female (59.1%) with an average age of 51 years (SD = 11.3; range 19–84). Most participants had fifteen years or more of experience (66.2%) and 12% had completed a post-residency program. The majority identified as primary care clinicians (93.8%) as compared to specialists (5.3%). Most identified as general pediatricians (92%) as compared to family practice, internal medicine/pediatrics, or another field. Participants reported seeing an average of 86 children during a typical week, with a mean number of 37.4 child wellness visits per week. Most (97.1%) reported that the largest portion of children seen in their practice were children less than 6 years of age. Finally, less than half responded they were “rarely” spanked or hit for discipline (45.1%). The rest reported being “sometimes” (28.0%), “never” (18.3%), or “often” hit (6.9%).
Table 1.
Respondent Characteristics (n=787)
| n | % | |
|---|---|---|
| Gender | ||
| Female | 465 | 59.1 |
| Male | 315 | 40.0 |
| Race | ||
| White | 545 | 69.3 |
| Black | 27 | 3.4 |
| Asian | 117 | 14.9 |
| Hispanic-identified | 51 | 6.5 |
| Other | 33 | 4.2 |
| Region of U.S. | ||
| Northeast | 245 | 31.1 |
| Midwest | 120 | 15.2 |
| West | 184 | 23.4 |
| South | 222 | 28.2 |
| Years of Experience | ||
| <15 yrs | 259 | 32.9 |
| 15–24 yrs | 223 | 28.3 |
| 25+ yrs | 298 | 37.8 |
| Spanked as Child | ||
| Never | 144 | 18.3 |
| Rarely | 355 | 45.1 |
| Sometimes | 220 | 28.0 |
| Often | 54 | 6.9 |
| Type of Practice | ||
| Private Practice | 437 | 55.5 |
| Community-Based Practice | 209 | 26.6 |
| Hospital | 91 | 11.6 |
| Other | 43 | 5.5 |
| Type of Pediatrician | ||
| Primary care | 738 | 93.8 |
| Specialist | 42 | 5.3 |
| Area of Pediatrics | ||
| General pediatrics | 724 | 92.0 |
| Other | 56 | 8.0 |
| Member of AAP | ||
| Yes | 665 | 85.0 |
| No | 107 | 13.6 |
| Largest age group of children seen | ||
| <6 years old | 764 | 97.1 |
| >6 years old | 6 | 0.7 |
| Mean (SD) | Range | |
| Age | 51.93 (11.3) | 29–84 |
| Avg. number of kids seen weekly | 86 (46.2) | 0–500 |
| Avg. number of wellness visits weekly | 37.4 (35.5) |
Not all percents for each variable add up to 100% due to missing values, which never exceeded 2% for any one variable.
Mean scores for participants’ preparedness and perceived preparedness of colleagues to advise parents about child discipline, value placed in advising parents, and motivation to participate in activities designed to shift norms regarding CP are presented in Table 2. Overall, participants felt somewhat prepared to advise parents about how best to discipline their children (mean 3.19; SD 0.65) and perceived their colleagues to be slightly less prepared than them (mean 2.85; SD 0.64). Participants did place high value in advising parents by reporting they very much agree that there is value in providing advice on child discipline to parents (mean 3.59; SD 0.58). Respondents also reporting being very motivated (mean 3.60; SD 0.75) to participate in activities designed to change norms regarding CP including learning about research findings, talking to parents and colleagues about using techniques not involving CP, and challenging parents’ and colleagues’ viewpoint that support CP.
Table 2.
Descriptive Statistics of Measures Assessing Preparedness, Norms and Motivation (N=787)
| Measures | n | Alpha | Mean | SD |
|---|---|---|---|---|
| 1. Prepared to advise parents about child discipline | 783 | 0.70 | 3.19 | 0.65 |
| 2. Value in advising parents about child discipline | 782 | 0.70 | 3.59 | 0.58 |
| 3. Perceived professional norms of preparedness about advising parents about child discipline | 784 | 0.73 | 2.85 | 0.64 |
| 4. Motivation to participate in activities designed to change norms regarding the use of corporal punishment | 783 | 0.83 | 3.60 | 0.75 |
Note. Means are on a scale of: 1=not at all, 2= a little, 3=somewhat/moderately, 4=very, and 5=extremely;
Chronbach’s alpha coefficients were given as a measure of internal consistency and scale reliability, an alpha above 0.65 is considered good reliability.
