Abstract
Introduction
Various surgical societies constantly update their recommendations in order to adapt surgical activity on current Pandemic conditions. The aim of this study is to analyze how hospitalizations and emergency operations have changed in our Department of Medical and Surgical Sciences in the Hospital of Foggia during covid-19 pandemic.
Methods
Our cohort-study was conducted by analyzing two groups of patients admitted to the Department of Medical and Surgical Sciences of the Hospital of Foggia: those admitted during the no-covid period from March 09th, 2019 to May 09th, 2019 and those during the covid period from March 09th, 2020 to May 09th, 2020.
Results
A total of 750 patients admitted during the no-covid period of 2019 and 171 during the covid period of 2020, of these 222 were emergency admission during 2019 and 97 during 2020, 528 were elective admission during 2019 and 74 during 2020. Of the emergency admissions (222 during 2019 and 97 during 2020), 91 were operated during the no covid period in 2019 and 52 during the covid period in 2020. The mean Mannheim Peritonitis Index Score, that is a scoring system used in peritonitis which is simple and cost-effective, were 15.6 during the no covid period of 2019 and 22.2 during the covid period of 2020. We observed 29 post-operative complications during 2019 and 26 during 2020.
Conclusions
Contraction of admissions for urgent and emergent conditions in the first period of lockdown has been followed from some positive effects as well as aggravating consequences.
Keywords: Covid-19, General surgery, Pandemic, Emergency surgery
Highlights
-
•
In this study, a comparison between hospitalization rates during the Covid-19 period and the Non Covid-19 period was held.
-
•
This report shows a significant decrease in elective admission.
-
•
With this study it was observed a reluctance of seriously ill patients to seek medical assistance, with a worsening of the postoperative outcome.
•We have noted a later and slower clinical recovery in patients treated during the COVID-19 period (March to May 2020).
1. Introduction
On December 31st, 2019, 27 pneumonia cases of unknown aetiology were identified in Wuhan City, Hubei province, China [1]. Those cases mainly presented with clinical symp-toms of dry cough, dyspnea, fever and bilateral lung infiltrates on imaging. The causative agent was identified from throat swab samples performed at Chinese Centre for Disease Control and Prevention (CDC) on January 7th, 2020. The disease was subsequently named Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), while World Health Organization (WHO) named it COVID-19 [2,3].
After an initial diffusion in China [4], Italy represents one of the most affected countries, with more than 230,000 cases on June 4, 2020 [5]. Worldwide health systems were reorganized with the aim to both cope with the new disease and maintain essential health service delivery. In this scenario, a concrete risk of health system collapse should be taken into consideration. The large number of patients suffering from respiratory distress syndrome led to an inevitable modification of daily clinical and surgical activity. Various international surgical societies constantly update their recommendations in order to adapt surgical activity on current conditions [6,7].
The patients in need of sub-intensive or intensive care increased esponentially and for most of the healthcare systems around the globe this was a crisis of unprecedented magnitude in the post-world war era. While the population continues to be affected by the whole spectrum of pre-existing diseases, hospitals were swamped with a massive number of COVID-19 patients to the point that prompted the Institutions to create COVID-19 dedicated wards and hospitals with redistribution of healthcare workers (HCW) from non-COVID-19 to COVID-19 intensive and sub-intensive units. In this context, majority of surgical departments were forced, due to reduced manpower/facilities and to limit the viral spread, to re-schedule their activity giving priority to urgent/emergent and non-deferrable oncological cases. The prioritization of patients is a complex strategy that set several organizational and ethical chellenges. The aim of this study is to analyze how hospitalizations and emergency operations have changed in our Department of Medical and Surgical Sciences in the Hospital of Foggia during covid-19 pandemic.
2. Materials and methods
Our cohort-study was conducted by analyzing two groups of patients admitted to the Department of Medical and Surgical Sciences of the Hospital of Foggia, Apulia southern part of Italy: those admitted during the no-covid period from March 09th, 2019 to May 09th, 2019 and those during the covid period from March 09th, 2020 to May 09th, 2020. We considered emergency admissions and its treatment (operated and not-operated), demographic and clinical characteristic of urgently operated patients (sex, age, ASA, Mannheim peritonitis Index score and Clavien-Dindo classification).
