Abstract
Purpose
During the COVID-19 pandemic, there is growing concern that patients are forgoing necessary care. Emergency departments (ED) represent an important site of eye care. We analyzed patterns of ED visits at an eye-specific ED since the declaration of the public health crisis.
Materials and Methods
In this retrospective, cross-sectional single center study, medical records of 6744 patients who presented to the Massachusetts Eye and Ear ED between March 1st and April 30th in 2018, 2019, and 2020 were studied. The primary outcome measures were total volume of ED visits, proportion of urgent ED visits, and proportion of surgical visits.
Results
Overall, the median number of daily visits to the ED decreased by 18 visits per day since the declaration of public health guidelines (interquartile range, 9–24, p < 0.001). This accounted for a 32% decrease in the total volume of ED visits in 2020 compared to prior years during the study period (p < 0.001). There was a 9% increase in the proportion of primary diagnoses considered urgent (p = 0.002). The proportion of visits requiring urgent surgery increased by 39% (p = 0.004).
Conclusion
The total number of eye-specific ED visits dropped compared to prior years while the proportion of urgent visits increased. Patients were likely more reluctant to seek eye care, deferring less urgent evaluation.
Keywords: COVID-19, urgent ophthalmic diagnoses, epidemiology, eye-specific emergency department, medical services
Introduction
Coronavirus disease 2019 (COVID-19) is an emerging respiratory infectious disease that was first detected in early December 2019 in Wuhan, China.1 As of October 20th, 2020, COVID-19 has spread quickly throughout the world, with more than 40 million people infected and 1.1 million people dead.2 In the United States, the second half of March was marked by constantly evolving public health policies. On March 15th, the Center for Disease Control (CDC) recommended social distancing.3 In Massachusetts, Governor Charlie Baker ordered the closure of nonessential businesses on March 23rd and issued a stay-at-home advisory on March 24th.4,5 More specifically for ophthalmologists, on March 18th, the American Academy of Ophthalmology (AAO) issued a guideline “to cease any treatment other than urgent or emergent eye care immediately.”6 The decision on how to define urgency was left to the individual physician, leaving physicians without clear guidelines and forcing physicians to carefully weigh the risks and benefits of delayed care for individual patients.7
Amidst the COVID-19 crisis and social distancing recommendations, the medical community has voiced concerns that some patients may be forgoing necessary care due to fear of accessing the healthcare system.8–11 A recent study has shown that the number of general medical emergency department (ED) visits has declined 42% during the early COVID-19 pandemic.12 Another recent study has shown that during the national lockdown in Italy, the number of total visits to an eye-specific ED in Bologna, Italy has decreased while the proportion of diagnoses considered emergent has increased.13 In our region, many large ophthalmic community-based practices temporarily closed all clinical sessions. While ophthalmic care is routinely provided on a nonurgent, outpatient basis, there are eye-specific EDs in the US and worldwide which provide direct ophthalmic care for eye emergencies, urgencies, and other walk-in evaluations.
Understanding patterns in eye-related emergency department visits during this pandemic can provide insight to the potential toll of COVID-19 on timely ophthalmic care. This understanding can guide ophthalmologists as we reopen and adjust to the “new normal.”14 We hypothesized that there would be an overall reduction in the number of visits to an eye-specific ED after the institution of public health guidelines. Furthermore, we hypothesized that the proportion of urgent eye diagnoses would be higher, as patients with less urgent diagnoses were more likely to stay home or seek other eye care options.
In this study, we extend the works of Pellegrini et al to evaluate the impact of the COVID-19 pandemic on the number of patients and the proportion of urgent diagnoses presenting to an eye-specific ED. This study is also the first study to look at changes in surgical volumes as a result of the COVID-19 pandemic at an eye-specific ED. We present a retrospective, cross-sectional study of patients presenting to the Massachusetts Eye and Ear Emergency Department, a 24-hour ophthalmology-specific ED in Boston, MA, amidst the COVID-19 pandemic.
