Abstract
BACKGROUND:
Group visits can support health behavior change and self-efficacy. In primary care, an advance care planning (ACP) group visit may leverage group dynamics and peer mentorship to facilitate education and personal goal setting that result in ACP engagement.
OBJECTIVE:
To determine whether the ENgaging in Advance Care Planning Talks (ENACT) group visits intervention improves ACP documentation and readiness in older adults.
METHODS:
This randomized clinical trial was conducted among geriatric primary care patients from the University of Colorado Hospital Seniors Clinic, Aurora, CO, from August 2017 to November 2019. Participants randomized to ENACT group visits (n = 55) participated in two 2-hour sessions with discussions of ACP topics and use of ACP tools (i.e., Conversation Starter Kit, Medical Durable Power of Attorney form, and PREPARE videos). Participants randomized to the control arm (n = 55) received the Conversation Starter Kit and a Medical Durable Power of Attorney form by mail. The primary outcomes included presence of ACP documents or medical decision-maker documentation in the electronic health record (EHR) at 6 months, and a secondary outcome was ACP readiness (validated four-item ACP Engagement Survey) at 6 months.
RESULTS:
Participants were a mean of 77 years old, 60% female, and 79% white. At 6 months, 71% of ENACT participants had an advance directive in the EHR (26% higher) compared with 45% of control arm participants (P < .001). Similarly, 93% of ENACT participants had decision-maker documentation in the EHR (29% higher) compared with 73% in the control arm (P < .001). ENACT participants trended toward higher readiness to engage in ACP compared with control (4.56 vs 4.13; P = .16) at 6 months.
CONCLUSION:
An ACP group visit increased ACP documentation and readiness to engage in ACP behavior change. Primary care teams can explore implementation and adaptation of ACP group visits into routine care, as well as longer-term impact on patient health outcomes.
Keywords: advance care planning, group medical visits, primary care, behavior change, advance directives
INTRODUCTION
Having conversations about advance care planning (ACP) and documenting treatment preferences are associated with higher goal-concordant care, lower healthcare utilization, enhanced patient quality of life, and better family experiences.1,2 Despite these benefits, many older adults do not engage in ACP.3–5 Barriers to effective ACP in primary care settings include lack of time, patient expectations that healthcare practitioners initiate discussions, and reluctance to discuss end-of-life care.6–8 To address some of these barriers, we developed an innovative model called ENgaging in Advance Care Planning Talks (ENACT) group visits intervention.9,10
ENACT group visits are based on group visits, which are strategic interventions that bring groups of patients together for medical care, education, and peer mentorship.11 Group visit interventions have included single visits (e.g., postoperative),12 multiple visits (e.g., diabetes mellitus, type II),13 and ongoing groups (e.g., older adults with chronic conditions).14–16 Strengths of group visits include patient-centered education, high patient and practitioner satisfaction, and increased patient behavior change.17–19 However, studies are needed to determine whether an ACP-focused intervention in primary care can result in high-quality ACP. High-quality ACP includes increasing discussions, decision-making among patients, surrogate decision makers, and healthcare practitioners, and increased ACP documentation with the ultimate goal of honoring patients’ wishes.
Model Description
ENACT group visits promote group dynamics, peer-based learning, and goal setting around ACP engagement. The groups aim to bring together 8 to 12 patients for two 2-hour sessions, 1 month apart (Figure 1). ENACT group visits integrate ACP Engagement Theory,20 Collaborative Learning Theory,21 and strengths of group visits.15 ACP Engagement Theory defines ACP behaviors that relate to: (1) engaging decision makers, (2) considering acceptable quality of life, (3) considering flexibility for decision makers, and (4) asking physicians questions about ACP.20 Collaborative Learning Theory states that learning is a social experience, learners are diverse in experiences and learning styles, and learning includes individual experiences alongside medical knowledge.21 Together, these complementary theories may support ACP actions, behavior change, and integration of evidence-based ACP tools into primary care.
Figure 1.