Study participants varied in how prepared they felt and how they perceived their colleagues felt in advising parents about child discipline (see Table 3). Most participants (74%) reported they felt “extremely” or “very” strongly that advising parents about child discipline was a part of their job. Further, most (68%) felt “extremely” or “very” confident in their ability to provide advice to parents about child discipline. However, less (49%) felt “very” or “extremely” supported by their workplace to provide such advice. Additionally, most (81%) said they either felt “a little/not at all” (40%) or “somewhat/moderately” (41%) well-trained during residency on how to provide such advice; even fewer felt well-trained on this topic in medical school. Regarding perceived profession-wide norms of preparedness in providing parents with advice, the majority felt that most people in their profession were only “somewhat or moderately” confident to provide such advice (61%) and only “somewhat or moderately” well-trained (51%).
Table 3.
Beliefs about Preparedness, Norms, and Value of Advising Parents about Child Discipline (N = 787)
| A little/Not at all % | Somewhat/moderately % | Very % | Extremely % | |
|---|---|---|---|---|
| Professional preparedness to provide such counsel | ||||
| Believe it is a part of their job | 4.5 | 21.1 | 49.2 | 24.4 |
| Feel confident in ability | 3.8 | 27.6 | 49.7 | 18.3 |
| Feel supported in professional practice | 15.6 | 33.5 | 38.1 | 10.4 |
| Felt well-trained in residency program | 40.1 | 41.3 | 16.0 | 1.5 |
| Felt well-trained in medical school | 62.5 | 30.2 | 5.6 | 1.1 |
| Value in advising | ||||
| Believe parents value advice | 2.8 | 24.5 | 55.1 | 16.9 |
| Believe parents follow advice | 7.1 | 56.4 | 33.2 | 2.4 |
| Priority to giving advice | 7.9 | 34.3 | 47.0 | 9.8 |
| Professional preparedness norms | ||||
| Feel other professionals confident in ability | 20.5 | 60.5 | 17.5 | 1.1 |
| Feel other professionals well-trained | 36.4 | 51.1 | 11.8 | 0.5 |
| How motivated are you to participate in each of the following: | ||||
| Talk to parents about using effective discipline strategies | 3.8 | 17.8 | 56.2 | 22.0 |
| Learn more about research findings on effective discipline strategies | 10.2 | 24.3 | 50.7 | 14.6 |
| Learn more about research findings on harmful discipline strategies | 11.5 | 26.0 | 48.0 | 14.1 |
| Challenge parents that use harmful and/or ineffective discipline strategies | 11.4 | 29.5 | 43.3 | 15.2 |
| Challenge colleagues that support the use of harmful and/or ineffective discipline strategies | 24.7 | 32.5 | 27.1 | 14.5 |
Although most (72%) respondents believed it was “extremely” or “very” likely that parents valued their advice about child discipline, only 57% were “extremely” or “very” likely to prioritize giving such counsel to parents and just over one-third (36%) believed parents were “extremely” or “very” likely to follow their advice. However, most respondents were highly motivated to participate in activities designed to change norms regarding CP. Most were “extremely” or “very” motivated to talk to parents about using effective discipline strategies (78%) and learn more about research findings on effective discipline strategies (65%). Respondents were least enthusiastic about challenging their colleagues that support the use of harmful and/or ineffective discipline strategies (42%).
Some of the main constructs we examined were highly correlated. Preparedness to advise parents about child discipline was strongly positively correlated with value of advising parents about child discipline (r=0.67) and perceived professional norms of preparedness to advise parents about child discipline (r=0.52). Perceived professional norms of preparedness to advise parents about child discipline was positively correlated with value of advising parents about child discipline (r=0.50).
Multivariable regressions highlight how respondents varied in their perceptions of preparedness, professional preparedness norms, and value of advising parents about child discipline, as well as in their level of motivation for changing relevant norms (Table 4). However, only one characteristic was important across all four of these constructs: how often the respondent had been spanked as a child. Those who had been hit “often” as a child, compared to all who’d been hit less or not at all, felt more prepared and felt there was greater value in advising parents about how best to discipline their children. Interestingly, those who never experienced CP in childhood were less motivated to change CP-related norms when compared to those who had experienced CP.