Materials and Methods
Data Collection
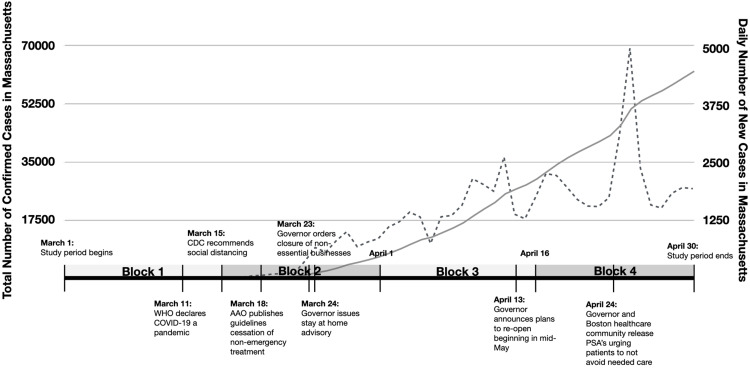
Data was collected retrospectively from charts of 6744 patients who were seen by an ophthalmologist at the Massachusetts Eye and Ear (MEE) Emergency Department (ED) between March 1st–April 30th for three consecutive years (2018–2020). The study period was broken into four blocks for each year: March 1st–March 15th, March 16th–March 31st, April 1st–April 15th, and April 16th–April 30th in order to capture evolving public health policies and rising community prevalence of COVID-19 in Massachusetts. The first block represents a period when there were relatively few public health guidelines; the second block represents a period with rapidly evolving guidelines after the CDC recommended social distancing; the third and fourth blocks represent periods with relative stability with guidelines in place. The study period also represents a period with rapidly rising prevalence and number of daily new cases of COVID-19 in Massachusetts, as shown in Figure 1. As of October 25th, 2020, the highest recorded number of daily new cases in Massachusetts occurred on April 24th, 2020, with 4946 new cases.15
Figure 1.
Timeline of announcements of public health recommendations regarding COVID-19 in Massachusetts and in the United States between March 1st, 2020 and April 30th, 2020 overlaid on graph of number of cumulative confirmed cases of COVID-19 in Massachusetts during the same time period (solid line) and number of daily new cases of COVID-19 in Massachusetts during the same period (dashed line).
Patients who were seen by an ophthalmology attending or trainee in the MEE ED for an initial visit during the study period were included in the study. The primary outcome measures in this study were the total volume of daily ED visits, the proportion of diagnoses considered urgent, and the proportion of patients who needed urgent surgeries or procedures. Diagnoses and interventions were documented with billing codes (ICD-10-CM). Secondary outcome measures used were visual acuity upon presentation and average time between first presentation and follow up.
Diagnostic groups were created by combining ICD-10-CM codes into clinically meaningful groups. The list of urgent diagnoses, defined as diagnoses that required intervention within 72 hours to avoid negative consequences to vision, was utilized from a previously published study on ophthalmic emergency room diagnoses, and a list of diagnoses requiring urgent surgeries was created manually by going through the list of all unique primary diagnoses made in the MEE ED during the study period.16 Urgent surgical diagnoses were defined as diagnoses that required surgery within 72 hours to avoid negative consequences to vision. Three expert ophthalmologists reviewed the list of diagnoses independently and came to a consensus. 271 patients with a primary ENT diagnosis were excluded in the analysis of urgent visits and surgical visits. However, as these patients presented with concerns that required evaluation by both an ophthalmologist and an otolaryngologist, they were included in other analyses.
Visual acuity (VA) data was collected using the Snellen chart and was converted to logMAR scale for analysis.17 The logMAR scale was chosen for easy linear comparison between data points. 210 patients who were unable to participate in the measurement of visual acuity (eg, infants, patients with altered mental status) were excluded in the VA analysis.
Statistical Analysis
Distribution of continuous data was checked by Shapiro–Wilk Normality test. Normally distributed data, including age and the number of days to follow up visits, was analyzed using Student’s t-test to assess statistically significant difference. Data which was not normally distributed, including total number of visits from year to year and visual acuity, was analyzed using Mann–Whitney U-test. Tukey’s Honest Significance test was used for block-wise comparisons in number of visits in each block. Two-Proportions Z-test was used to assess gender breakdown, racial breakdown, and the breakdown of urgent and urgent surgical visits. Linear regression models were used to better understand trends in ED visits over time. Every patient was accounted for in each analysis, and the sample size was reflected accordingly unless noted otherwise. Prevalence ratios and their confidence intervals were calculated using the Wald test. Alpha = 0.05 was used for data analysis. Analyses were performed using R software (R Foundation for Statistical Computing).18 Charts and tables were also generated with R, using the ggplot2 package.19
Ethics Approval
Institutional review board approval was obtained from Partners Healthcare for the Protection of Human Subjects. The authors certify that this work is HIPAA compliant and adhered to the tenets of the Declaration of Helsinki.
