Abstract
Patient: Male, 57-year-old Final
Diagnosis: COVID-19 pneumonia • reinfection
Symptoms: Cough • fever
Medication: —
Clinical Procedure: —
Specialty: Infectious Diseases
Objective:
Unusual clinical course
Background:
Coronavirus disease 2019 (COVID-19) has radically changed the world, and promising vaccine trials are currently underway. The immune responses in asymptomatic and symptomatic individuals infected with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are still under investigation, and data are evolving. While it is known that humoral and cell-mediated immune responses against SARS-CoV-2 are elicited, it is uncertain whether these responses protect against reinfection or that they provide definitive evidence of viral clearance. Very few cases have been reported in the literature regarding reinfection with SARS-CoV-2.
Case Report:
We present a case of a middle-aged man with asymptomatic SARS-CoV-2 infection who later developed mild symptomatic COVID-19 after a period of 3 months. The source of reinfection was likely from the community, which had a soaring burden of infection with the highest number of COVID-19 cases per million in the world at that time. The patient had 2 negative COVID-19 polymerase chain reaction (PCR) tests 2 weeks after the initial infection. During the second infection, a nasopharyngeal reverse-transcription PCR test and tests for the presence of COVID-19 immunoglobulin (Ig)M and IgG antibodies were all positive.
Conclusions:
Reinfection with SARS-CoV-2 is a strong possibility. This case raises concerns that asymptomatic infections may not provide long-term protective immunity to all patients, which could make them susceptible to rein-fection. Possible explanations for reinfection include an interval decrease in protective antibodies titers after SARS-CoV-2 infection that may be more prevalent in patients who had an asymptomatic infection. Other possibilities include viral reactivation after a prolonged carriage of the virus or delayed immune response.
MeSH Keywords: Coronavirus Infections, COVID-19, SARS Virus, Serology, Polymerase Chain Reaction
Background
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was declared a pandemic by the World Health Organization (WHO) in March 2020. Since then, the number of cases worldwide has risen dramatically despite extensive efforts to contain the virus. As of the August 26, 2020, 24 million people had been infected worldwide, with a global death rate of 5% among the confirmed cases [1].
The clinical presentation of COVID-19 is highly variable and ranges from asymptomatic to severe pneumonia and acute respiratory distress syndrome requiring intensive care ventilator support and possibly resulting in death. A critical question is whether reinfection with SARS-CoV-2 is possible. Reinfection with SARS-CoV-2 in individuals who have previously recovered would present a major and persistent public health concern across the world in terms of morbidity and mortality. The WHO has expressed uncertainty about whether the presence of antibodies in the blood provides full protection against reinfection with SARS-CoV-2 [2]. Reinfection has been classically defined as a second infection that appears after recovery from the first infection and arises from the same causative agent. Given the novelty of the disease, a standardized definition and the criteria for SARS-CoV-2 reinfection have yet to be made. The criteria for considering patients free of COVID-19 are also unclear. The WHO deems asymptomatic patients noninfectious 10 days after the initial positive reverse-transcription polymerase chain reaction (RT-PCR) test result, after which they no longer need to be in isolation [3]. Although further understanding regarding possible reinfection is still evolving, recent studies imply that the loss of antibodies may play a vital role.
Only a handful of possible reinfection or viral relapse cases have been reported in the literature so far [4–7]. Limited data are available for long-term immunological assessment of COVID-19. An immunological analysis of SARS-CoV-2 asymptomatic patients revealed that the titers of immunoglobulin (Ig)G levels and neutralizing antibodies decreased 2 to 3 months after the infection [8]. These low levels of antiviral IgG antibodies in asymptomatic patients could eventually turn into seronegativity, thereby predisposing them to reinfection. We present a case in which it is likely that the patient recontracted the virus from the community 3 months after an initial infection. The potential reinfection occurred in the setting of an extremely high rate of transmission and high burden of infection in the State of Qatar, which had the largest number of cases per million in the world during June 2020.