Table 4.
Preparedness and Perceived Professional Norms of Preparedness about Advising Parents about Child Discipline, and Motivations to Change Norms Regarding Corporal Punishment (CP) Regressed on Demographic Characteristics and History of Being Spanked.
| Preparedness to advise parents about child discipline | Professional Preparedness norms about advising parents about child discipline | Value of advising parents about child discipline | Motivation to participate in activities to change norms regarding the use of CP | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | B | SE B | β | |
| Gender (ref = Female) | ||||||||||||
| Male | −0.11 | 0.05 | −0.08* | −0.06 | 0.05 | −0.04 | −0.04 | 0.04 | −0.03 | 0.03 | 0.06 | 0.02 |
| Race (ref = White) | ||||||||||||
| Black | −0.19 | 0.13 | −0.05 | −0.43 | 0.13 | −0.12** | 0.09 | 0.11 | 0.03 | 0.16 | 0.15 | 0.04 |
| Asian | −0.26 | 0.07 | −0.14*** | −0.26 | 0.07 | −0.15*** | −0.09 | 0.06 | −0.05 | 0.14 | 0.08 | 0.07 |
| Hispanic | −0.02 | 0.10 | −0.01 | −0.20 | 0.10 | −0.08* | 0.13 | 0.09 | 0.05 | 0.15 | 0.12 | 0.05 |
| Other | −0.02 | 0.12 | −0.01 | −0.16 | 0.12 | −0.05 | 0.10 | 0.11 | 0.04 | 0.25 | 0.14 | 0.06 |
| Region of U.S. (ref = Northeast) | ||||||||||||
| Midwest | 0.05 | 0.07 | 0.03 | −0.07 | 0.07 | −0.04 | −0.02 | 0.07 | −0.01 | −0.02 | 0.09 | −0.01 |
| West | 0.07 | 0.06 | 0.05 | 0.02 | 0.06 | 0.01 | −0.03 | 0.06 | −0.02 | <0.00 | 0.07 | <0.00 |
| South | 0.04 | 0.06 | 0.04 | 0.01 | 0.06 | 0.01 | −0.13 | 0.06 | −0.11* | <0.00 | 0.07 | −0.13** |
| Years of Experience (ref = <14 yrs) | ||||||||||||
| 15–24 yrs | 0.08 | 0.06 | 0.06 | −0.04 | 0.06 | −0.03 | 0.14 | 0.05 | 0.11** | 0.06 | 0.07 | 0.04 |
| 25+ yrs | 0.06 | 0.06 | 0.05 | −0.04 | 0.06 | −0.03 | 0.16 | 0.05 | 0.14** | 0.13 | 0.07 | 0.08 |
| Spanked as Child (ref = Rarely) | ||||||||||||
| Never | −0.12 | 0.06 | −0.07 | −0.06 | 0.06 | −0.04 | −0.07 | 0.06 | −0.05 | −0.20 | 0.08 | −0.10** |
| Sometimes | 0.06 | 0.06 | −0.15*** | −0.11 | −0.11 | −0.08* | −0.03 | 0.05 | −0.02 | −0.09 | 0.07 | −0.05 |
| Often | 0.22 | 0.10 | 0.09* | 0.09 | 0.09 | 0.03 | 0.20 | 0.09 | 0.09* | 0.06 | 0.11 | 0.02 |
Note.
p<0.05;
p<0.01;
p<0.001;
B is the unstandardized beta coefficient, which is the degree of change in the outcome variable for every 1-unit change in the predictor variable; SE B is the standard error for the unstandardized beta, which is similar to the standard deviation for a mean; β is the standardized beta coefficient, which ranges from −1 to 0 or 0 to 1 depending on the direction of the relationship between the outcome and predictor, with a value closer to −1 or 1 indicating a stronger relationship.
There was no other characteristic that mattered across all four constructs. Gender mattered only for personal preparedness to advise with women reporting being more prepared than men. Race mattered only for perceived personal and collegial preparedness norms: Asian respondents felt less prepared than all others, and White respondents perceived greater preparedness among colleagues than all others. Of all regions in the U.S., respondents in the South were least likely to value advising parents about CP and least motivated to change norms regarding CP. Finally, respondents with 15 years or more of professional experience felt there was more value in providing such advice to parents compared to those with less experience.
