Abstract
Subtalar dislocation is defined as a separation of the talocalcaneal and talonavicular articulations, commonly caused by high-energy mechanisms, which include falls from height, motor vehicle crashes, and twisting leg injuries. The dislocations are divided into medial, lateral, anterior, and posterior types on the basis of the direction in which the distal part of the foot has shifted in relation to the talus. The most common type is medial dislocation resulted from inversion injury. Subtalar dislocation may accompany with other fractures. Physical examination must be performed carefully to assess for neurovascular compromise. Most of the subtalar dislocations can be treated with closed reduction under sedation. If this is not possible, open reduction without further delay should be conducted. After primary treatment, X-ray and computed tomography scan should be performed to evaluate the alignment and the fractures. We report a 37-year-old male patient sustained a subtalar dislocation without any bony injury when he was playing football. The patient was successfully treated by closed reduction, and a good alignment was observed at the last follow-up. The pathogenesis and treatment method of this case were analyzed, and the related literature were reviewed, which provided a reference for future clinical treatment.
Keywords: Subtalar joint, Ankle injuries, Dislocation, Trauma
Introduction
Because of the inherent stability conferred by the robust peritalar ligaments, subtalar dislocation is a rare injury that only accounts for 1%–2% of all dislocations, and is often associated with fractures of calcaneus, talus, or navicular. Prompt recognition of this injury prevents from negative sequelae associated with delayed treatment, as open reduction is often required because of anatomical impedance. Subtalar dislocation without an associated bone injury is uncommon and thus seldom reported. Also, because the relatively few studies on subtalar dislocation were performed with large number of patients, and the patients with an associated osseous injury usually included. The present case showed a subtalar dislocation occurred follow a low-energy mechanism, which also demonstrated that such injuries may be managed conservatively.
Case report
A 37-year-old male presented to the emergency department with injury of the left ankle. The patient complained of severe pain and deformity of ankle following the injury. He described that he slipped and fell, and his left foot plantar was flexed and inverted while playing soccer half an hour ago. The patient was unable to stand or walk with the injured foot. His past medical history was unremarkable. There was no history of ankle sprains or ligament laxity.
Physical and radiological examination
Clinical examination detected a deformation of his left foot: the left foot medially displaced, the talar-head was prominent dorsolaterally, and the skin stretched over the protrusion of talus without any wound. The head of the talus was palpable at the dorsolateral aspect of his ankle below the lateral malleolus. Swelling and bruising were present. The function of plantar flexion and dorsal extension were poor. Any attempt at correcting the plantarflexed position increased the pain. Dorsalis pedis pulse and posterior tibial pulse were palpable, but the sensation to light touch were poor. The blood biochemistries, chest X-ray images, and arterial blood gases were normal.
Radiographs of anteroposterior and lateral left foot were demonstrated (Fig. 1). The talocalcaneal joint and talonavicular joint were dislocated, the calcaneus dislocated medially, the talus head was upward and forward, and the tibiotalar joint remained undisturbed.
Fig. 1.
Radiographs of the left ankle demonstrated a medial subtalar dislocation without fractures.
Diagnosis
Differential diagnosis included other more common fractures and soft tissue injuries of the hind foot, such as calcaneal fracture, talar fracture, ankle fracture and ligamentous or tendinous injuries. The final diagnosis was subtalar joint dislocation (medial type).
Treatment
Under the combined spinal and epidural anesthesia, two participants are required to perform the closed reduction. The patient laid supine on a stretcher with the knee flexed to 90°, and an assistant firmly applied countertraction behind the knee to relax the gastrocnemius muscle, which increased the range of motion of the calcaneus. The first manoeuver was to apply a force in the same direction as the existing deformity, and then a traction was applied. At the same time a force in the opposite direction of the dislocation was performed, to achieve reduction of the talar-head into the concavity of the navicular.1 Reduction was achieved easily, and a good stability was found after that. After X-ray examination (Fig. 2), a short leg cast was applied after the foot was given a cold compress for 20 min every 2 h for 48 h.2 Computed tomography (CT) (Fig. 3) and magnetic resonance imaging (MRI) (Fig. 4) were performed to determine whether there were occult fractures or ligament injuries.3,4
Fig. 2.
