Abstract
Background
The Coronavirus disease 2019 (COVID-19) pandemic has imposed significant changes in cancer service delivery resulting in increased anxiety and distress in both patients and clinicians. We aimed to investigate how these changes have been perceived by patients diagnosed with colorectal cancer and identify determinants of increased anxiety.
Patients and Methods
An anonymized 32-item survey in the specialized lower gastrointestinal cancer outpatient clinics at a tertiary cancer center in North West England between May 18 and July 1, 2020. Self-reported anxiety was based on the General Anxiety Disorder-7 screening tool.
Results
Of 143 participants who completed the survey (response rate, 67%), 115 (82%) were male, and the median age group was 61 to 70 years. A total of 112 (78%) participants had telephone consultation (83% met needs), and 57 (40%) had radiologic scan results discussed over the phone (96% met needs). In total, 23 (18%) participants were considered to have anxiety (General Anxiety Disorder-7 score ≥ 5), with 7 (5.5%) scoring for moderate or severe anxiety. Those concerned about getting COVID-19 infection, and worried COVID-19 would have effect on their mental health, and affect their experience of cancer care, were most likely to have anxiety (P < .05, multivariate analysis). The majority did not feel they needed support during this phase of the pandemic. Participants felt that friends and family had been very supportive, but less so the primary care services (P < .05).
Conclusions
The findings of this survey suggest that some of the service changes implemented may have already improved the overall experience of cancer care among patients with colorectal cancer at our institute. Reassuringly, the incidence of participants with moderate to severe anxiety levels during the peak of COVID-19 in the United Kingdom was much lower than anticipated. Importantly, patients were much more concerned about their cancer treatment than COVID-19, emphasizing the need to continue to provide comprehensive cancer care even with a “second wave” of COVID-19.
Keywords: Anxiety, COVID-19, Psychological support, Psycho-oncology, Well-being
Micro-Abstract
We investigated the perception of service changes imposed by COVID-19 and identified determinants of anxiety in patients with colorectal cancer. A 32-item survey, including the General Anxiety Disorder-7 tool, was performed in a tertiary cancer center. Of 143 participants, 23 (18%) have anxiety (General Anxiety Disorder-7 score ≥ 5); 7 (6%) moderate/severe anxiety. An easy and practical pre-screening assessment questionnaire can help identify those in more need of further support.
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic has imposed significant challenges in the management of patients diagnosed with cancer. The National Institute of Health and Care Excellence in the United Kingdom (UK) and major oncology societies such as the European Society for Medical Oncology, among others, have published recommendations on how cancer treatment may be safely altered during the peak of the pandemic, with the primary goal of minimizing the spread of the disease while maintaining the quality of cancer care. In general, these include suggestions on the deferral of treatments when appropriate, change of intravenous to oral formulation whenever possible, and implementation of telemedicine to reduce hospital footfall.1, 2, 3
In the UK, in addition to lockdown restrictions (officially from March 23, 2020), patients with cancer considered in the vulnerable category were also asked to shield. ‘Shielding’ is a national measure to protect all those identified as ‘clinically extremely vulnerable’ from COVID-19 through a set of social restrictions including avoiding face-to-face contact, which was especially stringent during the first wave of the pandemic.4 Significant alterations in colorectal cancer service delivery with disruptions in the screening and diagnostic pathways and the surveillance endoscopies, as well as in the delivery of radiotherapy systemic treatment to patients with diagnosed colorectal cancer have been reported.5, 6, 7 Even with the provision of alternative screening tests to mitigate the risks of these unprecedented changes, the impact on the personal lives and psychological well-being of patients with cancer is largely unknown. Initial reports have suggested that having a diagnosis of cancer is already a significant risk factor for the development of anxiety and/or depression during the COVID-19 pandemic.8 In anticipation of this, different institutes have preemptively implemented strategies to address distress among both patients and clinicians.
Here, we report the experience of patients with colorectal cancer in our institute on the changes in cancer care, the support received, and perceived anxiety levels during the initial phase of the COVID-19 pandemic.
Materials and Methods
Participants
Consecutive patients with diagnosed colorectal cancer attending the specialized lower gastrointestinal cancer clinics at The Christie NHS Foundation Trust (Manchester, UK), either physically or remotely (via telephone or video consultations) between May 18 and July 1, 2020 were invited to participate in a survey. Participation was entirely voluntary and anonymized, and no incentive was offered for completion of survey.