Results
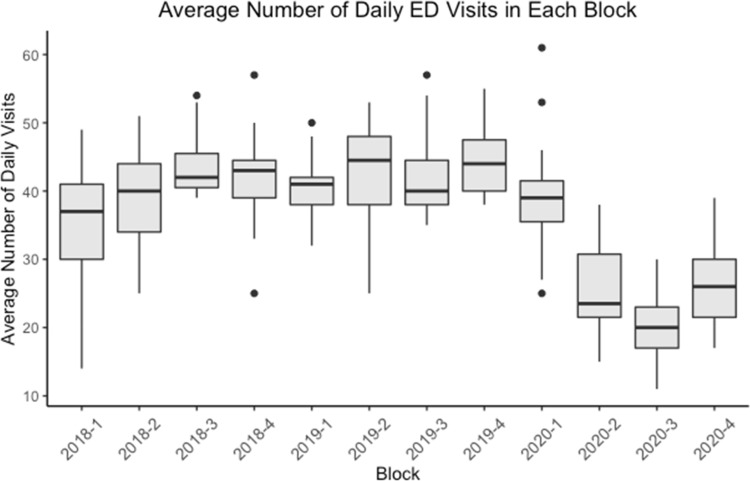
There were 2426, 2616, and 1702 initial ophthalmology visits to the ED between March 1st and April 30th in 2018, 2019, and 2020, respectively. The total number of visits to the ED fell by 32% in 2020 compared to the mean of prior years (p < 0.001). Particularly, looking at the average number of daily visits for each half-month block, there was a statistically significant decrease in the average number of daily visits to the ED in block 2, block 3, and block 4 of 2020 compared to all other blocks in pairwise comparisons (Figure 2, p < 0.01). All other pairs did not show any statistically significant difference, except for 2018–1 compared to 2018–3 and 2019–4 (p = 0.026 and 0.010). Overall, comparing visits before March 15th, 2020 to visits after March 15th, 2020, the median number of daily visits decreased by 18 visits (p < 0.001, interquartile range: 9–24) from a median of 40 visits daily prior to March 15th, 2020 to a median of 22 visits after March 15th, 2020. A linear regression analysis showed a statistically significant (p = 0.004) positive (β = 59.49) trend in the number of daily visits in 2018, no statistically significant trend in 2019 (p = 0.09), and a statistically significant (p < 0.001) negative (β = −110.37) trend in 2020.
Figure 2.
Boxplot of the average number of daily visits in each half-month block during the study period in 2018, 2019, and 2020.
The average age of patients was 48.70 in 2018, 48.22 in 2019, and 50.06 in 2020. Patients presenting to the ED in 2020 were on average 1.84 (0.65–3.02, p = 0.002) years older than patients presenting to the ED in 2019 and 1.36 (0.16–2.55, p = 0.03) years older than patients presenting to the ED in 2018. There was no statistically significant difference in the mean age between 2018 and 2019 during the study periods. 51% of patients presenting to the ED were female in 2020, while 54% of patients were female patients in both 2018 and 2019 (p = 0.107). The proportion of patients who identified as Asian decreased to 4% in 2020 from 7% and 6% in 2018 and 2019 respectively (p < 0.001). The proportion of patients who identified as Hispanic changed from 1% in 2018 to 0.5% in 2019 to 1% in 2020 (p = 0.019). There was no statistically significant change in the proportion of other racial groups (Table 1).
Table 1.
Demographic Information
| 2018 | 2019 | 2020 | P-value (t-Test) | ||
|---|---|---|---|---|---|
| Age | Mean Age (SD) | 48.70 (19.83) | 48.22 (20.24) | 50.06 (18.86) | 0.002*, 0.03* |
| Gender | Male (%) | 1103 (46%) | 1215 (46%) | 830 (49%) | 0.107 |
| Female (%) | 1323 (54%) | 1401 (54%) | 872 (51%) | 0.107 | |
| Race | White (%) | 1684 (69%) | 1810 (69%) | 1160 (68%) | 0.668 |
| Black (%) | 256 (11%) | 260 (10%) | 160 (9%) | 0.471 | |
| Asian (%) | 164 (7%) | 161 (6%) | 67 (4%) | < 0.001* | |
| Hispanic (%) | 31 (1%) | 14 (0.5%) | 18 (1%) | 0.019* | |
| Native Americans (%) | 6 (0.2%) | 5 (0.2%) | 1 (0.1%) | 0.360 | |
| Other (%) | 234 (10%) | 257 (10%) | 182 (11%) | 0.503 | |
| Declined (%) | 51 (2%) | 110 (4%) | 114 (7%) | 0.457 |
Note: *p <0.05.