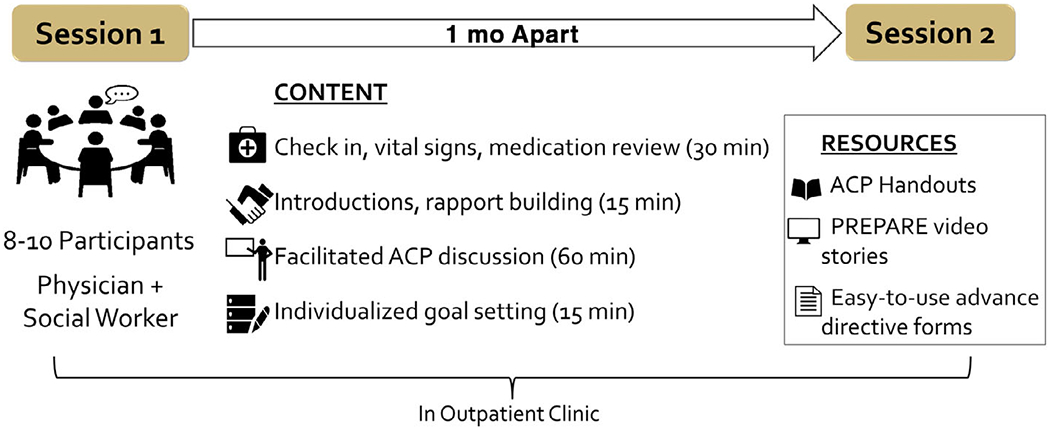
Overview of the ENgaging in Advance Care Planning (ACP) Talks group visits intervention.
ENACT group visits are facilitated by a healthcare practitioner who is able to bill for outpatient visits (e.g., physician, nurse practitioner, or physician assistant) and a second multidisciplinary team member. Facilitators use a published Facilitators’ Guide to lead an interactive group discussion of common ACP topics.9 Facilitators foster person-centered discussions that support sharing of personal experiences and diverse perspectives based on participants’ individual, family, social, cultural, and religious values and backgrounds. The first session focuses on sharing personal stories related to ACP experiences, consideration of personal values (including cultural or religious preferences), and roles of surrogate decision makers. The second session focuses on flexibility in decision-making, common medical decisions that may occur (i.e., cardiopulmonary resuscitation (CPR), hospitalizations, palliative care, and preferred place of care), and talking with trusted persons and healthcare teams. Facilitators provide education using multiple methods (i.e., question and answers, brief videos, and handouts) and ACP resources, such as the online PREPARE22 videos (www.PREPAREforYourCare.org) and the Conversation Starter Kit,23 to meet diverse learning styles. The PREPARE intervention has increased ACP discussions and ACP documentation; however, not all participants engaged, and some may have benefited from the support of a group visit model. Because ACP is a process that includes choosing surrogate decision makers and documenting preferences in advance directives, participants can bring copies of existing ACP documents or complete new advance directives to add to their electronic health record (EHR). State-specific and easy-to-use advance directives are available to participants.24 ENACT group visits core components and Facilitators’ Guide are available at www.ColoradoCarePlanning.org. Patients are informed that the ENACT group visits are billed to insurance, and that normal copayments for visits may apply. Details on clinical documentation and billing for ENACT group visits are published.9 We previously demonstrated the feasibility of the ENACT group visits intervention in three clinics.9,10
Evaluation of the ENACT Group Visits Intervention
Here, we present the findings of a randomized clinical trial to test whether the ENACT group visits intervention improves ACP documentation and readiness in older adults, compared with a control arm of mailed ACP materials. Selected as a lower-cost option that primary care clinics could implement, mailed materials were an overview letter on behalf of the patient’s primary care provider, a two-page version of the Conversation Starter Kit, and a one-page Colorado Medical Durable Power of Attorney form. We chose pragmatic and validated outcomes that are routinely collected or can be collected without undue burden, including presence of ACP documents, medical decision maker documentation in the EHR, and readiness based on the ACP Engagement Survey.25 We hypothesized that ACP documents and ACP engagement would be higher in the ENACT group visit arm compared with control at 6-month follow-up.
METHODS
Study Design
This is a two-arm randomized clinical trial at the University of Colorado Hospital Seniors Clinic. The goal was to determine the feasibility of randomization, recruitment, and retention to the ENACT group visits intervention, and effectiveness on patient-centered ACP outcomes after randomization to ENACT group visits versus mailed ACP materials. The study was approved by the Colorado Multiple Institutional Review Board and registered at ClinicalTrials.gov (NCT03141242). A safety officer monitored recruitment and adverse events. All participants provided written informed consent.