Survey Design
The survey is a 32-item questionnaire, including questions on basic demographics, the current status of their cancer, patients’ perception of their treatment, risk factors for COVID-19 infection, patients’ experience of telephone and/or video consultation, and the impact of COVID-19 in their mental health. The awareness and use of various support and coping mechanisms, as well as the evaluation of different support services, was also interrogated. This survey was designed by a multidisciplinary group of experienced oncologists, psychiatrists, nurse specialists, and with input from patient representatives.
Study Measures
We used the validated self-reported Generalized Anxiety Disorder scale (GAD-7) as a screening tool for symptoms of anxiety.9 GAD-7 comprise of 7 items that refer to the period of the past 2 weeks, with a 4-point Likert scale: “not at all” (0 points), “on individual days” (1 point), “more than half the days” (2 points), or “nearly every day” (3 points). The final GAD-7 score is calculated by summing up these items, ranging from 0 to 21, with higher values indicating more severe anxiety symptoms.
Implementation
Hard copies of the survey or an electronic link sent (emailed or texted to the patients), were used. The survey was categorized as a quality improvement project in our institute to assess the impact of COVID-19 pandemic on changes to delivery of cancer care and the support patients received during this period, and did not require formal ethics approval. This study was conducted following approval by the Christie Quality Improvement and Clinical Audit Department (reference number 2763).
Statistical Analysis
A complete descriptive analysis for all the variables was carried out using IBM SPSS Statistics for Windows, version 19 (IBM Corp, Armonk, NY). An exhaustive evaluation of associations between the different variables was performed using the χ2 test for comparing categorical variables and the Fisher exact test when appropriate. Normal distribution tests were applied to continuous variables. The non-parametric test was used to compare outcome dichotomous variables with the ordinal variables of the questionnaire. A Benjamini and Hochberg false discovery rate correction was applied to all the univariate comparisons to select variables to be included in the multivariable analysis. The multivariable analysis was performed using a logistic regression for binary outcomes (anxiety vs. no anxiety in particular) and odds ratios (OR) with 95% confidence intervals (CIs) were calculated. A Sankey diagram was drawn using ggplot2 and networkD3 packages in R. The rest of the graphic representation (donut, bar, and stacked bar charts) was perform using Microsoft Excel and GraphPad Prism version 8.0.0 for Mac (San Diego, CA).
Results
Survey Participants
A total of 211 consecutive patients were approached for this survey study, of which 143 patients completed the survey (response rate, 67%). Table 1 summarizes the demographic characteristics of the survey participants. All but one had a diagnosis of colorectal (anal cancer, n = 1). The median age group was 61 to 70 years, and a majority (n = 115; 82%) were male. Most of the respondents did not have any additional risk factors for COVID-19 (n = 100; 73%). For 73 (54%) patients, their disease was under control or they had no active disease (Table 1). Of note, 24 (17%) patients were living alone.
Table 1.
Participant Demographics (n = 143)
| Demographics | N | % |
|---|---|---|
| Age, y (n = 142) | ||
| 31-40 | 11 | 7.7 |
| 41-50 | 14 | 9.9 |
| 51-60 | 29 | 20.4 |
| 61-70 | 44 | 31.0 |
| 71-75 | 27 | 19.0 |
| >75 | 17 | 12.0 |
| Gender (n = 140) | ||
| Male | 115 | 82.1 |
| Female | 25 | 17.9 |
| Living alone (n = 140) | ||
| No | 114 | 82.6 |
| Yes | 24 | 17.4 |
| Disease status (n = 136) | ||
| No active disease or under control | 73 | 53.7 |
| Progressive disease | 24 | 17.6 |
| In progress, unknown, or other | 39 | 28.7 |
| Treatment status (n = 124) | ||
| Not changed | 95 | 76.6 |
| Delayed, break, or canceled | 29 | 23.4 |
| High-risk for COVID-19 (n = 137) | ||
| No | 100 | 73.0 |
| Yes | 37 | 27.0 |
Abbreviation: COVID-19 = Coronavirus disease 2019.
Preferences in Method of Consultation
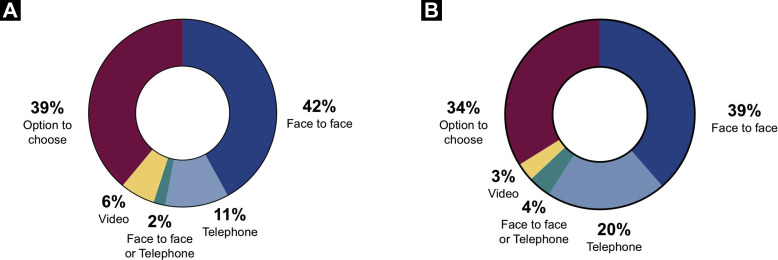
Owing to the COVID-19-imposed measures, 78% (n = 112) of participants had telephone consultations. The large majority (n = 95/114%; 83%) of patients reported that telephone consultations met their needs. Only 6 participants had video consultation during the survey period with high acceptance rate (80%). When participants were asked to indicate their preferred method of consultation, face-to-face consultation was still preferred (n = 57; 40%), although 38% (n = 54) wanted to be given the option to choose their preferred method for future consultations (Figure 1 A).
