Abstract
Background
Vaccinations are an effective choice to stop disease outbreaks, including COVID-19. There is little research on individuals' COVID-19 vaccination decision-making.
Objective
We aimed to determine individual preferences for COVID-19 vaccinations in China, and to assess the factors influencing vaccination decision-making to facilitate vaccination coverage.
Methods
A D-efficient discrete choice experiment was conducted across six Chinese provinces selected by the stratified random sampling method. Vaccine choice sets were constructed using seven attributes: vaccine effectiveness, side-effects, accessibility, number of doses, vaccination sites, duration of vaccine protection, and proportion of acquaintances vaccinated. Conditional logit and latent class models were used to identify preferences.
Results
Although all seven attributes were proved to significantly influence respondents’ vaccination decision, vaccine effectiveness, side-effects and proportion of acquaintances vaccinated were the most important. We also found a higher probability of vaccinating when the vaccine was more effective; risks of serious side effects were small; vaccinations were free and voluntary; the fewer the number of doses; the longer the protection duration; and the higher the proportion of acquaintances vaccinated. Higher local vaccine coverage created altruistic herd incentives to vaccinate rather than free-rider problems. The predicted vaccination uptake of the optimal vaccination scenario in our study was 84.77%. Preference heterogeneity was substantial. Individuals who were older, had a lower education level, lower income, higher trust in the vaccine and higher perceived risk of infection, displayed a higher probability to vaccinate.
Conclusions
Preference heterogeneity among individuals should lead health authorities to address the diversity of expectations about COVID-19 vaccinations. To maximize COVID-19 vaccine uptake, health authorities should promote vaccine effectiveness; pro-actively communicate the absence or presence of vaccine side effects; and ensure rapid and wide media communication about local vaccine coverage.
Keywords: COVID-19, Preference, Vaccine, Health policy
1. Introduction
By the end of July 2020, COVID-19 had infected more than 16 million people across 216 countries or territories, with more than 65,000 deaths worldwide [1]. During the pandemic, there have been no specific antiviral drugs to treat COVID-19 effectively, but existing drugs used to treat other viral diseases, such as dexamethasone, have improved the recovery of high-risk COVID-19 patients. A vaccine is seen as the effective choice to stop the pandemic, with more than 100 COVID-19 vaccines in development worldwide [2], including seven that have now been approved for human testing through clinical trials. Three vaccines are awaiting regulatory approval in the U.S. and U.K, and China and Russia are at an advanced stage of COVID-19 vaccine approval. With the hope that a COVID-19 vaccine will be approved in the near future, it is vital to understand individuals’ vaccination preferences and vaccination decision-making in order to predict vaccination coverage, to assess the factors influencing vaccination decision-making, and to improve COVID-19 vaccination coverage. There is little research on individuals’ COVID-19 vaccination decision-making. To addresses this lacuna, we test an individual choice COVID-19 vaccination model across six provinces in China.
Previous research using health belief models found that only 48.2% of Chilean population reported a definite intent to receive the COVID-19 vaccine, 46.1% with a probable intent or a possible intent [3]. Research suggests that the novelty of the disease may lead to individuals indicating reluctance to get vaccinated [4]. Previous studies of vaccine uptake identified various vaccine-specific factors that influence an individual’s vaccination preferences, such as the vaccine’s side effects, effectiveness, duration of protection, cost, number of doses, transmission route, location of vaccination sites, willingness to pay and the burden of the disease [3], [4], [5], [6], [7], [8], [9], [10], [11]. There is no agreement on the importance of these vaccine-specific aspects on the willingness to vaccinate. Also, there is no consensus on whether vaccine-led herd immunity leads to higher vaccine acceptance through altruistic motives [10], [12] or hinders individual vaccinations through the free-rider problem [13]. Further, inter-individual vaccination preference heterogeneity may impact vaccine uptake depending on individuals’ socio-demographic characteristics, such as age, education [10] and income [11], [12]. Also, trust in the vaccine and social trust may be important factors in individual heterogeneity, because they influence people’s decision to vaccinate, especially given that many vaccines have a reputation for poor quality, leading to a drop in vaccine coverage [14], [15].
Widely employed in studies of the hepatitis B virus (HBV) [7], [9], seasonal influenza [10] and human papillomavirus vaccines [11], we used the discrete choice experiment (DCE) method to reveal and measure preferences for a potential COVID-19 vaccine. The conditional logit model (CLM) was used to test whether respondents' predefined characteristics alter the mean preference associated with attribute values. In addition, the latent class model (LCM) was used to estimate inter-individual preference heterogeneity. Our study is one of the first attempts to determine the preferences of individuals in China for a COVID-19 vaccine. While a China-based study, the research will inform other countries on individual COVID-19 decision-making, facilitating vaccination coverage in line with China and World Health Organization goals.