Setting and Participants
Primary care patients were enrolled from August 2017 to September 2018. Patients aged 60 years and older were identified (1,945 patients via EHR and 14 via self-referral) and assessed for eligibility based on EHR review for key exclusion criteria: English not preferred language; diagnosis of cognitive impairment or dementia on the problem list; diagnosis of deafness on the problem list; nonlocal residence; or prior participation in earlier ACP group visit quality improvement sessions.10 Recognizing that ACP is a process where patients’ wishes may change over time based on their personal or clinical context, and that ACP involves several distinct actions, including discussions as well as documentation, potential participants were not excluded if they already had an ACP document in the EHR. Potentially eligible patients were reviewed by their primary care practitioner as appropriate for a group-based intervention. Research assistants who were not involved in the intervention or outcome collection invited eligible and approved patients via letter, which included the consent form, and up to three calls. If individuals were able to be reached and interested in the study, they received additional telephone screening to determine their ability to travel to the clinic, access to a telephone for follow-up, and lack of plans to move within 6 months. We excluded individuals with a partner or spouse already enrolled or who had participated in earlier ACP group visits to maintain independence of participants. We used a modified informed consent process, including a teach-back method, to obtain informed consent by telephone.26 Participants were compensated $25 after the 6-month assessment.
Randomization
Eligible participants were randomized using a computerized random number generator in blocks of four within strata defined by age and sex. Staff scheduled participants to ENACT group visits as appropriate. Participants randomized to control were informed that they would receive materials by mail. Control participants were offered nonstudy ENACT group visits after study completion.
Interventions
Participants randomized to ENACT group visits received a letter confirming the session dates, the Conversation Starter Kit, and the Colorado Medical Durable Power of Attorney form. ENACT group visits interventions were conducted 1 month apart. Groups were facilitated by a physician and clinic social worker in a clinic conference room. During check-in, a medical assistant assessed patient vitals, and participants completed a medical update form to assist with clinical documentation. ACP tools included a 4-minute video of a family having “the conversation” initially shown on ABC News,27 PREPARE videos on flexibility in decision-making, and ACP forms, including a Medical Durable Power of Attorney form and the Colorado Medical Orders for Scope of Treatment (MOST) form. After each session, participants could request a 10-minute individual clinic visit with the physician to discuss a specific medical or ACP-related need, although fewer than 5% of group visit participants used this option. The physician completed visit documentation for each participant, and most visits were billed as outpatient level 3 visits.
Participants randomized to mailed ACP materials received a letter confirming their participation in the study and encouraging them to discuss ACP with their primary care practitioner, the Conversation Starter Kit, and a Colorado Medical Durable Power of Attorney form.
Measurements
We assessed presence of ACP documents in the EHR at baseline and 3, 6, and 12 months after study enrollment. ACP documents included living wills, Medical Durable Power of Attorney forms, and MOST form or CPR directive, but did not include documentation of clinical discussions. In Colorado, clinical teams can also document an orally appointed decision maker in the EHR. Thus, medical decision-maker documentation in the EHR was based on presence of an orally appointed medical decision maker or a Medical Durable Power of Attorney form. We measured ACP readiness at baseline and 6 months using the four-item validated ACP Engagement Survey.25 The four questions assess readiness for discussing and documenting ACP preferences (five-point Likert scale). The four items were averaged to create the total ACP Engagement Score, with higher scores indicating a higher degree of readiness. There was less than 10% missingness for ACP readiness questions.
We tracked participant eligibility, enrollment, and participation rates. Participants completed baseline surveys on characteristics, including age, sex, race/ethnicity, relationship status, education level, insurance type, and caregiver status (“in the last 12 months, have you been a caregiver for another person to help them take care of themselves”); a validated measure of health status (excellent to very poor); and self-report of memory concerns.
Data Analysis
Descriptive statistics were calculated for age, sex, race, insurance type, relationship status, education, and whether patient was a caregiver. Chi-square tests compared patient characteristics between the two intervention arms. Primary outcomes were presence of advance directive and medical decision-maker documentation in the EHR at 6 months, compared with baseline. We compared mean responses of ACP readiness between study groups at baseline and 6 months and used t-tests to determine if the means were significantly different between study groups. Multivariate logistic regression analyses, including an interaction for time (baseline or 6 months) and intervention arms, assessed the association between study arm and each readiness question at baseline and 6 months, controlling for sex, age, and presence of ACP documents at baseline. Given the small sample size, we did not control for other sociodemographic variables. This relationship was described using an odds ratio (OR), 95% confidence intervals (CIs), and P value. We calculated within-group pre-post effect sizes with the help of bivariate Pearson correlation using standard, clinically meaningful thresholds (i.e., small, 0.20–0.49; medium, 0.50–0.79; and large, ≥0.80).28,29 All findings were considered significant at P < .05 (two sided). We used SAS version 9.4 for the analyses.
