Abstract
Acetabular cup optimum position is paramount for total hip arthroplasty (THA) good outcomes. Although controversial, Lewinnek proposed safe zone for cup placement still the most widely accepted target. Cup placement can be improved using specific anatomical landmarks, computer navigation system and handheld navigation devices. As using a smartphone on daily bases became popular among orthopedic surgeons, in this technical note, we describe how to use smartphone specific applications intraoperatively during total hip arthroplasty to adjust cup inclination angle, which we believe to be easy, cheap and beneficial for young less experienced surgeons.
Key Words: Cup, Inclination, Smartphone, THA
Introduction
Dislocation after primary THA reported to occur on average between 0% and 5% (1). Optimal cup inclination, which is under surgeon control, improves longevity as well as reduces the dislocation incidence after THA (2).
Lewinnek et al. recommended cup inclination and anteversion angles of 40º±10 and 15º±10, respectively, as the cup placement safe zone (3). However, inconsistent results with variations in cup placement within this safe zone ranging from 25.7% to 70.5% had been reported when using the freehand technique for cup placement considering floor level as a reference (4). This lead to the development of new technologies to improve cup placement accuracies such as computer-assisted surgery (CAS) and handheld navigation system, however, increased cost and limited availability among the concerns (5).
With the popularity of smartphones and its use among orthopedic surgeons, using it for cup placement optimization during THA had been reported by some authors (6, 7).
The purpose of this technical note is to describe how we used smartphone spirit level application intraoperatively during THA to adjust the cup inclination angle.
Technical Note
Written Informed consent (using an intraoperative smartphone was explained and included) was signed by all patients before surgery as issued and required by our department.
Spirit level application which is combined with the compass app in I phone 6 (Apple, Cupertino, CA, USA) was used as well as a free downloadable application (Bubble Level, Spirit Level, version 3.24, NixGame) for Android platform based smartphones and a Protractor app for angles measurement. Spirit level applications use the horizontal floor line as a 0° reference point, so when the smartphone is tilted, the application will show the degree of the tilting angle. The smartphone is placed in a gas plasma sterilized zip plastic bag (Snap & Seal; Classic consumer products, INC., Englewood, US) [Figure 1A].
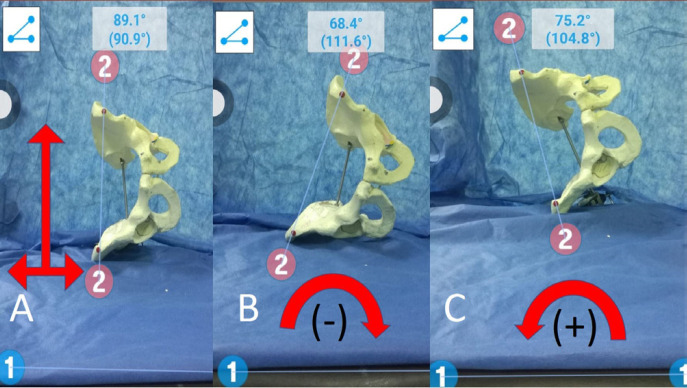
Figure 1.