2. Methods
2.1. Identification of attributes and levels
Identification of vaccine attributes and their levels is key for ensuring the validity of DCE. We retrieved relevant vaccine attributes and levels from the literature [3], [4], [5], [6], [7], [10], [16]. Attributes were then ranked, categorized and reduced through interviews with a group of eight experts in the field of vaccination, an eight person focus group discussion and a 30 survey pilot study. We identified seven key attributes and adopted a DCE design with 8 choice sets of two vaccine profiles.
The details of the attributes and levels are displayed in Table 1 . Vaccine effectiveness refer to the proportion of vaccinated persons protected by the vaccine, with three levels (40%, 60% and 85%), based on the effectiveness of seasonal influenza vaccinations [17], [18] and high effectiveness of H1N1 vaccination [19]. Side effects were assigned three levels: 50/100,000, 10/100,000 and 1/100,000. These levels were chosen to represent vaccines with moderate side effects, such as seasonal influenza vaccines [17], [18] and low side effects, such as H1N1 vaccine [20]. Access to the vaccine was specified as free and voluntary (reflecting H1N1 vaccination), free and compulsory (reflecting most current universal childhood vaccinations) and chargeable and voluntary (reflecting some partial or non-reimbursed seasonal influenza vaccines). Number of doses was described by two levels: one dose and two or more doses. Vaccination sites were described by three possible levels: village clinic or community health station, township or community health centre, and county hospital and above. The duration of vaccine protection was assigned three levels: 6 months, 1 year and two or more years. These duration levels were retrieved based on the duration of vaccine protection of seasonal influenza vaccinations [17], [18], H1N1 vaccination [19] and hepatitis B vaccine [9]. Acquaintances vaccinated was assigned 30%, 60% and 90% of close acquaintances (friends and family) already being vaccinated. This attribute was to quantify the importance of local coverage as a main driver for vaccination choices [10].
Table 1.
Attributes and Levels Used in the Discrete Choice Experiment.
| Attributes | Levels | Descriptions |
|---|---|---|
| Vaccine effectiveness | 40% | Protects 40% of vaccinated |
| 60% | Protects 60% of vaccinated | |
| 85% | Protects 85% of vaccinated | |
| Vaccine related side-effects | 50/100,000 | 50 out of 100,000 risk of severe side effect |
| 10/100,000 | 10 out of 100,000 risk of severe side effect | |
| 1/100,000 | 1 out of 100,000 risk of severe side effect | |
| Access to vaccine | Free and voluntary | Vaccine is free and it is voluntary to get vaccinated. |
| Free and compulsory | Vaccine is free and it is compulsory to get vaccinated | |
| Chargeable and voluntary | You must pay for vaccine yourself, but vaccination is voluntary. | |
| Number of doses | One dose | One dose |
| ≥2 doses | Two or more doses | |
| Vaccination sites | First level | Village clinic or community health station |
| Second level | Township or community health centre | |
| Third level | County hospital and above | |
| Duration of vaccine protection | Six months | Six months of vaccine protection |
| One year | One year of vaccine protection | |
| More than two years | More than two years | |
| Acquaintances vaccinated | 30% | 30% of your family, friends and acquaintances already vaccinated |
| 60% | 60% of your family, friends and acquaintances already vaccinated | |
| 90% | 90% of your family, friends and acquaintances already vaccinated | |
2.2. Experimental design
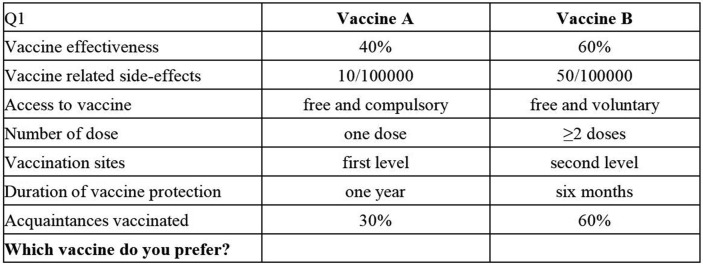
To guarantee that preference parameters can be estimated with maximal precision, the D-efficient partial profile design was used. Forty-eight hypothetical two-alternative choice tasks were created in STATA 15.0. For each choice task, respondents were asked to choose which vaccine they would prefer. To reduce the cognitive burden on respondents, these 48 choice tasks were divided randomly into 6 different versions of the questionnaire. As shown in the examples in Fig. 1 , each version included 8 choice tasks.
Fig. 1.
Example of choice sets.