Case Report
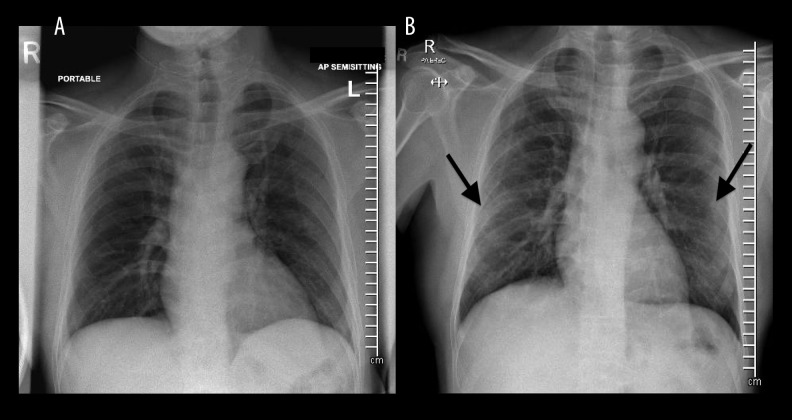
A 57-year-old man with a past medical history of long-standing type 2 diabetes mellitus presented with asymptomatic COVID-19 infection in March 2020 during the initial phase of the pandemic in the State of Qatar. He had no symptoms such as fever, cough, or shortness of breath. His vital signs were all within normal limits, and a physical examination was unremarkable. Chest X-ray did not reveal any abnormalities (Figure 1A). Basic laboratory investigations revealed a white blood cell count of 8.7×103/μL (reference range [4.0–10.0]×103/μL); lymphocytes, 3.8×103/μL (reference range [1.0–3.0]×103/μL); C-reactive protein, <5.0 mg/L (reference 0.0–5.0 mg/L); and glycated hemoglobin, 10.1%. A COVID-19 RT-PCR test from a nasopharyngeal swab was found to be positive (cycle threshold value of RdRp gene <30). The patient was screened for COVID-19 because he had been exposed to an infected work colleague. He received a 5-day course of chloroquine and oseltamivir per the local hospital COVID-19 treatment protocol at the time. The local clinical protocol (March 2020, Communicable Disease Center, Hamad Medical Corporation, Doha, Qatar) for asymptomatic patients was to administer chloroquine/hydroxychloroquine and oseltamivir orally for a total of 5 days. The patient was discharged to a quarantine facility and was found to have 2 negative COVID-19 PCR tests from nasopharyngeal swabs over a period of 3 weeks after the initial positive test.
Figure 1.
(A) Plain radiograph chest anteroposterior view at day 0. Chest X-ray at initial presentation with no significant abnormalities and no infiltration. (B) Plain radiograph chest anteroposterior view at day 86. Chest X-ray at 86 days with mild haziness in bilateral lower lung zones suggestive of infiltration (marked by black arrow). Infiltration is more notable in the peripheral area than the central area.
The patient returned to his home, which was in one of the focal outbreak areas in the country. He reported that several of his colleagues and housemates had contracted COVID-19 during his stay at home. After 86 days, the patient presented with fever, myalgia, headache, and a productive cough of 5 days’ duration (Figure 2). Upon initial examination, his temperature was 37.3°C; pulse, 91 beats per minute; blood pressure, 120/72 mmHg; respiratory rate, 17/min; and oxygen saturation, 97% on room air. The rest of the examination, including chest examination, was unremarkable. On this presentation, the patient’s chest X-ray was significant for accentuated bronchovascular and perihilar markings with mild haziness in bilateral lower lung zones suggestive of infiltration (Figure 1B). Basic investigations revealed a white blood cell count of 11.7×103/μL (reference [4.0–10.0]×103/μL); lymphocytes, 2.82×103/μL (reference [1.0–3.0]×103/μL); and C-reactive protein, 71 mg/L (reference 0.0–5.0 mg/L). A COVID-19 PCR test from a nasopharyngeal swab was again found to be positive with cycle threshold values of RdRp gene and E gene 29.89 and 31.37, respectively. The Cephpeid Xpert® Xpress SARS-CoV-2 test on the GeneXpert Instrument System was used for COVID-19 RTPCR testing, which is a validated approach that has been approved by the Food and Drug Administration (FDA). The test has high sensitivity, which was evaluated in a multicenter trial [9]. Rapid COVID-19 IgM and IgG were both reported to be reactive (rapid qualitative antibody test). Biohit SARS-CoV-2
Figure 2.