Instrument used, table, and patient position adjustment
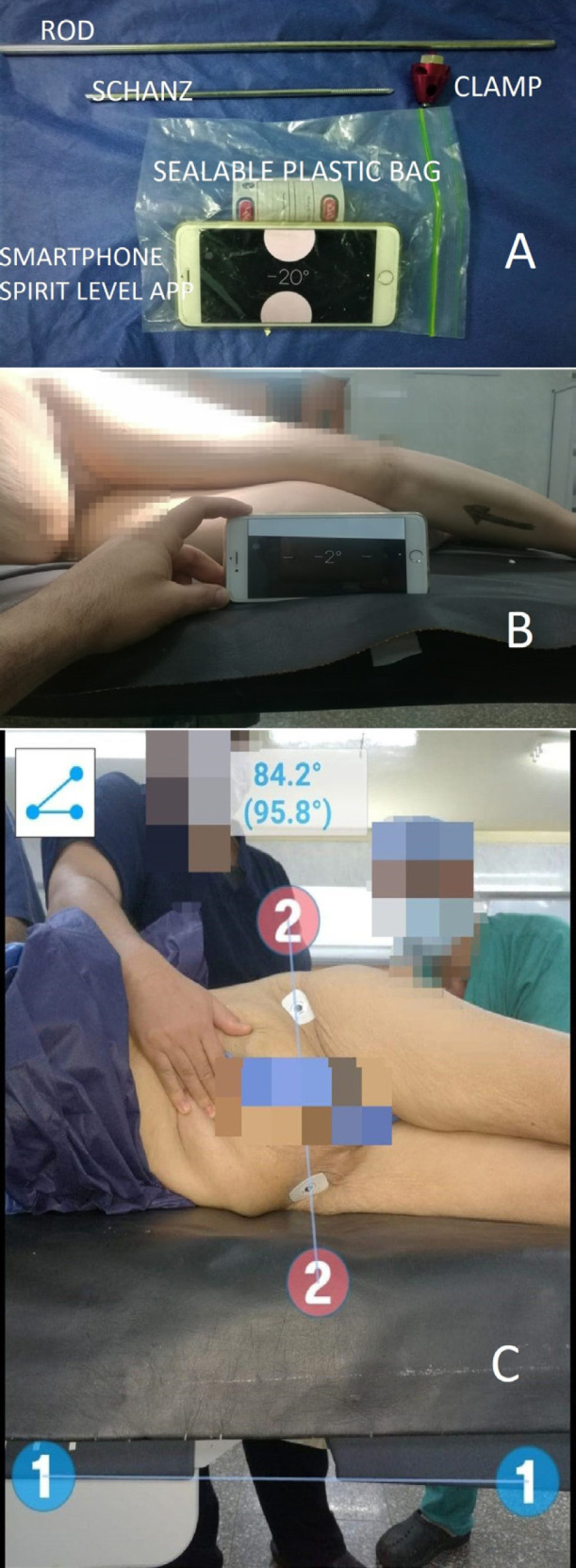
A: Instrument used during surgery (Schanz, rod, clamp, and smartphone enclosed inside a sealable sterilizable plastic bag with the spirit level application shown.
B: Adjusting the table level to 0˚ using the spirit level application (to be parallel to the floor level)
C: Measuring the amount of pelvic tilt after patient positioning as the angle between the line connecting ASIS bilaterally (line 2) and a line representing the table level (line 1).
Under spinal anesthesia (unless contraindicated according to anesthesia opinion) using a standard operative table, the approach to the hip was a modified direct lateral approach with the patient in a lateral decubitus position. Before the final positioning of the patient on the table, the spirit level app was used to make sure that the table is leveled with the floor and is set to 0° [Figure 1B]. Two marks created over the anterior superior iliac spine (ASIS) bilaterally then the patient was turned to the desired position with one support over the sacrum posteriorly, before securing the anterior support the camera function of the Protractor app was used to measure the angle between line connecting the two ASIS marks and the table level to detect the amount of pelvic tilt after the patient is turned to the lateral decubitus position [Figure 1C], the pelvic tilt was considered 0 if both lines are perpendicular (which is not always happening), however, if the pelvis was tilted toward the head of the patient which means that the angle will be more than 90 we considered it as a positive tilt, if the opposite occurs we considered it as a negative tilt, the measured value of the pelvic tilt will be taken in consideration when adjusting the inclination of the cup as what will be explained later [Figure 2].
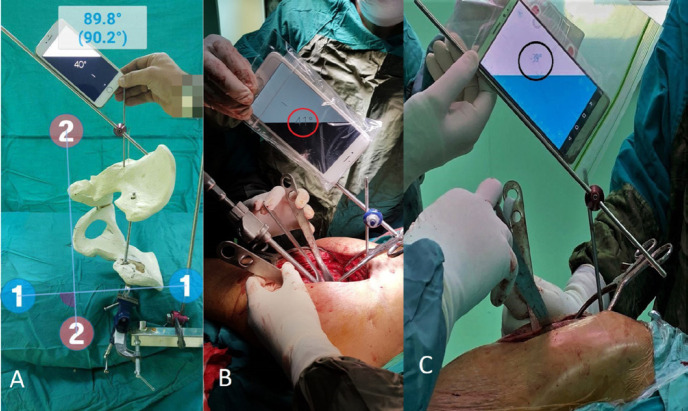
Figure 2.