Figure 1.
Participants’ Preferences for Future Clinical Appointments For Clinic Review (A), and Receiving Results of Radiologic Scans (B), Following Their Experience of Changes in Cancer Care Imposed During the Initial Phase of the Coronavirus Disease 2019 (COVID-19) Pandemic
Changes in Radiology and Clinic Appointments
There were 14 (10%) participants who had their assessment scans delayed or canceled, and all but one felt that the reason for this had been explained to them. Fifty-seven (40%) participants had their scan results discussed over the phone, and the majority (n = 51/53%; 96%) reported that the discussion met their needs to some extent, if not fully. In the future, however, they would prefer the discussion to be face-to-face (n = 49; 34%) or to be given the option to choose (n = 43; 30%) the way their scan results will be disclosed (Figure 1B).
Importantly, more than 90% (n = 131) of respondents felt safe to visit the treating hospital. Many patients (n = 91; 65%) had to come to their hospital appointments unaccompanied, and most felt that the reason for this was explained to them. However, 63% (n = 53) of the respondents felt that no alternative arrangements were offered to involve a family member.
COVID-19 Exposure
In our cohort, only a minority (n = 2) have had COVID-19 and needed to be admitted (see Supplemental Table 1 in the online version). At the time of this survey, more than two-thirds (n = 107; 77%) have never been tested for the virus. About one-half (n = 50; 44%) of those who had not been tested would have liked to have the test. Interestingly, 1 (n = 32) in 4 participants did not feel that they had enough communication about the pandemic.
Assessing the Mental Health Impact of COVID-19
The psychological effect of the COVID-19 pandemic was also explored. One-third (n = 43) of the participants were concerned about the negative impact of the pandemic on their cancer care, and almost 80% (n = 110) were worried about contracting the infection (see Supplemental Table 1 in the online version). A large majority of respondents (87%; n = 118) denied that they were more concerned about COVID-19 than their cancer. Indeed, in our cohort of patients, more than 60% (n = 88) were not worried at all about the effect of the pandemic on their mental health, nor were they worried about the effect of the mental health on their cancer care (n = 113; 85%) (see Supplemental Table 1 in the online version). More than two-thirds (n = 87) did not feel that they needed support, and this is concordant to the fact that majority (n = 118; 89%) did not feel they wanted more support in addition to the existing ones (see Supplemental Table 1 in the online version).
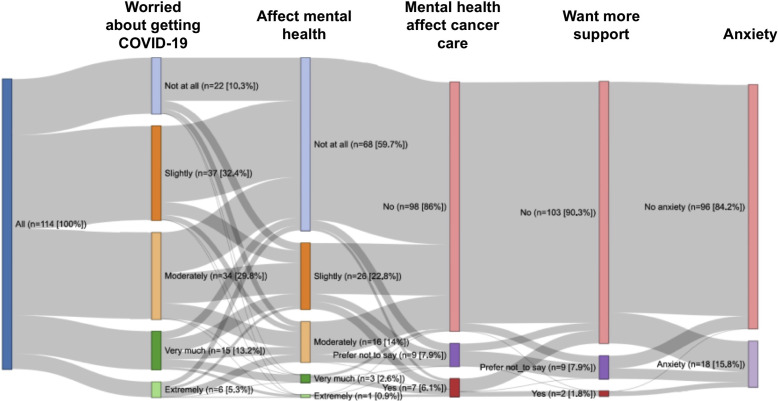
Anxiety (GAD-7)
A total of 125 patients completed the GAD-7 questionnaire. Objectively, 23 (18%) participants were considered to have anxiety according to the GAD-7 scale (GAD-7 score ≥ 5): 16 (12.5%) patients with mild anxiety (GAD-7 score, 5-9), and 7 (5.5%) patients with moderate or severe anxiety (GAD-7 score ≥ 10). After Benjamini and Hochberg false discovery rate correction, anxiety levels were correlated with those who had concerns about getting the infection, worried that COVID-19 would have effect on mental health and affect their experience of cancer care, and those wanted more support (P < .001) (Table 2 ). The initial 3 parameters were significantly associated with higher risk of anxiety in multivariate analysis (OR, 2.361; 95% CI, 1.187-4.694; OR, 3.219; 95% CI, 1.401-7.395; and OR, 3.206; 95% CI 1.036-9.920, respectively) (Table 2). The relationship of these parameters with anxiety is illustrated in Figure 2 .