RESULTS
We assessed 1,959 patients for eligibility. After excluding patients who were ineligible by EHR screen, 1,344 were reviewed by their primary care practitioner for ability to participate in a group-based intervention (Figure 2). Of 835 eligible and approved individuals who were invited to participate, 31 did not meet inclusion criteria, 203 were unable to be reached, 491 declined to participate, and 110 (13%) patients enrolled and were randomized to the ENACT group visits intervention or control (55 per arm). Of 491 patients who declined to participate, 206 stated they were not interested, 13 had plans to move from the area, 23 had transportation issues, 61 reported already completing ACP (preferred not to participate), 26 gave no reason, and 52 listed another reason.
Figure 2.
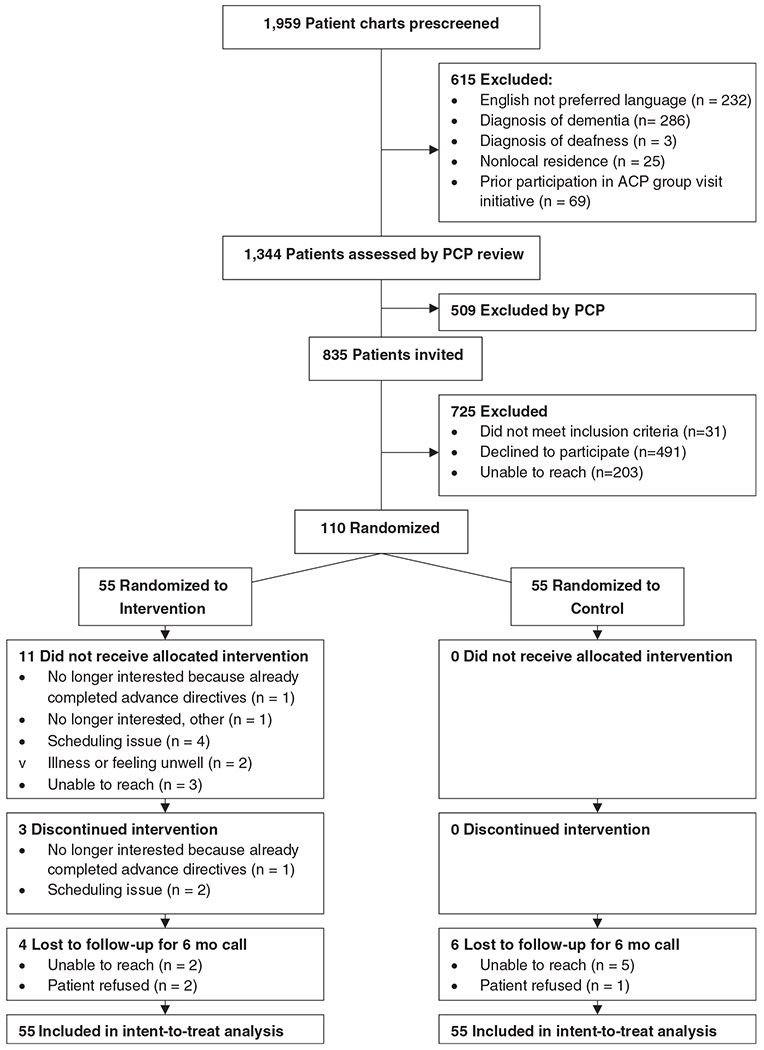
CONSORT diagram. ACP, advance care planning; PCP, primary care physician.
Mean age of participants was 77 years, and most were white and female (Table 1). Patients with self-reported memory concerns were similar in both arms. At baseline, the percentage of patients with ACP documents in the EHR was not different (44% in intervention and 40% in control; P = .7), although the rates were higher than reported averages in ACP studies of 36%.5 Baseline comparison between arms for medical decision makers in the EHR was not significantly different (P = .53). Group visit size ranged from 3 to 11 patients. For ENACT group visits, 44 participated in the first session and 41 participated in both sessions (91% retention rate).
Table 1.