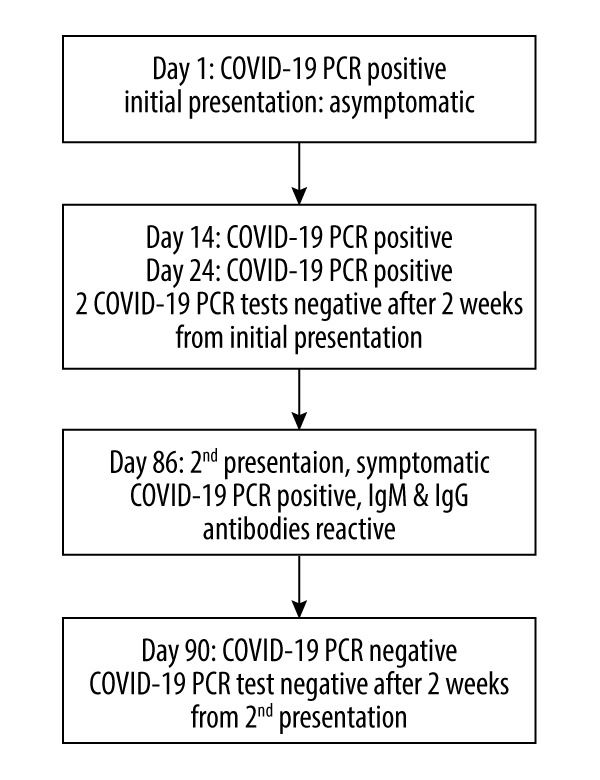
Timeline of severe acute respiratory syndrome coronavirus 2 reinfection over a period of 3 months. On day 1, the patient was found to have asymptomatic coronavirus disease 2019 (COVID-19). COVID-19 PCR samples were negative on days 14 and 24. On day 86, the patient developed symptomatic COVID-19 with reactive IgG and IgM antibodies.
IgM/IgG Antibody Test Kit by Biohit Healthcare (Hefei) Co. Ltd., which had been issued emergency use authorization by FDA, was used. Other causes of respiratory viral or bacterial illness were ruled out with a respiratory viral panel nasopharyngeal PCR test that covered influenza A and B; Middle East respiratory syndrome coronavirus; coronaviruses NL63, 229E, OC43, and HKU; parainfluenza viruses 1–4; respiratory syncytial virus; human metapneumovirus; human enterovirus and rhinovirus; Chlamydia pneumoniae; Mycoplasma pneumoniae; Bordetella parapertussis; and Bordetella pertussis. The patient was treated with azithromycin and oseltamivir during this admission. Repeated COVID-19 RT-PCR from the nasopharyngeal swab was found to be negative after 2 weeks. The patient was discharged in stable condition.
Discussion
The COVID-19 pandemic has affected countries worldwide, and governments are eager to reopen their economies. Two of the most important open questions about COVID-19 pertain to the chances of reinfection with SARS-CoV-2 and the development of long-term protective immunity against the virus. COVID-19 typically follows a course similar to other respiratory viral illnesses, and it is self-limiting in more than 80% of cases. An innate immune response involving T cells and B cells is activated, leading to the production of neutralizing antiviral antibodies. The incubation period of the disease typically varies from 5 to 10 days. The specific IgM antibody response starts to peak within the first 7 days. Specific IgG and IgA antibodies develop a few days after IgM and are hypothesized to persist at low levels, conferring lifelong protective antibodies [10] (Figure 3). While this hypothesis may hold true for symptomatic patients, emerging data have revealed negative IgM and IgG during the early convalescent phase in asymptomatic patients [8]. A seronegative status could leave open the possibility of reinfection, which seems to have happened in the case reported here. The patient’s initial infection was asymptomatic, while the reinfection occurred with symptoms. The cause for this finding is unknown, but it may be related to the viral load exposure on different occasions. We attributed the source of reinfection to community transmission because disease burden was at a peak level, with the State of Qatar having the highest number of cases per million worldwide during June 2020. This possibility emphasizes the necessity of strict public health measures when chances of reinfection could be of epidemiological importance.
Figure 3.

