Abstract
Organ abscesses caused by Streptococcus anginosus are relatively rare. We report the case of an elderly woman with splenic abscess caused by S. anginosus bacteremia after urinary tract infection. An 82-year-old woman had a history of frequency of urination, urgency, and fever with chills for over 10 days prior to admission. An abdominal computed tomography (CT) scan performed in the emergency room revealed a low-density lesion in the spleen, kidney cysts, some exudation around the kidney, and cystitis should be valued. She was treated with ceftriaxone and imipenem/cilastatin. After admission, the blood culture yielded positive results for S. anginosus. A contrast-enhanced abdominal CT scan showed that the low-density lesion previously found in the spleen was smaller than before. After percutaneous drainage of the splenic abscess and treatment with piperacillin/tazobactam based on the antibiotic sensitivity pattern, repeated abdominal CT scan revealed a significant reduction in the low-density lesion. The patient was discharged without recurrence or complications. A systematic review of organ abscess caused by S. anginosus bacteremia was performed. To our knowledge, there has been no report of splenic abscess caused by S. anginosus bacteremia secondary to urinary system tract infection, although urinary tract infections are also an important source.
Keywords: Streptococcus anginosus, bacteremia, splenic abscess, urinary infection, treatment
1. Introduction
Urinary tract infection is the most common parenteral infection among females worldwide. One-third of women experience symptomatic urinary tract infections by the age of 24 years, and more than 50% of women will experience it during their lifetime [1]. The reduction in estrogen secretion that occurs in menopausal and postmenopausal women contributes to the transition of the dominant vaginal flora from Lactobacillus to Escherichia coli or other Enterobacterales, and increases the risk of urinary tract infection [1]. We present the case of an 82-year-old female patient who presented with a urinary tract infection, and in whom S. anginosus, part of the normal flora of the urinary tract, invaded the circulation, leading to splenic abscess formation. We review the literature on organ abscess caused by S. anginosus bacteremia and emphasize that different sources of infection should be considered.
2. Case presentation
An 82-year-old woman was admitted to our hospital with a chief complaint of recurrent fever for more than 10 days. Ten days prior, the patient experienced frequency of micturition, urgency, and fever with chills with no obvious predisposition; the highest body temperature was as high as 39.5°C. She had no odynuria. She self-treated with antipyretics. Three days prior, the patient experienced fever again, with a body temperature of 40°C, accompanied by chills, unconsciousness, fatigue, and nausea, but no vomiting. She was admitted to the emergency room of our hospital and treated with intravenous ceftriaxone. Antibiotic therapy was escalated to imipenem/cilastatin due to recurrent fever that did not respond to ceftriaxone at a dose of 2.0 g once a day for two days, and the body temperature reduced slightly. The patient had lower abdominal pain, but no diarrhea, dizziness, or headache. The patient had been retired from her job for many years and had no history of smoking or drinking in the past. She had no significant medical or family history.
Physical examination after admission indicated a body temperature of 36°C, pulse rate of 63 bpm, respiratory rate of 18 breaths per minute, and blood pressure of 120/51 mmHg. The breath sounds were coarse, and no rhonchi or moist rales could be heard. Cardiac examination revealed no murmurs. Upon abdominal examination, there was mild tenderness in the lower abdomen with no rebound tenderness or guarding. No other obvious abnormalities were observed.
Laboratory examination performed in the emergency room indicated the following: a white blood cell (WBC) count of 16.3 × 109/L; neutrophils, 90.4%; and C-reactive protein level, 78.3 mg/L. A computed tomography (CT) scan of the lungs indicated subpleural patches in the lower dorsal lobe, considering for a sagging effect. A CT scan of the abdomen revealed splenomegaly, a low-density lesion in the spleen (Figure 1(a)), kidney cysts, a little exudation around the kidney (Figure 2), thickening of the bladder wall, a little gas in the bladder, and cystitis could not be ruled out (Figure 3). After admission, the procalcitonin level was 1.67 ng/mL; urine routine examination showed 1.7 WBCs/high-power field, red blood cell count 5.7/high-power field, and a bacterial count of 667/µL; and the albumin level was 32 g/L. Ultrasonography of the hepatobiliary tree and spleen revealed a cystic mass in the spleen. Echocardiography revealed aortic valve degeneration, aortic sclerosis, and normal left ventricular systolic function at rest.