Participant Characteristics, by Study Arm (n = 110)
| Participant characteristic | Control (N = 55) | ENACT group visits intervention (N = 55) | P value |
|---|---|---|---|
| Age, mean (SD), y | 77.2 | 77.4 | .84 |
| Women | 33 (60) | 33 (60) | 1.0 |
| Race/ethnicity | .49 | ||
| White | 42 (76) | 45 (82) | |
| African American | 6 (11) | 5 (9) | |
| Latino/Hispanic | 1 (2) | 3 (5) | |
| Asian/Pacific Islander | 1 (2) | 0 (0) | |
| American Indian/Native American | 2 (4) | 0 (0) | |
| Multiethnic/other | 3 (5) | 2 (4) | |
| Relationship status | .22 | ||
| Married/partnered | 35 (64) | 34 (62) | |
| Widowed | 8 (14) | 14 (25) | |
| Divorced or separated | 7 (13) | 2 (4) | |
| Single | 5 (9) | 5 (9) | |
| Education level | .23 | ||
| High school graduate | 5 (9) | 3 (6) | |
| Some college | 17 (31) | 9 (16) | |
| College graduate | 9 (16) | 11 (20) | |
| Postgraduate or professional education | 24 (44) | 32 (58) | |
| Insurance typea | |||
| Medicare | 54 (50) | 54 (50) | 1 |
| Medicare supplement | 33 (54) | 28 (46) | .34 |
| Medicaid | 2(100) | 0 | .15 |
| Tricare | 11 (48) | 12 (52) | .81 |
| Other | 8 (42) | 11 (58) | .45 |
| Caregiver in the past 12 mo | 12 (50) | 12 (50) | 1 |
| Self-rated quality of life | .92 | ||
| Excellent | 22 (40) | 22 (40) | |
| Fair | 7 (13) | 6 (11) | |
| Good | 24 (43) | 26 (47) | |
| Poor | 2 (4) | 1 (2) | |
| Self-report of memory concerns | 25 (45) | 24 (44) | .85 |
| ACP document in EHR at baseline | 22(40) | 24 (44) | .70 |
Note: Data are given as number (percentage), unless otherwise indicated.
Abbreviations: ACP, advance care planning; EHR, electronic health record; ENACT, ENgaging in Advance Care Planning Talks; SD, standard deviation.
Data are greater than 100%.
ACP Documents
At 6 months, 71% of ENACT participants had an ACP document in the EHR compared with 45% of control arm participants (P < .001), which is a 26% difference (Figure 3A). Similarly, 93% of ENACT participants had decision-maker documentation in the EHR compared with 73% in the control arm (P < .001) (Figure 3B). In a sensitivity analysis, the number of new ACP documents at 6 months was significantly different for ENACT (39 new documents) versus control (five new documents) (P = .0017).
Figure 3.
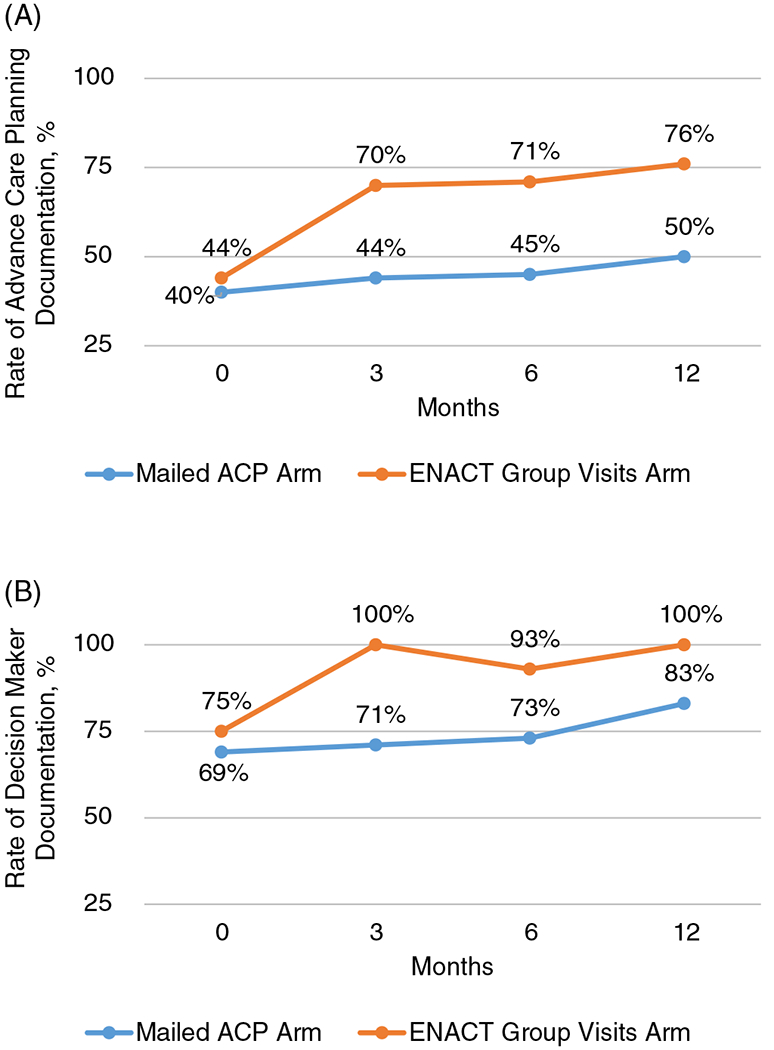
(A) Longitudinal data comparing rates of advance directive documentation in the electronic health record between the ENgaging in Advance Care Planning Talks (ENACT) group visit intervention arm and the mailed advance care planning (ACP) documents control arm (n = 110). (B) Longitudinal data comparing rates of decision-maker documentation between the ENACT group visit intervention arm and the mailed ACP documents control arm (n = 110).
