Abstract
BACKGROUND:
Gender disparities in authorship of heart failure (HF) guideline citations and clinical trials have not been examined.
METHODS:
We identified authors of publications referenced in Class I Recommendations in United States (n=173) and European (n=100) HF guidelines and of publications of all HF trials with >400 participants (n=118) published between 2001 and 2016. Authors’ genders were determined, and changes in authorship patterns over time were evaluated with linear regression and nonparametric testing.
RESULTS:
The median proportion of women authors per publication was 20% (interquartile range [IQR], 8%–33%) in United States guidelines, 14% (IQR, 2%–20%) in European guidelines, and 11% (IQR, 4%–20%) in HF trials. The proportion of women authors increased modestly over time in United States and European guidelines’ references (β=0.005 and 0.003, respectively, from 1986 to 2016; P<0.001) but not in HF trials (12.5% [IQR, 0%–20%] in 2001–2004 to 8.9% [IQR, 0%–20%] in 2013–2016; P>0.50). Overall proportions of women as first or last authors in HF trials (16%) did not change significantly over time (P=0.60). North American HF trials had the highest likelihood of having a woman as first or senior author (24%). HF trials with a woman first or senior author were associated with a higher proportion of enrolled female participants (39% versus 26%, P=0.01).
CONCLUSIONS:
In HF practice guidelines and trials, few women are authors of pivotal publications. Higher number of women authors is associated with higher enrollment of women in HF trials. Barriers to authorship and representation of women in HF guidelines and HF trial leadership need to be addressed.
Keywords: clinical trial, guideline, heart failure, publications, women
Women remain significantly underrepresented in cardiovascular medicine.1–8 Measures of academic productivity, like publications, also reflect this disparity. By convention, the first and last (ie, senior) authorship positions identify individuals who contributed most to article conception and generation.9 Despite being more likely than men to be employed as faculty at schools ranked highly in research, women cardiologists have fewer first and last author publications and are awarded fewer grants from the National Institutes of Health (NIH).10 Even among NIH R01-supported cardiovascular researchers, women were ≈50% less frequently positioned as last author and were first authors at a significantly lower rate than men in high-impact journals.11 Coinciding with disparities in publications, the odds of being a full professor affiliated with a United States medical school were 37% lower for women than men.10 Among the 40 top-ranked cardiology programs in the United States, no cardiology division or department chief is a woman.12
Among the cardiovascular subspecialties, Advanced Heart Failure and Transplant Cardiology has a relatively higher proportion of women physicians. Women comprised 31% of United States heart failure (HF) cardiology trainees in 2017 to 2018.13 Since 2016, increasing numbers of women cardiologists have taken the European Society of Cardiology’s postgraduate course and certification exam in HF.14 However, despite the higher representation in HF cardiology, recent international survey data showed that women were more likely to perceive gender-based differences in salary, promotion, and leadership in HF cardiology careers.15
In this study, we sought to investigate how these observations translate to the representation of women in HF research. We hypothesized that women are underrepresented both as leaders of and as participants in the work that heavily influences worldwide HF clinical practice. Thus, we examined the distributions and temporal trends in authorship among women and men in the publications cited in major society HF practice guidelines (HF guidelines citations), as these guidelines influence clinical care, and in pivotal contemporary HF trials (HF clinical trials), as these publications are most often used to support guideline recommendations. Finally, we explored the relationship between authorship and enrollment of women as participants in HF clinical trials.
This work was stimulated by the Heart Failure Collaboratory, a multi-stakeholder group comprised of patients, clinicians, investigators, the Food and Drug Administration, industry sponsors, and other government agencies that seek to improve evidence generation for and implementation of new HF therapies and representation of underrepresented populations in clinical trials.16
METHODS
HF Guidelines Citations
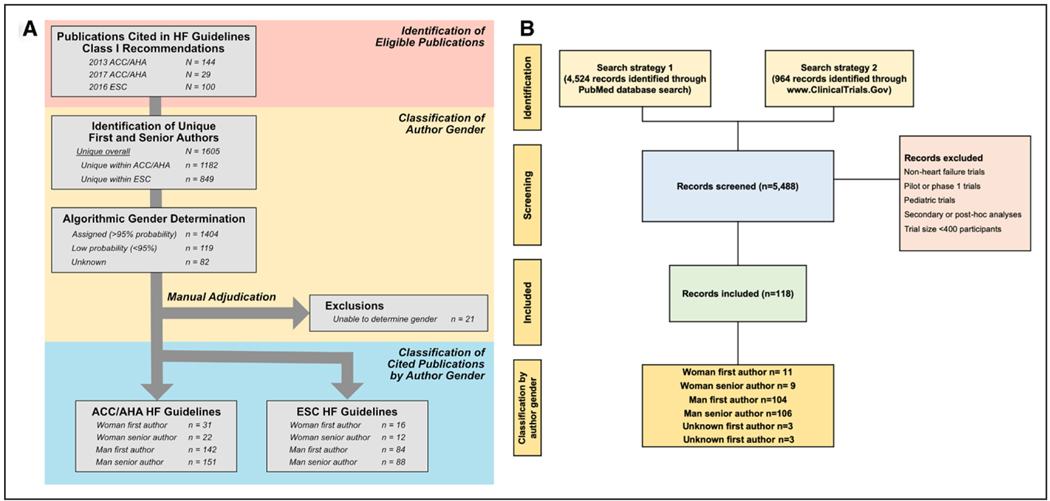
The data that support the findings of this study are available from the corresponding author upon reasonable request. We identified all unique publications cited in Class I Recommendations in the 2013 American College of Cardiology Foundation/American Heart Association (ACC/AHA), 2017 American College of Cardiology/American Heart Association/Heart Failure Society of America (ACC/AHA), and 2016 European Society of Cardiology (ESC) HF guidelines.17–19 Author order was used to determine first, middle, and senior authors. Co-first and co-senior authorships were not identified. Consortium and investigator groups were excluded. Citation metadata was extracted by a reference manager (EndNote, Clarivate Analytics) and included (1) author first and last name; (2) article title; (3) publication journal; and (4) publication year (Figure 1A).