2.3. Survey
A three-part questionnaire sought information on respondents’ background characteristics, attitudes to COVID-19 and the COVID-19 vaccine, and DCE preferences. Background characteristics comprised sex, age, location, educational attainment, job status, and income. Using a five-point Likert scale, attitudes to COVID-19 were surveyed by two questions and attitudes to the COVID-19 vaccine were surveyed by six questions as show in Appendix 1 Supplemental Material. Vaccine and COVID-19 related attitudes were tested as covariates with the DCE estimates to examine preference heterogeneity.
A pilot survey was conducted with 30 respondents. Based on the pilot, the survey was subsequently revised to improve phraseology and question layout. Also, the pilot allowed the survey to be adjusted to ease the cognitive load and to increase the quality of the responses, with 48 pairs of scenarios in the questionnaires divided into 6 questionnaires with 8 pairs of scenarios in each. To promote survey accuracy, our DCE started with a general description and an illustrative example of a simplified choice set to familiarize the respondents with the choice tasks ahead. The study was approved by Nanjing Medical University Ethics Committee (No. 2020565) and the face-to-face survey conducted by trained researchers.
Using a stratified random sampling method, six Chinese provinces were chosen based on high, medium and low GDP per capita, geographically covering east, central and west regions of China. In each province, three cities were chosen, also divided into high, medium and low GDP per capita, with 314 individuals randomly surveyed in each city.
2.4. Sample
The inclusion criteria were respondents aged over 18 years old, without cognitive impairments. According to the research standard proposed by Orme [21], the minimum sample size should be 94, with de Bekker-Grop et al. reporting from a DCE literature survey that only 9% of DCE sample sizes were greater than 10,000 [22]. Our study collected 1888 questionnaires, with 1883 (99.7%) of respondents answering all choices. The six versions of the questionnaires were evenly distributed, with version 1 accounting for 17.21%, version 2, 16.46%, version 3, 17.05%, version 4, 16.09%, version 5, 15.93% and version 6, 17.26% of all surveys. In total, 30,128 observations comprised the database.
2.5. Data analysis
Following previous research [23], all the variables describing attribute levels were introduced as dummy variables. The quality of the various discrete choice models was compared on the basis of the Bayesian information criteria (BIC) and Akaike information criteria (AIC) [24]. The preferences were estimated with two models, the conditional logit model (CLM) and latent class model (LCM). The CLM is commonly used to analyze preferences, with individual utility estimated by Eq. (1):
| (1) |
where Uijs is the utility of respondent i for scenario j in the choice set s (here j = 1, 2; s = 1,..,8), β is a parameter vector relating attribute values and utility levels and εijs is error of utility.
CLM assumes errors are independent and identically distributed, which limits the analysis of response heterogeneity and neglects preference heterogeneity. Not conforming to CLM model assumptions, LCM addresses these problems by classifying individuals into mutually exclusive groups, which display heterogeneous preferences, according to differences in share values, characteristics and behavior. The AIC and BIC criteria were used to determine the optimal number of classes [25]. The optimal utility function was:
| (2) |
where Uijs | c represents the utility of respondent i belonging to class segment c for scenario j in choice sets.
In addition to the utility function, the final model allowed for several covariates (age, education, region, income, trust in vaccines, and risk of infection) to enter into the class assignment model. The class assignment utility function for the final model was:
| (3) |
Policy analysis was conducted by calculating the probability of vaccine uptake. Utility scores were used as probabilities and attribute levels were predefined. Probabilities of vaccine uptake were calculated on the basis of an indirect utility analysis, using Eq. (1), whereby individual (n) will choose vaccine within a choice set of 1 out of j sets (j = 1, … j) of options.
| (4) |
3. Results
3.1. Respondent characteristics
Table 2 presents the respondents’ characteristics. Of the 1883 respondents, 50.98% were female and 60.33% live in urban areas, which was consistent with the current national population distribution making the sample broadly nationally representative. Key characteristics include 61.23% in the 18–44 age group; 59.27% were married; about 70% had a high school (9 < years of schooling ≤ 12 years) or higher education; 71% were employed or farmers; and almost 45% were in the lowest income category. The sample was evenly distributed across the three regions.
Table 2.