Possible immune response in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). SARS-COV-2 RNA and antigen are shown with dark blue; specific immunoglobulin (Ig)M, with light blue; specific IgG, with red; and specific IgA, with green. The figure depicts a peak in IgM followed by increasing IgG and IgA levels. The SARS-COV-2 RNA starts to decline after a peak in specific IgM and IgG levels. Low levels of antibodies may persist even after the convalescent phase [10].
Our case suggests that reinfection due to the novel virus is possible. To the best of our knowledge, this case is the first report of possible reinfection in the Arabian Peninsula. A case reported from Italy showed new IgM seroconversion and positive COVID-19 nasopharyngeal RT-PCR after 6 consecutive PCR tests over a period of 6 months [6]. High false-negative rates of COVID-19 RT-PCR tests have been common, which suggests that the patient in that case might have experienced a prolonged viral clearance rather than a new positive result or rein-fection [11]. However, the chance that 6 consecutive COVID-19 nasopharyngeal RT-PCR tests would be negative is less than 0.08%, so it is highly likely that the patient recovered and subsequently experienced reinfection [12]. Our case had 2 negative COVID-19 RT-PCR tests followed by a positive RT-PCR test along with detection of COVID-19 IgM and IgG 3 months after the initial positive test. This could indicate that an initial asymptomatic infection may not confer adequate long-term immune response, thus predisposing patients to reinfection. Rapid antibody tests for COVID-19 were not available at the time of the initial asymptomatic infection, which is one of the limitations of this case. A recent study suggested that for asymptomatic patients, up to 93.3% (28/30) and 81.1% (30/37) had reductions in IgG and neutralizing antibody levels, respectively, during the early convalescent phase, compared with 96.8% (30/31) and 62.2% (23/37) of symptomatic individuals [8]. These findings have further increased concerns that long-term protective immunity is not present in many patients.
In both instances, COVID RT-PCR testing was done with the Cephpeid Xpert® Xpress SARS-CoV-2 test on the GeneXpert Instrument System. A multicenter evaluation of this test revealed that it is highly specific (positive agreement 99.5% [219/220], negative agreement 95.8% [250/261]) [9]. Sample collection and handling was done in accordance with WHO guidelines for COVID-19 clinical specimen collection. The laboratory in which testing was carried out is accredited by the College of American Pathologists. Apart from the high false-negative rate of RT-PCR, other possibilities for inaccurate results include sample contamination or the presence of viral nucleic acids alone rather than the whole virus [13]. A false-positive COVID-19 RT-PCR due to any other disease is highly unlikely because the test is specific for SARS-CoV-2 RNA. In addition to a positive RT-PCR test, our case included the development of COVID-19 symptoms, radiological deterioration, and immunological evidence in terms of positive IgM and IgG antibodies. These factors seem to indicate a reinfection rather than other possibilities.
In such cases, a false-negative result could be attributable to factors such as improper sampling techniques, testing when the patient has a low viral load, and suboptimal quality control of the collected specimen. Previously, false-negative RT-PCR results have been associated with subpar sampling techniques that do not follow WHO guidelines, samples being taken when a patient is relatively less symptomatic (i.e., has a lower viral load), and unchecked quality control of the specimen [14]. To further prove the presence of reinfection, a thorough laboratory workup is needed. Materials from the nasopharyngeal swab could be inoculated on cell lines such as Vero/E6 or Vero/ hSLAM cells to prove infectivity [15]. A detailed analysis using electron microscopy, phylogenetic sequencing, and whole-genome sequencing may also provide clues about reinfection [7]. Further studies on the epidemiologic, virological, and immunological aspects of COVID-19 are required to understand the mechanisms of possible SARS-CoV-2 reinfection, viral relapse, reactivation, or inflammatory rebound.