Figure 1. Methodology for publication/trial selection and author gender identification.
A, Methodology for heart failure guideline citations analysis. B, Methodology for heart failure clinical trial analysis. ACC/AHA indicates American College of Cardiology/American Heart Association; ESC, European Society of Cardiology; and HF, heart failure.
HF Clinical Trials
We identified all HF clinical trials published between January 2001 and December 2016 using (1) PubMed/MEDLINE query with the following limits: publication year, “heart failure,” “trial*,” and “randomized” and (2) ClinicalTrials.gov query with the following limits: adult (18 years and older), interventional, phase II–IV, “heart failure.” We excluded phase I, pilot trials, secondary, interim, or post hoc analyses. Trials enrolling <400 patients were excluded as they mostly represent single-center, early phase trials. Two independent reviewers screened 5488 studies identified and a third reviewer resolved discordant assessments as previously described.20 A total of 118 published trials met inclusion criteria for this study (Figure 1B).
The following data were abstracted: (1) year of publication; (2) intervention; (3) enrollment duration; (4) total subjects enrolled; (5) number of participating centers; (6) number of countries; (7) mean age of the cohort; (8) proportion of women enrolled; (9) race and ethnicity when reported; (10) primary end points; and (11) funding sources.
The proportions of enrolled women per trial were obtained from trial publications and were reported as weighted means indexed to sample size of each trial. Based on ClinicalTrials. gov designations, funding source was classified as (1) industry; (2) government; and (3) university or other nonprofit or nonfederal organizations. Primary end points were classified as (1) mortality; (2) intermediate (eg, quality of life, dyspnea relief, hospitalization, length of stay); or (3) surrogate (eg, pulmonary capillary wedge pressure, natriuretic peptides, etc). Regions were divided based on region of primary enrollment: (1) exclusively North America; (2) exclusively Western Europe; (3) exclusively outside of North America and Western Europe, that is, rest of the world; and (4) mixed/multiregional. For information not reported in the main published article, we searched the supplementary data and corresponding trial registration entries.
Identification of Authors’ Gender
For the HF guidelines citations, first, middle, and senior authors genders were determined by matching first name with predicted gender using a previously validated database (Genderize.io).21 Gender was assigned to an author if Genderize.io predicted the gender at a probability ≥95%, a higher threshold than has been used in prior work with this database.11,22 Using this approach, 82 unique authors were categorized as unknown and 119 did not meet the 95% probability threshold (ie, low probability). These authors’ names were independently reviewed, and search engines, social media profiles, and institutional websites that linked publications to authors were used to manually adjudicate gender and authorship. Authors were not directly contacted to confirm gender assignment. Twenty-one unknown authors’ genders could not be distinguished, and they were excluded from the primary analyses.
For HF clinical trials, author genders were determined by confirming first name with self-identification on institutional websites, social media accounts with publications listed, and other search engines to find photographs or biographical paragraphs. Authors with gender not clearly distinguishable from these sources were marked as unknown, and the corresponding article was excluded from the analysis (n=3).
Statistical Analysis
HF Guideline Citation Authorship
From the HF guidelines citation authorship data set, we derived the total number of authors per publication, percent women authorship, and indicators of women first or senior authorship. Continuous variables were described with medians and interquartile ranges (IQRs) and categorical variables as n (%). Scatterplots of individual publications and fitted linear regression were used to evaluate percent women authorship over time, weighted by total publication authorship, and performed separately for ACC/AHA and ESC guideline sources. The Wald test was used to test if the regression slope was equal to zero. A P<0.05 was regarded to be statistically significant. Stacked bar charts were used to display the gender proportions on an individual publication basis. We created violin plots to evaluate the number of men versus women authors per publication, stratified by guideline source, and further subdivided by first and senior author genders. Wilcoxon rank-sum tests were used to compare strata, with a Bonferroni correction for 2 comparisons applied (thus regarding P<0.025 as statistically significant). The numbers of publications per unique author were compared between sources using Wilcoxon rank-sum tests and displayed using jittered scatterplots. We used multivariable linear regression with forward stepwise selection and a minimized Bayesian Information Criterion to identify a final model with predictors of publication percent women authorship, considering first male author, last male author, number of authors, guideline source, and year of publication as potential predictors. We performed a sensitivity analysis assuming that the 21 unknown gender authors were all women.