Regarding the change in the level of urgency of visits, the volume of nonurgent visits fell by 37% in 2020 compared to prior years while the volume of urgent visits fell by only 26% compared to prior years. While the volume of both types of visits fell, the volume of nonurgent visits decreased by a greater degree. Put another way, a statistically significantly greater proportion of visits were considered urgent in 2020 compared to prior years; 41%, 40%, and 45% of the visits were considered urgent during the study period in 2018, 2019, and 2020 respectively, accounting for a 9% increase in the proportion of visits considered urgent in 2020 compared to prior years (p = 0.017). Similarly, the proportion of visits requiring urgent surgical intervention increased by 39% in 2020 compared to prior years (p = 0.004). Looking at the breakdown of types of surgery performed, the most common indications for surgery were retinal detachment, retinal tear, and trauma for all three years. There was no statistically significant difference in the reasons for surgery across the years.
There were 721 unique primary ICD-10-CM diagnoses made during the study period. These 721 ICD-10-CM codes were combined into 182 clinically meaningful diagnostic groups. Looking more closely at the frequency of primary diagnostic groups, the five most frequent diagnostic groups remained fairly consistent in 2018 and 2019. However, in 2020, diagnoses such as vitreous degeneration, foreign body, and retinal detachment were made more frequently compared to prior years (Table 2). Additionally, the prevalence ratio (PR) was calculated for each diagnostic group as the proportion of ED visits in 2020 divided by the proportion of ED visits in 2018 and 2019. Looking at the PR of diagnostic groups across the years, diagnostic groups such as contusion of the eyeball, retinal vascular occlusion, and retinal detachments were more prevalent in 2020 than in 2018 and 2019 (Table 3). Other diagnostic groups, such as eyelid disorders, contact lens related disorders (excluding keratitis), and allergic conjunctivitis were less prevalent in 2020 compared to 2018 and 2019 (Table 4).
Table 2.
Frequency and Prevalence Ratios of Diagnostic Groups. List of top 5 primary diagnostic groups that presented to the MEE ED between March 1st and April 30th in 2018, 2019, and 2020 with the corresponding number of presentations in parentheses. Analysis was performed for the entire study period as well as for the four blocks of each year. Visual disturbances was a diagnostic group that appeared in the top five diagnostic groups in many blocks across the years. It included visual disturbances such as aura, flashes, floaters, blurred vision, and visual field defects.
| Top 5 Diagnostic Groups, Overall and by Blocks (2018-2020) | ||||
| 2018 | ||||
| Overall (2426) | Block 1: 3/1 – 3/15 (525) | Block 2: 3/16 – 3/31 (627) | Block 3: 4/1 – 4/15 (646) | Block 4: 4/16 – 4/30 (628) |
| Hordeolum/chalazion (186) | Hordeolum/chalazion (36) | Injury of conjunctiva and corneal abrasion without foreign body (47) | Hordeolum/chalazion (54) | Hordeolum/chalazion (50) |
| Injury of conjunctiva and corneal abrasion without foreign body (151) | Injury of conjunctiva and corneal abrasion without foreign body (33) | Hordeolum/chalazion (46) | Injury of conjunctiva and corneal abrasion without foreign body (43) | Foreign body (41) |
| Keratitis (118) | Vitreous degeneration (32) | Keratitis (36) | Foreign body (29) | Keratitis (35) |
| Foreign body (108) | Keratitis (21) | Retinal detachment (24) | Visual disturbances (28) | Injury of conjunctiva and corneal abrasion without foreign body (28) |
| Vitreous degeneration (105) | Viral conjunctivitis (21) | Visual disturbances (23) | Vitreous degeneration (28) | Visual disturbances (28) |
| 2019 | ||||