Demonstration on a saw bone pelvic model showing different directions of pelvic tilt
A: the pelvis is squared to the table (ASIS line is perpendicular to table level line)
B: the pelvis is tilted toward the feet of the patient (angle between ASIS line and table level line is less than 90˚= 68.4˚)
C: the pelvis is tilted toward the head of the patient (angle between ASIS line and table level line is more than 90˚ =104.8˚)
After performing the initial neck cut and following full exposure of the acetabulum, a supraacetabular 4 mm Schanz screw (from the trauma external fixator set) is inserted about one centimeter proximal to the superior acetabulum ridge (no need to enlarge the approach), it should be superior enough not to penetrate the acetabulum, then a rod is attached to the Schanz screw with a clamp. Before securing the clamp, the angle of the rod (which will act as a guide for further reaming and cup placement) is adjusted to the desired cup inclination angle using the spirit level app which we decided to be 40 degrees (within the safe zone) in all cases taking into account the measured pelvic tilt (for example if the pelvis is titled +5 degrees we will adjust the angle to 45 instead of 40 degrees and vice versa) [Figure 3]. Then preparation of the acetabulum is started with the reamer handle being parallel to the supra-acetabular rod. Before the final reamer, the angle of the rod is re-checked using the spirit level app and the parallelism of the reamer with the rod is checked using the protractor app by the circulating nurse and the value was recorded, anteversion was adjusted using the transverse Acetabular ligament (TAL) as a reference, after finishing reaming and trailing, the cup is placed with its handle parallel to the supraacetabular rod [Figure 4].
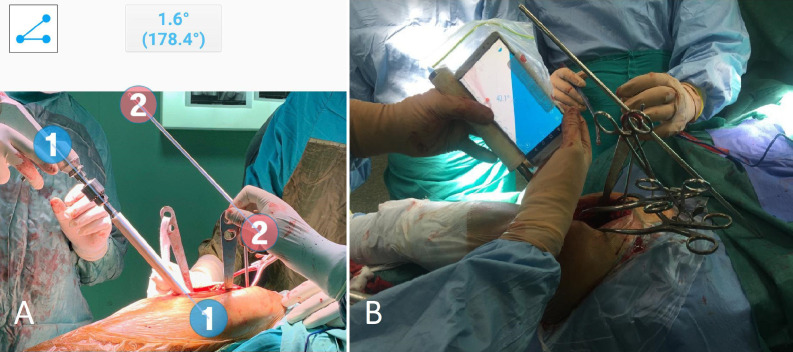
Figure 3.
Demonstration of how the technique work
A: saw bone model showing the pelvis squared to the table (inter-ischial line “line 2” is perpendicular to table level line “line 1”), the supraacetabular rod is adjusted to 40˚ using smartphone spirit level application. Intraoperative images are showing using different types of smartphone applications, B: iPhone spirit level app. And C: android platform based smartphone bubble level app.
Figure 4.
Acetabulum preparation and final cup placement
A: acetabulum reaming being performed with the reamer parallel to the supraacetabular rod
B: final check before the real cup impaction with the smartphone is being put on the cup introducer.
Post-operative assessment
Postoperative cup inclination was measured in a standard pelvic AP radiographs as the angle between the trans-ischial line as a horizontal reference and a second line connecting the superolateral and inferomedial edge of the cup representing its long axis using (IC measure Digital software, The Imaging Source Europe GmbH, Bremen, Germany) [Figure 5].