The statistical analysis were carried out using Fisher exact test, Chi-Square test, Standard Deviation and T-test unpaired one tailed.
3. Results
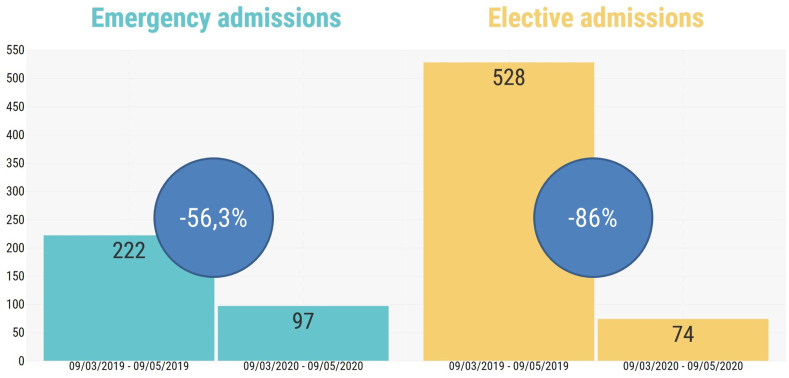
From the collected data and the statistical analysis carried out we observed a total of 750 patients admitted during the no-covid period of 2019 and 171 during the covid period of 2020, of these 222 (29,6%) were emergency admission during 2019 and 97 (56,7%) during 2020 (p < 0.00001), 528 (70,4%) were elective admission during 2019 and 74 (43,3%) during 2020 (p < 0.00001) (Table 1).(Table 2) (Table 3).
Table 1.
Of the emergency admissions (222 during 2019 and 97 during 2020), 91 (41%) were operated during the no covid period in 2019 and 52 (53.6%) during the covid period in 2020.
| Admissions to the surgery department in 2019 and 2020 | |||
|---|---|---|---|
| 09/03/2019 |
09/03/2020 |
p-value | |
| 09/05/2019 | 09/05/2020 | ||
| Total admissions, n | 750 | 171 | <0.00001* |
| Type of admission, n (%) | <0.00001** | ||
| Emergency | 222 (29.6) | 97 (56.7) | |
| Elective | 528 (70.4) | 74 (43.3) | |
*Fisher exact test; **Chi-square test.
Table 2.
Urgently operated patients were equally distributed between the two sexes in both the 2019 and 2020 periods, with a mean age of 64.6 years in 2019 and 65.3 years in 2020, with ASA score mainly II (39 patients (42.8%) during 2019 and 18 patients (34.6%) during 2020 and III (31 patients (34,1%) during 2019 and 21 patients (40,4%) during 2020).
| Emergency admissions to the surgery department in 2019 and 2020 | |||
|---|---|---|---|
| 09/03/2019 |
09/03/2020 |
p-value | |
| 09/05/2019 | 09/05/2020 | ||
| Emergency admissions, n | 222 | 97 | <0.00001∗ |
| Treatment, n (%) | 0.037∗ | ||
| Operated | 91 (41) | 52 (53.6) | |
| Not-operated | 131 (59) | 45 (46.4) | |
Chi-square test.
Table 3.
The mean Mannheim Peritonitis Index Score, that is a scoring system used in peritonitis which is simple and cost-effective, were 15.6 (8.7) during the no covid period of 2019 and 22.2 (10.2) during the covid period of 2020 (p = 0.017).
| Demographic and clinical characteristics of urgently operated patients in 2019 and 2020 | |||
|---|---|---|---|
| 09/03/2019 |
09/03/2020 |
p-value | |
| 09/05/2019 |
09/05/2020 |
||
| (n = 91) | (n = 52) | ||
| Sex, n (%) F M |
0.568* | ||
| 43 (47.3) | 22 (42.3) | ||
| 48 (52.7) | 30 (57.7) | ||
| Age (y) | 0.425** | ||
| Mean (SD) | 64.6 (20.2) | 65.3 (19.3) | |
| Median | 68 | 71 | |
| Range | 16–97 | 18–92 | |
| ASA score, n (%) | 0.753* | ||
| I | 13 (14.3) | 7 (13.5) | |
| II | 39 (42.8) | 18 (34.6) | |
| III | 31 (34.1) | 21 (40.4) | |
| IV | 8 (8.8) | 6 (11.5) | |
SD, Standard Deviation; ASA, American Society of Anesthesiology; *Chi-square test; **T-test unpairedone-tailed.