Characteristics of the study sample (n = 1883).
| Characteristics | n | % |
|---|---|---|
| Gender | ||
| Male | 923 | 49.02 |
| Female | 960 | 50.98 |
| Age | ||
| Age 18–44 | 1153 | 61.23 |
| Age 45–59 | 545 | 28.94 |
| Age 60– | 185 | 9.82 |
| Marital status | ||
| Unmarried | 688 | 36.54 |
| Married | 1116 | 59.27 |
| Widowed/divorced | 79 | 4.20 |
| Residence | ||
| Urban area | 1136 | 60.33 |
| Rural area | 747 | 39.67 |
| Education | ||
| Low education (years of schooling ≤9 years) | 576 | 30.59 |
| Medium education (9 <years of schooling ≤12 years) | 809 | 42.96 |
| High education (years of schooling >12 years) | 498 | 26.45 |
| Occupation | ||
| Farmer | 395 | 20.98 |
| Employed | 957 | 50.82 |
| Other (including students and retired) | 531 | 28.20 |
| Household yearly income | ||
| <4500RMB | 847 | 44.98 |
| 4500–9000RMB | 579 | 30.75 |
| >9000RMB | 457 | 24.27 |
| Region | ||
| East | 634 | 33.67 |
| Central | 624 | 33.14 |
| West | 625 | 33.19 |
3.2. Attitudes to vaccine and COVID-19
In general, trust in the vaccine and the vaccination process was ranked as high importance, with 81.9% agreeing or strongly agreeing that the vaccine was safe and 90% of respondents agreeing or strongly agreeing that vaccinating was very important. The perceived COVID-19 risk was not high: only 24.8% agreed or strongly agreed that they and their friends and relatives were at risk of COVID-19 and 14.5% of respondents agreed or strongly agreed that someone in their community will have COVID-19 (See Appendix 1 in Supplemental Materials).
3.3. Estimation of preferences and their heterogeneity
Table 3 presents the results of the conditional logit model. All attributes were shown to be significant (p < 0.01), except for “free and compulsory” and “second level” (township or community health center) vaccination sites. Vaccine effectiveness and side-effects were the most important attributes, followed by duration of vaccine protection, proportion of acquaintances vaccinated and access to the vaccine. Number of doses and vaccination sites were the least significant attributes. Our result show that there was a higher probability for vaccination take-up when the vaccine was more effective, had small risk of serious side-effects, was free and voluntary, required fewer doses, had a longer protection duration, and the higher the proportion of acquaintances who vaccinated. The positive correlation between vaccine utility and the proportion of acquaintances vaccinated demonstrated the peer influence and altruistic motives on herd immunity. The vaccination sites showed a significant direct linear relationship with vaccine utility, with a low trust in primary health care and high preference for municipal and above hospitals as vaccination sites.
Table 3.
Conditional logit model of respondent preferences (n = 1883).
| Attribute | ß | SEa | 95% CI |
|---|---|---|---|
| Vaccine effectiveness (reference = 40%) | |||
| 60% | 0.389*** | 0.026 | 0.338, 0.440 |
| 85% | 0.994*** | 0.027 | 0.941, 1.047 |
| Vaccine related side-effects (reference = 50/100,000) | |||
| 10/100,000 | 0.469*** | 0.026 | 0.418, 0.520 |
| 1/100,000 | 0.932*** | 0.027 | 0.879, 0.985 |
| Access to vaccine (reference = free and voluntary) | |||
| Free and compulsory | 0.025 | 0.026 | −0.025, 0.075 |
| Chargeable and voluntary | −0.279*** | 0.026 | −0.330, −0.228 |
| Number of doses (reference = one dose) | |||
| ≥2 doses | −0.057*** | 0.018 | −0.093, −0.022 |
| Vaccination sites (reference = first level) | |||
| Second level | −0.030 | 0.027 | −0.082, 0.022 |
| Third level | 0.073*** | 0.026 | 0.023, 0.124 |
| Duration of vaccine protection (reference = six months) | |||
| One year | 0.152*** | 0.025 | 0.102, 0.202 |
| More than two years | 0.257*** | 0.026 | 0.206, 0.309 |
| Acquaintances vaccinated (reference = 30%) | |||
| 60% | 0.155*** | 0.026 | 0.104, 0.206 |
| 90% | 0.257*** | 0.026 | 0.206, 0.307 |
| Model fit | |||
| Observations = 30128 | Prob > chi2 = 0.000 | ||
| Respondents = 1883 | LR chi2 (13) = 3064.46 | ||
| AIC | 17017.97 | ||
| BIC | 17234.11 | ||
SE standard errors.
Statistically significant at 0.01%
To estimate preference heterogeneity, latent class models were estimated. We selected the three-class model with six socio-demographic covariates based on AIC and BIC comparisons across two-class, three-class or four-class models, including socio-demographic covariates that can improved the model fit [26], model simplicity and interpretability of class membership. Table 4 shows clearly the different preference heterogeneity among the three classes, and the class probabilities indicated that 54.8% of respondents were assigned to class 1, 23.2% to class 2, and 21.9% to class 3. For class 1, respondents had identical preferences to the mean preferences of the whole sample, with the coefficients and their significance of attribute levels similar to those estimated by the CLM. Vaccine effectiveness, proportion of acquaintances vaccinated, side-effects and duration of vaccine protection were also important attributes in the LCM, although their rankings differ from the CLM. Access to vaccine and vaccination sites were less important than the other attributes, and the number of doses were no longer significant.