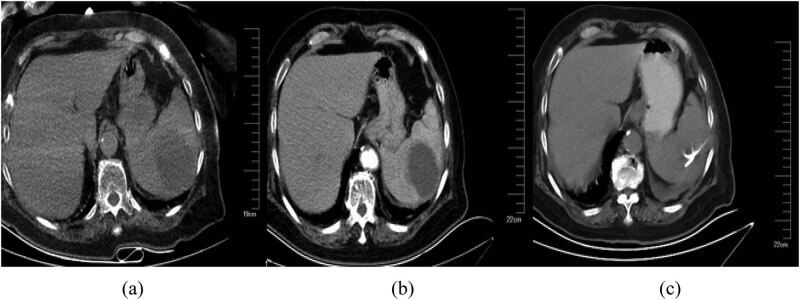
Figure 1.
A CT scan of the abdomen revealed a low-density lesion in the spleen (a) before admission, (b) on day 5 after admission, (c) after paracentesis and drainage of the splenic abscess.
Figure 2.
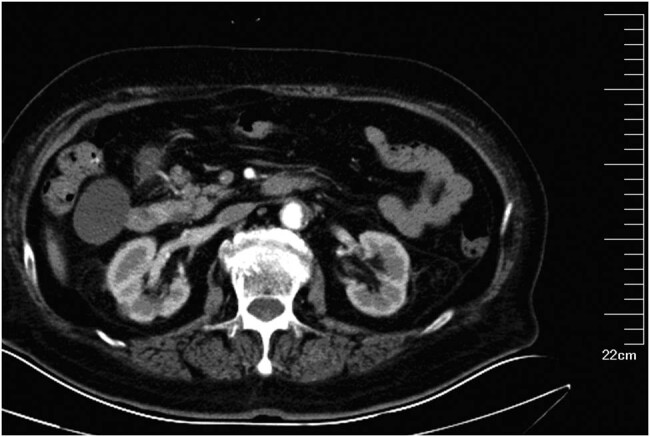
An abdominal CT scan showed kidney cysts and a little exudation around the kidneys.
Figure 3.
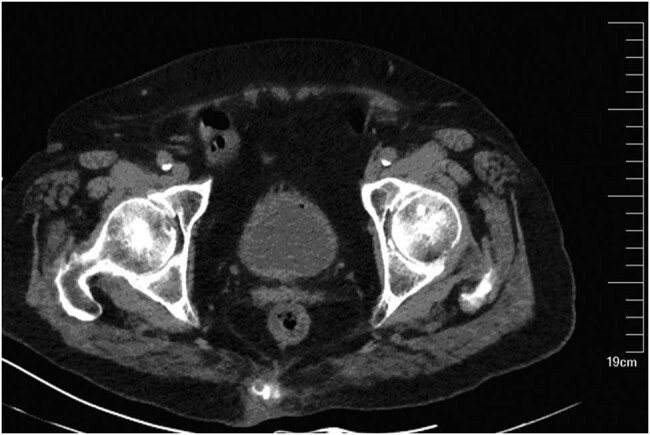
An abdominal CT scan showed thickening bladder wall and a little gas in the bladder.
After admission, the patient received imipenem intravenously at a dose of 0.5 g every 6 h, and the body temperature dropped significantly. The blood culture yielded positive results for S. anginosus. On day 5 after admission, a contrast-enhanced abdominal CT scan showed splenomegaly, and a smaller low-density lesion in the spleen than before, with multiple peripheral honeycomb-like weakly enhanced low-density lesions, indicative of splenic abscess (Figure 1(b)). The kidney cysts and exudation around the kidney were nearly the same as before. Percutaneous drainage was performed, and S. anginosus was isolated from the pus sample. Next, a drug susceptibility test was performed with bacterial suspensions by using the PMCI/ID-2 card matched by Phoenix 100 (BD Company, America) or disk diffusion method. The interpretation of antimicrobial susceptibility was performed by applying clinical breakpoints defined by the Clinical Laboratory Standards Institute M100-S29. The result showed that S. anginosus in the blood and pus was sensitive to penicillin G. And the antibiotics were changed to intravenous 80 piperacillin/tazobactam at a dose of 4.5 g every 8 h (Table 1).
Table 1.