Post-operative Intensive Care Unit admissions were 17 (18,7%) during the no covid period of 2019 and 20 (38,5%) during the covid period of 2020 (p = 0,009).
We observed 29 (31.9%) post-operative complications during 2019 and 26 (50%) during 2020 (p = 0.032).
Mean length of stay was 7,7 days during the no covid period of 2019 and 9.7 days during the covid period of 2020 (p = 0.045) (Table 4).
Table 4.
Intra and postoperative characteristics of urgently operated patients in 2019 and 2020
| Intra and postoperative characteristics of urgently operated patients in 2019 and 2020 | |||
|---|---|---|---|
| 09/03/2019 |
09/03/2020 |
p-value | |
| 09/05/2019 |
09/05/2020 |
||
| (n = 91) | (n = 52) | ||
| MPI Score | 0.017* | ||
| Mean (SD) | 15.6 (8.7) | 22.2 (10.2) | |
| Median | 12 | 21 | |
| Range | 5–34 | 5–40 | |
| Post-op ICU admission, n (%) | 17 (18.7) | 20 (38.5) | 0.009** |
| Post-op complications, n (%) | 29 (31.9) | 26 (50) | 0.032** |
| Clavien-Dindo classification, n (%) | 0.226** | ||
| I | 4 (13.9) | 3 (11.5) | |
| II | 7 (24.1) | 5 (19.3) | |
| III | 1 (3.4) | 5 (19.3) | |
| IV | 5 (17.2) | 1 (3.8) | |
| V | 12 (41.4) | 12 (46.1) | |
| Duration of stay (d) | 0.045* | ||
| Mean (SD) | 7.7 (5.6) | 9.7 (7.4) | |
| Median | 6 | 7 | |
| Range | 2–30 | 2–40 | |
MPI Score, Mannheim Peritonitis Index Score; ICU, Intensive Care Unit; SD, Standard Deviation; *T-test unpairedone-tailed; **Chi-square test.
4. Discussion
On December 2019, the World Health Organization (WHO) declared the novel coronavirus disease 2019 (COVID-19) a global pandemic [8,9], which classifies the outbreak in Wuhan, China. The pathogen, named SARS-CoV-2 by the World Health Organization (WHO) [10], is responsible for a novel pneumonia affecting the lower respiratory tract, referred to as Coronavirus Disease 2019 (COVID-19). COVID-19 represents a global pandemic, affecting 212 countries and territories around the world, with over 3.200.000 infected subjects and more than 228.000 deaths [11,12].
The rapidly spreading outbreaks imposes an unprecedented burden of the effectiveness and sustainability of our healthcare system [13,14].
In our hospital and especially in our surgery department we had to face acute challenges [15,16].
Following the declaration of the pandemic, we were obliged to cancel elective surgery as a high risk of virus spreading subsisted [[17], [18], [19]].
While our institution postponed non-urgent elective surgeries and discharged all the medically fit inpatients, we had to rapidly expand the acceptance capacity for patients needing respiratory support. In this study, focused on the impact of COVID-19 on hospitals, a comparison between hospitalization rates during the Covid-19 period and the Non Covid-19 period was held [20,21]. This evaluation shows a significant decrease in hospitalization rates across our units during the days of Covid-19 outbreak [[22], [23], [24]]. 171 patients were hospitalized in 2020, notably less than the 750 patients held during the same time interval in 2019 (p < 0.0001) (Fig. 1).
Fig. 1.
Admissions to the surgery department in 2019 and 2020.
This report shows a significant decrease in elective admission, accounting to the 56,7% of total hospitalizations in 2020. This rate was significantly lower than the rate expressed during the previous year, in which elective admission constitued the 70% of total hospitalizations (Fig. 2).
Fig. 2.
Emergency and elective admission to the surgery department in 2019 and 2020.
Considering all our admission, only the 41% of the patients underwent surgical treatment in 2019, in comparison with the 53% of the current year. This information might be explained considering that the number of “improper accesses” to the Emergency Room during the pandemic period suffered a large decrease in numbers and, consequently, the hospitalizations in the surgical department were actually more likely to need surgical treatment.