| Overall (2616) | Block 1: 3/1 – 3/15 (609) | Block 2: 3/16 – 3/31 (682) | Block 3: 4/1 – 4/15 (656) | Block 4: 4/16 – 4/30 (669) |
| Hordeolum/chalazion (178) | Hordeolum/chalazion (52) | Injury of conjunctiva and corneal abrasion without foreign body (48) | Foreign body (44) | Vitreous degeneration (43) |
| Injury of conjunctiva and corneal abrasion without foreign body (155) | Injury of conjunctiva and corneal abrasion without foreign body (37) | Hordeolum/chalazion (45) | Hordeolum/chalazion (40) | Hordeolum/chalazion (41) |
| Foreign body (142) | Visual disturbances (32) | Foreign body (37) | Injury of conjunctiva and corneal abrasion without foreign body (34) | Injury of conjunctiva and corneal abrasion without foreign body (36) |
| Vitreous degeneration (112) | Foreign body (31) | Keratitis (27) | Vitreous degeneration (29) | Foreign body (30) |
| Visual disturbances (111) | Ocular pain (26) | Visual disturbances (26) | Visual disturbances (27) | Lacrimal gland dysfunction (27) |
| 2020 | ||||
| Overall (1702) | Block 1: 3/1 – 3/15 (593) | Block 2: 3/16 – 3/31 (411) | Block 3: 4/1 – 4/15 (302) | Block 4: 4/16 – 4/30 (396) |
| Vitreous degeneration (131) | Foreign body (45) | Injury of conjunctiva and corneal abrasion without foreign body (30) | Vitreous degeneration (31) | Vitreous degeneration (43) |
| Foreign body (118) | Hordeolum/chalazion (45) | Vitreous degeneration (28) | Foreign body (23) | Foreign body (28) |
| Injury of conjunctiva and corneal abrasion without foreign body (110) | Injury of conjunctiva and corneal abrasion without foreign body (34) | Hordeolum/chalazion (26) | Injury of conjunctiva and corneal abrasion without foreign body (23) | Injury of conjunctiva and corneal abrasion without foreign body (23) |
| Hordeolum/chalazion (109) | Vitreous degeneration (29) | Foreign body (22) | Hordeolum/chalazion (18) | Keratitis (21) |
| Retinal detachment (70) | Visual disturbances (25) | Retinal detachment (20) | Retinal detachment (10) | Hordeolum/chalazion (20) |
Table 3.
Prevalence Ratios of Diagnostic Groups. Diagnostic groups that are more prevalent in 2020 compared to prior years, as indicated by prevalence ratios greater than 1.00.
| Diagnosis | PR | 95% CI |
|---|---|---|
| Contusion of eyeball | 10.37 | (2.16, 49.86) |
| Benign intracranial hypertension | 5.92 | (1.09, 32.32) |
| Toxic exposure | 2.33 | (1.34, 4.06) |
| Laceration of eyelid | 2.80 | (1.45, 5.42) |
| Amaurosis fugax | 2.09 | (1.01,4.37) |
| Retinal vascular occlusion | 1.95 | (1.15, 3.28) |
| Vitreous degeneration | 1.79 | (1.45, 2.21) |
| Retinal detachments | 1.41 | (1.07,1.87) |
| Foreign body | 1.40 | (1.13, 1.73) |
Table 4.
Prevalence Ratios of Diagnostic Groups. Diagnostic groups that are less prevalent in 2020 compared to prior years, as indicated by prevalence ratios less than 1.00.
| Diagnosis | PR | 95% CI |
|---|---|---|
| Contact lens related disorder (excluding keratitis) | 0.27 | (0.11, 0.68) |
| Eyelid disorder | 0.32 | (0.17, 0.59) |
| Allergic conjunctivitis | 0.38 | (0.15, 0.98) |
| Vitreous opacities | 0.55 | (0.34, 0.88) |
We did not find any obvious trend in the visual acuity (VA) of the patients who presented to the ED during the study period. The distribution of visual acuity measurements remained fairly consistent over the years. 8%, 10%, and 9% of patients had best corrected visual acuity (BCVA) measurement greater than or equal to 1.9 on the logMAR scale, corresponding to BCVA worse than “Counting Fingers.”17 The median BCVA was 0.12 for all three years. Per documentation, 29%, 32%, and 31% of patients did not show any improvement with pinhole in 2018, 2019, and 2020, respectively. For patients who did show improvement in VA with pinhole, the mean improvement values were 0.22, 0.22, and 0.24 in 2018, 2019, and 2020, respectively.
