Abstract
Objective
Access to abortion care in the United States (US) is restricted by numerous logistical and financial barriers, which have been further intensified by the COVID-19 pandemic. We sought to understand the ways in which COVID-19 prompted changes in clinical practices in abortion care among independent abortion clinics.
Study design
We surveyed independent US abortion clinics and documented changes in practice regarding the provision of abortion since March 1, 2020.
Results
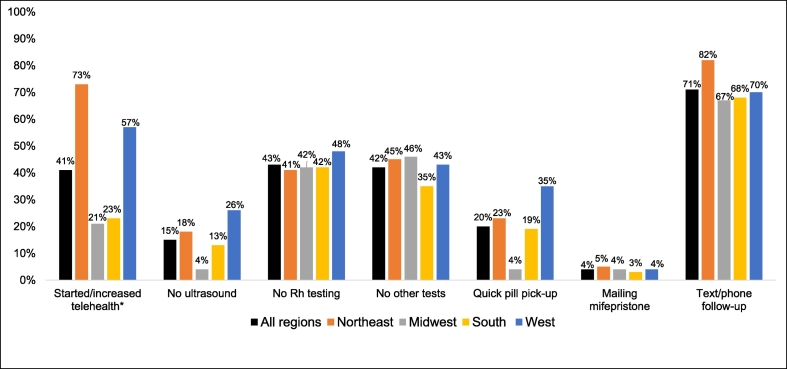
Among about 153 independent clinics invited, 100 clinics contributed relevant data and were included in the analytic sample. A total of 87% reported changes in protocols in response to the COVID-19 pandemic. Reported changes included moving to telehealth (phone or video) for follow-up (71%), starting or increasing telehealth for patient consultations and screening (41%), reducing Rh testing (43%) and other tests (42%), and omitting the preabortion ultrasound (15%). A total of 20% reported allowing quick pickup of medication abortion pills, and 4% began mailing medications directly to patients after a telehealth consultation. Clinical practice changes were reported throughout all regions of the US, but facilities in the Northeast (73%) were more likely to report starting or increasing telehealth than facilities in the South (23%, p < .001).
Conclusion
The COVID-19 pandemic accelerated use of telehealth among independent abortion clinics, but many clinics, particularly those in the South, have been unable to make these changes. Other practices such as reducing preabortion ultrasounds were less common in all regions despite clinical guidelines and evidence supporting such changes in practice and positive benefits for public health and patient-centered care.
Implications
The COVID-19 pandemic has created a window of opportunity to remove barriers to abortion, including expanding telehealth and reducing preabortion tests. Clinics can strive for a culture shift towards simplifying the provision of medication abortion and routinely avoiding preabortion tests and in-person visits. Such changes in practice could have positive benefits for public health and patient-centered care.
Keywords: Abortion, Independent abortion clinics, COVID-19, Medication abortion, Telehealth, Practice changes, Mifepristone, USFDA REMS
1. Introduction
Access to abortion care in the United States (US) is hampered by numerous logistical and financial barriers, and the COVID-19 context has intensified these barriers. Nearly 90% of US counties have no abortion provider [1], and there are 27 abortion deserts — major cities where residents must travel 100 miles or more to reach an abortion provider [2]. Traveling long distances for abortion care, which often involves multiple visits, results in increased costs for travel and childcare, lost wages from time off work and missed days of school [[2], [3], [4], [5]]. The COVID-19 pandemic has strained the healthcare workforce; forced people to travel greater distances for care, including crossing state lines; reduced appointments available; and increased wait times for abortion services [6,7]. Additionally, 11 states declared that abortion is not an essential health service and attempted to discontinue all abortion services [8,9].
The COVID-19 pandemic has brought new attention to medication abortion because it can be provided without any physical contact between a patient and clinician, which protects both patients and clinical staff. In recent months, professional organizations, including the American College of Obstetricians and Gynecologists and the National Abortion Federation, have issued statements endorsing telehealth and no-test (also called no-touch or no-contact) approaches for abortion care to maintain social distancing [[10], [11], [12]]. Additionally, several leading professional organizations came together to publish a sample protocol for providing no-test medication abortion [13].