Readiness for ACP
Based on the four-item composite ACP Engagement Score, ENACT participants reported higher readiness to engage in ACP compared with control (4.56 vs 4.13) at 6 months, although this was not statistically significant (Table 2). For ENACT intervention participants, the ACP Engagement Score increased significantly from baseline to 6-month follow-up, with a 22.5% increase in score (P = .02). Control participants also reported positive change in the ACP Engagement Score over time, although the magnitude of the change was smaller (7.5% increase in score; P = .05). In the ENACT arm, the effect sizes were small (0.20–0.49) for two items (readiness to talk with the physician and readiness to sign documents about medical care), and the effect sizes for change in readiness over time for each ACP readiness item in the control arm were negligible (Table 2). The effect sizes representing the increase in readiness over time were significantly different between the two groups (P = .0056).
Table 2.
ACP Engagement at Baseline and 6 Months After ENACT Group Visits or Control
| Baseline (n = 110) |
6 mo (n = 100) |
Baseline to 6-mo follow-up (n = 100) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Control, mean (SD) | Intervention, mean (SD) | P value | Control, mean (SD) | Intervention, mean (SD) | P value | Control effect sizea | Intervention effect sizea | |
| ACP Engagement Score (four-item composite) | 4.00 (0.4) | 4.21 (0.5) | .54 | 4.13 (0.4) | 4.56 (0.4) | .16 | 0.075 | 0.225 | |
| Readiness questions | Sign official papers naming a medical decision maker | 4.25 (1.2) | 4.49 (0.9) | .25 | 4.39 (1.0) | 4.80 (0.7) | .015 | 0.06 | 0.19 |
| Talk to your decision maker about medical care | 4.25 (1.1) | 4.65 (0.8) | .03 | 4.28 (1.2) | 4.74 (0.8) | .03 | 0.014 | 0.053 | |
| Talk to your physician about medical care | 3.47 (1.3) | 3.47 (1.1) | 1 | 3.59 (1.3) | 3.99 (1.2) | .16 | 0.046 | 0.20 | |
| Sign official papers about medical care | 4.04 (1.1) | 4.24 (1.0) | .31 | 4.26 (1.1) | 4.69 (0.9) | .03 | 0.11 | 0.24 | |
Note: Significant P values are bolded.
Abbreviations: ACP, advance care planning; ENACT, ENgaging in Advance Care Planning Talks; SD, standard deviation.
Clinically meaningful effect sizes were calculated from changes from baseline (i.e., mean ENACT scores minus mean control scores, divided by pooled baseline SDs) and are based on standardized criteria (i.e., 0.20–0.49, small; 0.50–0.79, medium; and ≥0.80, large).28
After adjusting for age, sex, and prior ACP documents, ENACT participants reported increased readiness for individual ACP actions that was significantly higher than control participants, including readiness to sign papers for a medical decision maker (adjusted OR = 1.43; 95% CI = 1.06–1.94), readiness to talk with a decision maker (OR = 1.6; 95% CI = 1.17–2.23), and readiness to sign papers about medical wishes (OR = 1.37; 95% CI = 1.03–1.82). There were no significant differences for readiness to talk to the physician about medical care.
DISCUSSION
This study demonstrates that an innovative, primary care–based ACP group visit model, the ENACT group visits intervention, increased ACP documentation in the EHR and some measures of ACP engagement among community-dwelling older adults. Planned as a pilot study, the study was not powered to detect clinical effectiveness, although the final results showed a clinically meaningful effect because the observed difference due to the intervention was sizable. A key strength of the ENACT group visits intervention is integration with the patient’s medical care, as evidenced by high rates of ACP documents in the EHR and over 90% documentation rates of the patient’s preferred medical decision maker. Even in this homogeneous population that was predominantly older, educated white women with a baseline rate of ACP documentation that is above U.S. average rates, ENACT group visits participants had significantly increased ACP documentation compared with baseline.