Gender-age and ASA score related admissions rates remained unchanged during the COVID-19 pandemic if compared to the previous year.
It has been widely reported that Accident & Emergency (A&E) attendances have dropped significantly during the pandemic. Two scoring system were employed to evaluate the outcomes of the surgery-requiring emergency admissions.
The Mannheim Peritonitis Index (MPI) is one of the most reliable scoring systems for peritonitis. Peritonitis from perforation of abdominal viscera is associated with high mortality.
This study shows an increase of the MPI during the considered period. As we already stated, the A&E attendance during the COVID-19 dropped to the lowest level. These changes may have led to some positive effects (such as reducing non relevant access to A&E) as well as aggravating consequences: for istance the reluctance of severely ill patients to ask for medical assistance.
Delays in hospital admission for severe cases are tipically associated with a higher number of post operative complications.
In our study we furtherly analysed the post-operative complications considering the Clavien-Dindo classification: 50% of patients treated during the covid period suffered post-operative complications, in comparison with the 31.9% recorded during the same period in 2019.
From the collected data we also highlighted an increase in hospital stay durations: 9.9 days during the covid 2020 period in opposition to a mean value of 7.7 days of the non-covid 2019 period.
All patients were examined after 5–10 and 15 days from the date of discharge. Oncological patients were sent to oncological follow-up and possible chemotherapy. We have noted a later and slower clinical recovery in patients treated during the COVID-19 period (March 09th, 2020 to May 09th, 2020).
Considering all the emergency surgery held during the COVID-19 pandemic, 38.5% of the patients required admission in the ICU, while only 18.7% of the patients treated during the non-Covid period needed the same support.
The limitations of our study are the short period considered and the inequality of number of patients between the two groups considered, but the exceptionality of the period must be considered.
5. Conclusions
One mainly consideration arises from this data: contraction of admissions for urgent and emergent conditions in the first period of lockdown has been followed from some positive effects (such as reducing non relevant access to A&E) as well as aggravating consequences: for istance the reluctance of severely ill patients to ask for medical assistance, with a worsening of postoperative outcome.
Declaration of competing interest
The authors declare no competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2020.12.001.
Declarations
Ethics approval and consent to participate: The ethics committee of our institution approved the study.
Consent for publication: Informed consent was obtained from all individual participants included in the study.
Availability of data and material.
Funding
No funding.
Authors' contributions
NICOLA TARTAGLIA and GIOVANNA PAVONE performed the study conception and design. VINCENZO LIZZI and FERNANDA VOVOLA analysed and interpreted the data. MARIO PACILLI and FAUSTO TRICARICO contributed to acquisition of the data. ANTONIO AMBROSI revised the manuscript. Provenance and peer review Not commissioned, externally peer reviewed.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al Jabir A. World health organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j. ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez Morales A.J., Cardona Ospina J.A., Gutiérrez Ocampo E., Villamizar Peña R., Holguin Rivera Y., Escalera Antezana J.P. Latin American net- work of coronavirus disease 2019-COVID-19 research (LAN- COVID-19). Electronic address. 2020. https://www.lancovid.org Clinical, laboratory and imaging features of COVID-19: a sys- tematic review and meta-analysis. Travel Med Infect Dis. 13, 101623.