These no-test approaches preserve the usual standard of care, except that they replace the in-person ultrasound or physical exam with other evidence-based methods to assess the patient's duration of pregnancy and screen for ectopic pregnancy [14]. They involve evaluating the patient by video or phone and rely on the reported date of the patient's last menstrual period to assess duration of pregnancy and then monitor patient symptoms via remote follow-up to rule out ectopic pregnancy [14,15]. This practice has been shown to be safe and effective for those who are certain of the date of their last menstrual period and have no known risk factors for ectopic pregnancy [14].
Adoption of no-test medication abortion practices could minimize the time that patients spend in healthcare facilities and reduce physical contact between patients and providers. Telehealth approaches — where a clinical consultation is conducted over video or phone and the medications are mailed to the patient — would confer the most protection. However, efforts to use telehealth for medication abortion have been hindered because the Federal Drug Administration (FDA) has placed a strict set of rules known as the Risk Evaluation and Mitigation Strategy (REMS) on mifepristone, the first pill taken for a medication abortion [16,17]. Among these restrictions is the requirement that mifepristone must be dispensed in a clinic, doctor's office or hospital rather than allowing for the common dispensing of medication in a pharmacy. In addition to the FDA restrictions, 18 states have effectively prohibited telemedicine for abortion [18].
It is unknown how many abortion providers have adopted such practices in response to COVID-19. In this paper, we document the changes in clinical practice regarding the provision of abortion beginning March 1, 2020, through mid-May 2020 among a sample of independent abortion providers.
2. Methods
2.1. Sample and recruitment
From April 16 to May 22, 2020, we invited independent abortion providers throughout the US to participate in a brief online survey about the ways in which COVID-19 had affected their abortion clinic. The larger study aimed to understand management strategies that clinics adopted to respond to the COVID-19 pandemic. The main findings that focus on changes in administrative and nonclinical practices were published separately [7]. The University of California, San Francisco Institutional Review Board approved this study (#20-30453).
We recruited participants via two abortion clinic listservs: the Abortion Care Network (ACN) [19] with about 110 independent clinics and the Abortion Clinical Research Network (ACRN) with 70 members, which included academic/hospital-affiliated independent clinics and Planned Parenthood clinics [20] (personal communication with Mary Tschann, September 1, 2020). We also sent emails directly to approximately 96 abortion clinic contacts with whom the authors had existing relationships and requested colleagues to forward the survey to other clinic contacts. There was some overlap between the two listservs, with 29 clinics subscribing to both, and about 90 of the emailed invitees were also members of the ACN. Taken together and removing duplicates, we estimate that the study team, ACN, and ACRN directly sent the invitation to 110 ACN members, 37 ACRN members, and 6 other independent clinic contacts, totaling approximately 153 unique independent abortion clinics.
Respondents aged 18 or older and who could complete the survey in English were eligible to complete the survey. While we primarily sought to survey clinic managers or directors, we also accepted responses from any individual at an independent abortion clinic who could report on the clinic's practices during COVID-19.
2.2. Data collection
The recruitment email contained a link to a Qualtrics survey. All respondents first provided electronic consent before answering a series of questions about their role at the clinic, the clinic's regional location and the services provided before COVID-19. If respondents indicated that they oversaw more than one clinic, we invited them to complete a separate survey for each clinic. The survey asked respondents their age, position at the clinic and geographic location of the clinic. We then asked a series of questions regarding how COVID-19 impacted their clinic and about any clinical practice changes as a result of the pandemic. The survey asked two specific items regarding medication abortion. The first item was, “Has your clinic changed your telemedicine practices related to abortion since March 1, 2020, due to COVID-19?” with response choices of no change, decreased existing telemedicine abortion services, started new telemedicine abortion services and increased telemedicine abortion services. The second item was, “How have the clinical practices in your clinic changed since March 1, 2020, due to COVID-19?” with specific response choices listed (as shown in Fig. 1). Participants could select all that applied to their practices. Additionally, the survey asked open-ended questions about other ways COVID-19 affected their clinic or services.
Fig. 1.
Percentage of clinics enacting each clinical practice change by geographic region.
2.3. Data analysis
Data analysis sought to describe the proportion of clinics reporting changes to their clinical practices as a result of the COVID-19 pandemic. Because the geographic distribution of abortion clinics and state laws that either support or hinder abortion access often influences access to abortion care, we then used Fisher's Exact Test to analyze whether clinical practice changes differed by geographic region of facilities, setting significance at p < .05.