HF Clinical Trial Authorship
Trials were classified based on their publication year into 4 four-year periods (2001–2004, 2005–2008, 2009–2012, and 2013–2016). Continuous variables were described with medians and IQRs and categorical variables as n (%). Categorical variables were compared using χ2 testing. Continuous variables were compared across nominal categories with the use of the Kruskal-Wallis test. Given smaller numbers in the subgroups, a composite of woman first or last author was used. We determined the correlation between the proportion of women authors in each trial and trial characteristics. To test for a trend in women authors across our study period, we performed simple linear regression models using year of publication as the independent variable. For predictors of women enrollment per trial (log-transformed given skewed distribution), we used a linear regression model considering trial characteristics (number of participants, number of sites, region of enrollment, funding mechanism, trial intervention, and proportion of women authors in each trial) as potential predictors.
As publicly available data were used and individual patient-level data were not accessed, this analysis was not submitted for institutional review board review. Data analyses were performed using STATA 15.1/IC (College Station, TX) and IBM SPSS 25 (IBM Corporation). Authors Drs Reza and Tahhan had access to the data and take responsibility for its integrity and analysis.
RESULTS
HF Guideline Citation Authorship
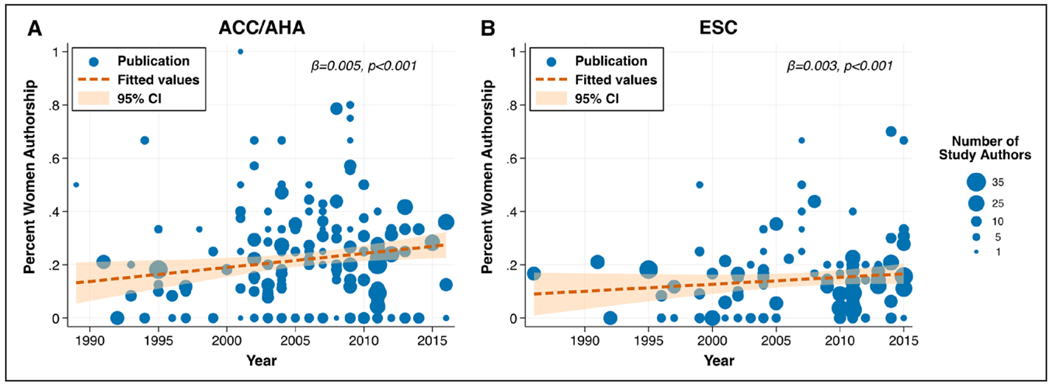
A total of 144 publications, 29 publications, and 100 publications were analyzed from the 2013 ACC/AHA, 2017 ACC/AHA, and 2016 ESC HF guidelines, respectively. Overall, 2031 authors were cited by the United States (n=1182) and European (n=849) guidelines; 1605 of these authors were unique. The median author number per cited publication was 9 (IQR, 5–12) for ACC/AHA, and 10 (IQR, 6–17) for ESC (Table 1). Percent women authorship was lower in ESC guideline citations as compared with ACC/AHA (14% versus 20%, P=0.002). The overall proportions of women as first authors in the United States and European guideline citations were 18% and 16%, respectively, and as last authors were 13% and 12%. From 1986 to 2016, percent women authorship modestly increased in both United States and European guideline citations (Figure 2A and 2B, each P<0.001). Qualitatively, a large proportion of cited publications were exclusively authored by men in both guidelines, with comparatively few publications having a predominance of women authorship (Figure IA and IB in the Data Supplement).
Table 1.