Table 4.
Latent class logit model of respondent preferences (n = 1883).
| Attribute | Class 1 |
Class 2 |
Class 3 |
|||
|---|---|---|---|---|---|---|
| ß | SEa | ß | SE | ß | SE | |
| Vaccine effectiveness | ||||||
| 60% | 0.202*** | 0.042 | 0.736*** | 0.212 | 2.366*** | 0.231 |
| 85% | 0.505*** | 0.049 | 1.806*** | 0.167 | 4.435*** | 0.338 |
| Vaccine related side-effects | ||||||
| 10/100,000 | 0.170*** | 0.039 | 3.134*** | 0.105 | 0.790*** | 0.168 |
| 1/100,000 | 0.366*** | 0.043 | 6.510*** | 0.532 | 0.935*** | 0.204 |
| Access to vaccine | ||||||
| Free and compulsory | 0.043 | 0.037 | −1.007*** | 0.190 | 0.434** | 0.180 |
| Chargeable and voluntary | 0.000*** | 0.039 | −2.017*** | 0.164 | 0.145 | 0.176 |
| Number of doses | ||||||
| ≥2 doses | −0.037 | 0.027 | −0.902*** | 0.108 | 0.218* | 0.115 |
| Vaccination sites | ||||||
| Second level | −0.072** | 0.037 | 0.493** | 0.203 | 0.114 | 0.180 |
| Third level | 0.025 | 0.036 | 0.844*** | 0.163 | 0.173 | 0.163 |
| Duration of vaccine protection | ||||||
| One year | 0.187*** | 0.037 | −0.412*** | 0.149 | 0.102 | 0.151 |
| More than two years | 0.309*** | 0.036 | 0.151 | 0.215 | 0.606*** | 0.196 |
| Acquaintances vaccinated | ||||||
| 60% | 0.221*** | 0.036 | 0.798*** | 0.188 | −0.161 | 0.180 |
| 90% | 0.405*** | 0.037 | 0.522*** | 0.168 | −0.006 | 0.163 |
| Class probability model | ||||||
| Age | 0.467*** | 0.119 | 0.350** | 0.135 | – | – |
| Education | −0.257*** | 0.093 | 0.109 | 0.105 | – | – |
| Region | 0.183** | 0.090 | 0.083 | 0.098 | – | – |
| Average monthly household income | −0.375*** | 0.086 | −0.109 | 0.094 | – | – |
| Trust in vaccines | −0.156 | 0.104 | −0.558*** | 0.125 | – | – |
| Risk of infection | −0.094 | 0.088 | −0.228** | 0.103 | – | – |
| Constant | 1.707*** | 0.353 | 0.242 | 0.485 | – | – |
| Class probability | ||||||
| Average | 0.548 | 0.232 | 0.219 | |||
| Model fit | ||||||
| Observations = 30128 | ||||||
| Respondents = 1883 | ||||||
| AIC | 16334.25 | |||||
| BIC | 16766.54 | |||||
SE standard errors.
Statistically significant at the 1%.
At 5%.
At 10% level.
For LCM class 2, respondents had some different preferences from those estimated by the CLM and LCM class 1. The significant difference was that side-effects was the attribute whose level made utility vary most, followed by access to the vaccine. All attributes, including number of doses, were significant, except for the “two years level of duration of vaccine protection”. Respondents in LCM class 3 showed large differences in preferences compared to those estimated by the LCM class 1 and class 2. Vaccine effectiveness had the highest importance, which was higher than the side-effect attribute, and “free and compulsory”, number of doses and “two years” levels were significant in LCM class 3.
Estimating the probability of belonging to any class based on four individual socio-demographic characteristics, risk perception and vaccine trust, we found they were significantly associated with the membership of preference classes, including age, education, region, average monthly household income, trust in vaccines and risk of infection. Older age respondents had a higher probability of preferring COVID-19 vaccinations. For LCM class 1, respondents with lower education levels and lower income levels had a higher probability of preferring the COVID-19 vaccination compared with those with higher education level and higher income level. Compared with those in east region, respondents in central and west region had a higher probability of preferring the COVID-19 vaccination. For LCM class 2, individuals who had a higher trust in vaccines and a higher perceived risk of COVID-19 infection, displayed a higher probability to prefer the COVID-19 vaccination.