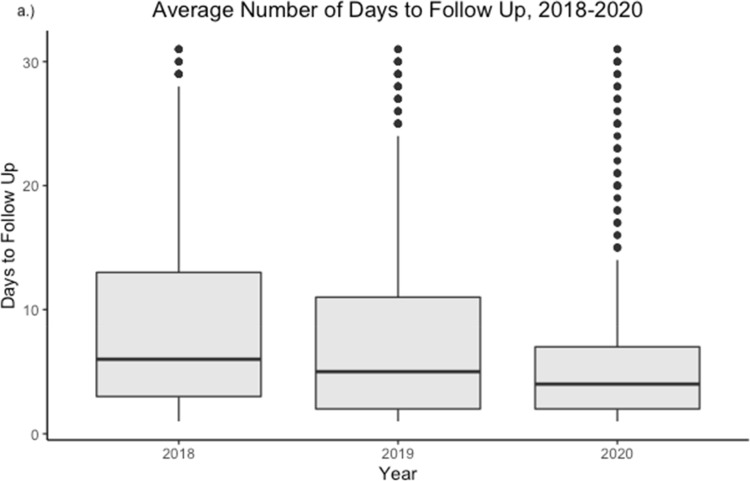
Looking at patients who had a follow up clinic visit within 31 days of their ED visit, the average time to follow up in 2020 was 6.09 days (Figure 3). The average time to follow up was 2.52 days (p < 0.001, 95% CI: 1.63–3.42) shorter in 2020 compared to 2018 and 1.68 days (p < 0.001, 95% CI: 0.8–2.55) shorter in 2020 compared to 2019.
Figure 3.
Days to follow up for patients who received follow up care < 31 days since their ED visit in 2018, 2019, and 2020.
Discussion
Overall, the volume of ED visits fell by 32% in 2020. We found that the proportion of patients seeking urgent care in 2020 was higher than that of 2018 and 2019. Particularly, we saw a rise in the proportion of diagnoses considered urgent in 2020 by 9%. Additionally, the proportion of patients who required urgent surgery increased by 39%, further reinforcing the idea that patients on average presented with more urgent concerns. However, the breakdown of indications for surgery remained unchanged, suggesting that patients who required urgent surgeries continued to present to the hospital despite the pandemic. The average number of days to follow up was shorter in 2020 compared to 2018 and 2019, which could be attributed to more ED visits requiring close follow up or greater follow up clinic availability given the cancellation of most nonurgent and nonemergent visits in clinics during COVID.
The average age of patients presenting to the ED was statistically significantly older in 2020 by roughly 1 year compared to prior years, which may indicate that fewer young patients were presenting to the ED during the pandemic. There was no change in the gender of patients. There was a statistically significant decrease in the proportion of patients who identified as Asian in 2020 compared to prior years. This may be attributed to a relative decline in the number of eye problems in the Asian community, increased avoidance of the health system by Asian patients during the pandemic, or lack of Asian patients presenting specifically to the ophthalmic emergency room. However, further studies that examine whether there exists any cultural or racial response to the pandemic are necessary to better understand this observation.
These shifts can likely be attributed to social guidelines that advised people to stay home and the fear of exposure to COVID-19, resulting in a higher threshold to visit the emergency room.20 Additionally, there is growing evidence and publicity around the fact that the ocular surface, which harbors ACE2 receptors, is a potential site of entry of viral pathogens and thus can increase possibility of infection upon exposure. This possibility may also have discouraged patients from seeking eye care.21 Further, MEE ED is located adjacent to the Massachusetts General Hospital (MGH) ED, so it is possible that patients perceived a higher degree of risk due to this geographic proximity to an epicenter of COVID-19 treatment in Boston or fear of infection while taking public transport to the ED. At the same time, in the wake of the COVID-19 pandemic, many ophthalmology clinics have changed their practice to reduce the risk of exposure by adopting telemedicine for many routine visits, while trying to develop more home-based testing or hybrid approaches.22–25 Limited outpatient clinic availability for nonurgent visits could have also led some patients to seek care in the ED instead, partially accounting for the nonurgent ED visits during the study period of 2020.
Though many eye conditions are not immediately life threatening or vision threatening, many disease processes can benefit from early intervention. Further, ocular manifestations are often the first manifestations of systemic diseases, which can include COVID-19.26,27 Thus, it is important to understand the burden of COVID-19 on timely ophthalmic care, as delay in care may lead to worse visual outcomes or health outcomes. This study underscores the impact of public health measures related to COVID-19 on ophthalmic care. COVID-19 is challenging the existing paradigms of healthcare in the United States, and this study shows decreased emergency department utilization during this public health crisis.28 Although beyond the scope of this specific study, future studies could examine the negative effect of missed clinic visits and delayed interventions on visual outcomes.