The susceptibility results of S. anginosus
| Antibiotic name | Method | Sensitivity | Result | Determination standard | ||
|---|---|---|---|---|---|---|
| Sensitive | Intermediary | Resistance | ||||
| Cefotaxime | MIC | S | ≤0.5 | ≤1 | 2 | ≥4 |
| Chloramphenicol | MIC | S | 4 | ≤4 | 8 | ≥16 |
| Cefepime | MIC | S | ≤0.5 | ≤1 | 2 | ≥4 |
| Clindamycin | MIC | R | >1 | ≤0.25 | 0.5 | ≥1 |
| Erythromycin | MIC | R | >4 | ≤0.25 | 0.5 | ≥1 |
| Linezolid | MIC | S | ≤1 | ≤2 | — | — |
| Vancomycin | MIC | S | 1 | ≤1 | — | — |
| Penicillin G | MIC | S | 0.125 | ≤0.12 | 0.25–2 | ≥4 |
On day 16 after admission, re-examination via the abdominal CT scan revealed changes after paracentesis and drainage of the splenic abscess, and the low-density lesion had significantly reduced in size. A little gas could be seen in and around the spleen (Figure 1(c)). The levels of C-reactive protein and procalcitonin were 39.1 mg/L and 0.116 ng/mL, respectively. On day 22 after admission, the patient was discharged without recurrence or complications.
Ethical approval: The research related to human use has been complied with all the relevant national regulations, institutional policies, and in accordance with the tenets of the Declaration of Helsinki, and has been approved by the authors’ institutional review board or equivalent committee.
Informed consent: Informed consent has been obtained from all individuals included in this study.
3. Discussion
Urinary tract infections are the most common parenteral infections in women worldwide, especially among the elderly. Among outpatient female patients with symptoms of urinary tract infection such as dysuria and frequency of micturition without vaginal discharge, the incidence of cystitis is 96% [2]. Studies have shown that E. coli is the most common pathogen of urinary tract infection in the elderly. García-Agudo et al. also found that E. coli is the most common pathogen in community-acquired urinary tract infection, followed by Klebsiella pneumoniae, Enterococcus faecalis, Pseudomonas aeruginosa, and Proteus mirabilis [3], and the blood culture result was positive in 15–25% of urinary tract infection patients [4]. Krystal et al. confirmed that S. anginosus was one of the pathogens of genitourinary infection [5]. However, no study has reported that S. anginosus invading the blood after a urinary infection and resulting in a splenic abscess. In our case, the patient had symptoms of urinary tract infection such as frequency of micturition and urgency, and an abdominal CT scan indicated cystitis. The levels of bacteria and red blood cells were high in the urine. The normal WBC level in the urine may have been explained by the antibiotic treatment received before admission. It was a great pity that we neglected to perform a urine culture test because the symptoms of frequent urination and urgency disappeared after admission. Our patient was an elderly woman with a low albumin level, poor nutritional status, and decreased immunity. The colonization of the genitourinary system by S. anginosus could cause urinary tract infection, and lead to splenic abscess after entering the circulation. Thus, when urinary tract infection is suspected, we should be alert to the possibility of S. anginosus infection. Active treatment of the primary disease, early intervention, and effective prevention of bacteremia can control or prevent the occurrence or progression of the abscess.
The S. anginosus group comprises S. anginosus, Streptococcus intermedius, and Streptococcus constellatus [6], which are normal flora of the oral cavity, upper respiratory tract, gastrointestinal tract, and urogenital tract [7,8]. Epidemiological data show that S. anginosus can cause mild skin infection and even suppurative life-threatening infection [9]. The distribution and incidence of pyogenic infection are different among S. anginosus, S. intermedius, and S. constellatus. Studies have confirmed that S. anginosus is more likely to be isolated from the gastrointestinal tract and urogenital system, while S. intermedius is more possible to cause the infection of the central nervous system. S. constellatus can be isolated more widely, relatively more common in the respiratory tract, but less common in the central nervous system [10]. Moreover, S. intermedius has the tendency to form abscesses and infection in deep tissue and is more likely to cause suppurative non-bacterial infection, which requires surgical intervention. In contrast, S. constellatus and S. anginosus have a lower incidence of pyogenic infection [11].
Some studies have shown that S. anginosus can be associated with head, neck, and esophageal cancer [12]. Other studies have concluded that the most common source of S. anginosus bacteremia is the hepatobiliary system [13]. In a study of 127 cases of cancer, Sasaki et al. concluded that S. anginosus bacteremia was more common in esophageal and gastric cancer among patients with solid tumors complicated by S. anginosus group bacteremia [14]. This may be accounted for by the increasing amount of S. anginosus in the stomach when gastric tumors occur [15].