Table 2.
Univariate and Multivariate Analyses of Factors Associated With Anxiety as Scored by Generalized Anxiety Disorder-7 (GAD-7) Screening Tool
| Variables | Responses | Univariate Analysis |
Multivariate analysis |
||||
|---|---|---|---|---|---|---|---|
| n (%) | No Anxiety, n (%) | Anxiety, n (%) | P | Odds Ratio (95% CI) | P | ||
| Concerns about getting the infection (n = 125) | Not at all | 25 (20.0) | 25 (24.5) | 0 (0) | <.001 | 2.361 (1.187-4.694) | .014 |
| Slightly | 42 (34.0) | 37 (36.3) | 5 (21.7) | ||||
| Moderately | 34 (27.2) | 29 (28.4) | 5 (21.7) | ||||
| Very much | 15 (13.6) | 8 (7.8) | 9 (39.1) | ||||
| Extremely | 7 (5.6) | 3 (2.9) | 4 (17.4) | ||||
| I feel the COVID-19 pandemic situation has affected my mental health (n = 127) | Not at all | 78 (61.4) | 73 (70.2) | 5 (21.7) | <.001 | 3.219 (1.401-7.395) | .006 |
| Slightly | 21 (22.0) | 21 (20.2) | 7 (30.5) | ||||
| Moderately | 10 (13.4) | 10 (9.6) | 7 (30.5) | ||||
| Very much | 3 (2.4) | 0 (0) | 3 (13.0) | ||||
| Extremely | 1 (0.8) | 0 (0) | 1 (4.3) | ||||
| My mental health has affected my experience of cancer care (n = 120) | No | 104 (86.7) | 93 (93.0) | 11 (55.0) | <.001 | 3.206 (1.036-9.920) | .043 |
| Yes | 7 (5.80) | 2 (2.0) | 5 (25.0) | ||||
| Prefer not to say | 9 (7.5) | 5 (5.0) | 4 (20.0) | ||||
| Wanted more support (n = 119) | No | 108 (90.8) | 94 (94.9) | 14 (70.0) | <.001 | 1.283 (0.387-4.250) | .683 |
| Yes | 2 (1.7) | 0 (0) | 2 (10.0) | ||||
| Prefer not to say | 9 (7.5) | 5 (5.6) | 4 (20.0) | ||||
Abbreviations: CI = Confidence interval; COVID-19 = Coronavirus disease 2019.
Figure 2.
Sankey Diagram of How Individual Patients Responded to 4 Items in This Survey (Worried About Getting Coronavirus Disease 2019 [COVID-19], Affect Mental Health, Mental Health Affect Cancer Care and Want More Support) and Their Association to Self-Reported Anxiety (n = 114; Only Patients With Valid Data in All the Fields of the Graph are Included in This Plot). The Vertical Colored Bars Denote the Patient Cohort, Split Into Different Groups. The Gray Horizontal Bars Denote Associations Between the Different Groups, With Wider Bars Denoting More Overlap
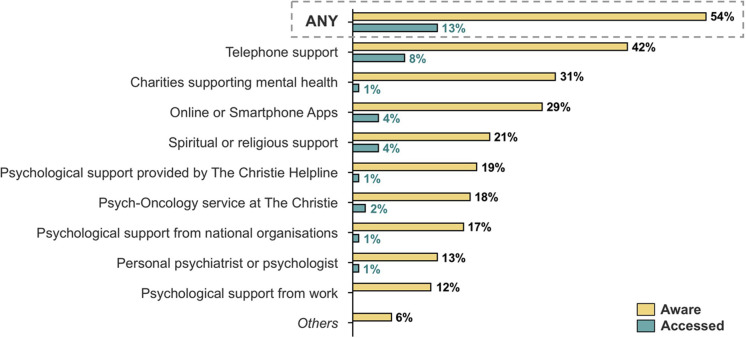
Support Available During COVID-19
More than one-half (n = 77) of the patients seemed to be aware of the various support services available to them during the COVID-19 pandemic, particularly in the form of telephone support and those charities supporting mental health (Figure 3 ). Nevertheless, only a minority (n = 18; 13%) had accessed these support services.
Figure 3.