Characteristics of Publications of HF Trials and Guidelines Citations
| Publication Characteristics | All HF Trials | Man, as First or Senior Author | Woman, as First or Senior Author | ACC/AHA Citations | ESC Citations |
|---|---|---|---|---|---|
| Authors, median (IQR) | |||||
| No. of publications | 118 | 97 | 18 | 173 | 100 |
| Total no. of authors per publication | 12 (8–15) | 12 (9–15) | 9 (7–11) | 9 (5–12) | 10 (6–17) |
| No. of women authors per publication | 1.0 (1.0–2.0) | 1.0 (0–2.0) | 2.5 (1.0–4.0) | 2.0 (1.0–3.0) | 1.0 (0.5–3.0) |
| Proportion of women authors per publication | 11.1 (3.5–20) | 8.3 (0–17.6) | 22.1 (16.7–33.3) | 20.0 (8.3–33.3) | 14.3 (1.6–20.4) |
| Woman first author | 11 (9.6) | 0 (0) | 11 (61.1) | 31 (17.9) | 16 (16.0) |
| Woman senior author | 9 (7.8) | 0 (0) | 9 (50) | 22 (12.7) | 12 (12.0) |
| Sponsor, n (%) | |||||
| Government | 23 (19.5) | 13 (13.4) | 8 (44.4) | … | … |
| University/Organization | 19 (16.1) | 15 (15.5) | 3 (16.7) | … | … |
| Industry | 74 (62.7) | 67 (69.1) | 7 (38.9) | … | … |
| Unclear | 2 (1.7) | 2 (2.1) | 0 (0) | … | … |
| Primary outcome* n (%) | |||||
| Mortality | 83 (70.3) | 67 (69.1) | 16 (88.9) | … | … |
| Nonmortality intermediate outcomes | 22 (18.6) | 18 (18.6) | 2 (11.1) | … | … |
| Surrogate outcomes | 13 (11) | 12 (12.4) | 0 (0) | … | … |
| Intervention, n (%) | |||||
| Invasive | 29 (24.6) | 26 (26.8) | 3 (16.7) | … | … |
| Medication | 63 (53.4) | 55 (56.7) | 6 (33.3) | … | … |
| Others | 26 (22) | 16 (16.5) | 9 (50) | … | … |
| Population studied, n (%) | |||||
| HF with reduced EF | 94 (79.7) | 80 (82.5) | 11 (61.1) | … | … |
| HF with preserved EF | 4 (3.4) | 1 (1) | 3 (16.7) | … | … |
| HF regardless of EF | 20 (16.9) | 16 (16.5) | 4 (22.2) | … | … |
| Region of enrollment, n (%) | |||||
| North America | 29 (26.1) | 22 (23.9) | 7 (43.8) | … | … |
| Western Europe | 19 (17.1) | 15 (16.3) | 3 (18.8) | … | … |
| Rest of the world | 6 (5.4) | 3 (3.3) | 1 (6.3) | … | … |
| Mixed/multiregional | 57 (51.4) | 52 (56.5) | 5 (31.3) | … | … |
| Patient enrolled, median (IQR) | 994 (550–1854) | 1030 (572–2033) | 876 (614–1050) | … | … |
| Duration (y), median (IQR) | 2.8 (2–3.9) | 2.6 (1.9–3.9) | 3 (2.2–3.9) | … | … |
| No. of sites per trial, median (IQR) | 82 (28–171) | 91 (43–173) | 40 (9–161) | … | … |
| No. of countries per trial, median (IQR) | 4 (1–15.5) | 6 (1–16) | 2 (1–8) | … | … |
ACC indicates American College of Cardiology; AHA, American Heart Association; EF, ejection fraction; ESC, European Society of Cardiology; HF, heart failure; and IQR, interquartile range.
Nonmortality intermediate outcomes included quality of life, dyspnea relief, hospitalization, length of stay. Surrogate outcomes included pulmonary capillary wedge pressure, natriuretic peptides.
Figure 2. Percent women authorship per publication over time.
A, American College of Cardiology/American Heart Association (ACC/AHA) heart failure guidelines Class I Recommendations citations.
B, European Society of Cardiology (ESC) heart failure guidelines Class I Recommendations citations. Fitted regression lines are weighted by total number of authors per cited publication. Total number of authors per cited publication is represented by varying dot sizes as shown at figure right.
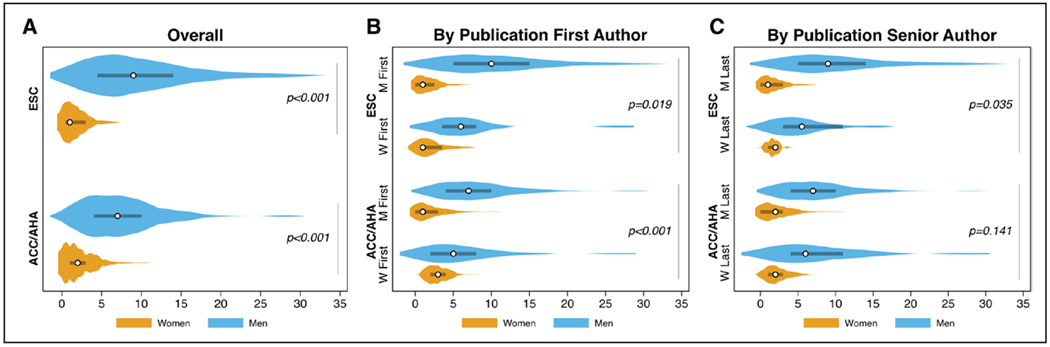
When evaluating the absolute number of men and women authors per cited publication, the number of women was significantly lower in both guideline sources (Figure 3A, each P<0.001). The gap in men versus women author predominance significantly narrowed when the cited publication first author was a woman in both ACC/AHA (P<0.001) and ESC (P=0.019) guidelines (Figure 3B). Although similar numerical trends were observed with the gender of cited publication senior authorship, these did not reach statistical significance (ACC/AHA P=0.141, ESC P=0.035; Figure 3C). In multivariable logistic regression, woman first (β=0.238, P<0.001) and woman senior authorship (β=0.101, P=0.001) were significantly associated with higher percent woman publication authorship. When including all unknown gender authors as women in a sensitivity analysis, these results were similar (woman first [β=0.240, P<0.001] and woman senior authorship [β=0.166, P=0.001]). Regarding individual author cited publication quantity, women had a significantly lower number of cited publications compared with men in the United States (P<0.001) but not European guidelines (Figure IIA and IIB in the Data Supplement).