Participants were asked to rate how effective various disciplinary strategies are at improving a child’s behavior, assuming age-appropriate application (Figure 1). Of the fifteen strategies named, a majority rated eleven of them as “somewhat” to “extremely” effective. Respondents identified the most effective strategies as being consistent with rules, praising good behavior, applying awareness of a child’s developmental capabilities, redirection, and rewards for good behavior. Conversely, a majority rated the remaining four strategies, including shaming, yelling, spanking, and assigning chores as punishment, as only a little or not at all effective.
Figure 1.
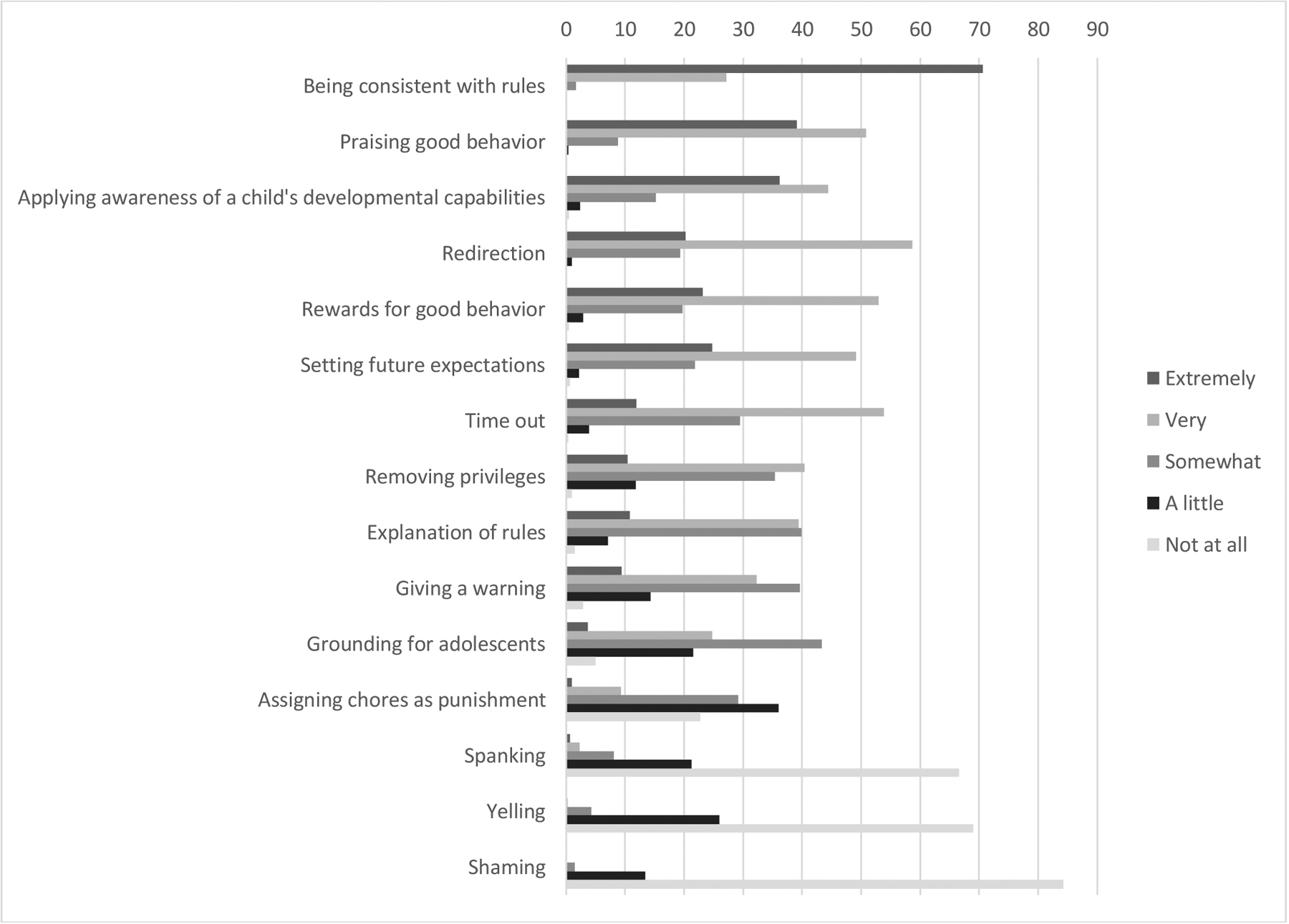
Responses to “How Effective Overall are the Following Disciplinary Strategies at Improving a Child’s Behavior, Assuming Age-Appropriate Application?” (N=787)
Lack of time was identified as the most frequent barrier (89.7%) to educating parents about child discipline. The other barriers ranked as follows: 1) lack of reimbursement for counseling parents on this topic (48.0%), 2) lack of training about how to best counsel parents (46.6%), 3) concerns about cultural sensitivity (44.0%), 4) lack of employer resources (43.5%), 5) lack of knowledge about how to best counsel parents (31.5%), 6) lack of confidence about how to best counsel parents (29.0%), 7) lack of evidence that counseling parents about discipline is effective (22.7%), 8) discomfort with the topic (18.7%), and 9) belief that this issue is not a priority for your time with parents (14%). Respondents were also given the option to name additional barriers though only 9.8% did and no other common barrier emerged. When asked what might help to reduce or remove the barriers, 28% provided suggestions. One common theme to emerge was the potential for developing parenting education training for pediatricians in medical school and residency programs including “improve[ment of] developmental/parenting education in family medicine and pediatric training programs” and “more training and education on how to approach and give the parents the necessary training on discipline they need.” Additionally, educational materials for parents regarding child discipline were suggested to assist pediatricians including “learning videos that can be watched by families in the office that pertain to effective discipline & positive parenting,” “websites to direct parents to,” and “concise handouts for parents with appropriate strategies at various ages.” Finally, improved reimbursement by insurance companies for time spent with families discussing child discipline was highlighted as needing change including “better reimbursement for behavior consults to allow for more consistent follow up.”
DISCUSSION
Results of the current study offer an important supplement to our understanding of pediatrician’s attitudes and perceived injunctive norms about parents’ use of CP with examination of specific constructs not previously studied. Although pediatricians saw the value in providing advice to parents regarding child discipline, they only felt somewhat prepared to advise parents about how best to discipline their children and perceived colleagues to be slightly less prepared, a common finding in pediatrician self-assessments.25 These findings indicate a need to focus on additional training for all pediatricians on how to most effectively engage with parents regarding healthy child discipline. Brief interventions designed to train pediatricians to counsel parents regarding child discipline have shown great promise in improving pediatricians’ self-efficacy to advise parents, their promotion of alternative child discipline strategies with parents, and increased communication between pediatricians and parents regarding child discipline.26–29