3.4. Probability of take-up
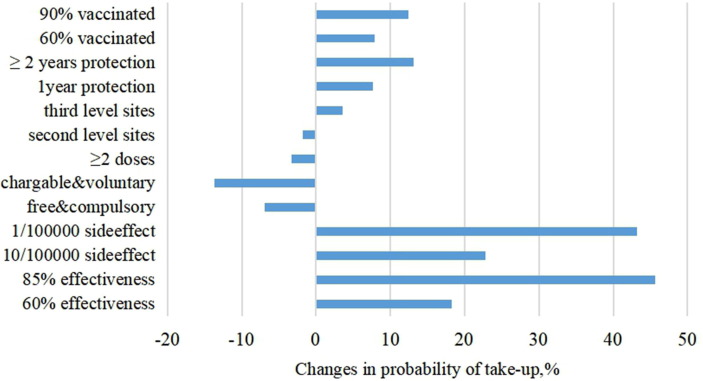
Vaccine uptake probabilities were calculated on the basis of an indirect utility analysis, using CLM. Fig. 2 presents the vaccine uptake probabilities. As a comparative standard, we defined a base vaccination program: 40% vaccine effectiveness, 50/100,000 risk of severe side-effects, free and voluntary vaccinations, one dose, village clinic or community health station, protection duration of 6 months and 60% of acquaintances vaccinated. The base case is indicated as zero change in the probability on the X-axis in Fig. 2. When the vaccine effectiveness increased from 40% to 85%, the vaccination uptake increased 45.68% and when the risk of severe side effects fell from 50/1,000,000 to 1/1,000,000, the vaccination uptake increased 43.18%. The vaccination uptake rate increased 12.38% when the proportion of acquaintances vaccinated increased from 30% to 90%.
Fig. 2.
Changes in probability of individual take-up.
Taking the base vaccination program, the predicted vaccination uptake was 45.82%. The predicted vaccination uptake of the worst vaccination scenario, (vaccine effectiveness of 40%, 50/100,000 risk of severe side-effects, chargeable and voluntary to get vaccinated, two dose, vaccination sites of first level, protection duration of 6 months and acquaintances vaccinated of 30%) was still 23.53%. The predicted vaccination uptake of the optimal vaccination scenario (vaccine effectiveness of 85%, 1/100,000 risk of severe side-effects, free and voluntary vaccinations, one dose, third level vaccination sites, protection duration of 2 years and 90% of acquaintances vaccinated) was 84.77%.
4. Discussion
To our knowledge, this is the first study to estimate individual preferences for a COVID-19 vaccine using a DCE for a nationally representative population in China. Vaccine effectiveness, side-effects, proportion of acquaintances vaccinated, vaccine protection, number of doses, access to vaccine and vaccination sites were attributes significantly influencing the preferences for COVID-19 vaccinations. Older age individuals, those with a lower education level, lower income, higher trust in vaccines and high perceived risk of infection had a higher probability to vaccinate. The predicted vaccination uptake of the optimal vaccination scenario in our study was 84.77%.
Vaccine effectiveness, side-effects, and proportion of acquaintances vaccinated were most important attributes, but their rankings differed between CLM and LCM. Consistent with Verelst et al.’s [10] flu study and Sadique et al.’s [27] study of three hypothetical vaccines, side-effects were the most important factor in the CLM and class 2 LCM. But, vaccine effectiveness was the most important attribute in the class 1 and class 3 LCM, which is consistent with Guo et al.’s [9] study on HBV vaccinations and Wong et al.’s [11] research on human papillomavirus vaccinations. We found the local vaccine coverage (or proportion of acquaintances vaccinated) was the second most important attribute in class 1 LCM (54.85% of the sample), and even more important than side-effects. This finding was different from Verelst et al.’s [10] flu study where the local vaccine coverage was less important than side-effects, accessibility and burden of disease attributes. The more acquaintances who vaccinated, the more individuals preferred to vaccinate against COVID-19. This finding suggests that herd immunity through vaccination will lead to higher levels of vaccine acceptance through altruistic motives and attenuate the free-rider motives. Rapid and wide media communication about local vaccine coverage can help to improve the vaccination coverage.
Costs were still an important factor for vaccination preferences. Compared with free vaccinations, a vaccination charge reduced the probability of vaccination. However, the effects of voluntary or compulsory vaccination are different among three classes of respondents. Under the premise of free vaccine policy, the effects of voluntary or compulsory vaccination policy needs further study. We expected that when a medical institution vaccination site was convenient, vaccinations would be more likely to be taken-up. However, our results showed the opposite. Vaccination sites showed a significant direct linear relationship with vaccine utility in the CLM and LCM class 2, which may be explained by the low trust in primary health care centers compared to more distant, but higher trust, municipal and above hospitals. Also, vaccination sites might reflect the quality of the vaccination service, with individuals in China reporting more confidence in municipal and above hospital services compared to primary-level medical and health care institutions [9]. Not surprisingly, respondents preferred fewer doses, in part because fewer visit to a vaccination site saves time and transportation costs, which was in line with Shono and Kondo [8] flu and Guo et al. [9] hepatitis B vaccinations findings. The longer the duration of protection, the more individuals prefer to vaccinate.