Figure 3. Numbers of women and men authors per publication cited in the ACC/AHA and ESC heart failure guidelines Class I Recommendations.
A, author numbers stratified by guideline source. B, author numbers stratified by publication first author gender. C, author numbers stratified by publication senior author gender. Circle = median; Line = interquartile range. ACC/AHA indicates American College of Cardiology/American Heart Association; and ESC, European Society of Cardiology.
HF Clinical Trial Authorship
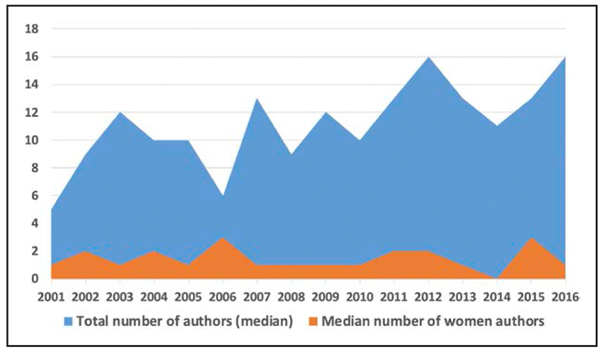
We identified 118 HF clinical trials of which 80% studied HF with reduced ejection fraction, and 31% of trials were conducted in multiple geographic regions (Table 1). Complete information on the gender of all authors was available for 115 (98%) of the trials; the remaining 3 trials were excluded. Overall, HF trials were cumulatively authored by 1488 authors (median 12, IQR, 8–15 per trial). The total number of authors per trial increased significantly from median of 9 (IQR, 7–12) authors in 2001 to 2004 to 13 (IQR, 11–17) authors in 2013 to 2016 (P<0.001 for trend, Figure 4). First (10%) and senior (8%) authors were infrequently women with 16% of publications having a woman as first or senior author. The median number of women authors per trial was 1.0 (IQR, 1.0–2.0). The median proportion of women first/senior authors per trial was 11% (IQR, 4%–20%). This distribution did not significantly change over time (14% first/senior woman author in 2001 to 2004 compared with 13% in 2013 to 2016, P for trend=0.66). Similarly, the median proportion of women authors did not significantly change over time (13% [IQR, 0%–20%] in 2001–2004 to 9% [IQR, 0%– 20%] in 2013–2016; P for trend >0.5, Figure 4).
Figure 4. Trends in number of total and women authors of heart failure clinical trials over 16-year study period.
Trials were classified based on their publication year into 4 four-year periods (2001–2004, 2005–2008, 2009–2012, and 2013–2016).
The total number of authors varied by region of primary enrollment. The highest number of total authors was found in trials conducted exclusively outside of North America and Western Europe, that is, rest of the world, with a median of 17 (IQR, 8–26) compared with 13 authors (IQR, 10–15) in mixed/multiregional trials, 12 (IQR, 8–14) authors in Western Europe, and 10 (IQR, 7–12) authors in North America (P=0.02 for comparison). The proportion of women authors per trial was significantly higher in trials conducted in North America (29%) compared with trials conducted in Western Europe (12%), mixed/multiregional (7%), and rest of the world (13%; P<0.001 for comparison). Similarly, publications of trials conducted in North America had the highest likelihood of having a woman as first or senior author (24%) compared with mixed/multiregional (9%) and Western European trials (17%; Table 2, Figure III in the Data Supplement).
Table 2.