Despite lack of training, pediatricians indicated having knowledge about effective discipline strategies that are not harmful to children, as well as clearly recognizing ineffective strategies. Further, pediatricians were very motivated to participate in activities designed to change norms regarding CP. Participants were especially motivated to talk to parents about using effective discipline strategies, learn more about research findings on effective discipline strategies, and learn more about research findings on harmful discipline strategies. Given that pediatricians are a trusted and influential source of advice for parents,14–16 a unique opportunity exists to engage pediatricians in learning more about research regarding child discipline and how to effectively engage with parents regarding use of CP and more effective strategies. Pediatricians often have regular contact with families to provide information and discuss common challenges with child behavior. Such information on the harms of CP and how to implement more effective discipline strategies could be provided in short well-visits over time, with opportunity for parents to follow-up with questions or concerns. Respondents were least enthusiastic about challenging their colleagues that support the use of harmful and/or ineffective discipline strategies (42%). Incorporation of training into residency training programs is needed to shift overall attitudes regarding forms of harmful discipline amongst pediatricians and to increase capacity amongst pediatricians to engage with colleagues about the harms of CP. Additionally, policy statements and resources released through organizations relevant for most pediatricians, like the AAP, may be an effective way to educate pediatricians and shift norms regarding providing parents advice on child discipline.22,30
Pediatricians identified several barriers to advising parents on child discipline that are likely to stand in their way of effectively sharing this knowledge with parents. Time was considered the greatest barrier. Development and distribution of educational materials on age-appropriate discipline strategies for pediatric clinics and hospitals to provide to parents could reduce the burden of additional time expected for pediatricians to address discipline with parents. For example, short video interventions provided for parents in a clinical setting have been shown to reduce attitudes supportive of CP use and help parents change how they discipline their children.31–34 Such brief interventions are one potential method for reducing the additional time burden placed on pediatricians to engage with families around child discipline; they could be administered electronically in waiting or examination rooms before the well visit with pediatricians.30 Additionally, the identification of unsupportive workplaces as a barrier to engaging with families highlights the need to start with educating clinic administrators about the importance of addressing this topic and how to best support pediatricians in this endeavor. The last major barrier, lack of reimbursement for counseling on this topic, is more challenging to address but no less important. Addressing time, along with the related issue of reimbursement, will likely require a combination of policy changes and research. AAP policy currently recommends that providers educate parents about discipline,21 but reimbursement policies are not adequate to incentivize all pediatricians to provide this important educational service. Some parents will require more educational support than others. Efforts should focus on testing brief parenting assessment tools to help pediatricians identify at-risk children and adjust their time and resources accordingly.35,36 Because only one parent may be present for office visits, parenting assessment tools could assess the discipline behaviors of other caregivers and providers could encourage parents to share evidence-based resources with other family members.36