Respondents in our study showed preference heterogeneity for COVID-19 vaccinations. Information of preference heterogeneity and knowing the differences in personal values towards COVID-19 vaccinations will help policy makers to understand individual preferences for vaccinations, which will promote increased vaccine coverage. For example, respondents who are older, have a lower education level and reported lower incomes had a higher probability to vaccinate. This finding suggests that older, poorer and less educated individuals may overestimate the benefits from vaccinations; younger, higher educated and high income respondents may underestimate the safety of the vaccine. Therefore, pro-actively communication on side-effects and effectiveness of vaccine is critical to stimulate vaccine uptake, especially for younger, higher educated and high income respondents.
We found more than 30% of the respondents who did not want to get vaccinated were worried about the side-effects. We also found the trust in the COVID-19 vaccine and the perceived risk of COVID-19 increased COVID-19 vaccine take-up. One policy implication is that health authorities need campaigns to shape the knowledge and attitudes towards COVID-19 and the COVID-19 vaccine to address any cognitive biases and distrust in the public. Further, the evidence of altruistic take-up of the vaccine should encourage policy makers to launch widespread media communications about local vaccine coverage.
The study had some limitations. First, an opt-out option was not included in our DCE. This is consistent with the answers obtained in our pilot survey and with the design of our experiment. Second, we did not include willingness to pay (WTP) or an out-of-pocket cost attribute in our DCE. To reduce the cognitive burden of respondents, we offered only the binary “free” versus “chargeable” level for the vaccine. As a result, we cannot estimate and compare the WTP for different vaccination scenarios, which should be addressed in future studies.
In conclusion, this study provides evidence-based individual preference to policy makers in terms of quality of vaccine, vaccination accessibility, local vaccine coverage and trust in the COVID-19 vaccine. This study also verifies that inter-individual preference heterogeneity was substantial. It is critical to stimulate vaccine uptake by emphasizing vaccine effectiveness and pro-actively communicating about any side-effects and local vaccine coverage. A higher local vaccine coverage can create an altruistic incentive to vaccinate. Compared with free vaccinations, charging for the vaccine reduced for 70% of the respondents their utility of vaccinating, resulting in a lower probability of vaccinating. Under the premise of a free vaccine, the effects of voluntary or compulsory vaccination policy were different among the three classes of respondents, which requires further study. Preference heterogeneity among individuals should lead health authorities to address the diversity of expectations about COVID-19 vaccinations by providing people-oriented immunization services.
5. Contributors
AL and JW contributed towards the article by making substantial contributions to conception and design. AL contributed towards the article by collecting data and undertaking the statistical analysis, interpretation of the data, and writing the manuscript. SN, EM and RL engaged in interpreting the results and writing the paper. SW engaged in undertaking the statistical analysis and part of literature survey. All authors read and approved the final version of the manuscript.
Data sharing
The dataset supporting the conclusions of this article is available from the corresponding author on reasonable request.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 72004117), China Postdoctoral Science Foundation (grant number 2019M662392) and Qingdao Postdoctoral Foundation.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors are grateful to research students in Shandong University,Nanjing Medical University, Inner Mongolia Medical University, Ningxia Medical University, Xinxiang Medical University for their assistance in collecting data. The authors thank the editor and reviewers for suggestions that have significantly improved the paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2020.12.009.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.WHO. Coronavirus disease (COVID-19) pandemic-27 July 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [accessed July 27, 2020].
- 2.WHO. DRAFT landscape of COVID-19 candidate vaccines–30 April 2020. https://www.who.int/whodocuments-detail/draft-landscape-of-COVID-19-candidate-vaccines [accessed May 5, 2020].