Organ abscesses caused by S. anginosus bacteremia are relatively rare, with only nine cases in the literature (Table 2). Almost all cases presented fever and abdominal pain and three cases showed nausea and vomiting. Most cases presented abdominal tenderness. Six cases had a gastrointestinal focus among which three had tumors of the digestive tract. Two cases had an oropharyngeal focus, and the patients had poor oral hygiene or suffered from dental caries and oral mucosal ulcers. Only one case had a biliary focus. The main mechanism underlying those with a digestive tract focus is that gastrointestinal tumors or invasive surgeries destroy the mucosa, offering an opportunity for the normal flora S. anginosus to invade the blood and cause abscesses in other parts of the body. The male/female ratio of these nine cases was 6:3; the mean age was 51 (range 32–63) years. Two patients experienced improvement after conservative intravenous medication without invasive procedures, and the other patients were treated with additional abscess drainage or surgery. Most patients had a good prognosis after intravenous medication and operation if necessary, and only two patients died (mortality rate, 22.2%), both of whom had abscesses involving the mediastinum, and one of them had tumor metastasis. Therefore, when mediastinal abscesses occur, treatment is relatively difficult, and early active intervention should be taken to reduce the mortality. In addition, S. anginosus bacteremia can also contribute to other infections without abscess formation, such as infective endocarditis [16], osteomyelitis [17], gas gangrene [18], endogenous endophthalmitis [19], and acute glomerulonephritis [20].
Table 2.
Published cases of S. anginosus bacteremia leading to abscess formation
| Ref. | Gender | Age (years) | Underlying diseases | Invasive pathway | Organ with abscess | Number of abscesses | Treatment of abscess | Outcome |
|---|---|---|---|---|---|---|---|---|
| Prashanth Rawla et al. [23] | Male | 62 | Hypertension, dyslipidemia, hypothyroidism,colon cancer | Cancer destroyed the integrity of the blood-mucosal barrier and led to the S. anginosus bacteremia | Liver | Single | Empirical antibiotics (vancomycin, metronidazole, piperacillin-tazobactam). Positive blood culture (ceftriaxone) | Improved |
| Umair Masood et al. [24] | Male | 62 | Hypertension, diabetes mellitus, colorectal cancer | Cancer destroyed the colonic mucosa, and the pathogens invaded the circulation | Liver | Multiple | Empirical antibiotics (vancomycin, piperacillin-tazobactam). Positive blood culture (ceftriaxone) | Improved |
| Marina Gorelik et al. [25] | Female | 63 | Hypertension, diabetes mellitus, ileal stromal tumors | Cancer destroyed the colonic mucosa, and the pathogens invaded the circulation | Liver | Multiple | Ceftriaxone, metronidazole, percutaneous drainage | Improved |
| Miguel E. Cervera-Hernandez et al. [26] | Female | 45 | Hypertension, asthma, morbid obesity status | Laparoscopic sleeve gastrectomy destroyed the colonic mucosa, and the pathogens invaded the circulation | Spleen | Single | Empirical antibiotics (piperacillin-tazobactam). Positive blood culture (meropenem, linezolid, ceftriaxone, metronidazole), percutaneous drainage | Improved |
| Daniel C Baumgart [27] | Male | 41 | Ulcerative colitis, fulminant pancolitis | Inflammatory bowel disease caused bacterial translocation of the gut, resulting in bacteremia | Endocardium | Empirical antibiotics (gentamicin, vancomycin), surgery | Improved | |
| J Campos et al. [28] | Male | 53 | Hepatocarcinoma | Oropharyngeal infection | Peritonsillar abscess with adrenal and bone extending to the right posterior neck space and to the mediastinum | Piperacillin-tazobactam, imipenem, linezolid, fluconazole | Died | |
| Huseyin Agah Terzi et al. [29] | Male | 32 | Poor oral hygiene, dental caries, impairment of mucosal integrity | Poor oral hygiene caused abscess and bacteremia | Abdominal cavity | Multiple | Ceftriaxone, metronidazole | Improved |
| Jia Dong et al. [30] | Female | 41 | Pneumonia | Mediastinum | Ciprofloxacin, clindamycin, moxifloxacin, etimicin, oseltamivir phosphate, linezolid | Died | ||
| Norikazu Arakura et al. [31] | Male | 63 | Acute obstructive suppurative cholangitis | Round ligament of the liver | Meropenem trihydrate, levofloxacin, surgical operation | Improved |
Splenic abscesses can be formed by hematogenous or local dissemination, which often occurs in people with immunocompromised status. The management of patients with splenic abscesses includes antibiotic therapy, percutaneous drainage, or splenectomy [21]. Percutaneous drainage is recommended when the risk of sepsis is high after splenectomy, but multilocular abscesses, intractable abscesses, and ruptured abscesses with bleeding are contraindications for percutaneous drainage [22]. In our case, the splenic abscess was a single focus, and improved after percutaneous drainage and medication without splenectomy.