There are limitations to this study. This is the first study to assess many of these specific constructs and our measures have not been previously tested, so further studies are needed to replicate these findings. Additionally, despite the similar response rate to other professional surveys, there is the possibility that non-respondents differed from those who responded to the survey and so there may be a lack of generalizability of results to all primary care pediatricians in the U.S. The current study sample, however, is very similar demographically to the 2016 AAP membership (64% female and 73% White).37
With the release of the policy statement by the AAP on CP use,21 the timing is especially suitable for implementing further steps for training pediatricians in how to best counsel parents about child discipline. The current study provides insight into the educational training needs for pediatricians to understand harmful discipline strategies, more effective discipline strategies, and how to engage families regarding child discipline. It is important to implement training given that most physicians report witnessing parental CP use at some point in a medical setting38 and the significant influence of pediatricians in advising parents regarding CP.15,16 Medical professionals have the power to spread scientific knowledge and consensus regarding public health issues39 like CP use. Study results also highlight the major barriers for pediatricians to providing advice regarding child discipline to parents that need to be addressed, including physician time constraints. Additional research is also needed to identify effective ways for pediatricians to integrate child discipline advice into well child visits that are also time efficient. Ultimately such interventions should educate parents about the harms of CP and provide them with information about alternative forms of discipline that are both emotionally and physically healthier for children.
WHAT’S NEW.
The current study assesses pediatricians’ training gaps and barriers to providing parents with advice regarding child discipline. Results inform development of effective training interventions for pediatricians to engage with parents.
Funding:
The authors acknowledge partial funding from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (5K01HD058733; PI: Taylor). The authors would like to thank Ben Siegel, M.D., F.A.A.P. for his consultation, review, and advice regarding the content of the survey questionnaire. We also would like to thank Ana Bales for her involvement in the early stages of survey design.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Potential Conflicts of Interest: Dr. Scholer is an author of a parenting education program, Play Nicely, owned by Vanderbilt University. Otherwise, the authors have no conflicts of interest relevant to this article to disclose.
Disclosure: The authors have no financial relationships relevant to this article to disclose.
References
- 1.Gershoff ET, Grogan-Kaylor A. Spanking and child outcomes: Old controversies and new meta-analyses. Journal of Family Psychology. 2016;30(4):453–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Afifi TO, Ford D, Gershoff ET, et al. Spanking and adult mental health impairment: The case for the designation of spanking as an adverse childhood experience. Child Abuse and Neglect. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Afifi TO, MacMillan HL, Boyle M, et al. Child abuse and physical health in adulthood. Public Health Reports. 2016;27(3):10. [PubMed] [Google Scholar]
- 4.Afifi TO, Mota N, Macmillan HL, Sareen J. Harsh physical punishment in childhood and adult physical health. Pediatrics. 2013;132(2):e333–e340. [DOI] [PubMed] [Google Scholar]
- 5.Tomoda A, Suzuki H, Rabi K, Sheu Y-S, Polcari A, Teicher MH. Reduced prefrontal cortical gray matter volume in young adults exposed to harsh corporal punishment. Neuroimage. 2009;47(Suppl 2):T66–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnelly M, Straus MA. Corporal punishment of children in theoretical perspective. New Haven: Yale University Press; 2005. [Google Scholar]
- 7.Child Trends Databank. Attitudes towards spanking. 2015; https://www.childtrends.org/wp-content/uploads/2016/03/indicator_1458002400.003.pdf.