There are limitations to the present study. First, we did not exclude frequent ED users from our study. It is possible that some of the patients had repeated visits to emergency rooms for the same complaint or a very low threshold to visit an ED.29 This group of patients may have overestimated the proportion of nonurgent diagnoses or the total volume of ED visits. However, given that our access to health records was limited to those in our own system, it would have been difficult for us to gauge whether a patient may have utilized an emergency department outside of our own. Therefore, we decided against making frequency of ED use an exclusion criteria. Second, in light of COVID-19, MEE instituted changes in its follow up policies during the pandemic to ensure most patients that needed a follow-up appointment left the ED with one in hand. As a result, it is possible that the discrepancy in time to follow up in 2020 compared to prior years when patients were receiving post-visit calls from the subspecialty services could be partially attributed to this change in policy. Third, we did not account for inclement weather or other possible causes of daily fluctuation. However, winter in Boston is fairly consistent year to year, so there is no reason to believe that inclement weather conditions would have affected year-to-year comparisons. Lastly, our data may not be generalizable to all-purpose emergency departments worldwide. Massachusetts Eye and Ear is one of only four 24-hour ophthalmology-specific EDs in the United States. As previous studies have suggested, utilization of general EDs for eye-related emergencies may be perceived differently compared to patients’ perspectives while seeking care in an ophthalmology-specific ED.30,31 Further, there is growing evidence that different parts of the world are affected differently due to both socioeconomic factors and genetic factors.32 This means that different parts of the world will respond differently to the pandemic and that patterns identified in this study may not apply to all countries around the world.
Conclusions
As the wider public is adjusting to the “new normal,” the trends identified in this study carry an important message for ophthalmologists. There may be ophthalmic diagnoses—both urgent and nonurgent—that were missed because patients were more reluctant to seek care. While there may be no immediate consequences, ophthalmologists need to be more vigilant about missed diagnoses as patients begin to return to clinics. Further, both the general public and healthcare workers need clearer guidance and information on balancing the risks of delayed care and the risks of exposure to COVID-19.
Acknowledgments
The authors are grateful for the support from Fran McDonald and Anne Murphy in the Massachusetts Eye and Ear Department of Information Technology.
Funding Statement
There was no funding for this project.
Ethics Approval
Institutional review board approval was obtained from Partners Healthcare for the Protection of Human Subjects. The authors certify that this work is HIPAA compliant and adhered to the tenets of the Declaration of Helsinki.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
John B Miller reports personal fees from Alcon outside the submitted work. The authors report no other potential conflicts of interest for this work.
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Coronavirus Disease. (COVID-19) Dashboard [Internet]. World Health Organization; 2020. [cited October20, 2020]. Available from: https://covid19.who.int. [Google Scholar]
- 3.Social Distancing [Internet]. Center for Disease Control and Prevention; 2020. [Cited July15, 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/. [Google Scholar]
- 4.Interim Guidance for Coronavirus Disease 2019 (COVID-19) [Internet]. Center for Disease Control; 2020. [Cited July15, 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/large-events/mass-gatherings-ready-for-covid-19.html. [Google Scholar]
- 5.COVID-19 Updates and Information [Internet]. Massachusetts Department of Public Health; 2020. [Cited June24, 2020]. Available from: https://www.mass.gov/info-details/covid-19-updates-and-information#regulations-&-guidance-. [Google Scholar]
- 6.Recommendations for urgent and nonurgent patient care [Internet]. American Academy of Ophthalmology; 2020. [Cited May11, 2020]. Available from: https://www.aao.org/headline/new-recommendations-urgent-nonurgent-patient-care. [Google Scholar]