Responses to Which Well-being Support Services Participants Were Aware of And/Or Accessed During the Coronavirus Disease 2019 (COVID-19) Pandemic (n = 143)
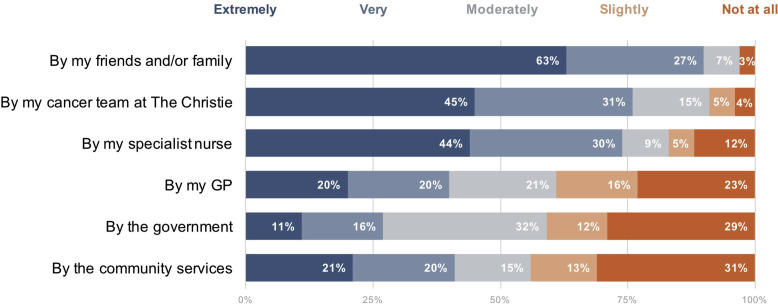
Moreover, almost all (n = 119; 97%) patients reported that they were well-supported by their families and friends (Figure 4 ). In terms of rating the support received, patients reported they were moderately to extremely well-supported by their care providers as follows: cancer team (n = 113/124%; 91%), nurse specialists (n = 88/106%; 83%), general practitioners (n = 66/108%; 61%), and community services (n = 53/95%; 56%). Fifty-nine percent (n = 61/104) felt moderately to extremely well-supported by the government. The differences between the various groups were statistically significant (P < .05).
Figure 4.
An Overview of How Well-supported (5-Point Likert Scale: Not at All to Extremely Well) Participants Have Felt During the Coronavirus Disease 2019 (COVID-19) Pandemic. The Percentages are Based on Valid Data (n = 95-124) Without Considering System and User Missing (Not Applicable: NA) Data
Abbreviation: GP = General practitioner.
Discussion
COVID-19 has undeniably resulted in significant personal changes in the lives of patients diagnosed with cancer. Initial reports have suggested that this has been accompanied by significant impact on the quality of life, and increasing levels of anxiety and depression during the period of the pandemic.10, 11, 12, 13 In this report, we present for the first time how patients diagnosed with colorectal cancer have perceived the changes imposed on them personally and owing to changes in their cancer care during the pandemic.
Alternative methods of consultation have been used to reduce hospital footfall and provide a COVID-19–secure environment. This has been reflected in our survey, as 90% of the participants felt safe to visit the treating hospital. In addition, both methods of remote consultation (telephone and video) were very well-received, and they should remain as possible options for the future, beyond the restrictions of the pandemic. During the period of the survey, facilities for video consultations were not as well-established, and hence, only a minority of patients had this mode of clinical encounter. Our results may indicate that some scan results can be easily delivered by telephone. It might be that the perceived completeness of the information received is linked to the outcome, though. It will be essential to consider accommodating family members in such consultations as per patients’ wishes.
Despite the high levels of concern shared by health professionals and health authorities on the risk of COVID-19 infection, our cohort of patients were more worried about their cancer diagnosis and continuing to receive optimal cancer care. Recently published data on the largest cohort of patients with cancer on anti-neoplastic treatment in the UK have indicated that there was no higher mortality risk from COVID-19 disease compared with those not on treatment.14 Results from a smaller cohort of patients with COVID-19 indicated that cancer did not seem to increase the risk of mortality.15 Therefore, we believe that it would be reasonable to continue treatment for our patients after the appropriate risk assessment on an individual basis.
During the initial period of the pandemic in the UK, a lot of effort had been invested to ensure that patients were provided with adequate support. Nevertheless, anecdotally, patients were on occasion confused by the advice given and often worried by the letters they received from Public Health England about shielding and self-isolation. In our cohort of survey participants, to our disappointment, one-half were still unaware of the relevant services available, and even more worrisome was the lack of awareness of the services provided through the treating hospital. Although lockdown restrictions and shielding being in place during the survey period may have resulted in this lack of awareness, the results of this survey might indicate that more targeted interventions will be needed to reach out to patients. Nevertheless, it was unsurprising therefore that only a few participants used these services, as the majority did not feel that they actually needed support during this time.
Furthermore, we asked the participants how well-supported they felt from the hospital, community services, and the government, as well as friends and family. Family and friend support scored the highest when compared with the rest of the items in this question. This might have had an impact on the lower levels of anxiety reported, as the importance of family and friend support on quality of life with has been previously well-described.16 In our cohort, there was no direct association between this and anxiety levels. However, the fact that general practitioner and community services scored low will need to be considered carefully from the primary care sector. There have been significant changes in this area during the pandemic that could potentially explain the finding; however, patients’ expectations could be higher during this period and not actually met. The low score for the government support will need to be further understood with more in-depth analysis of patients’ expectation in subsequent surveys.
