Abstract
Proximal interphalangeal (PIP) fracture-dislocation is a relatively common injury that results from “jamming” a finger. Treatment hinges on the degree of articular surface involvement, which determines stability of the joint. For unstable injuries, a variety of surgical interventions have been described including extension block pinning, open reduction internal fixation, volar plate arthroplasty, static or dynamic external fixation, and hemi-hamate reconstruction. We present the case of an unstable, subacute ring finger PIP dorsal fracture dislocation for which the above options were not possible or desirable to the patient.
We performed temporary bridge plate fixation of the joint, based on the success of a similar procedure used to treat comminuted and unstable distal radius fractures.
The procedure allowed immediate return to work, which was the patients’ primary goal, and resulted in a reasonable short-term outcome, similar to other mentioned procedures.
Temporary bridge plate fixation can be considered among treatment choices for PIP fracture dislocation when other, more established options are not possible or desirable.
Key Words: Bridge plating, PIP fracture dislocation, Proximal interphalangeal joint
Introduction
Proximal interphalangeal joint (PIP) fracture dislocations can occur from “jamming” a finger which causes a hyperextension moment and axial load across the PIP. The injury typically results in a middle phalanx volar base fracture with dorsal joint subluxation. Depending on the degree of articular surface involvement and ligament disruption, the injury can display varying degrees of stability. Hastings and Carroll classified injuries with a fracture involving less than 30% of the joint surface as stable (1). The PIP joint becomes potentially unstable with joint involvement between 30-50%, while fractures involving more than 50% are inherently unstable by virtue of the loss of the volar bony buttress to dorsal translation.
For unstable injuries, a number of well recognized surgical treatments have been studied, but with no clear consensus as to the most effective (2). Surgical techniques include extension block pinning, closed reduction and pinning, open reduction internal fixation, volar plate arthroplasty, static and dynamic external fixation, and hemi-hamate reconstruction. The common goals of treatment are: 1) maintain a concentric PIP joint, and 2) provide stability for early range of motion exercises to mitigate against joint stiffness. Outcome studies, in general, show some degree of permanent finger stiffness and progressive joint degeneration (1, 3-6).
We present the case of a 58-year-old plumber with a sub-acute presentation of an unstable PIP dorsal fracture dislocation for whom the above surgical options were not possible or desirable. The patient is an independent contractor and his top priority was to minimize time off from work. He was not willing to tolerate exposed K-wires, obtrusive splints, prolonged therapy, or post-op precautions and donor site morbidity of the hemi-hamate procedure. Based on these concerns we offered him: (1) buddy taping and delayed arthrodesis if necessary, or (2) a novel technique of temporary PIP bridge plating, which would allow immediate post-operative use of the finger without exposed hardware or a large splint. The caveats of finger stiffness, continued PIP degeneration, and the necessity of a second surgery for hardware removal were discussed. Given the potential to salvage the joint and continue working, he opted for bridge plating.
Case presentation
A 58-year-old plumber injured his non-dominant ring finger falling backwards down a flight of stairs 3 weeks prior to presentation. He had persistent PIP pain and swelling, but continued to work full time. Radiographs demonstrated a comminuted, impacted fracture of the middle phalanx volar base with dorsal subluxation. Approximately 75% of the joint surface was fractured, with a large central radial articular fragment impacted 5 millimeters [Figure 1]. Active PIP motion was 20-40 degrees with painful crepitus. Distal interphalangeal joint (DIP) motion demonstrated 20 degrees hyperextension to 30 degrees of flexion.
Figure 1.
PIP fracture dislocation; 75% of joint surface impacted
In the operating room, under a regional block, a closed reduction was attempted. The middle phalanx would not come fully out to length, indicating contracture of the ligaments and joint capsule, as expected. A dorsal curvilinear incision was made over the PIP joint. Through windows between the central slip and lateral bands, the collateral ligaments were released from their origins. Nascent fibrous scar tissue was excised from under the central slip allowing a concentric, yet unstable, PIP reduction. The joint was temporarily transfixed with a 1.6mm Kirschner wire in a concentric position, in 30 degrees of flexion. Slight flexion was chosen so the joint would be in a functional position in the event he was not able to generate much motion after removal of the hardware. The volar base fracture fragments were percutaneously disimpacted with a blunt tip K-wire.
An explicit goal of the surgery was to limit extensor tendon adhesions, so manipulation of the tendon complex was minimized and the locking plate was fixed 1-2 millimeters off of the tendon so as not to compress it. A Medartis 1.5 mm, 8 hole grid plate was contoured to sit on the dorsal and radial aspects of the PIP to achieve fixation in 2 planes. After drilling through stab incisions in the tendon, 4 bicortical locking screws were placed on either side of the joint [Figures 2-6]. The K-wire was removed and the joint was found to be stable with stress maneuvers under fluoroscopy. The skin was closed and a bulky dressing applied.