Radiographs shows a satisfactory reduction of the medial subtalar dislocation.
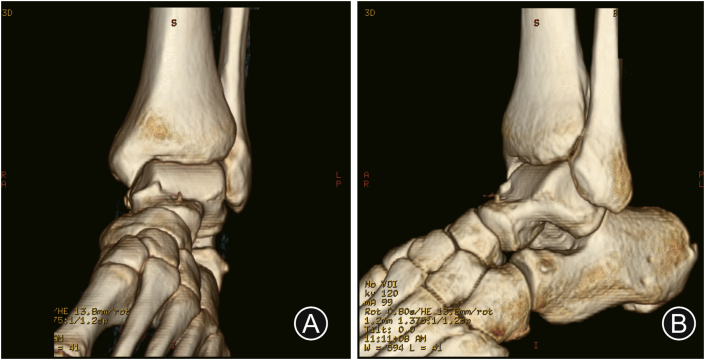
Fig. 3.
Computed tomography reconstruction demonstrates several non-displaced small fracture fragments of the talar bone with congruent ankle and subtalar joints.
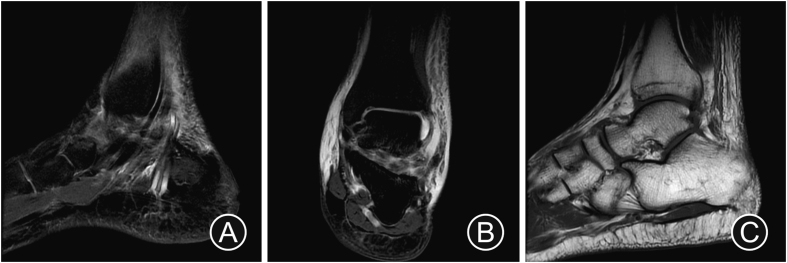
Fig. 4.
Magnetic resonance imaging demonstrated (A) the striking structure of tarsal sinus and (B) (C) the talus contusion.
Outcome and follow-up
The patient continued to be followed up in our hospital. After 2 weeks, physical examination revealed mild swelling as well as painful limited range of motion at subtalar joint. Hence, the patient was replaced with short leg tubular plaster external fixation for 2 more weeks and he was instructed to remain non-weight bearing to allow sufficient time for soft tissue healing. Thereafter, the cast was removed and active assisted range of motion exercises of ankle and foot were begun 4 weeks after injury. At the 6th week, the patient was transitioned to partial weight bearing, gradually progressing to full weight bearing as the patient's tolerance. Three months later, the follow-up examination roentgenograms showed good alignment with no evidence of avascular necrosis. The patient had normal passive and active range of motion. He has returned to full sport activity without pain, swelling, or instability. The American Orthopaedic Foot and Ankle Society Ankle-hindfoot score was 96.
Discussion
Subtalar joint dislocation is defined as a simultaneous dislocation of both subtalar (talocalcaneal) and talonavicular joints, but tibiotalar and calcaneocuboid joints remain undisturbed. The incidence is low, and it is easy to be confused with ankle dislocation, which accounts for about 1% of total joint dislocation.5, 6, 7 Rarity of this injury can be attributed to the strong ligaments connecting the talus and the calcaneus, the strong biomechanical properties of the ankle and the tight joint capsule.8 Most of the literature on this rare injury consists of isolated case reports rather than large case series, based on a PubMed literature search within the past 10 years.