3. Results
3.1. Sample
Overall, 120 people working at independent clinics responded to the survey. As reported previously [7], among these, there were five in which more than one respondent per clinic responded to the survey. In those instances, we kept only one response per clinic in the dataset for analysis, retaining the survey that was completed at the later date with the assumption that it would be more likely to capture the broadest range of experiences unless this survey was completed by someone other than the clinic manager or director. Another 15 respondents did not provide responses to the specific questions of interest for this manuscript. The final analytic sample was 100 clinics, resulting in a response rate of 65%. Clinics were well distributed among the 4 regions, including 31 in the South, 22 in the Northeast, 24 in the Midwest and 23 in the West. Clinics also reported a range of clinic volumes, with 8% providing fewer than 100 medication abortions in 2019, 36% providing 100–500, 29% providing 500–1000 and 25% providing more than 1000.
3.2. Closed-ended responses
Overall, 87% of abortion clinics stated that they changed their clinical practice in some way for at least some patients in response to COVID-19. Moving to phone or video follow-up to confirm complete abortion was the most commonly reported change in practice due to COVID-19, with 71% of clinics reporting this change (Fig. 1). Similarly, 41% reported starting or increasing telehealth for the patient's initial consultation appointment.
In terms of reducing tests, 43% of clinics reported omitting Rhesus (Rh) testing, 42% reported omitting other tests like hemoglobin and anemia, and 15% began omitting the preabortion ultrasound for some patients due to COVID-19. To dispense the medications, 20% reported allowing quick pickup of medications after a phone or telehealth consultation, and 4% reported mailing medications to patients after a phone or telehealth evaluation. No clinics reported initiating in-person delivery of medications to a patient's home.
The only statistically significant change in practice by region was adoption of telehealth, with facilities in the Northeast (73%) more likely to report starting or increasing telehealth than facilities in the South (23%, p < .001). Addition of quick pill pickup was higher in the West (35%) than in the Midwest (4%), though this difference did not reach statistical significance (p = .06).
3.3. Open-ended responses
In response to the open-ended questions, several participants, mostly in the Midwest, mentioned wanting to reduce tests and make other practice changes but cited state-level restrictions that prohibited such changes or the REMS requirement that bans mailing of medications.
“We are limited by the state as to what we can and cannot omit without facing possible legal repercussions. We have not been able to change much in terms of the provision of abortion care (testing, consult and ultrasound 24 hours prior to starting, medication ab's instead of aspiration for those under 11 weeks, etc.). We are not permitted to waive Rh testing, ultrasounds, or hemoglobin testing.” — Clinic director of a Midwest clinic.
“We have a state law … that requires medication abortions to be given in person by a physician. We also have a 24-hour consent law. The same physician who signs the 24-hour consent form with the patient is required to physically give the patient the pill. With reworking of physician schedules due to the pandemic, we have had difficulty with follow-up. We also are required to recommend the patient follow up in our clinic for an in-person ultrasound after a pill abortion — which we still recommend, but the patients are doing at home pregnancy tests in 1 month and calling us if they are positive.” — Clinic director of a Midwest clinic.
“Our state criminalizes teleabortion [telemedicine for abortion] so we have not moved mife [mifepristone] patients to video as we'd like.” — Physician at a Midwest clinic.
Other participants mentioned that the reductions in tests and an increase in telehealth improved or have the potential to improve quality of care.
“… patients mostly love the increased access and convenience of telehealth visits; for the patients we do see in clinic, we generally have so much more time to spend with them now without being rushed; some clinicians have been able to expand their practice to now offer medication abortion to meet the need.” — Clinician at a clinic in the West.
“I would be delighted to do No-Touch abortion for pts [patients] unable to come in to the office and mail pts their medication directly. This would be the safest and most effective way to deliver abortion care and would reach the greatest number of patients at lowest risk to all and would expand access and reduce unnecessary delays.” — Physician and owner at a clinic in the Northeast.
However, at least one participant was so enthusiastic about the potential for no-test medication abortions to reduce potential COVID risk that the clinic is “strongly encouraging” it over aspiration abortion.
“We implemented telehealth as a result of COVID-19 and are strongly encouraging MAB when appropriate. We are using Low-touch & No-touch MAB protocols and sending patients home with pregnancy tests for follow-up purposes (along with follow up call).” — Administrative Officer at a clinic in the West.