In our cohort, the levels of self-reported anxiety were similar or lower, compared with previous studies in patients with colorectal cancer.17, 18, 19 However, it remains noteworthy that only 6% of our patients reported moderate or severe anxiety that would trigger further intervention, which might reflect the support they were getting from friends and family as well as the treating team during this challenging period. We could not identify these participants owing to the anonymous nature of this survey, but as part of the survey, participants were signposted to support services if required. These results are similar to the ones from the recently presented French study, where 6% of the participants reported severe stress, although in this report, the number of patients with colorectal cancer was smaller.13 In our detailed analysis, we could not specifically identify any ‘at risk’ groups that would need more support. Interestingly, neither patients who were considered high-risk of COVID-19 nor those living alone were more anxious. The fact that this survey was done in a tertiary cancer center, where the overall support is expected to be better, could potentially explain this observation. Noticeably, treatment delays or deferrals did not increase anxiety levels.
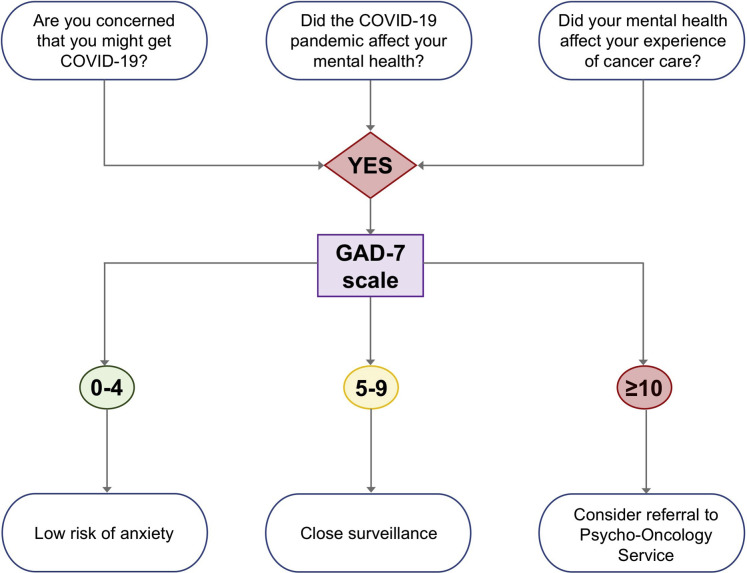
As the pandemic continues, we plan to prospectively identify patients who might need further mental health support. In our cohort, we were able to identify that answers to 3 particular questions were linked to anxiety. Because those participants who felt that the pandemic had affected their mental health were at an increased risk of suffering from anxiety, further work to validate these results in an external cohort could potentially be used to triage the psychological needs and explore ongoing assessments and support. We suggest an easy and practical pre-screening assessment questionnaire that might help identify those in more need of further support, especially in services where screening of anxiety is not an integral part of cancer service delivery (Figure 5 ). Once validated, this finding could potentially be applicable to future life-altering crises, including a pandemic. In addition, addressing the higher anxiety related to the perceived changes in care delivered and that related to contracting the virus might also be beneficial.
Figure 5.
Proposed Schematic Model of a Screening Tool That Can be Incorporated Into Routine Delivery of Cancer Care to Triage the Need For Further Support From Psycho-Oncology Service
Abbreviations: COVID-19 = Coronavirus disease 2019; GAD-7 = General Anxiety Disorder-7.
Despite the strengths of our study in providing contemporary results in a large cohort of patients with colorectal cancer, we have to acknowledge the limitations of a survey. The survey was done in a tertiary cancer canter, and these results may not be applicable in practices whereby support services might be more restricted (eg, by lack of psycho-oncology services, dedicated clinical nurse specialists, mental health helpline, etc). We were also not able to formally assess other important factors contributing to overall well-being (eg, depression or suicidal ideation), as this was a quality improvement project, and we did not want to overwhelm patients with lengthy questionnaires during this already stressful era. Despite this, our data could be used to improve patients’ experience by understanding their expectations and tailoring interventions to address their needs. Likewise, the survey was conducted during the initial phase of the pandemic. Changes in delivery of health services is an ongoing effort to identify the best and an optimal model where possible, incorporating the rapidly evolving evidence as they are reported. The impact of these changes will need to be evaluated in subsequent studies.
