Abstract
The COVID-19 pandemic has affected millions of individuals worldwide. In the United States, the rapid transmission of cases has created challenges for healthcare systems across the country. We report a case of a patient who fully recovered from COVID-19 with intermittent negative RT-PCR testing and a symptom free interval who went on to develop a second infection. The patient's second infection resulted in a more severe clinical course. The patient developed Acute Respiratory Distress Syndrome resulting in intubation twice and an extensive stay in the intensive care unit. Six weeks post-discharge, the patient was evaluated for continued dyspnea, hypoxia, and continued oxygen dependence. The patient subsequently underwent right heart catherization for further evaluation and was found to have newly developed pulmonary hypertension. Given the possibility of second wave infections this fall and winter, this case highlights the concern that re-infections with COVID-19 could cause substantially worse clinical outcomes and long-term complications. In terms of ongoing vaccine development, the short lived immune response in this case calls into question the ability of a future vaccine to provide long term lasting immunity against COVID-19.
Keywords: COVID-19, SARS-CoV-2, ARDS, Coronavirus, Pulmonary hypertension, Reinfection
1. Introduction
As of October 2020, the Coronavirus Disease 2019 (COVID-19) pandemic has affected over 40.2 million individuals worldwide and caused over 1.1 million deaths [1]. The spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes COVID-19, occurs through respiratory droplets and particles resulting in easy transmissibility between human hosts [2]. Individuals affected by COVID-19 have a wide-ranging clinical presentation from mild flu-like symptoms to more severe respiratory distress [1,2]. Very few cases of re-infection with COVID-19 have been documented in the medical literature [3,4]. At this time, there are no documented cases of severe re-infection leading to Acute Respiratory Distress Syndrome (ARDS) with a negative reverse transcriptase polymerase chain reaction (RT-PCR) test during the symptom free interval. We report a case of a patient who fully recovered from COVID-19 with intermittent negative RT-PCR testing who went on to develop a second infection leading to severe ARDS requiring intubation and an extensive stay in the intensive care unit. Post-discharge, the patient developed new pulmonary hypertension and remains chronically oxygen dependent. Given the possibility of a “second wave” this fall and winter, this case highlights the concern that second infections could cause substantially worse clinical outcomes and long-term complications.
2. Case presentation
A 62 year old female with past medical history of previously diagnosed and treated COVID-19 infection, hypertension, hypothyroidism, chronic lower back pain, degenerative disk disease, previous L2-L4 lumbar fusion, and anxiety presented to the emergency department in August 2020 for one week history of progressively worsening shortness of breath and cough. She reported recent contact with a known COVID positive individual. Her grandson had tested positive 10–14 days prior to the onset of her new symptoms.
The patient was previously diagnosed with COVID-19 in April 2020. At that time, she was hospitalized and underwent a typical treatment approach based on early understanding of COVID-19 with broad spectrum antibiotics, hydroxychloroquine, vitamin C, and zinc [5]. She recovered and was discharged home with complete resolution of symptoms and no lingering dyspnea or hypoxia. Prior to her COVID-19 diagnosis, the patient had been following with neurosurgery for chronic lower back pain. Planned surgical intervention was delayed due to her SARS-CoV-2 infection. In July, the patient underwent pre-operative clearance for neurosurgical intervention. She was tested for COVID-19 with a resulting negative RT-PCR test on July 16, 2020. She was asymptomatic at that time and had no fever, dyspnea, or hypoxia.