- 8.Gershoff ET, Lansford JE, Sexton HR, Davis-Kean P, Sameroff AJ. Longitudinal links between spanking and children’s externalizing behaviors in a national sample of White, Black, Hispanic, and Asian American families. Child Development. 2012:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finkelhor D, Turner H, Wormuth BK, Vanderminden J, Hamby S. Corporal Punishment: Current Rates from a National Survey. Journal of Child and Family Studies. 2019;28(7):1991–1997. [Google Scholar]
- 10.Ajzen I The theory of planned behavior. Organizational Behavior and Human Decision Processes. 1991;50(2):179–211. [Google Scholar]
- 11.Taylor CA, Hamvas L, Rice JC, Newman D, DeJong W. Perceived social norms, expectations, and attitudes toward corporal punishment among an urban community sample of parents. Journal of Urban Health. 2011;88(2):254–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fleckman JM, Taylor CA, Theall KP, Andrinopoulous K. Perceived social norms in the neighborhood context: The role of perceived collective efficacy in moderating the relation between perceived injunctive norms and use of corporal punishment. Child and Adolescent Social Work. 2019;36(1):29–41. [Google Scholar]
- 13.Fleckman JM, Taylor CA, Theall KP, Andrinopoulous K. The association between perceived injunctive norms toward corporal punishment, parenting support, and risk for child physical abuse. Child Abuse and Neglect. 2019;88:246–255. [DOI] [PubMed] [Google Scholar]
- 14.Taylor CA, McKasson S, Hoy G, DeJong W. Parents’ primary professional sources of parenting advice moderate predictors of parental attitudes toward corporal punishment. Journal of Child and Family Studies. 2017;26(2):652–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor CA, Moeller W, Hamvas L, Rice JC. Parents’ professional sources of advice regarding child discipline and their use of corporal punishment. Clinical Pediatrics. 2013;52(2):147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fortson BL, Moseley C, Burton T. Use of audience segmentation and focus group research to better reach parents: Implications for child maltreatment prevention American Professional Society on the Abuse of Children 21st Annual Colloquium; 2013; Las Vegas, NV. [Google Scholar]
- 17.Taylor CA, Fleckman JM, Scholer SJ, Branco N. U.S. Pediatricians’ Attitudes, Beliefs, and Perceived Professional Injunctive Norms about Spanking. Journal of Developmental and Behavioral Pediatrics. 2018. [DOI] [PubMed] [Google Scholar]
- 18.McCormick KF. Attitudes of primary care physicians toward corporal punishment. JAMA 1992;267(23):3161–3165. [PubMed] [Google Scholar]
- 19.American Academy of Pediatrics. Periodic Survey #38: Pediatrician Views on the Treatment & Prevention of Violent Injuries to Children Periodic Survey of Fellows, Division of Child Health Research, Executive Summary 1998; http://www.aap.org/en-us/professional-resources/Research/Pages/Pediatrician-Interest-in-Violence-Prevention-Results-From-1998-and-2003-AAP-Periodic-Surveys.aspx. Accessed Aug. 26, 2014.