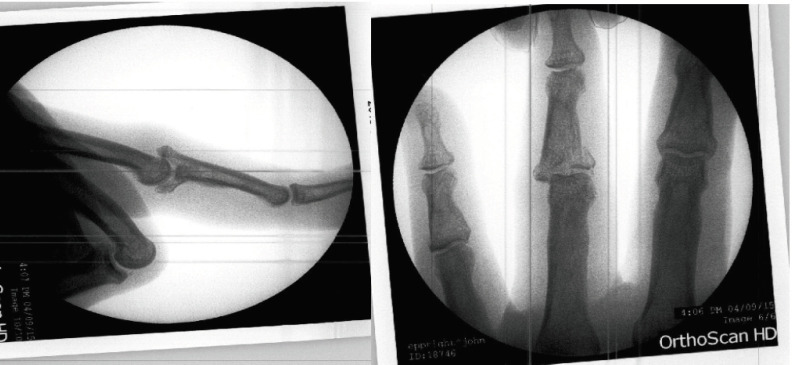
Figure 2-6.
AP, Lateral and oblique radiographic views of bridge plate spanning the PIP joint
The patient returned to the office 3 days later where a PIP volar gutter splint was fabricated (MP and DIP free). He was allowed to return to work, full duty, being mindful to keep his incision clean and dry. The patient was pleased with the pain relief and his ability to squeeze a pipe wrench and tighten plumbing fixtures. Eight weeks post-op he stopped wearing the splint. At ten weeks from surgery, the patient returned to the operating room for removal of the plate, under local anesthesia with epinephrine and no tourniquet (WALANT). The hardware was removed easily. We performed a tenolysis of the lateral bands and central slip, as well as a partial release of the radial collateral ligament to achieve 10 – 80 degrees of active PIP motion. Active DIP motion was from 0-30 degrees. Flouroscopy showed the joint to be concentric over the entire range of motion. Immediate hand therapy was prescribed but the patient did not attend. He returned to work 2 days later. At 2 weeks post op, X-rays show subchondral irregularity, joint space narrowing, and some widening of the middle phalanx base [Figures 7-9]. He was subsequently lost to follow up. At 9 months from surgery, by phone interview, the patient reported the finger is “stiff but usable” and without pain.
Figure 7-9.
Radiographs 2 weeks post-removal of the bridge plate
Discussion
Unstable PIP fracture dislocations continue to be a vexing problem for the hand surgeon with no clear “gold standard” treatment and mixed outcomes, with many studies showing some residual joint contracture and progressive degenerative changes despite adequate treatment (1, 8). Treatment principles however, are clear—obtain a concentric joint with enough stability to permit a normal gliding arc of motion. Conversely, subluxed PIP joints move by hinging at the fracture edge and lead to progressive joint degeneration and poor functional outcomes (9-11). Various treatments have been advocated, but due to lack of comparative studies, treatment is largely based on the experience and personal preference of the treating surgeon.
When the fracture is comminuted and encompasses >50% of the articular surface, traction devices and hemi-hamate reconstruction are appropriate choices. Traction device outcomes have been reported in multiple studies with an average final PIP arc of motion from 66-80% and good grip strength, though superficial pin tract infections were common and up to 61% showed progressive degenerative changes (12, 6, 13). More recently, hemi-hamate reconstruction has been lauded as the “go-to” for the most difficult fracture dislocations to treat. In a recent systematic review of 71 hemi-hamate reconstructions with a mean follow up of 36 months, PIP arc of motion was 77O and few patients complained of pain or stiffness. There was, however, a 35% complication rate and up to 50% showed radiographic signs of osteoarthritis (14).
A dynamic wireframe external fixator or hemi-hamate reconstruction were recommended to our patient. However, he refused to have exposed wires or the splinting/restrictions required to rehab the hemi-hamate procedure. His only goal was to continue working, even at the expense of a deformed, stiff, and arthritic finger. Based on prior positive experiences with bridge plating of distal radius fractures, a bridge plate technique was offered as an alternative which would allow immediate use of the hand with minimal immobilization. Since expectant management would likely yield a painful, stiff PIP ultimately requiring arthrodesis or replacement, we decided to proceed with this new application of a proven technique.
There were some unknowns to consider. Would the plate construct be strong enough to support everyday use of the hand? As any hardware failure would result in re-dislocation, we chose to additionally support the finger with a small volar gutter PIP splint for protection. The patient was able to work as a plumber while wearing the splint. Also, we chose to use a grid plate, which allowed biplanar fixation. Logically, this would provide more support than a unilateral plate. The 1.5mm plate system had the right compromise of strength and small profile. In fact, just prior to plate removal, the patient developed skin sensitivity over the distal edge of the plate indicating the possibility of skin breakdown if a larger plate were used. A locking plate system is critical for stability across the joint and to prevent compression of the tendon. A plate placed on the lateral aspect of the joint could have been placed under the extensor mechanism but we feel our construct was stronger since it fixed the joint in 2 planes and acted as a buttress to dorsal translation.
As with any bridge plating technique, the ideal time to remove the plate must be determined. We chose to err on the side of stability and stiffness. To allow adequate time for bony consolidation, we opted to remove the hardware ten weeks from the index procedure. We were encouraged by the immediate active arc of motion. In fact, most of the motion (20-70 degrees) was achieved prior to joint release and tenolysis. Given the appearance of the post-operative x-rays, this joint is likely to degenerate over time. This is a known consequence of the injury itself and occurs after other treatments as well. While the radiographic outcome admittedly is not perfect, the patient currently has a usable and pain free finger. The short-term results suggest that the bridge plate procedure for unstable PIP fracture dislocation is a viable option, particularly for the patient who is unable to tolerate external hardware or properly rehab the hand.