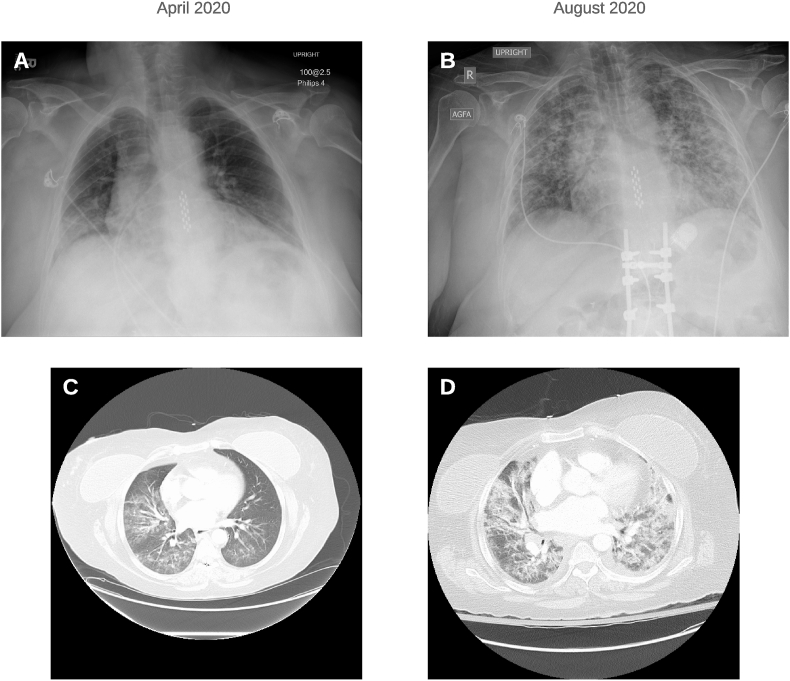
In the emergency department, the patient was tachycardic, tachypneic, and profoundly hypoxic with oxygen saturation as low as 77%. Initial admission arterial blood gas showed worsening hypoxia. She was placed on high flow oxygen at 30 L, 60% FiO2, and admitted to the medical floor. Initial work-up was significant for CTA pulmonary with diffuse bilateral pulmonary opacities suggestive of multifocal pneumonia and ARDS. Comparison of imaging to prior CTA done in April revealed extensive progression of infiltrates (see Fig. 1). Inflammatory markers were significant for sedimentation rate 72, C-reactive protein 10.8, fibrinogen 601, d-dimer 2.035, ferritin 804, and lactate dehydrogenase 508 (see Table 1). She was started on dexamethasone, remdesevir, ceftriaxone, azithromycin, vitamin C, and zinc [6].
Fig. 1.
Imaging studies.
Chest radiographs (Panels A and B) taken at time of first presentation to the emergency room show interval development of worsening bilateral pulmonary opacities between April (Panel A) and August (Panel B).
Axial, contrast enhanced CT angiography images (Panels C and D) taken at time of first presentation to the emergency room show bilateral pulmonary opacities. Panel D (August) represents development of multifocal pneumonia suggestive of Acute Respiratory Distress Syndrome.
Table 1.
Laboratory data.
| Variable | Reference Range, Adults, This Hospital | Initial Presentation, April 2020 | Second Presentation, August 2020 |
|---|---|---|---|
| Arterial Blood Gas* | |||
| pH | 7.35–7.45 | 7.342 | 7.426 |
| PaO2 (mmHg) | 80–95 | 85 | 67 |
| PaCO2 (mmHg) | 35–45 | 42.1 | 33.6 |
| Inflammatory Markers | |||
| Ferritin (ng/mL) | 3.0–105.0 | 138.3 | 804.1 |
| Fibrinogen (mg/dL) | 196–493 | 456 | 601 |
| Sedimentation rate (mm) | 0–30 | 30 | 72 |
| C-reactive protein (mg/dL) | 0.0–0.60 | 15.8 | 10.8 |
| D-dimer, quantitative (ug/mL FEU) | ≤0.400 | 1.359 | 2.035 |
| Procalcitonin (<0.1UG/L) | <0.1 | 8.198 | 0.314 |
Overnight on day two of admission, she became progressively more hypotensive with increased work of breathing, lethargy, and confusion. Oxygen requirements continued to increase from the previous day to high flow at 40 L, 70% FiO2. At 7am, a rapid response was called. A repeat chest x-ray showed worsening of severe interstitial opacities. The patient was started on BiPAP and pressor support and was transferred to the intensive care unit. Upon admission to the ICU, the decision was made to intubate the patient due to increased work of breathing, progressive hypoxia, and respiratory muscle fatigue. Later that day, her admission COVID test resulted as positive.
Three days later, the patient made some interval improvement and was extubated. Unfortunately, she decompensated again and required re-intubation. At time of second intubation, due to the severity of her condition, she was started on convalescent plasma, broad spectrum antibiotic therapy, and a continuous steroid drip. Five days later, she was able to tolerate extubation and was transferred to the medical floor on 6 L of nasal cannula oxygen. Prior to discharge, she tested negative for COVID-19 and went home on 3 L of oxygen.