The first literature reported this rare injury dates back to the year 1803. This is a condition that mainly affects young men and the right lower limb. Common causes are high-energy trauma, such as road traffic accident or fall from height. It is also commonly accompanied by fractures of the malleoli, talus or fifth metatarsal. Different force directions applied to the foot may lead to different types of dislocation.1 Medial subtalar dislocation occurs when a forceful inversion injury to the forefoot causes the talus to pivot on the sustentaculum tali, stressing the subtalar and talonavicular joints.2 The mechanism for medial subtalar dislocation is forceful inversion of the foot blocked on the ground causing ligament tears in a specific chronological manner. Firstly, the dorsal talonavicular ligament is injured, then the two interosseous ligaments and finally the calcaneofibular ligament. The lateral dislocation begins with the foot eversion. First a deltoid ligament rupture occurs, then a disruption of the interosseous ligament and the talo-calcaneal joint followed by dorsal talo-navicular ligament failure.9 Lateral dislocation often leads to injury of the posterior tibial tendon and vascular nerve, so the trauma is more serious. Medial dislocation is more common than lateral dislocation.8,10 Biomechanical studies show that the metatarsal flexion of the joint around the talus allows less energy storage and is more vulnerable to violence than the dorsal flexion. A violence above the level of ankle joint is an indirect violence to the foot varus complex. If there is an energy transfer process in the injury of the foot ligamentous complex, the energy storage of bone tissue is less than that of ligament tissue. Violence can lead to the release of energy from the injury of bone structure. Therefore, it does not cause dislocation around talus. Only when low-level violence directly acts on the tense ligament tissue around the talus, the ligament tissue will be damaged by the released energy, and the dislocation around the talus will occur. Rapid loading of violence is more likely to cause ligament tissue damage and dislocation.
Apart from obvious trauma history and local swelling, pain and functional limitation after injury, tarsometatarsal joint dislocation often presents varus or valgus deformity, sometimes with skin cyanosis and sensory numbness. Positive, lateral and oblique X-ray films of feet should be taken, because CT scanning is necessary to make the further diagnosis. The articular surface of talus and calcaneus is divided into anterior, middle and posterior parts, but not every subtalar joint has the three parts. During development, the anterior and middle parts of the subtalar joint are fused into anterior joints, which make the subtalar joint consist of only two saddle-like articular surface tissues. This is the internal instability factor of the subtalar joint. The external stability of the subtalar joint depends on the ligaments, tendons and capsules around the joint, among which ligaments play a key role. The ligaments around the joint mainly include talonavicular ligament, anterior talofibular ligament, calcaneofibular ligament, posterior talofibular ligament and triangular ligament.11 When the dislocation around talus is accompanied by foot varus, the anterior talofibular ligament can be broken first, and then the inter-talofibular ligament can be broken or relaxed, and after that the talofibular ligament can be broken.
In order to avoid soft tissue and vascular complications, early diagnosis, clear dislocation type, early reduction are key factors for the treatment of subtalar joint dislocation, which provided an important basis for the treatment. Once the diagnosis of fresh closed dislocation was confirmed, a manual reduction should be performed at first, in order to avoid damaging the blood supply around talus, to reduce the compression and necrosis of ankle skin or nerve and to avoid blood vessel injury, and the joint will become stable after reduction.12,13 After successful reduction, concurrent fractures should be treated at the same time. Although closed reduction of the peripheral talus joint is easy to success, there is still a failure rate of about 20%, and manual reduction of lateral dislocation is more difficult to success.14 Failure of closed reduction is often due to other injuries, including: (1) the talar head is buttonholed through the extensor retinaculum or the extensor digitorum brevis; (2) the talus is entrapped and impacted on the navicular due to a fracture of the talus; (3) the talar head is entrapped by the peroneal or posterior tibial tendons.
Regardless of the method of reduction, the subtalar joint is usually stable after closed or open treatment and does not require internal fixation. Although the injury is stable (unlikely to re-dislocate), ligament healing requires strict immobilization. Therefore, it is recommended that the patient should be placed in cast.