Conclusions
The case presented here advances the discussion of whether SARS-CoV-2 reinfection is possible. A history of exposure along with positive COVID-19 RT-PCR results, seropositivity for IgG and IgM, and signs and symptoms of COVID-19 after 2 negative RT-PCR tests (over a period of 3 months) makes reinfection more likely, although viral relapse cannot be completely ruled out. Based on the available evidence, we hypothesize that asymptomatic COVID-19 infection might not confer long-term protective immunity to all patients and may predis-pose them to reinfection. A previous study on asymptomatic patients revealed neutralizing antibody status in the early convalescent phase of infection [8]. Viral relapse or reactivation might be one differential, as previously seen in a few cases [4,5]. In a community experiencing a high burden of infection, public health agencies must be alert to the possibility of reinfection from SARS-CoV-2. Although the exact incidence of reinfection is unknown, this finding may have a significant impact on public health measures. Such actions might include prolonged infection control measures along with education of infected patients (mild/asymptomatic) and health care workers regarding the possibility of reinfection in areas of high transmission. More immunological data and detailed investigation of possible cases of COVID-19 reinfection are warranted.
Acknowledgments
We thank Dr. Peter Coyle, Senior Consultant, Head of Virology, Hamad Medical Corporation (HMC) for the expert input.
Footnotes
Conflicts of Interest
None.
References:
- 1.Coronavirus Update (Live) 10,175,868 Cases and 502,869 Deaths from COVID-19 Virus Pandemic – Worldometer. https://www.worldometers.info/coronavirus/
- 2.World Health Organization (WHO) “Immunity passports” in the context of COVID-19 [Internet] Geneva: WHO; 2020. https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19. [Google Scholar]
- 3.World Health Organization (WHO) Criteria for releasing COVID-19 patients from isolation. Geneva: WHO; 2020. https://www.who.int/publications/i/item/criteria-for-releasing-covid-19-patients-from-isolation. [Google Scholar]
- 4.Gousseff M, Penot P, Gallay L, et al. Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound? J Infect. 2020 doi: 10.1016/j.jinf.2020.06.073. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lafaie L, Célarier T, Goethals L, et al. Recurrence or relapse of COVID-19 in older patients: A description of three cases. J Am Geriatr Soc. 2020 doi: 10.1111/jgs.16728. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bentivegna E, Sentimentale A, Luciani M, et al. New IgM seroconversion and positive RT-PCR test after exposure to the virus in recovered COVID-19 patient. J Med Virol. 2020 doi: 10.1002/jmv.26160. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.To KK, Hung IF, Ip JD, et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1275. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Long Q-X, Tang X-J, Shi Q-L, et al. Clinical and immunological assessment of asymptomatic SARS-CoV-2 infections. Nat Med. 2020;26(8):1200–4. doi: 10.1038/s41591-020-0965-6. [DOI] [PubMed] [Google Scholar]
- 9.Loeffelholz MJ, Alland D, Butler-Wu SM, et al. Multicenter evaluation of the Cepheid Xpert Xpress SARS-CoV-2 Test. J Clin Microbiol. 2020;58(8):e00926–20. doi: 10.1128/JCM.00926-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Azkur AK, Akdis M, Azkur D, et al. Immune response to SARS-CoV-2 and mechanisms of immunopathological changes in COVID-19. Allergy. 2020;75(7):1564–81. doi: 10.1111/all.14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lan L, Xu D, Ye G, et al. Positive RT-PCR test results in patients recovered from COVID-19. JAMA. 2020;323(15):1502–3. doi: 10.1001/jama.2020.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arevalo-Rodriguez I, Buitrago-Garcia D, Simancas-Racines D, et al. False-negative results of initial RT-PCR assays for COVID-19: A systematic review. Infectious Diseases (except HIV/AIDS) 2020;2020:20066787. doi: 10.1371/journal.pone.0242958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atkinson B, Petersen E. SARS-CoV-2 shedding and infectivity. Lancet. 2020;395(10233):1339–40. doi: 10.1016/S0140-6736(20)30868-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fang Y, Zhang H, Xie J, et al. Sensitivity of chest CT for COVID-19: Comparison to RT-PCR. Radiology. 2020;296(2):E115–17. doi: 10.1148/radiol.2020200432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alvarez-Moreno CA, Rodríguez-Morales AJ. Testing dilemmas: Post negative, positive SARS-CoV-2 RT-PCR – is it a reinfection? Travel Med Infect Dis. 2020;35:101743. doi: 10.1016/j.tmaid.2020.101743. [DOI] [PMC free article] [PubMed] [Google Scholar]