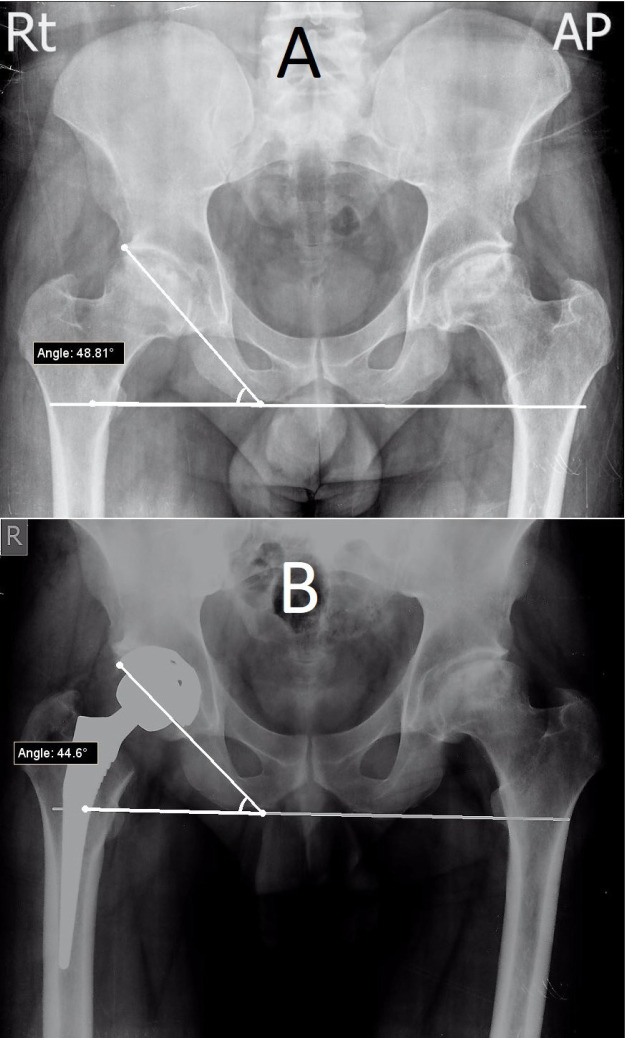
Figure 5.
Male patient 45 years old with bilateral hip AVN, right side treated by Cementless THA
A: preoperative native cup inclination angle
B: postoperative cup inclination angle measured between interischial line and line of the cup
The initial results after using this technique in 15 consecutive patients done by the youngest, less experienced surgeon (A. A. K.) were as follows: patients diagnosed preoperatively as five primary hip osteoarthritis, five rheumatoid arthritis of the hip, three avascular necrosis and two patients with fractured neck of the femur. The implant used were cemented cups (ZCA all-poly cups by Zimmer, Warsaw, Indiana, USA) in 8 cases and cementless cups (Pinnacle by DePuy, Warsaw, Indiana, USA) in 7 cases. The average measured preoperative pelvic tilt was 6 degrees (range +7: -5), The average postoperative cup inclination measured on pelvis AP plain radiograph was 43° (range, 33°:52°). We reported no wound complications at the time of stitches removal after two weeks.
Discussion
Optimum position and alignment of the cup are some of the most critical and essential technical issues in THA (2). Since poor cup positioning is related to poor results associated with the increased risk of instability, accelerated wear, adverse local tissue reactions, and limited range of motion (4).
Although safe zone for cup placement described by Lewinnek et al. is the most acceptable target, however, it is still a controversial issue (3, 4).
In a study by Pongkunakorn et al. where they compared cup orientation in 2 groups of patients done by the same surgeon, they used smartphone applications in one prospective group to help accurate cup placement; the other was a retrospective group done using the usual mechanical guides, in the smartphone group, more cups were placed in the Lewinnek safe zone (90.2% vs. 56.1%, p<0.001), they concluded that using smartphone during surgery could improve the accuracy of cup placement (6).
We found using smartphone apps technique as efficient as what had been reported in the previous study, Nevertheless, we felt that our technique was less challenging and more surgeon friendly than Pongkunakorn et al. as they used intra-operative Fluoroscopy which culminated in longer operating time as well as inserting a pin in the ASIS outside the surgical approach, the authors admitted the technical complexity and the need for a learning curve to make the surgeon familiar with these instrument to get a good result (6).
In a prospective case series by Peters et al. where they used the accelerometer and camera feature of an iPhone in a level indicator and protractor application for cup placement in 50 patients, they placed all the cups within the Lewinnek safe zone, the difference between the preoperative, intraoperative, and postoperative acetabular inclinations was less than 5% (7).