In conclusion, splenic abscesses caused by S. anginosus bacteremia are rare, and no study has reported the urinary tract as the original focus till now. Our case expands the knowledge about the potential source of infection in such patients. Treatment of the primary disease should be instituted as early as possible. Active intervention, prevention of S. anginosus invasion of the blood, control, or avoidance of the occurrence or progression of the abscess can effectively improve the prognosis and increase the survival rate.
Acknowledgments
We are grateful for the advice on microbiological methods from Dr Zhijie Zhang at the Department of Clinical Laboratory, Shengjing Hospital.
Footnotes
Conflicts of interest: There are no conflicts of interest.
Funding: Supported by Shengjing Hospital 345 Talent Project.
Author contributions: HW collected and analyzed the medical data of the patient, and wrote and revised the manuscript. RZ made a critical revision of the manuscript. Both authors read and approved the final manuscript.
References
- [1].Dielubanza EJ, Schaeffer AJ. Urinary tract infections in women. Med Clin North Am. 2011;95(1):27–41. [DOI] [PubMed]; Dielubanza EJ, Schaeffer AJ. Urinary tract infections in women. Med Clin North Am. 2011;95(1):27–41. doi: 10.1016/j.mcna.2010.08.023. [DOI] [PubMed] [Google Scholar]
- [2].Kumar S, Dave A, Wolf B, Lerma EV. Urinary tract infections. Dis Mon. 2015; 61(2):45–59. [DOI] [PubMed]; Kumar S, Dave A, Wolf B, Lerma EV. Urinary tract infections. Dis Mon. 2015;61(2):45–59. doi: 10.1016/j.disamonth.2014.12.002. [DOI] [PubMed] [Google Scholar]
- [3].García-Agudo L,Rodríguez-Iglesias M,Carranza-González R, Galán F, Asencio MA, Huertas Vaquero M, et al. Urinary tract infection in the oldest old: a work overload for the microbiology laboratory. Rev Esp Quimioter. 2017;30(5):379–81. [PubMed]; García-Agudo L, Rodríguez-Iglesias M, Carranza-González R, Galán F, Asencio MA, Huertas Vaquero M. et al. Urinary tract infection in the oldest old: a work overload for the microbiology laboratory. Rev Esp Quimioter. 2017;30(5):379–81. [PubMed] [Google Scholar]
- [4].Horcajada JP, Shaw E, Padilla B, Pintado V, Calbo E, Benito N, et al. Healthcare-associated, community-acquired and hospital-acquired bacteraemic urinary tract infections in hospitalized patients: a prospective multicentre cohort study in the era of antimicrobial resistance. Clin Microbiol Infect. 2013;19(10):962–8. [DOI] [PubMed]; Horcajada JP, Shaw E, Padilla B, Pintado V, Calbo E, Benito N. et al. Healthcare-associated, community-acquired and hospital-acquired bacteraemic urinary tract infections in hospitalized patients: a prospective multicentre cohort study in the era of antimicrobial resistance. Clin Microbiol Infect. 2013;19(10):962–8. doi: 10.1111/1469-0691.12089. [DOI] [PubMed] [Google Scholar]
- [5].Thomas-White K, Forster SC, Kumar N, Van Kuiken M, Putonti C, Stares MD, et al. Culturing of female bladder bacteria reveals an interconnected urogenital microbiota. Nat Commun. 2018;9(1):1557–63. [DOI] [PMC free article] [PubMed]; Thomas-White K, Forster SC, Kumar N, Van Kuiken M, Putonti C, Stares MD. et al. Culturing of female bladder bacteria reveals an interconnected urogenital microbiota. Nat Commun. 2018;9(1):1557–63. doi: 10.1038/s41467-018-03968-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Walkty A, Embil JM, Nichol K, Karlowsky J. An unusual case of Streptococcus anginosus group pyomyositis diagnosed using direct 16S ribosomal DNA sequencing. Can J Infect Dis Med Microbiol. 2014;25(1):32–4. [DOI] [PMC free article] [PubMed]; Walkty A, Embil JM, Nichol K, Karlowsky J. An unusual case of Streptococcus anginosus group pyomyositis diagnosed using direct 16S ribosomal DNA sequencing. Can J Infect Dis Med Microbiol. 2014;25(1):32–4. doi: 10.1155/2014/170517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sasaki M, Kodama Y, Shimoyama Y, Ishikawa T, Kimura S. Aciduricity and acid tolerance mechanisms of Streptococcus anginosus. J Gen Appl Microbiol. 2018;64:174–9. [DOI] [PubMed]; Sasaki M, Kodama Y, Shimoyama Y, Ishikawa T, Kimura S. Aciduricity and acid tolerance mechanisms of Streptococcus anginosus . J Gen Appl Microbiol. 2018;64:174–9. doi: 10.2323/jgam.2017.11.005. [DOI] [PubMed] [Google Scholar]