Representation of Women Authors in HF Clinical Trials Based on Key Trial-Level Characteristics
| Trial Characteristics | Total No. of Trials, n (%) | Total No. of Authors Per Trial, Median (IQR) | Proportion of Women Authors Per Trial (%), Median (IQR) | First/Senior Woman Author, N (%) |
|---|---|---|---|---|
| Region of enrollment | ||||
| North America | 29 (26) | 10 (7–12) | 28.6 (12.5–39.1) | 7 (24) |
| Western Europe | 19 (17) | 12 (8–14) | 11.8 (7.1–16.7) | 3 (17) |
| Mixed/multiregional | 57 (51) | 13 (10–15) | 6.7 (0–15.4) | 5 (9) |
| Rest of the world | 6 (6) | 16.5 (8–26) | 13.4 (6.3–23.8) | 1 (25) |
| Funding source | ||||
| Government | 23 (20) | 10 (8–17) | 20 (14.3–33.3) | 8 (38) |
| NIH/NHLBI | 10 (9) | 10 (9–17) | 28 (20–50) | 5 (50) |
| Non-NIH/NHLBI | 13 (11) | 11 (8–19) | 13 (8–22) | 3 (30) |
| University/Organization | 19 (16) | 13 (8–18) | 19.7 (10–33.3) | 3 (17) |
| Industry | 74 (64) | 11 (8–14) | 7.4 (0–15.4) | 7 (9) |
| HF setting | ||||
| HF with reduced EF | 83 (70) | 11 (8–14) | 9.5 (0–172) | 10 (12) |
| HF with preserved EF | 4 (3) | 14 (73–21.5) | 17.9 (16.9–24.1) | 3 (75) |
| HF regardless of EF | 15 (13) | 9 (8–14) | 28.6 (12.5–33.3) | 4 (27) |
| Acute HF | 16 (14) | 14 (10–16) | 7.7 (6.3–20) | 1 (7) |
EF indicates ejection fraction; HF, heart failure; IQR, interquartile range; NHLBI, National Heart, Lung, and Blood Institute; and NIH, National Institutes of Health.
The total number of authors was similar across different funding mechanisms (P=0.32). The proportion of women authors per trial was significantly lower in industry-sponsored trials (median 7%; IQR, 0%–15%) compared with trials funded by government (median 20%; IQR, 14%–33%) or nonprofit organizations or universities (median 20%; IQR, 10%–33%; P<0.001 for comparison). About 38% of trials sponsored by government had a woman as first or senior author compared with 17% in nonprofit/university funded trials and 10% in industry-sponsored trials (P=0.01). Of the government-sponsored trials, NIH funded trials had higher proportions of women authors per trial (median 28%; IQR, 20%–50%) compared to non-NIH funded trials (median 13%; IQR, 8%–22%; Table 2, Figure III in the Data Supplement).
Trials testing therapies for acute HF were less likely to have a first/senior woman author (7%) compared with chronic HF therapy trials (17%). The average proportion of women authors was 8% in acute HF trials compared with 12% in chronic HF trials. Trials testing nonmedication, noninvasive interventions were more likely to have a first or senior woman author (36%) compared with trials testing medication (10%) or invasive interventions (10%; P=0.007).
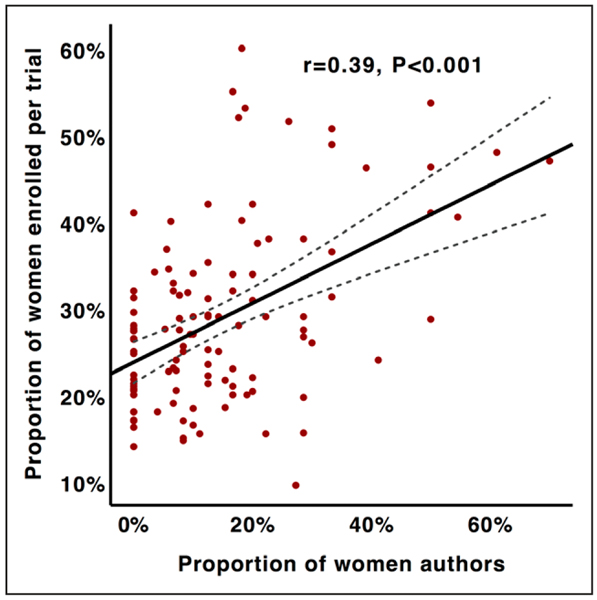
Association Between Women Authors and Enrollment of Female Participants
Trials with a woman as first or senior author were associated with higher proportion of weighted average of enrolled female participants (39% versus 26%, P=0.01). Similarly, trials authored by a larger proportion of women tended to enroll higher proportions of female participants (r=0.39, P<0.001; Figure 5). After adjusting for the number of participants, number of sites, region of enrollment, funding mechanism, and trial intervention, we found that the proportion of women authors per trial was the only significant independent predictor of female participant enrollment (β=0.31, P<0.001). The association between proportion of women authors and enrolled female participants was not modified by region of primary enrolment (P=0.70 for interaction).
Figure 5. Association between women authors and enrollment of women participants per trial.
DISCUSSION
In a comprehensive examination of ≈1500 unique authors contributing to contemporary HF guideline citations and ≈1500 authors of recent HF trials, we define the gender differences in bibliometric data that influence clinical HF practice. Fewer than 20% of authors of the publications that form the basis for the Class I Recommendations in the recent major international society HF practice guidelines and clinical trials are women. In the United States, ≈10% to 14% of active cardiologists are women.3,23,24 As of December 2018, women comprised 33.7% of the membership of ESC and a similar proportion of the membership of the Heart Failure Association of the ESC.14 Our data suggest that the proportions of women authors in guidelines and HF trials are consistently low.