In a study by Kurosaka et al., they were able to achieve reasonable cup positioning in five cadavers using the iPhone/ iPad technique for cup placement irrespective of the level of surgeon experience (8).
In the previous two studies, when using the body axis as a guide for cup inclination, the cup was placed with the assumption that the pelvis is in a neutral position. However, when the patient in a lateral decubitus position the pelvis proved to have various degrees of tilt. To eliminate this unattended effect of pelvic tilt on the cup placement after patient positioning, we tend to measure the amount of this tilt before draping and considering this when calculating the desired final cup inclination according to the degree of the tilt (9).
The pelvic tilt change was clinically proved in a study by Hill et al., where they reported a 12.7° difference between the intended intraoperative cup inclination and the resultant postoperative radiographic measured inclination; They attributed this change to the unnoticed pelvis adduction after patient positioning (10).
This technique got some limitation, as it doesn’t help with adjustment of the cup version, also the possibility of measurement fallacies which may occur with miss interpretation of the angles on the spirit level apps.
We believe from our early results that using intraoperative smartphone specific applications can be of great help for young and less experienced surgeons in optimizing the cup inclination during THA. However, another technical aspect to improve the outcome should be taken into consideration.
References
- 1.Delaunay C, Hamadouche M, Girard J, Duhamel A. What are the causes for failures of primary hip arthroplasties in France? Clinical orthopaedics and related research. 2013;471(12):3863–9. doi: 10.1007/s11999-013-2935-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ha Y-C, Yoo JJ, Lee Y-K, Kim JY, Koo K-H. Acetabular Component Positioning Using Anatomic Landmarks of the Acetabulum. Clinical Orthopaedics and Related Research®. 2012 ;470(12):3515–23. doi: 10.1007/s11999-012-2460-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978 ;60(2):217–20. [PubMed] [Google Scholar]
- 4.Callanan MC, Jarrett B, Bragdon CR, Zurakowski D, Rubash HE, Freiberg AA, et al. The John Charnley Award: risk factors for cup malpositioning: quality improvement through a joint registry at a tertiary hospital. Clinical orthopaedics and related research. 2011;469(2):319–29. doi: 10.1007/s11999-010-1487-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morgenstern R, Su EP. Handheld navigation for direct anterior total hip arthroplasty. Seminars in Arthroplasty. 2018 ;29(3):153–6. [Google Scholar]
- 6.Pongkunakorn A, Chatmaitri S, Diewwattanawiwat K. Use of smartphone to improve acetabular component positioning in total hip athroplasty: A comparative clinical study. Journal of orthopaedic surgery (Hong Kong) 2019;27(1):2309499019825578. doi: 10.1177/2309499019825578. [DOI] [PubMed] [Google Scholar]
- 7.Peters FM, Greeff R, Goldstein N, Frey CT. Improving Acetabular Cup Orientation in Total Hip Arthroplasty by Using Smartphone Technology. The Journal of Arthroplasty. 2012 ;27(7):1324–30. doi: 10.1016/j.arth.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Kurosaka K, Fukunishi S, Fukui T, Nishio S, Fujihara Y, Okahisa S, et al. Assessment of Accuracy and Reliability in Acetabular Cup Placement Using an iPhone/iPad System. Orthopedics. 2016;39(4):e621–6. doi: 10.3928/01477447-20160610-05. [DOI] [PubMed] [Google Scholar]
- 9.Kanazawa M, Nakashima Y, Ohishi M, Hamai S, Motomura G, Yamamoto T, et al. Pelvic tilt and movement during total hip arthroplasty in the lateral decubitus position. Modern Rheumatology. 2016 ;26(3):435–40. doi: 10.3109/14397595.2015.1092914. [DOI] [PubMed] [Google Scholar]
- 10.C HJ P, GD , R , P E BD. Photographic measurement of the inclination of the acetabular component in total hip replacement using the posterior approach. The Journal of Bone and Joint Surgery . 2010;92-B(9):1209–14. doi: 10.1302/0301-620X.92B9.24476. [DOI] [PubMed] [Google Scholar]