4. Discussion
This paper finds that the COVID-19 pandemic accelerated the use of telehealth for abortion. The use of telehealth has become common practice among independent abortion providers, used in some way with patients either for preabortion counseling or in follow-up, although not necessarily negating a visit to the clinic. This is consistent with practices that were already changing well before the COVID-19 pandemic [21,22]. Moving more of the patient–provider interaction to video or phone for all abortions, even those that require a clinic visit like a later abortion, may be cost-effective and may facilitate staffing management for clinics especially during a time when COVID-19 risks make some staff reluctant or unable to physically work at the clinic. Additionally, more clinics are now omitting Rh testing for patients, which is consistent with trends that began in 2019 when the National Abortion Federation first released a guideline that providers may forego anti-D immune globulin for Rh-negative patients, also before COVID-19 [23].
Omitting the ultrasound for patients who are medically eligible was surprisingly less common, with only 15% of providers nationally making this change in the first three months of the pandemic in the US despite evidence that it is safe [14] and the new guidelines [11,12,24] that endorse omitting such tests when possible to reduce physical contact and subsequent risk of COVID infection. Requiring a preabortion ultrasound severely limits the value of telehealth. Mailing of medication abortion pills was similarly rare. This low rate could be because the FDA REMS requires that Mifeprex be dispensed only in clinics, doctors' offices and hospitals [17]. These data were collected before a July 2020 Federal ruling that the FDA's in-clinic requirement is unconstitutional [25,26]. For as long as the ruling is upheld and the COVID pandemic continues, the ruling makes it permissible for clinicians to mail medications to their patients so that patients may avoid a trip to a clinic, but this is only possible in states where other laws do not prohibit telehealth for abortion. The open-ended responses suggest that indeed there are other barriers besides the FDA REMS restrictions, particularly state laws that not only ban telemedicine but also require unnecessary in-person tests like ultrasound and Rh testing. Although not mentioned by the participants, another potential barrier is the concern that public or private insurance would not cover telemedicine or would reduce reimbursements if tests are not done. To reduce COVID-19 risk, insurances should reimburse providers a global rate for a medication abortion, trusting clinicians to decide whether such care can be delivered by telemedicine and which tests are needed to deliver that care.
Even in states where it is legal to omit tests, like in the Northeast and West, many providers did not change their practice of routinely conducting preabortion ultrasounds and other tests, which puts the public, patients and providers at risk of COVID-19. This is especially concerning where abortion clinics are scarce. For the clinics that did begin this practice, it is unknown whether they will be able to continue such innovations beyond the pandemic. New practice models for medication abortion could have positive benefits beyond the pandemic if they allow individuals to get abortions earlier in pregnancy [27]. While medication abortion is extremely safe and effective [28,29], efficacy is higher at earlier gestations. Additionally, it simplifies the abortion experience and reduces logistical and emotional burdens for patients. Eliminating unnecessary ultrasounds is consistent with trauma-informed care, as sparing patients from undergoing unnecessary procedures can reduce stress and triggers [30].
The findings reported here are consistent with an analysis of 62 abortion facilities including academic centers and Planned Parenthood centers, in which 22% reported no longer routinely conducting ultrasound and 34% reported no longer conducting Rh testing when providing medication abortion [31]. While the present study included more clinics (100) and focused on changes at independent clinics, this remains a small subsample of the 344 independent clinics that exist nationwide [19]. Those that are networked through the listservs or through our contacts may be more knowledgeable of the latest research and paradigms in abortion care. Thus, they may be systematically different from those that we did not reach, and these findings may not be generalizable to the larger universe of independent clinics. We achieved a response rate of about 65% but do not have data on those clinics that chose not to participate. Given the emergency state that clinics were in during the data collection period, it may have been that among those invited, better resourced clinics had more time to complete the survey. Thus, clinics that responded to our survey may have had greater resources to incorporate clinical practice changes and may be overrepresented. However, we were still able to recruit a wide variety of clinics in terms of region and patient volume.
Clinics can strive for a culture shift to routinely offer patients who are medically eligible the ability to avoid preabortion tests and in-person visits, which could have positive health benefits for the public during the pandemic and for patient-centered care. At the same time, having a choice between medication abortion and procedural abortion is paramount to patient-centered care, and thus, it is important that clinics not pressure patients to opt for a medication abortion. Providing information on both options and explaining that a medication abortion can be done without a clinic visit may naturally shift more people to select a medication abortion.