The blood supply of talus is complex. Gelberman and Murfinger15,16 found that the blood supply of talus body came from tarsal canal artery (posterior tibial artery branch), deltoid branch (posterior tibial artery branch) and tarsal sinus artery formed by anterior tibial artery and perforating branch of peroneal artery. The blood supply of talus head came from the branches of dorsal pedal artery and tarsal sinus artery. Tarsal sinus artery, tarsal canal artery and triangular branch are the most important blood vessel sources of talus, which is consistent with Miller's experimental results.17 When the anterior tibial artery was damaged by talus neck fracture, the branches of posterior tibial artery, especially the deltoid branch, can still provide a large amount of blood supply, thus avoiding the occurrence of talus avascular necrosis to some extent.7 Because the talus did not dislocate from the ankle joint, the vessel that the anterior articular capsule of the ankle entered the talus body and the vessel below the medial articular surface of the ankle were retained. As long as the talus could be positioned in time, there would be no talus avascular necrosis.
According to the follow-up results, the patients who were easy to reposition had good curative effect; those with intra-articular fracture may lead to traumatic arthritis or fracture of adjacent bone and long-term braking may cause stiffness of subtalar joint.7 Traumatic arthritis mainly occurs in subtalar joint. The talus-navicular joint and the tibial-talus joint are relatively rare. According to the literature, the incidence rate of traumatic arthritis is about 63%, especially in the cases of intra-articular fracture, and also can occur in the simple joint dislocation cases.18,19 Open dislocation patients had poor curative effect. The causes of pain in subtalar joint are related to articular cartilage injury, subtalar intra-articular fracture, traumatic arthritis and instability of subtalar joint. Lateral dislocation has a high incidence of complications, mainly due to severe trauma and associated bone or cartilage injury. For those who are prone to ischemic necrosis of talus, the weight-free time should be prolonged after operation, and the changes of talus should be observed. If the talus cannot be improved and the articular surface collapses, joint fusion should be used when there is pain.
In conclusion, for the treatment of closed subtalar dislocation, urgent closed manual reduction should be performed as soon as possible under anesthesia to reduce the occurrence of early or late complications, and the successful rate of manual reduction is high.20,21 CT is recommended to assess for the fractures and joint congruity.22 For those who have not succeeded in closed reduction or incomplete reduction, open reduction should be performed in time to restore the anatomical integrity of the subtalar joint, obtain accurate joint alignment and avoid sequelae. Excellent results are generally obtained for simple dislocations without associated injuries after treatment and a short period of immobilization. In contrast, dislocations with associated injuries including fractures usually result in poor outcomes and a high incidence of complications such as stiffness or degenerative changes.9
Funding
Nil.
Ethical Statement
The patient involved in this study gave his verbal informed consent authorizing use and disclosure of his protected health information.
Declaration of Competing Interest
The authors declare that they have no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Medical Association.
References
- 1.Macey A.R., Grama C. An ankle that just didn't look right. BMJ. 2016;354:1–3. doi: 10.1136/bmj.i5056. [DOI] [PubMed] [Google Scholar]
- 2.De Palma L., Santucci A., Marinelli M. Clinical outcome of closed isolated subtalar dislocations. Arch Orthop Trauma Surg. 2008;128:593–598. doi: 10.1007/s00402-007-0459-8. [DOI] [PubMed] [Google Scholar]
- 3.Biz C., Ruaro A., Giai Via A. Conservative management of isolated medial subtalar joint dislocationsin volleyball players: a report of three cases and literature review. J Sports Med Phys Fit. 2019;59:1739–1746. doi: 10.23736/S0022-4707.19.09531-8. [DOI] [PubMed] [Google Scholar]