- 3.García L.Y., Cerda A.A. Contingent assessment of the COVID-19 vaccine. Vaccine. 2020;38(34):5424–5429. doi: 10.1016/j.vaccine.2020.06.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chou W.Y.S., Budenz A. Considering Emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 5.Feng-Cai Z., Yu-Hua L., Xu-Hua G. Li-Hua Hou, et al., Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet. 2020;395:1845–1854. doi: 10.1016/S0140-6736(20)31208-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong L.P., Alias H., Wong P.F. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vacc Immunotherapeut. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guo N., Wang J., Nicholas S. Behavioral differences in the preference for hepatitis B virus vaccination: A discrete choice experiment. Vaccines. 2020;8(3):527. doi: 10.3390/vaccines8030527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shono A., Kondo M. Parents' preferences for seasonal influenza vaccine for their children in Japan. Vaccine. 2014;32:5071–5076. doi: 10.1016/j.vaccine.2014.07.002. [DOI] [PubMed] [Google Scholar]
- 9.Guo N., Zhang G., Zhu D. The effects of convenience and quality on the demand for vaccination: Results from a discrete choice experiment. Vaccine. 2017;35:2848–2854. doi: 10.1016/j.vaccine.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Verelst F., Willem L., Kessels R. Individual decisions to vaccinate one's child or oneself: A discrete choice experiment rejecting free-riding motives. Soc Sci Med. 2018;207:106–116. doi: 10.1016/j.socscimed.2018.04.038. [DOI] [PubMed] [Google Scholar]
- 11.Wong C., Man K., Ip P. Mothers' preferences and willingness to pay for human papillomavirus vaccination for their daughters: A discrete choice experiment in Hong Kong. Value Health. 2018;21:622–629. doi: 10.1016/j.jval.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 12.Laguzet L., Turinici G. Individual vaccination as Nash equilibrium in a SIR model with application to the 2009–2010 influenza A (H1N1) epidemic in France. B Math Biol. 2015;77:1955–1984. doi: 10.1007/s11538-015-0111-7. [DOI] [PubMed] [Google Scholar]
- 13.Vietri J.T., Li M., Galvani A.P. Vaccinating to help ourselves and others. Med Decis Mak. 2012;32:447. doi: 10.1177/0272989X11427762. [DOI] [PubMed] [Google Scholar]
- 14.Miyachi T., Takita M., Senoo Y. Lower trust in national government links to no history of vaccination. The Lancet. 2020;395:31–32. doi: 10.1016/S0140-6736(19)32686-8. [DOI] [PubMed] [Google Scholar]
- 15.Liu Z., Yang J.Z. In the wake of scandals: how media use and social trust influence risk perception and vaccination intention among Chinese parents. Health Commun. 2020;7716:1–12. doi: 10.1080/10410236.2020.1748834. [DOI] [PubMed] [Google Scholar]
- 16.Christine, Michaels-Igbokwe, Shannon Individual preferences for child and adolescent vaccine attributes: a systematic review of the stated preference literature. Patient. 2017;10:687–700. doi: 10.1007/s40271-017-0244-x. [DOI] [PubMed] [Google Scholar]
- 17.CDD Centers for disease control vaccine effectiveness – How well does the flu vaccine work? https://www.cdc.gov/flu/about/qa/vaccineeffect.htm, 2017. [accessed May 14, 2017].
- 18.Kelly H., Carville K., Grant K. Estimation of influenza vaccine effectiveness from routine surveillance data. PLoS ONE. 2009;4:e5079. doi: 10.1371/journal.pone.0005079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yu HJ. The vaccination protection rate of HIN1 vaccine exceeds 85%. Persistence is still under observation. https://www.ixueshu.com/document/756eb25879eaa0d6318947a18e7f9386.html [accessed Nov 05, 2009] [in Chinese].
- 20.Deng HH, More than 150 cases of HINI vaccination have been reported abnormal reaction in more than 300,000 people nationwide. http://cn.chinagate.cn/infocus/2009-10/10/content_18678045.htm [accessed Oct 10, 2009] [in Chinese].
- 21.Orme B. 2nd ed. Research Publishers LLC; Madison: 2010. Getting started with conjoint analysis: strategies for product design and pricing research. [Google Scholar]
- 22.De Bekker-Grob E.W., Donkers B., Jonker M.F. Sample size requirements for discrete-choice experiments in healthcare: a practical guide. Patient. 2015;8:373–384. doi: 10.1007/s40271-015-0118-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daly A., Dekker T., Hess S. Dummy coding vs effects coding for categorical variables: clarifications and extensions. J Choice Model. 2016;21:36–41. [Google Scholar]
- 24.Hauber A.B., Gonzalez J.M., Prior T. Statistical methods for the analysis of discrete choice experiments: A report of the ISPOR conjoint analysis good research practices task force. Value Health. 2016;19:300–315. doi: 10.1016/j.jval.2016.04.004. [DOI] [PubMed] [Google Scholar]
- 25.Hole A.R. Modelling heterogeneity in patients' preferences for the attributes of a general practitioner appointment. J Health Econ. 2008;27:1078–1094. doi: 10.1016/j.jhealeco.2007.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Guo N., Marra C.A., Fitzgerald J.M. Patient preference for latent tuberculosis infection preventive treatment: A discrete choice experiment. Value Health. 2011;14:937–943. doi: 10.1016/j.jval.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Sadique M.Z., Nancy D., Edmunds W.J. The effect of perceived risks on the demand for vaccination: results from a discrete choice experiment. PLoS ONE. 2013;8:e54149. doi: 10.1371/journal.pone.0054149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.