Conclusion
The findings of this survey suggest that some of the service changes already implemented, such as increased telephone follow-up, may well improve the overall experience of cancer care for patients and the efficient running of cancer centers. Also, it is reassuring that the incidence of participants with moderate to severe anxiety levels during the peak of the COVID-19 pandemic in the UK were much less than we anticipated. Importantly, patients were much more concerned about their cancer treatment than COVID-19, emphasizing the need to continue to provide comprehensive cancer care even if we get a “second wave” of COVID-19.
Clinical Practice Points
-
•
COVID-19 has imposed significant challenges in the management of patients diagnosed with cancer.
-
•
There have been several national and international published recommendations on how cancer treatment may be safely altered during the peak of the pandemic, but patients’ perception of these have not been assessed.
-
•
The incidence of participants with moderate to severe anxiety levels during the peak of the COVID-19 pandemic in the UK were much less than anticipated.
-
•
Patients were much more concerned about their cancer treatment than COVID-19, emphasizing the need to continue to provide comprehensive cancer care even if we get a “second wave” of COVID-19.
-
•
An easy and practical pre-screening assessment questionnaire might be used to help identify those in more need of further support.
Disclosure
MS reports personal fees from Servier Global, Merck, UK, and Amgen, UK, outside the submitted work. JB reports grants and non-financial support from Ipsen, non-financial support from Novartis, personal fees and non-financial support from Pfizer, non-financial support from AAA, non-financial support from Nanostring, Unites States, and personal fees from Nutricia, Netherlans, outside the submitted work. The remaining authors have stated that they have no conflicts of interest.
Acknowledgments
The authors would like to thank the Macmillan User Involvement group at the Stockport NHS Foundation Trust for their useful feedback and contribution in the design of the final survey used in this study. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. KHJL is currently funded by the Wellcome-Imperial 4i Clinical Fellowship.
Footnotes
Supplemental table accompanying this article can be found in the online version at https://doi.org/10.1016/j.clcc.2020.11.006.
Supplemental Data
Supplemental Table 1.
Personal COVID-19–Related Questions
| COVID-19–Related Questions | N | % |
|---|---|---|
| COVID-19 test (n = 139) | ||
| No | 107 | 77.0 |
| Yes | 32 | 23.0 |
| Test positive (n = 139) | ||
| No | 28 | 20.1 |
| Yes | 2 | 1.4 |
| N/A | 109 | 78.4 |
| Would you like to be tested? (n = 113) | ||
| No | 58 | 51.3 |
| Yes | 50 | 44.2 |
| N/A | 5 | 4.4 |
| Hospitalization (n = 115) | ||
| No | 112 | 97.4 |
| Yes | 2 | 1.7 |
| N/A | 1 | .9 |
| Adequate communication about COVID-19 (n = 134) | ||
| No | 32 | 23.9 |
| Yes, definitely | 61 | 45.5 |
| Yes, to some extent | 41 | 30.6 |
| Concerns about COVID-19 | ||
| Concern about negative impact of COVID-19 (n = 136) | ||
| No | 55 | 40.4 |
| Yes | 43 | 31.6 |
| Don't know | 38 | 27.9 |
| More concern than cancer (n = 135) | ||
| No | 118 | 87.4 |
| Yes | 16 | 11.9 |
| Don't know | 1 | .7 |
| Concerns about getting the infection (n = 139) | ||
| Not at all | 29 | 20.9 |
| Slightly | 46 | 33.1 |
| Moderately | 35 | 25.2 |
| Very much | 19 | 13.7 |
| Extremely | 10 | 7.2 |
| Assessing psychological impact of COVID-19 | ||
| Effect on mental health (n = 141) | ||
| Not at all | 88 | 62.4 |
| Slightly | 29 | 20.6 |
| Moderately | 19 | 13.5 |
| Very much | 3 | 2.1 |
| Extremely | 2 | 1.4 |
| Support from Christie (n = 129) | ||
| No | 23 | 17.8 |
| Yes | 5 | 3.9 |
| I did not need support | 87 | 67.4 |
| Prefer not to say | 14 | 10.9 |
| My mental health has affected my experience of cancer care (n = 133) | ||
| No | 113 | 85.0 |
| Yes | 10 | 7.5 |
| Prefer not to say | 10 | 7.5 |
| Wanted more support (n = 132) | ||
| No | 118 | 89.4 |
| Yes | 4 | 3.0 |
| Prefer not to say | 10 | 7.6 |
Abbreviations: Christie = The Christie NHS Foundation Trust; COVID-19 = Coronavirus disease 2019; N/A = not applicable.