Not all of the women authors examined in our study were cardiologists, an important consideration in the interpretation of these data. We were unable to quantify the demographics of individuals in each profession, however, we acknowledge that other health professionals and industry collaborators are represented in these authorships. As such, while we are unable to establish whether women authors are representative of the current cardiologist workforce, these data do support the global need to increase the number of women in cardiology, including in leadership positions and in clinical trial authorship.
Gender Differences in Authorship
Of the authors of all phase II–IV HF clinical trials published between 2001 and 2016, only one in 6 trials had a woman as a first or senior author. Our work aligns with other recent studies of gender disparities in cardiovascular research.25–28 These studies showed an increase in women authorship over time, a finding we corroborated in the HF Guideline Citation analysis. However, we found no significant change in the proportions of women first and senior authors of HF trials from 2001 to 2016 or in the total proportion of women authors of these trials. This suggests that while women may be becoming better represented as authors of general cardiovascular scholarship, the inclusion of women in clinical trial authorship has lagged.
Among publications cited for Class I Recommendations in US HF guidelines, individual women were less likely to author multiple publications, whereas individual men had significantly higher numbers of publications. Publications with a man as first or senior author were more likely to have a higher proportion of men as coauthors. This may suggest that men have greater access to high-impact research networks, collaborations, and support. Through these connections, their work may be assessed more favorably at peer review and serve to support additional scholarship. This in group bias, in which the alignment of some affinity between author and reviewer influences the article’s review, was demonstrated in a study in which fellowship applicants who had personal ties with an evaluation committee member were deemed to be significantly more competent than applicants of the same gender and academic productivity level who did not.29,30 Medical school faculty who publish more research and are promoted are known to frequently consult their colleagues.31 Women are known to be less involved with collaborative research in scientific fields and to negotiate less for professional requests.32,33 Women’s networks less often include men and collaborators from prior institutions of employment and are more likely to be negatively affected by parenthood and career transitions.31 In addition, there is considerable evidence to show that women in academia are held to and judged by a higher standard than men to garner similar accolades.29,34 This may translate to more stringent criteria for positive evaluations in peer review, study sections, and promotion for women and in fewer opportunities for collaboration. These biases likely contribute to this gender disparity in authorship and serve to exclude women from academic advancement.
Cardiology articles with women senior authors have been shown to be more likely to have women as first and middle authors, a finding we replicate, consistent with a positive influence of women role models in the field.26 In a large survey of United States medical residents regarding career choice, having a role model was one of the most highly rated professional development needs identified, and women were more likely to negatively perceive the lack of diversity and role modeling in cardiology.35 Further research exploring the factors related to exclusively female or male-authored articles may lend insights into interventions to support gender parity in research in the future.
Enrollment of Women in Clinical Trials
We found that the proportion of women authors per trial was the only significant independent predictor of female participant enrollment after accounting for potential trial-level confounders. Improvement in women representation in cardiovascular clinical trials has been a longstanding target for federal organizations.36 Since 1990, the US General Accounting Office, Food and Drug Administration, and NIH have published targeted regulations to increase enrollment of women in clinical trials and reports on gender-based differences, the cornerstone being the 1993 NIH Revitalization Act.37 Yet, one-quarter of large contemporary HF trials do not report variations in treatment response by gender.38 Our group previously recognized that women comprise only 28% of participants in contemporary HF trials published over the past 16 years.20 While women first and last authorship in medical research has been associated with a higher likelihood of sex-related reporting,39 ours is the first study to suggest an impact of women authorship on the inclusion of women as participants in clinical trials in HF.
The reasons for this finding are not well defined. Limited data regarding women’s participation in cardiovascular disease trials supporting new drug application approvals suggest that the lower number of women trial enrollees is due, in part, to the lower number of women referred for trial participation screening.40 Women authors may study conditions that affect women at a higher relative proportion. Interestingly, of the 4 trials focused on HF with preserved ejection fraction in our analysis, 3 had women as a first or senior author (Table 2). Women participants may be more likely to enroll in trials that they know are being conducted by women investigators. Women authors may be more likely to design trials in ways that are more accommodating to women participants. A multicenter randomized study of the relationship between gender and willingness to participate in cardiovascular prevention trials demonstrated that women perceive a greater risk of harm from trial participation and have lower willingness to participate but have less distrust of medical researchers compared with men.41
Our analyses show variation in women authorship by trial sponsor. Industry-funded trials have lower proportions of women authors per trial and fewer women as first or senior authors compared with those funded by other mechanisms. In surgical specialties, physicians with financial ties to industry have been shown to be more academically productive.42 Collaborating with industry sponsors may allow physicians increased opportunities for public speaking, networking, and participation in additional research partnerships. For investigators, research funding is a key component for academic promotion. Our findings may suggest a selection bias for men as leaders of industry-sponsored clinical trials, resulting in higher professional visibility, and career advancement gained through these opportunities and leaving women physicians at a disadvantage. The disparity of industry-sponsored funding represents a major gender-based barrier that necessitates attention.