Patients randomized to the ENACT group visits intervention reported higher levels of readiness for three of the four ACP readiness questions. However, there was no difference in readiness to talk with their physician about future medical care. This may be due to the ACP resources for the intervention and control arms focusing on values clarification and communication with a medical decision maker, rather than the healthcare practitioner. These ACP actions are goals that individuals can take independently without setting up an appointment with their physician and were not specifically emphasized. Although the ACP Engagement Survey, including short versions, is feasible and validated to measure the ACP process, there may also have been a ceiling effect in these participants who had higher than average baseline rates of ACP documentation. However, analyses were adjusted for prior ACP documentation. Future studies could consider tailoring ACP interventions to level of readiness for a range of ACP behaviors. It is also likely that other meaningful outcomes of the ENACT group visits intervention were not measured, including value of the group dynamic/peer support or influence on future decision-making and goal-concordant care.
This study compares an in-person group visit that focuses on patient engagement and values clarification with a control arm of mailed materials, where patients were not scheduled to meet with a healthcare practitioner. Therefore, it is not possible to tell which ENACT group visits components resulted in increased ACP documentation. Because there are implementation challenges for ACP interventions, like visits with a physician or other facilitator, we instead chose a comparison arm that is lower cost and could potentially be a clinic-level initiative to increase awareness, and potentially ACP engagement.
This study has limitations. One limitation is that 20% (n = 11) of individuals randomized to the group visits did not attend a group visit session at all. Although this intention-to-treat analysis showed that participants randomized to ENACT had higher rates of ACP outcomes, from a feasibility and potential sustainability perspective, specific processes are still needed for pragmatic outreach, recruitment, and even flexible delivery options (i.e., evenings, weekends, and telehealth) for clinic-based ACP interventions. The high baseline rate of ACP documentation and medical decision-maker documentation may be related to the participants’ high levels of education and socioeconomic status, suggesting a selection bias. Future effectiveness and implementation studies will need to focus on increasing generalizability to real-world settings. Existing resources, like PREPARE and the Letter Writing Project,30 have been designed for socioeconomically diverse older adults, including those with lower health literacy or those who may prefer ACP resources in their native language. Finally, the overall recruitment rate of 13% is low and indicates a need for robust recruitment processes. Taken together, future work is needed to further test the effectiveness and implementation of ENACT group visits in diverse, real-world primary care settings.
This study demonstrates that a structured group visit around person-centered ACP values and experiences increased ACP documentation, medical decision-maker documentation, and readiness for some ACP action steps. Individuals who received mailed materials had significantly less engagement in ACP and advance directives in the EHR over a 6-month period. Primary care teams can explore implementation and adaptation of the ENACT group visits intervention into routine care, including developing sustainability plans that leverage the ability to bill for these visits and involve the strengths of the interprofessional primary care team.
ACKNOWLEDGMENTS
The authors thank Kirbie Hartley, LCSW, Sue Felton, Adreanne Brungardt, Sarah Jordan, Elizabeth Staton, Daniel Matlock, and Robert Schwartz.
Sponsor’s Role: The sponsor had no role in the design, methods, subject recruitment, data collection, analysis, or preparation of the article.
Footnotes
Publisher's Disclaimer: Disclaimer: The content of and views expressed in this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs.
Trial Registration: ClinicalTrials.gov ID NCT03141242; COMIRB 16-1922.
Conflict of Interest: Dr Sudore and University of California, San Francisco, regents licensed PREPARE for use in this study.
REFERENCES
- 1.Bond WF, Kim M, Franciskovich CM, et al. Advance care planning in an accountable care organization is associated with increased advanced directive documentation and decreased costs. J Palliat Med. 2018;21(4):489–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Houben CH, Spruit MA, Groenen MT, Wouters EF, Janssen DJ. Efficacy of advance care planning: a systematic review and meta-analysis. J Am Med Dir Assoc. 2014;15(7):477–489. [DOI] [PubMed] [Google Scholar]
- 3.Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. 2013;61(2):209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yadav KN, Gabler NB, Cooney E, et al. Approximately one in three US adults completes any type of advance directive for end-of-life care. Health Aff (Millwood). 2017;36(7):1244–1251. [DOI] [PubMed] [Google Scholar]