References
- 1.National Institute of Health and Care Excellence (NICE) guideline [NG161] COVID-19 rapid guideline: delivery of systemic anticancer treatments. https://www.nice.org.uk/guidance/ng161 Available at: [PubMed]
- 2.European Society for Medical Oncology (ESMO) Cancer patient management during the covid-19 pandemic. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic Available at:
- 3.Mauri D., Kamposioras K., Tolia M., Alongi F., Tzachanis D., International Oncology Panel and European Cancer Patient Coalition collaborators. Summary of international recommendations in 23 languages for patients with cancer during the COVID-19 pandemic. Lancet Oncol. 2020;21:759–760. doi: 10.1016/S1470-2045(20)30278-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Health and Social Care (United Kingdom) Guidance on shielding and protecting extremely vulnerable persons from COVID-19. 2020. https://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19 Available at:
- 5.Colorectal Cancer COVID Research Collaborative The impact of the COVID-19 pandemic on colorectal cancer service provision. Br J Surg. 2020;107:e521–e522. doi: 10.1002/bjs.11990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loveday C., Sud A., Jones M.E., et al. Prioritisation by FIT to mitigate the impact of delays in the 2-week wait colorectal cancer referral pathway during the COVID-19 pandemic: a UK modelling study. Gut. 2020 doi: 10.1136/gutjnl-2020-321650. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.D’Ovidio V., Lucidi C., Bruno G., Lisi D., Migliorisi L., Bazuro M.E. Impact of COVID-19 pandemic on colorectal cancer screening program. Clin Colorectal Cancer. 2020 doi: 10.1016/j.clcc.2020.07.006. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo Y., Cheng C., Zeng Y., et al. Mental health disorders and associated risk factors in quarantined adults during the COVID-19 outbreak in China: a cross-sectional study. J Med Internet Res. 2020;22:e20328. doi: 10.2196/20328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A brief measure for assessing generalized anxiety disorder. Arch Intern Med. 2006;166:1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 10.Frey M.K., Ellis A.E., Zeligs K., et al. Impact of the COVID-19 pandemic on quality of life for women with ovarian cancer. Am J Obstet Gynecol. 2020;223:725.e1–725.e9. doi: 10.1016/j.ajog.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Košir U., Loades M., Wild J., et al. The impact of COVID-19 on the cancer care of adolescents and young adults and their well-being: results from an online survey conducted in the early stages of the pandemic. Cancer. 2020;126:4414–4422. doi: 10.1002/cncr.33098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Romito F., Dellino M., Loseto G., et al. Psychological distress in outpatients with lymphoma during the COVID-19 pandemic. Front Oncol. 2020;10:1270. doi: 10.3389/fonc.2020.01270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joly F., Leconte A., Grellard J.-M., et al. LBA69: Impact of the COVID-19 pandemic on management of medical cancer treatments and psychological consequence for the patients. Ann Oncol. 2020;31:S1200. [Google Scholar]
- 14.Lee L.Y., Cazier J.-B., Angelis V., et al. UK Coronavirus Monitoring Project Team. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395:1919–1926. doi: 10.1016/S0140-6736(20)31173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Joharatnam-Hogan N., Hochhauser D., Shiu K.-K., et al. Outcomes of the 2019 novel coronavirus in patients with or without a history of cancer: a multi-centre North London experience. Ther Adv Med Oncol. 2020;12 doi: 10.1177/1758835920956803. 1758835920956803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yan B., Yang L.-M., Hao L.-P., et al. Determinants of quality of life for breast cancer patients in Shanghai, China. PLoS One. 2016;11:e0153714. doi: 10.1371/journal.pone.0153714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Powell-Chandler A., Boyce K., James O., et al. PISA Trial Management Group Psychological sequelae of colonic resections. Colorectal Dis. 2020;22:945–951. doi: 10.1111/codi.14986. [DOI] [PubMed] [Google Scholar]
- 18.Mols F., Schoormans D., de Hingh I., Oerlemans S., Husson O. Symptoms of anxiety and depression among colorectal cancer survivors from the population-based, longitudinal PROFILES Registry: prevalence, predictors, and impact on quality of life. Cancer. 2018;124:2621–2628. doi: 10.1002/cncr.31369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aminisani N., Nikbakht H., Jafarabadi M.A., Shamshirgaran S.M. Depression, anxiety, and health related quality of life among colorectal cancer survivors. J Gastrointest Oncol. 2017;8:81–88. doi: 10.21037/jgo.2017.01.12. [DOI] [PMC free article] [PubMed] [Google Scholar]