- [8].Janssen EHCC, Bree LCJD, Kant KM, van Wijngaarden P. Spontaneous fracture of the femur due to osteomyelitis caused by the Streptococcus anginosus group. Neth J Med. 2017;75(3):121–4. [PubMed]; Janssen EHCC, Bree LCJD, Kant KM, van Wijngaarden P. Spontaneous fracture of the femur due to osteomyelitis caused by the Streptococcus anginosus group. Neth J Med. 2017;75(3):121–4. [PubMed] [Google Scholar]
- [9].Obszańska K, Kern-Zdanowicz I, Kozińska A, Machura K, Stefaniuk E, Hryniewicz W, et al. Streptococcus anginosus (milleri) group strains isolated in Poland (1996-2012) and their antibiotic resistance patterns. Pol J Microbiol. 2016;65(1):33–41. [DOI] [PubMed]; Obszańska K, Kern-Zdanowicz I, Kozińska A, Machura K, Stefaniuk E, Hryniewicz W. et al. Streptococcus anginosus (milleri) group strains isolated in Poland (1996-2012) and their antibiotic resistance patterns. Pol J Microbiol. 2016;65(1):33–41. doi: 10.5604/17331331.1197323. [DOI] [PubMed] [Google Scholar]
- [10].Whiley RA, Beighton D, Winstanley TG, Fraser HY, Hardie JM. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol. 1992;30(1):243–4. [DOI] [PMC free article] [PubMed]; Whiley RA, Beighton D, Winstanley TG, Fraser HY, Hardie JM. Streptococcus intermedius, Streptococcus constellatus, and Streptococcus anginosus (the Streptococcus milleri group): association with different body sites and clinical infections. J Clin Microbiol. 1992;30(1):243–4. doi: 10.1128/jcm.30.1.243-244.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kobo O, Nikola S, Geffen Y, Paul M. The pyogenic potential of the different Streptococcus anginosus group bacterial species: retrospective cohort study. Int J Epidemiol. 2017;145:3065–9. [DOI] [PMC free article] [PubMed]; Kobo O, Nikola S, Geffen Y, Paul M. The pyogenic potential of the different Streptococcus anginosus group bacterial species: retrospective cohort study. Int J Epidemiol. 2017;145:3065–9. doi: 10.1017/S0950268817001807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Karpinski TM. Role of oral microbiota in cancer development. Microorganisms. 2019;7(1):20. [DOI] [PMC free article] [PubMed]; Karpinski TM. Role of oral microbiota in cancer development. Microorganisms. 2019;7(1):20. doi: 10.3390/microorganisms7010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Suzuki H, Hase R,Otsuka Y,Hosokawa N. Bloodstream infections caused by Streptococcus anginosus group bacteria: a retrospective analysis of 78 cases at a Japanese tertiary hospital. J Infect Chemother. 2016;22:456–60. [DOI] [PubMed]; Suzuki H, Hase R, Otsuka Y, Hosokawa N. Bloodstream infections caused by Streptococcus anginosus group bacteria: a retrospective analysis of 78 cases at a Japanese tertiary hospital. J Infect Chemother. 2016;22:456–60. doi: 10.1016/j.jiac.2016.03.017. [DOI] [PubMed] [Google Scholar]
- [14].Sasaki H, Ishizuka T, Muto M, Nezu M, Nakanishi Y, Inagaki Y, et al. Presence of Streptococcus anginosus DNA in esophageal cancer, dysplasia of esophagus, and gastric cancer. Cancer Res. 1998;58(14):2991–5. [PubMed]; Sasaki H, Ishizuka T, Muto M, Nezu M, Nakanishi Y, Inagaki Y. et al. Presence of Streptococcus anginosus DNA in esophageal cancer, dysplasia of esophagus, and gastric cancer. Cancer Res. 1998;58(14):2991–5. [PubMed] [Google Scholar]