These results showed that there was a change after the COVID-19 pandemic in medication abortion models, but further research is needed to ensure the change in practice persists even after the pandemic. Retrospective studies are needed to confirm that no-test and telehealth models for medication abortion are safe and effective, and further research is needed to better understand patient satisfaction and acceptability. Human-centered design approaches could be employed to develop models that are optimized for patient needs. Additionally, research on the impact of these models on the time to care is also needed, as these models may actually improve safety and effectiveness if, overall, patients are having medication abortions at earlier gestations.
5. Conclusion
The COVID-19 pandemic accelerated use of telehealth among independent abortion clinics, but many clinics, particularly those in the South and Midwest, have been unable to make these changes. Other practices such as reducing preabortion ultrasounds were less common in all regions despite clinical guidelines and evidence supporting such changes in practice and positive benefits for public health and patient-centered care. Enabling patients to obtain abortion care in the way that they desire, and as early as possible, could improve both patient satisfaction and abortion outcomes.
Acknowledgments
Acknowledgments
We appreciate the efforts made by the independent clinics to participate in this study during an incredibly difficult time. We also appreciate the efforts of Carole Joffe, Rebecca Willman, Jennifer Price, and the Abortion Care Network, for reaching out to clinics for participation.
Declaration of competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Declarations of interest: none.
References
- 1.Jones R.K., Witwer E., Jerman J. Guttmacher Institute; September 2019. Abortion incidence and service availability in the United States, 2017.https://www.guttmacher.org/report/abortion-incidence-service-availability-us-2017 [Google Scholar]
- 2.Cartwright A.F., Karunaratne M., Barr-Walker J., Johns N.E., Upadhyay U.D. Identifying national availability of abortion care and distance from major US cities: systematic online search. J Med Internet Res. 2018;20 doi: 10.2196/jmir.9717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bearak J.M., Burke K.L., Jones R.K. Disparities and change over time in distance women would need to travel to have an abortion in the USA: a spatial analysis. Lancet Public Health. 2017;2(11):E493–E500. doi: 10.1016/S2468-2667(17)30158-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen D.S., Joffe C.E. University of California Press; Oakland, California: 2020. Obstacle course : the everyday struggle to get an abortion in America. [Google Scholar]
- 5.Upadhyay U.D. Innovative models are needed for equitable abortion access in the USA. Lancet Public Health. 2017;2(11):E484–E485. doi: 10.1016/S2468-2667(17)30181-0. [DOI] [PubMed] [Google Scholar]
- 6.North A. What it takes to get an abortion during the coronavirus pandemic. Vox; 2020. [Accessed September 1, 2020]; Available from: https://www.vox.com/2020/4/1/21200247/coronavirus-texas-abortion-ban-pandemic-covid-19.
- 7.Roberts S.C.M., Schroeder R., Joffe C. COVID-19 and independent abortion providers: findings from a rapid-response survey. Perspect Sex Reprod Health. December 2020 doi: 10.1363/psrh.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donley G., Chen B., Borrero S. The legal and medical necessity of abortion care amid the COVID-19 pandemic. Journal of Law & the Biosciences, Forthcoming. 2020;7(1):lsaa013. doi: 10.1093/jlb/lsaa013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sobel L, Ramaswamy A, Frederiksen B, Salganicoff A. State action to limit abortion access during the COVID-19 pandemic. [Accessed September 1, 2020]; Available from: https://www.kff.org/coronavirus-covid-19/issue-brief/state-action-to-limit-abortion-access-during-the-covid-19-pandemic/
- 10.American College of Obstetricians and Gynecologists Joint statement on abortion access during the COVID-19 outbreak. 2020. https://www.acog.org/clinical-information/physician-faqs/~/link.aspx?_id=43CF073F75B0407882567D8C250A2A76&_z=z Available from:
- 11.American College of Obstetricians and Gynecologists. COVID-19 FAQs for obstetrician–gynecologists, gynecology. [Accessed September 1, 2020]; Available from: https://www.acog.org/en/clinical-information/physician-faqs/COVID19-FAQs-for-Ob-Gyns-Gynecology