Unfortunately the patient in this case report, despite numerous attempts to get him to return to the office for formal evaluation, refused to follow up after his initial post-operative visit. That said, the authors were able to discuss his outcome over the phone with him, and he states he is ‘happy with his finger’. He states he has ‘good, though not perfect, motion, excellent strength and good function’. He denies any pain at this time. He works as plumber, and has been able to return to work without difficulty. He was even able to work with the bridge plate in place prior to removal, which was the ultimate goal for him. All in all, the we are pleased with his overall reported results.
Conflict of Interest:
The authors declare that they have no conflict of interest
Statement of Human and Animal Rights:
This article does not contain any studies with human or animal subjects.
Informed consent:
Informed consent was obtained from all individual participants included in the study.
Statement of Funding:
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1.Hastings 2nd H, Carroll CT. Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clinics. 1988;4(3):503. [PubMed] [Google Scholar]
- 2.Gonzalez RM, Hammert WC. Dorsal fracture-dislocations of the proximal interphalangeal joint. Journal of Hand Surgery. 2015;40(12):2453–5. doi: 10.1016/j.jhsa.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 3.Waris E, Mattila S, Sillat T, Karjalainen T. Extension block pinning for unstable proximal interphalangeal joint dorsal fracture dislocations. The Journal of Hand Surgery. 2016;41(2):196–202. doi: 10.1016/j.jhsa.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Haseth KB, Neuhaus V, Mudgal CS. Dorsal fracture-dislocations of the proximal interphalangeal joint: evaluation of closed reduction and percutaneous Kirschner wire pinning. Hand. 2015;10(1):88–93. doi: 10.1007/s11552-014-9660-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Deitch MA, Kiefhaber TR, Comisar BR, Stern PJ. Dorsal fracture dislocations of the proximal interphalangeal joint: surgical complications and long-term results. The Journal of hand surgery. 1999;24(5):914–23. doi: 10.1053/jhsu.1999.0914. [DOI] [PubMed] [Google Scholar]
- 6.Ruland RT, Hogan CJ, Cannon DL, Slade JF. Use of dynamic distraction external fixation for unstable fracture-dislocations of the proximal interphalangeal joint. The Journal of hand surgery. 2008;33(1):19–25. doi: 10.1016/j.jhsa.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 7.Lauder A, Agnew S, Bakri K, Allan CH, Hanel DP, Huang JI. Functional outcomes following bridge plate fixation for distal radius fractures. The Journal of hand surgery. 2015;40(8):1554–62. doi: 10.1016/j.jhsa.2015.05.008. [DOI] [PubMed] [Google Scholar]
- 8.Unglaub F, Langer MF, Hahn P, Müller LP, Ahrens C, Spies CK. Fractures of the proximal interphalangeal joint: Diagnostic and operative therapy options. Der Unfallchirurg. 2016;119(2):133–43. doi: 10.1007/s00113-016-0142-z. [DOI] [PubMed] [Google Scholar]
- 9.Hamer DW, Quinton DN. Dorsal fracture subluxation of the proximal interphalangeal joints treated by extension block splintage. Journal of Hand Surgery. 1992;17(5):586–90. doi: 10.1016/s0266-7681(05)80249-9. [DOI] [PubMed] [Google Scholar]
- 10.Inanami H, Ninomiya S, Okutsu I, Tarui T, Fujiwara N. Dynamic external finger fixator for fracture dislocation of the proximal interphalangeal joint. The Journal of hand surgery. 1993;18(1):160–4. doi: 10.1016/0363-5023(93)90265-5. [DOI] [PubMed] [Google Scholar]
- 11.Krakauer JD, Stern PJ. Hinged device for fractures involving the proximal interphalangeal joint. Clinical Orthopaedics and Related Research (1976-2007). 1996;327:29–37. doi: 10.1097/00003086-199606000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Nilsson JA, Rosberg HE. Treatment of proximal interphalangeal joint fractures by the pins and rubbers traction system: a follow-up. Journal of plastic surgery and hand surgery. 201448(4):259–64. doi: 10.3109/2000656X.2013.870909. [DOI] [PubMed] [Google Scholar]
- 13.Kubitskiy A, Soliman BA, Dowd MB, Curtin P. External fixation of the hand: a simple approach to comminuted proximal interphalangeal joint fractures. Hand Surgery. 2014;19(01):85–9. doi: 10.1142/S0218810414500142. [DOI] [PubMed] [Google Scholar]
- 14.Frueh FS, Calcagni M, Lindenblatt N. The hemi-hamate autograft arthroplasty in proximal interphalangeal joint reconstruction: a systematic review. Journal of Hand Surgery (European Volume) 2015;40(1):24–32. doi: 10.1177/1753193414554356. [DOI] [PubMed] [Google Scholar]