- 6.Ahluwalia SC, Bekelman DB, Huynh AK, Prendergast TJ, Shreve S, Lorenz KA. Barriers and strategies to an iterative model of advance care planning communication. Am J Hosp Palliat Care. 2015;32(8):817–823. [DOI] [PubMed] [Google Scholar]
- 7.Arnett K, Sudore RL, Nowels D, Feng CX, Levy CR, Lum HD. Advance care planning: understanding clinical routines and experiences of interprofessional team members in diverse health care settings. Am J Hosp Palliat Care. 2017; 34(10):946–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lund S, Richardson A, May C. Barriers to advance care planning at the end of life: an explanatory systematic review of implementation studies. PLoS One. 2015;10(2):e0116629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lum HD, Jones J, Matlock DD, et al. Advance care planning meets group medical visits: the feasibility of promoting conversations. Ann Fam Med. 2016;14(2):125–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lum HD, Sudore RL, Matlock DD, et al. A group visit initiative improves advance care planning documentation among older adults in primary care. J Am Board Fam Med. 2017;30(4):480–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edelman D, McDuffie JR, Oddone E, Gierisch JM, Nagi A, Williams JW Jr. Shared Medical Appointments for Chronic Medical Conditions: A Systematic Review. Washington, DC: Department of Veterans Affairs (US); 2012. [PubMed] [Google Scholar]
- 12.Lorentz PA, Swain JM, Gall MM, Collazo-Clavell ML. Combined group and individual model for postbariatric surgery follow-up care. Surg Obes Relat Dis. 2012;8(2):220–224. [DOI] [PubMed] [Google Scholar]
- 13.Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. CMAJ. 2013;185(13):E635–E644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cherniack EP. The use of shared medical appointments in the care of the elderly. J Ambul Care Manage. 2014;37(1):32–37. [DOI] [PubMed] [Google Scholar]
- 15.Scott JC, Conner DA, Venohr I, et al. Effectiveness of a group outpatient visit model for chronically ill older health maintenance organization members: a 2-year randomized trial of the cooperative health care clinic. J Am Geriatr Soc. 2004;52(9):1463–1470. [DOI] [PubMed] [Google Scholar]
- 16.May SG, Cheng PH, Tietbohl CK, et al. Shared medical appointments to screen for geriatric syndromes: preliminary data from a quality improvement initiative. J Am Geriatr Soc. 2014;62:2415–2419. [DOI] [PubMed] [Google Scholar]
- 17.Cohen S, Hartley S, Mavi J, Vest B, Wilson M. Veteran experiences related to participation in shared medical appointments. Mil Med. 2012;177(11): 1287–1292. [DOI] [PubMed] [Google Scholar]
- 18.Bronson DL, Maxwell RA. Shared medical appointments: increasing patient access without increasing physician hours. Cleve Clin J Med. 2004;71(5): 369–370, 372, 374 passim. [DOI] [PubMed] [Google Scholar]
- 19.Eisenstat SA, Ulman K, Siegel AL, Carlson K. Diabetes group visits: integrated medical care and behavioral support to improve diabetes care and outcomes from a primary care perspective. Curr Diab Rep. 2013;13(2): 177–187. [DOI] [PubMed] [Google Scholar]
- 20.Sudore RL, Stewart AL, Knight SJ, et al. Development and validation of a questionnaire to detect behavior change in multiple advance care planning behaviors. PLoS One. 2013;8(9):e72465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bruffee KA. Collaborative Learning: Higher Education, Interdependence, and the Authority of Knowledge. Baltimore, MD: Johns Hopkins University Press; 1993. [Google Scholar]
- 22.Sudore RL, Knight SJ, McMahan RD, et al. A novel website to prepare diverse older adults for decision making and advance care planning: a pilot study. J Pain Symptom Manage. 2014;47(4):674–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The Conversation Project. Starter kits. http://theconversationproject.org/starter-kit/intro/. Accessed October 13, 2012.
- 24.Sudore RL, Boscardin J, Feuz MA, McMahan RD, Katen MT, Barnes DE. Effect of the PREPARE website vs an easy-to-read advance directive on advance care planning documentation and engagement among veterans: a randomized clinical trial. JAMA Intern Med. 2017;177:1102–1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sudore RL, Heyland DK, Barnes DE, et al. Measuring advance care planning: optimizing the advance care planning engagement survey. J Pain Symptom Manage. 2017;53(4):669–681. e668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sudore RL, Landefeld CS, Williams BA, Barnes DE, Lindquist K, Schillinger D. Use of a modified informed consent process among vulnerable patients: a descriptive study. J Gen Intern Med. 2006;21(8):867–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The Conversation Project. Top TCP tools. 2018. https://theconversationproject.org/top-tcp-tools/. Accessed March 16, 2018.
- 28.Cohen J Statistical Power Analysis for the Behavioral Sciences. 2nd ed Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- 29.Sudore RL, Schillinger D, Katen MT, et al. Engaging diverse English- and Spanish-speaking older adults in advance care planning: the PREPARE randomized clinical trial. JAMA Intern Med. 2018;178(12):1616–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Periyakoil VS, Neri E, Kraemer H. A randomized controlled trial comparing the letter project advance directive to traditional advance directive. J Palliat Med. 2017;20:954–965. [DOI] [PubMed] [Google Scholar]