- 12.National Abortion Federation Abortion & COVID-19. 2020. https://prochoice.org/abortion-covid-19/ Available from:
- 13.Raymond E.G., Grossman D., Mark A. Commentary: no-test medication abortion: a sample protocol for increasing access during a pandemic and beyond. Contraception. 2020;101:361–366. doi: 10.1016/j.contraception.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raymond E.G., Tan Y.L., Comendant R. Simplified medical abortion screening: a demonstration project. Contraception. 2018;97:292–296. doi: 10.1016/j.contraception.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 15.Raymond E.G., Grossman D., Mark A. Commentary: no-test medication abortion: a sample protocol for increasing access during a pandemic and beyond. Contraception. 2020;101(6):361–366. doi: 10.1016/j.contraception.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mifeprex REMS Study Group Sixteen years of overregulation: time to unburden Mifeprex. N Engl J Med. 2017;376:790–794. doi: 10.1056/NEJMsb1612526. [DOI] [PubMed] [Google Scholar]
- 17.US Food and Drug Administration Mifeprex risk evaluation and mitigation strategy (REMS) program. 2016. https://www.accessdata.fda.gov/drugsatfda_docs/rems/Mifeprex_2016-03-29_REMS_document.pdf Available from:
- 18.Ramaswamy A WG, Sobel L, Salganicoff A. Medication abortion and telemedicine: innovations and barriers during the COVID-19 emergency. Kaiser Family Foundation 2020; [Accessed September 1, 2020]; Available from: https://www.kff.org/policy-watch/medication-abortion-telemedicine-innovations-and-barriers-during-the-covid-19-emergency/
- 19.Abortion Care Network Communities need clinics. 2019. https://abortioncarenetwork.org/wp-content/uploads/2020/08/CommunitiesNeedClinics2019.pdf Available from:
- 20.Society of Family Planning Abortion Clinical Research Network. 2020. https://www.societyfp.org/research-support/abortion-clinical-research-network/ Available from:
- 21.Endler M., Lavelanet A., Cleeve A., Ganatra B., Gomperts R., Gemzell-Danielsson K. Telemedicine for medical abortion: a systematic review. BJOG. 2019;126:1094–1102. doi: 10.1111/1471-0528.15684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fok W.K., Mark A. Abortion through telemedicine. Current opinion in obstetrics and gynecology. 2018;30:394–399. doi: 10.1097/GCO.0000000000000498. [DOI] [PubMed] [Google Scholar]
- 23.National Abortion Federation . National Abortion Federation; Washington, D.C.: 2019. NAF 2019 Clinical Policy Guidelines for Abortion Care. [Google Scholar]
- 24.American College of Obstetricians and Gynecologists Practice bulletin no. 225: medical abortion up to 70 days of gestation. Obstet Gynecol. 2020:136. [Google Scholar]
- 25.Coleman J. Judge waives requirement for in-person visit to get abortion pill during pandemic. The Hill. 2020. https://thehill.com/policy/healthcare/507158-judge-waives-requirement-for-inperson-visit-to-get-abortion-pill-during Available from:
- 26.Kunzelman M. Federal judge rules women can get abortion pill without doctor visits. 2020. https://www.pbs.org/newshour/health/federal-judge-rules-women-can-get-abortion-pill-without-doctor-visits Available from:
- 27.Upadhyay U.D., Grossman D. Telemedicine for medication abortion. Contraception. 2019;100:351–353. doi: 10.1016/j.contraception.2019.07.005. [DOI] [PubMed] [Google Scholar]
- 28.Cleland K., Creinin M.D., Nucatola D., Nshom M., Trussell J. Significant adverse events and outcomes after medical abortion. Obstet Gynecol. 2013;121:166–171. doi: 10.1097/aog.0b013e3182755763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Upadhyay U.D., Desai S., Zlidar V. Incidence of emergency department visits and complications after abortion. Obstet Gynecol. 2015;125:175–183. doi: 10.1097/AOG.0000000000000603. [DOI] [PubMed] [Google Scholar]
- 30.Ward L.G. Trauma-informed perinatal healthcare for survivors of sexual violence. J Perinat Neonatal Nurs. 2020;34:199–202. doi: 10.1097/JPN.0000000000000501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tschann M LH, Ly E, Hilliard S. Family planning visits during the COVID-19 pandemic: phase 1 results now available. Society for Family Planning, July 2020. 2020; [Accessed September 1, 2020]; Available from: https://societyfp.org/wp-content/uploads/2020/07/SFP_FamilyPlanningDuringCovid_Final_July_2020.pdf