At her six week follow up appointment, the patient reported continued dyspnea and new lower extremity edema. A trans-thoracic echocardiogram done at this time found newly elevated right ventricular systolic pressures. In order to confirm the diagnosis of pulmonary hypertension, she underwent a right heart catherization. Catherization studies demonstrated elevations in pulmonary artery pressure, pulmonary capillary wedge pressure, and pulmonary vascular resistance consistent with the diagnosis of pulmonary hypertension. At this time, she remains on home oxygen with substantial dyspnea and fatigue (Fig. 2).
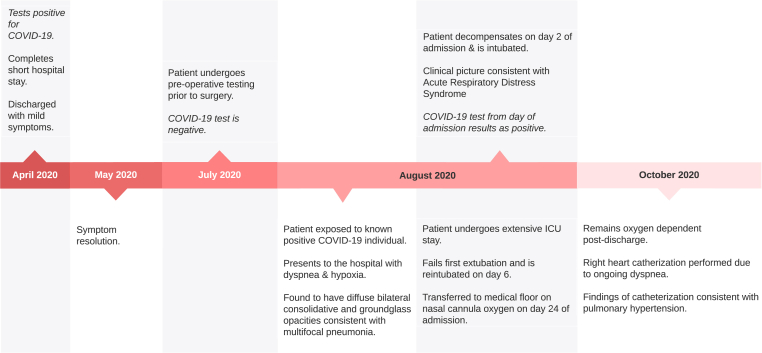
Fig. 2.
Timeline.
3. Discussion
Due to its recent emergence, the scientific community is continuing to gather new information on COVID-19. In this case, our patient had two seemingly unrelated COVID-19 infections with intermittent recovery and negative testing. The second infection resulted in a substantially more severe hospital course with lasting cardiopulmonary effects. While it is possible that the patient never cleared the first infection completely, it is unlikely given her full recovery and negative testing. This case poses two interesting questions. What is the likelihood of recurrence of COVID-19 and to what extent will a patient be affected by a recurrent infection? This will need to be further evaluated over time as we continue to learn more about SARS-CoV-2. The second question revolves around immunity and vaccine development. Recent studies have shown significant loss of IgG antibodies to SARS-CoV-2 within two to three months of onset of initial symptoms [7]. In this patient, the antibody response was clearly short lived providing little long term protection against a second infection. We must question how much success a vaccine will have and for what length of time it will confer immunity when administered.
Ethics approval and consent to participate-not applicable
Consent for publication-provided by patient and form available for review.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Authors' contributions
SS was the primary author of this manuscript. FF provided edits of the first manuscript and content review. All authors read and approved the final manuscript.
Declaration of competing interest
The authors have no competing interests to report.
Acknowledgements
Dr. Louise Jones for editorial assistance.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.rmcr.2020.101314.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.World Health Organization Coronavirus disease—COVID-19 global data. WHO. https://covid19.who.int/
- 2.Shereen M.A., Khan S., Kazmi A., Bashir N., Siddique R. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Torres Acosta M.A., Singer B.D. Pathogenesis of COVID-19-induced ARDS: implications for an ageing population. European Journal of Respiratory Medicine. 2020;56(3) doi: 10.1183/13993003.02049-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lafaie L., Celarier T., Goethals L. Recurrence or relapse of COVID-19 in older patients: a description of three cases. Journal of the American Geriatrics Society. 2020;68:2179–2183. doi: 10.1111/jgs.16728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gautret P., Lagier J.C., Parola P. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. International Journal of Antimicrobial Agents. 2020;56:105949. doi: 10.1016/j.ijantimicag.2020.105949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oroojalian F., Haghbin A., Baradaran B. Novel insights into the treatment of SARS-CoV-2 infection: an overview of current clinical trials. International Journal of Biological Macromolecules. 2020;165:18–43. doi: 10.1016/j.ijbiomac.2020.09.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu T., Wu S., Tao H. Prevalence of IgG antibodies to SARS-CoV-2 in Wuhan—implications for the ability to produce long-lasting protective antibodies. MedRxIV. 2020 https://www.medrxiv.org/content/10.1101/2020.06.13.20130252v1 (pre-print) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.