- 20.Gershoff ET, Font SA, Taylor CA, et al. Medical center staff attitudes about spanking. Child Abuse and Neglect. 2016;61:55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sege RD, Siegel BS, Council on Child Abuse and Neglect, Committee on Psychosocial Aspects of of Child and Family Health. Effective Discipline to Raise Healthy Children. Pediatrics. 2018:e20183112. [DOI] [PubMed] [Google Scholar]
- 22.Jr. Hagan J, Shaw J, Duncan P. Bright Futures: Guidelines for Health Supervision of Infants, Children and Adolescents, 4th Edition Itasca, IL: American Academy of Pediatrics; 2017. [Google Scholar]
- 23.Stevenson J, Dykema J, Kniss C, Assad N, Taylor CA. Effects of Sequential Prepaid Incentives to Increase Participation and Data Quality in a Mail Survey of Pediatricians Midwest Association of Public Opinion Research; November 18, 2016, 2016; Chicago, IL. [Google Scholar]
- 24.Cho YI, Johnson TP, Vangeest JB. Enhancing surveys of health care professionals: a meta-analysis of techniques to improve response. Eval Health Prof. 2013;36(3):382–407. [DOI] [PubMed] [Google Scholar]
- 25.Davis DA, Mazmanian PE, Fordis M, Van Harrison R, Thorpe KE, Perrier L. Accuracy of physician self-assessment compared with observed measures of competence: A systematic review. JAMA. 2006;296(9);1094–1102. [DOI] [PubMed] [Google Scholar]
- 26.Scholer SJ, Brokish PA, Mukherjee AB, Gigante J. A violence-prevention program helps teach medical students and pediatric residents about childhood aggression. Clinical Pediatrics. 2008;47(9):891–900. [DOI] [PubMed] [Google Scholar]
- 27.Scholer S A Brief Intervention Facilitates Discussions About Discipline in Pediatric Primary Care. In: Hudnut-Beumler J, ed: SAGE; 2015. [DOI] [PubMed] [Google Scholar]
- 28.Burkhart K, Knox M, Hunter K. Changing Health Care Professionals’ Attitudes Toward Spanking. Clinical Pediatrics. 2016;55(11):1005–1011. [DOI] [PubMed] [Google Scholar]
- 29.Scholer S, Reich S, Boshers R, Bickman L. A brief program improves counseling of mothers with children who have persistent aggression. Journal of Interpersonal Violence. 2011;27(6):991–1004. [DOI] [PubMed] [Google Scholar]
- 30.Sege R, Siegel BS, Council on Child Abuse and Neglect, Committee on Psychosocial Aspects of Child and Family Health. Effective Discipline to Raise Healthy Children. Pediatrics. 2018:e20183112. [DOI] [PubMed] [Google Scholar]
- 31.Scholer SJ, Mukherjee AB, Gibbs KI, Memon S, Jongeward KL. Parents view a brief violence prevention program in clinic. Clinical Pediatrics 2007;46(8):724–734. [DOI] [PubMed] [Google Scholar]
- 32.Chavis A, Hudnut-Beumler J, Webb M, et al. A brief intervention affects parents’ attitudes toward using less physical punishment. Child Abuse & Neglect. 2013;37(12):1192. [DOI] [PubMed] [Google Scholar]
- 33.Scholer SJ, Hamilton EC, Johnson MC, Scott TA. A brief intervention may affect parents’ attitudes toward using less physical punishment. Family & Community Health: The Journal of Health Promotion & Maintenance. 2010;33(2):106–116. [DOI] [PubMed] [Google Scholar]
- 34.Scholer SJ, Hudnut-Beumler J, Dietrich MS. A brief primary care intervention helps parents develop plans to discipline. Pediatrics. 2010;125(2):e242–249. [DOI] [PubMed] [Google Scholar]
- 35.O’Connell LK, Davis MM, Bauer NS. Assessing Parenting Behaviors to Improve Child Outcomes. Pediatrics. 2015;135(2):e286–e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Research Related to Quick Parenting Assessment and Pediatric ACEs Algorithm. April 27, 2020.
- 37.American Academy of Pediatrics. Pediatricians’ Practice and Personal Characteristics: US only, 2016. 2017; Source: American Academy of Pediatrics, Division of Health Services Research, Periodic Survey of Fellows #92, 93, 94, and 95, 2016. Available at: https://www.aap.org/en-us/professional-resources/Research/pediatrician-surveys/Pages/Personal-and-Practice-Characteristics-of-Pediatricians-US-only.aspx. Accessed October 31, 2017.
- 38.Font SA, Gershoff ET, Taylor CA, et al. Staff responses when parents hit children in a hospital setting. Journal of Developmental and Behavioral Pediatrics. 2016;37(9):730–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brandt AM. The Cigarette Century. New York: Basic Books; 2007. [Google Scholar]