- [15].Liu X, Shao L, Liu X, Ji F, Mei Y, Cheng Y, et al. Alterations of gastric mucosal microbiota across different stomach microhabitats in a cohort of 276 patients with gastric cancer. EBioMedicine. 2019;40:336–48. [DOI] [PMC free article] [PubMed]; Liu X, Shao L, Liu X, Ji F, Mei Y, Cheng Y. et al. Alterations of gastric mucosal microbiota across different stomach microhabitats in a cohort of 276 patients with gastric cancer. EBioMedicine. 2019;40:336–48. doi: 10.1016/j.ebiom.2018.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Chen ZW, Fang LZ, Huang LX, Zhou B, Han YM. Cerebral hemorrhage, splenic and renal embolisms due to infective endocarditis. Int Med. 2009;48(14):1247–50. [DOI] [PubMed]; Chen ZW, Fang LZ, Huang LX, Zhou B, Han YM. Cerebral hemorrhage, splenic and renal embolisms due to infective endocarditis. Int Med. 2009;48(14):1247–50. doi: 10.2169/internalmedicine.48.2054. [DOI] [PubMed] [Google Scholar]
- [17].Krebs NM, Krebs RC, Yaish AM. Femoral osteomyelitis presenting as a pathologic fracture in a 53 year old male: a rare case report. J Orthop Case Rep. 2017;7(6):85–8. [DOI] [PMC free article] [PubMed]; Krebs NM, Krebs RC, Yaish AM. Femoral osteomyelitis presenting as a pathologic fracture in a 53 year old male: a rare case report. J Orthop Case Rep. 2017;7(6):85–8. doi: 10.13107/jocr.2250-0685.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Iii GRT, Crawford GE. Pneumorachis caused by metastatic gas gangrene. Diagn Microbiol Infect Dis. 2009;63(1):108–10. [DOI] [PubMed]; Iii GRT, Crawford GE. Pneumorachis caused by metastatic gas gangrene. Diagn Microbiol Infect Dis. 2009;63(1):108–10. doi: 10.1016/j.diagmicrobio.2008.08.010. [DOI] [PubMed] [Google Scholar]
- [19].Itoh M, Ikewaki J, Kimoto K, Itoh Y, Shinoda K, Nakatsuka K. Two cases of endogenous endophthalmitis caused by gram-positive bacteria with good visual outcome. Case Rep Ophthalmol. 2010;1(2):56–62. [DOI] [PMC free article] [PubMed]; Itoh M, Ikewaki J, Kimoto K, Itoh Y, Shinoda K, Nakatsuka K. Two cases of endogenous endophthalmitis caused by gram-positive bacteria with good visual outcome. Case Rep Ophthalmol. 2010;1(2):56–62. doi: 10.1159/000320601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Maharaj S, Seegobin K, Chrzanowski S, Chang S. Acute glomerulonephritis secondary to Streptococcus anginosus. BMJ Case Rep. 2018;5(9):bcr2017223314. [DOI] [PMC free article] [PubMed]; Maharaj S, Seegobin K, Chrzanowski S, Chang S. Acute glomerulonephritis secondary to Streptococcus anginosus . BMJ Case Rep. 2018;5(9):bcr2017223314. doi: 10.1136/bcr-2017-223314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Davido B, Dinh A, Rouveix E, Crenn P, Hanslik T, Salomon J. Splenic abscesses: from diagnosis to therapy. Rev Med Int. 2017;38:614–8. [DOI] [PubMed]; Davido B, Dinh A, Rouveix E, Crenn P, Hanslik T, Salomon J. Splenic abscesses: from diagnosis to therapy. Rev Med Int. 2017;38:614–8. doi: 10.1016/j.revmed.2016.12.025. [DOI] [PubMed] [Google Scholar]
- [22].Chiang IS, Lin TJ, Chiang IC, Tsai MS. Splenic abscesses: review of 29 cases. Kaohsiung J Med Sci. 2003;19(10):510–5. [DOI] [PMC free article] [PubMed]; Chiang IS, Lin TJ, Chiang IC, Tsai MS. Splenic abscesses: review of 29 cases. Kaohsiung J Med Sci. 2003;19(10):510–5. doi: 10.1016/S1607-551X(09)70499-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Prashanth R, Vellipuram AR, Bandaru SS, Raj JP. Colon carcinoma presenting as\r, Streptococcus anginosus\r, bacteremia and liver abscess. Gastroenterol Res. 2017;10(6):376–9. [DOI] [PMC free article] [PubMed]; Prashanth R, Vellipuram AR, Bandaru SS, Raj JP.. Colon carcinoma presenting as\r, Streptococcus anginosus\r, bacteremia and liver abscess. Gastroenterol Res. 2017;10(6):376–9. doi: 10.14740/gr884w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Masood U, Sharma A, Lowe D, Khan R. Colorectal cancer associated with Streptococcus anginosus bacteremia and liver abscesses. Case Rep Gastroenterol. 