- 7.Napoli PE, Nioi M, d’Aloja E, Fossarello M. Safety recommendations and medical liability in ocular surgery during the COVID-19 pandemic: an unsolved dilemma. J Clin Med. 2020;9(5):1403. doi: 10.3390/jcm9051403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet. 4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones D, Neal RD, Duffy SRG, Scott SE, Whitaker KL, Brain K. Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: the view from primary care. Lancet. 2020;21(6):748–750. doi: 10.1016/S1470-2045(20)30242-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic.BMJ 75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong L, Hawkins J, Langness S, Murrell K, Iris P, Sammann A. Where are all the patients? Addressing covid-19 fear to encourage sick patients to seek emergency care. N Engl J Med. 2020. [Google Scholar]
- 12.Hartnett K, Kite-Powell A, DeVies J, Gundlapalli A. Impact of the COVID-19 pandemic on emergency department visits — United States, January1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pellegrini M, Roda M, Lupardi E, Di Geronimo N, Giannaccare G, Schiavi C. The impact of COVID-19 pandemic on ophthalmological emergency department visits. Acta Ophthalmol. 2020. doi: 10.1111/aos.14489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu S, Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395(10233):1321–1322. doi: 10.1016/S0140-6736(20)30845-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.COVID-19 Response Reporting [Internet]. Commonwealth of Massachusetts; 2020. [Cited October24, 2020]. Available from: https://www.mass.gov/info-details/covid-19-response-reporting. [Google Scholar]
- 16.Hall L, Jeng-Miller K, Gardiner M, Lee E.Utilization trends of an ophthalmology-specific emergency department: the Massachusetts eye and ear experience.Digit J Ophthalmol.2020Available from: http://www.djo.harvard.edu/site.php?url=/physicians/oa/3932#OA_RS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bailey IL, Lovie-Kitchin JE. Visual acuity testing. From the laboratory to the clinic. Vision Res. 2013;90:2–9. doi: 10.1016/j.visres.2013.05.004 [DOI] [PubMed] [Google Scholar]
- 18.Team RC R: A Language and Environment for Statistical Computing; 2020. Available from: https://www.R-project.org. Accessed November 13, 2020.
- 19.Wickham H. Ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag; 2016; Available from: https://ggplot2.tidyverse.org. Accessed November 13, 2020. [Google Scholar]
- 20.Harper CA, Satchell LP, Fido D, Latzman RD. Functional fear predicts public health compliance in the COVID-19 pandemic. Int J Ment Health Addict. 2020;1–14. doi: 10.1007/s11469-020-00281-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Napoli PE, Nioi M, d’Aloja E, Fossarello M. The ocular surface and the coronavirus disease 2019: does a Dual “ocular route” exist? J Clin Med. 2020;9(5):1269. doi: 10.3390/jcm9051269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Olivia Li J-P, Shantha J, Wong TY, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. 2020;127(5):569–572. doi: 10.1016/j.ophtha.2020.03.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lu E, Houston S, Rahimy E, Miller JB. Telehealth implementation in retina practices during COVID-19. Retina. 2020. Available from: http://retinatoday.com/2020/06/telehealth-implementation-in-retina-practices-during-covid-19/. [Google Scholar]
- 24.Miller JB, Zeng R. The future of home-based OCT for retina patients. Retina. 2019. Available from: http://retinatoday.com/2019/12/the-future-of-home-based-oct-for-retina-patients [Google Scholar]
- 25.Bowe T, Hunter DG, Mantagos IS, et al. Virtual visits in ophthalmology: timely advice for implementation during the COVID-19 public health crisis. Telemed E Health. 2020;26(9):1113–1117. doi: 10.1089/tmj.2020.0121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Klig J. `Ophthalmologic complications of systemic disease. Emerg Med Clin North `Am. 2008;26(1):217–231. doi: 10.1016/j.emc.2007.10.003 [DOI] [PubMed] [Google Scholar]
- 27.Xia J, Tong J, Liu M, Shen Y, Guo D.Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection.J Med Virol.doi: 10.1002/jmv.25725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keesara S, Jonas A, Schulman K. Covid-19 and health care’s digital revolution. N Engl J Med. 2020;382(23):82. doi: 10.1056/NEJMp2005835 [DOI] [PubMed] [Google Scholar]
- 29.Okuyemi KS, Frey B. Describing and predicting frequent users of an emergency department. J Assoc Acad Minor Phys. 2001;12(1–2):119–123. [PubMed] [Google Scholar]
- 30.Vaziri K, Schwartz SG, Flynn HW, Kishor KS, Moshfeghi AA. Eye-related emergency department visits in the United States, 2010. Ophthalmology. 2016;123(4):917–919. doi: 10.1016/j.ophtha.2015.10.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134(3):312. doi: 10.1001/jamaophthalmol.2015.5778 [DOI] [PubMed] [Google Scholar]
- 32.Napoli PE, Nioi M. Global spread of coronavirus disease 2019 and malaria: an epidemiological paradox in the early stage of a pandemic. J Clin Med. 2020;9(4):1138. doi: 10.3390/jcm9041138 [DOI] [PMC free article] [PubMed] [Google Scholar]