- 4.Zaraa M., Jerbi I., Mahjoub S. Irreducible subtalar dislocation caused by sustentaculum tali incarceration. J Orthop Case Rep. 2017;7:58–60. doi: 10.13107/jocr.2250-0685.688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benabbouha A., Ibou N. Rare case of pure medial subtalar dislocation in a basketball player. Pan Afr Med J. 2016;23:106. doi: 10.11604/pamj.2016.23.106.8848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prada-Cañizares A., Auñón-Martí I., Vilá Y Rico J. Subtalar dislocation: management and prognosis for an uncommon orthopaedic condition. Int Orthop. 2016;40:999–1007. doi: 10.1007/s00264-015-2910-8. [DOI] [PubMed] [Google Scholar]
- 7.Flippin M., Fallat L.M. Open talar neck fracture with medial subtalar joint dislocation: a case report. J Foot Ankle Surg. 2019;58:392–397. doi: 10.1053/j.jfas.2018.08.049. [DOI] [PubMed] [Google Scholar]
- 8.Giannoulis D., Papadopoulos D.V., Lykissas M.G. Subtalar dislocation without associated fractures: case report and review of literature. World J Orthoped. 2015;6:374–379. doi: 10.5312/wjo.v6.i3.374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Veltman E.S., Steller E.J., Wittich P. Lateral subtalar dislocation: case report and review of the literature. World J Orthoped. 2016;7:623–627. doi: 10.5312/wjo.v7.i9.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoexum F., Heetveld M.J. Subtalar dislocation two cases requiring surgery and a literature review of the last 25 years. Arch Orthop Trauma Surg. 2014;13:1237–1249. doi: 10.1007/s00402-014-2040-6. [DOI] [PubMed] [Google Scholar]
- 11.Tochigi Y., Takahashi K., Yamagata M. Influence of the interosseous talocalcaneal ligament injury on stability of the ankle-subtalar joint complex -a cadaveric experimental study. Foot Ankle Int. 2000;21:486–491. doi: 10.1177/107110070002100607. [DOI] [PubMed] [Google Scholar]
- 12.Nanjayan S.K., Broomfield J., Johnson B. Total dislocation of the talus: a case report. Foot Ankle Spec. 2014;7:71–73. doi: 10.1177/1938640013507105. [DOI] [PubMed] [Google Scholar]
- 13.Yaoici F., Coskun M., Arslan M.C. Open reduction of a total talar dislocation: a case report and review of the literature. World J Clin Cases. 2019;7:1850–1856. doi: 10.12998/wjcc.v7.i14.1850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gaba S., Kumar A., Trikha V. Posterior dislocation of subtalar joint without associated fracture: a case report and review of literature. J Clin Diagn Res. 2017;11:RD01–RD02. doi: 10.7860/JCDR/2017/27794.10553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gelberman R.H., Mortensen W.W. The arterial anatomy of the talus. Foot Ankle. 1983;4:64–72. doi: 10.1177/107110078300400204. [DOI] [PubMed] [Google Scholar]
- 16.Mulfinger G.L., Trueal J. The blood supply of the talus. J Bone Joint Surg. 1970;52:160–167. PMID: 5436202. [PubMed] [Google Scholar]
- 17.Miller A.N., Prasarn M.L., Dykel P. Quantitative assessment of the vascularity of the talus with godolinium-enhanced magnetic trsonance imaging. J Bone Joint Surg. 2011;93:1116–1121. doi: 10.2106/JBJS.J.00693. [DOI] [PubMed] [Google Scholar]
- 18.Camarda L., Abruzzese A., attuta G., L A. Results of closed subtalardislocations. Musculoskelet Surg. 2016;100:63–69. doi: 10.1007/s12306-015-0380-1. [DOI] [PubMed] [Google Scholar]
- 19.Ohl X., Harisboure A., Hemery X., Dehoux E. Long-term follow-up after surgical treatment of talar fractures:twenty cases with an average follow-up of 7.5 years. Int Orthop. 2011;35:93–99. doi: 10.1007/s00264-009-0930-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karampinas P.K., Kavroudakis E., Polyzois V. Open talar dislocations without associated fractures. Foot Ankle Surg. 2014;20:100–104. doi: 10.1016/j.fas.2013.12.005. [DOI] [PubMed] [Google Scholar]
- 21.Weston J.T., Liu X., Wandtke M.E. A systematic review of total dislocation of the talus. Orthop Surg. 2015;7:97–101. doi: 10.1111/os.12167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramzan M.M., Fadl S.A., Sandstrom C.K. Core curriculum case illustration: medial peritalar dislocation. Emerg Radiol. 2018;25:329–330. doi: 10.1007/s10140-017-1499-1. [DOI] [PubMed] [Google Scholar]