2016;10(3):769–74. [DOI] [PMC free article] [PubMed]; Masood U, Sharma A, Lowe D, Khan R. Colorectal cancer associated with Streptococcus anginosus bacteremia and liver abscesses. Case Rep Gastroenterol. 2016;10(3):769–74. doi: 10.1159/000452757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Gorelik M, Sabates B, Elkbuli A, Dunne T. Ileal GIST presenting with bacteremia and liver abscess: a case report and review of literature. Int J Surg Case Rep. 2018;42:261–5. [DOI] [PMC free article] [PubMed]; Gorelik M, Sabates B, Elkbuli A, Dunne T. Ileal GIST presenting with bacteremia and liver abscess: a case report and review of literature. Int J Surg Case Rep. 2018;42:261–5. doi: 10.1016/j.ijscr.2017.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Cerverahernandez ME, Pohl D. Splenic abscess caused by Streptococcus anginosus following laparoscopic sleeve gastrectomy a case report of a rare complication of bariatric surgery. J Surg Case Rep. 2017;4:1–3. [DOI] [PMC free article] [PubMed]; Cerverahernandez ME, Pohl D. Splenic abscess caused by Streptococcus anginosus following laparoscopic sleeve gastrectomy a case report of a rare complication of bariatric surgery. J Surg Case Rep. 2017;4:1–3. doi: 10.1093/jscr/rjx072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Baumgart DC. How many lives does an ulcerative colitis patient have? Lancet. 2010; 376(9744):928. [DOI] [PubMed]; Baumgart DC. How many lives does an ulcerative colitis patient have? Lancet. 2010;376(9744):928. doi: 10.1016/S0140-6736(10)60955-5. [DOI] [PubMed] [Google Scholar]
- [28].Campos J, Otero E, Moldes L, Rodriguez L, Gonzalez-Quintela A. Descending deep neck infection in a liver transplant patient. Transpl Infect Dis. 2010;12(3):265–8. [DOI] [PubMed]; Campos J, Otero E, Moldes L, Rodriguez L, Gonzalez-Quintela A.. Descending deep neck infection in a liver transplant patient. Transpl Infect Dis. 2010;12(3):265–8. doi: 10.1111/j.1399-3062.2009.00485.x. [DOI] [PubMed] [Google Scholar]
- [29].Terzi HA, Demiray T, Koroglu M, Cakmak G, Hakki Ciftci I, Ozbek A, et al. Intra-abdominal abscess and primary peritonitis caused by Streptococcus anginosus. Jundishapur J Microbiol. 2016;9(6):e33863. [DOI] [PMC free article] [PubMed]; Terzi HA, Demiray T, Koroglu M, Cakmak G, Hakki Ciftci I, Ozbek A. et al. Intra-abdominal abscess and primary peritonitis caused by Streptococcus anginosus . Jundishapur J Microbiol. 2016;9(6):e33863. doi: 10.5812/jjm.33863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Jia D, Zhao M. Streptococcus anginosus infection accompanied by mediastinal abscess with sore throat as initial symptom: report of one case. Chinese Gen Pract. 2013;16(8B):2763–4.; Jia D, Zhao M. Streptococcus anginosus infection accompanied by mediastinal abscess with sore throat as initial symptom: report of one case. Chinese Gen Pract. 2013;16(8B):2763–4. [Google Scholar]
- [31].Arakura N, Ozaki Y, Yamazaki S, Ueda K, Maruyama M, Chou Y, et al. Abscess of the round ligament of the liver associated with acute obstructive cholangitis and septic thrombosis. Int Med. 2009;48(21):1885–8. [DOI] [PubMed]; Arakura N, Ozaki Y, Yamazaki S, Ueda K, Maruyama M, Chou Y. et al. Abscess of the round ligament of the liver associated with acute obstructive cholangitis and septic thrombosis. Int Med. 2009;48(21):1885–8. doi: 10.2169/internalmedicine.48.2396. [DOI] [PubMed] [Google Scholar]