- 3.Francesca Sanguedolce, Matteo Landriscina, Antonio Ambrosi, Nicola Tartaglia, Pasquale Cianci, Marcello Di Millo. 2017. Bladder Metastases from Breast Cancer: Managing the Unexpected. A Systematic Review. UROLOGIA INTERNATIONALIS, ISSN. [DOI] [Google Scholar]
- 4.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. China novel coronavirus investigating and research team. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. Feb 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Remuzzi A., Remuzzi G. vol 20. 2020. (COVID-19 and Italy: what Next? Lancet). Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tao K.X., Zhang B.X., Zhang P., Zhu P., Wang G.B., Chen X.P. General surgery branch of Hubei medical association, general surgery branch of Wuhan medical association. Recommendations for general surgery clinical practice in 2019 coronavirus disease situation. Zhonghua Wai Ke Za Zhi. 2020;58(3):170–177. doi: 10.3760/cma.j.issn.0529-5815.2020.03.003. (Chinese) [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons releases recommendations for surgical management of elective operations during COVID-19 pandemic. https://www.facs.org/about-acs/covid-19/information-for-surgeons
- 8.Nicola Tartaglia, Pasquale Cianci, Alessandra Di Lascia, Alberto Fersini, Antonio Ambrosi, Vincenzo Neri. Laparoscopic antegrade cholecystectomy: a standard procedure? Open Med. 2016;11:429–432. doi: 10.1515/med-2016-0078. ISSN: 2391-5463, doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neri Vincenzo, Ambrosi Antonio, Fersini Alberto, Tartaglia Nicola, Cianci Pasquale, Lapolla Francesco. Laparoscopic cholecystectomy: evaluation of liver function tests. Ann. Ital. Chir. 2014;85(5):431–437. 1 September 2014, ISSN: 0003-469X. [PubMed] [Google Scholar]
- 10.WHO Country & Technical guidance - coronavirus disease (COVID-19) 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical- guidance,
- 11.Worldometer, Cases Coronavirus. Worldometer. 2020. [DOI]
- 12.Wacha H., Linder M.M., Feldman U., WeschG Gundlach E., Steifensand R.A. Mannheim peritonitis index - prediction of risk of death from peritonitis: construction of a statistical and validation of an empirically based index. Theor. Surg. 1987;1:169–177. [Google Scholar]
- 13.Tartaglia N., Pavone G., Di Lascia A. Robotic voluminous paraesophageal hernia repair: a case report and review of the literature. J. Med. Case Rep. 2020;14(1):25. doi: 10.1186/s13256-020-2347-6. Published 2020 Feb 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Polito R., Scarinci A., Ambrosi A. The beneficial effects of physical activity and weight loss on human colorectal carcinoma cell lines. Journal of Human Sport and Exercise. 2020;15(Proc2):S252–S260. doi: 10.14198/jhse.2020.15.Proc2.16. [DOI] [Google Scholar]
- 15.Cascella M., Rajnik M., Cuomo A. Features, evaluation and treatment coronavirus (COVID-19) 2020. https://www.ncbi.nlm.nih.gov/books/NBK554776 Mar 8. [PubMed]
- 16.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475–481. doi: 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhou F., Yu T., Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;S0140–6736(20):30566–30573. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organisation . WHO; Geneva: 2020. WHO Director General's Open- Ing Remarks at the Media Briefing on COVID-19–11 March 2020. [Google Scholar]
- 19.Spina S., Marrazzo F., Migliari M., Stucchi R., Sforza A., Fumagalli R. The response of milan's emergency medical system to the COVID-19 outbreak in Italy. Lancet. 2020;395(10227):e49–e50. doi: 10.1016/S0140-6736(20)30493-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Lascia A., Tartaglia N., Petruzzelli F. Right hemicolectomy: laparoscopic versus robotic approach [published online ahead of print, 2020 Jun 10] Ann. Ital. Chir. 2020;9 S0003469X20031656. [PubMed] [Google Scholar]
- 21.Longhitano L., Tibullo D., Giallongo C., Lazzarino G., Tartaglia N., Galimberti S. Proteasome inhibitors as a possible therapy for SARS-CoV-2. Int. J. Mol. Sci. 2020;21:3622. doi: 10.3390/ijms21103622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gallieni M., Del Maestro M., Luzzi S., Trovarelli D., Ricci A., Galzio R. Endoscope-assisted microneurosurgery for intracranial aneurysms: operative technique, reliability, and feasibility based on 14 Years of personal experience. Acta Neurochir. Suppl. 2018;129:19–24. doi: 10.1007/978-3-319-73739-3_3. [DOI] [PubMed] [Google Scholar]
- 23.Bongetta D., Zoia C., Luzzi S. Neurosurgical issues of bariatric surgery: a systematic review of the literature and principles of diagnosis and treatment. Clin. Neurol. Neurosurg. 2019;176:34–40. doi: 10.1016/j.clineuro.2018.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Luzzi S., Giotta Lucifero A., Del Maestro M. Anterolateral approach for retrostyloid superior parapharyngeal space schwannomas involving the jugular foramen area: a 20-year experience. World Neurosurg. 2019;132:e40–e52. doi: 10.1016/j.wneu.2019.09.006. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.