Limitations
Limitations of this analysis should be considered. First, we were unable to assign gender to 1.3% of authors of guideline citations and 2% of authors of trials. Despite application of our algorithms for gender determination, misclassification may have occurred. We did not contact individual authors to determine self-identified gender and were unable to identify individuals with multiple or transgender identities. We were not able to identify co-first and co-senior authorships and were unable to quantify the contribution of each author to each publication. Second, professional and credentialing societies do not collect granular data regarding the numbers of women cardiologists in academic versus nonacademic positions; therefore, these proportions could not be classified. Third, we were unable to quantify the proportion of women entering the heart failure field over time. This is relevant because although recent US medical school classes have become increasingly gender balanced, the historical exclusion of women from medical training has likely contributed to a lag time resulting in fewer women now considered eligible for senior investigator roles. However, this lag time is unlikely to fully explain the persistent disparity in academic rank between women and men in medicine over the past 20 years, as women physicians are significantly less likely to be full professors despite adjustment for age, years since residency training, and measures of research and clinical productivity.10,43 Finally, the dearth of comprehensive demographic and longitudinal data regarding the international heart failure workforce limited our ability to fully contextualize gender disparities in this field. Dedicated inquiry into gender differences in heart failure research and practice is an important future step.
Conclusions
Our study demonstrates that women comprise <20% of the authorship of major international HF guideline citations and pivotal HF clinical trials, especially in key authorship positions. These data argue for broad-scale efforts to increase the numbers of women authors in clinical trials, consensus statements, and guidelines. Multiple stakeholders in the heart failure research enterprise must work in partnership to address these disparities in patient engagement and clinical research culture. The Heart Failure Collaboratory has begun outlining challenges and cultivating potential solutions.44 Our data should also encourage editorial boards, study sections, and promotions committees to prioritize the inclusion of women as editors, peer reviewers, and referees. Downstream benefits may include the development of experienced and accomplished women investigators and mentors in HF and increased enrollment of women in clinical trials. These changes should take place in conjunction with systematic, programmatic, and organizational agendas focused on increased diversity and inclusion, mentorship, and academic advancement for women.
Supplementary Material
WHAT IS NEW?
Despite the relatively higher number of women in advanced heart failure (HF) and transplant cardiology, fewer than 20% of the first authors of publications referenced in the Class I Recommendations of the United States and European HF guidelines are women, and fewer than 15% of the senior authors are women.
Of the 118 phase II–IV HF clinical trials published between 2001 and 2016 we examined, only 16% had a woman as a first or senior author.
Published clinical trials with higher proportions of women authors tended to have higher enrollments of female participants.
WHAT ARE THE CLINICAL IMPLICATIONS?
Proportions of women first and senior authors of HF trials have not significantly changed over the past 15 years, and concerted efforts to rectify these disparities should be made.
We confirm that HF research publications with women as first or senior authors more often have higher proportions of total women authors.
We identify women authorship of HF clinical trials as an important independent predictor of the enrollment of female participants.
Increasing the number of women as leaders of HF clinical trials may help reduce the underrepresentation of women as participants in HF clinical trials.
Acknowledgments
We thank the participants involved in the Heart Failure Collaboratory for their support in increasing diversity in heart failure research.
Sources of Funding
Dr Reza is supported by the National Institutes of Health National Human Genome Research Institute Ruth L. Kirschstein Institutional National Research Service T32 Award in Genomic Medicine (T32 HG009495).
Disclosures
Dr Vaduganathan is supported by the KL2/Catalyst Medical Research Investigator Training award from Harvard Catalyst (National Institutes of Health [NIH]/NCATS Award UL 1TR002541), serves on advisory boards for Amgen, AstraZeneca, Baxter Healthcare, Bayer AG, and Boehringer Ingelheim and participates on clinical end point committees for studies sponsored by Novartis and the NIH. Dr Greene is supported by a Heart Failure Society of America/Emergency Medicine Foundation Acute Heart Failure Young Investigator Award funded by Novartis, has received research support from Amgen, Bristol-Myers Squibb, and Novartis, and serves on an advisory board for Amgen. Dr Fonarow reports consulting for Abbott, Amgen, Bayer, CHF Solutions, Janssen, Medtronic, and Novartis.
Nonstandard Abbreviations and Acronyms
- ACC
American College of Cardiology
- AHA
American Heart Association
- ESC
European Society of Cardiology
- HF
heart failure
- IQR
interquartile range
- NIH
National Institutes of Health
Footnotes
The other authors report no conflicts.
This manuscript was sent to Kelly M. Chin, MD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCHEARTFAILURE.119.006605.
REFERENCES
- 1.Association of American Medical Colleges. 2017 Applicant and Matriculant Data Tables. 2017. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/5c/26/5c262575-52f9-4608-96d6a78cdaa4b203/2017_applicant_and_matriculant_data_tables.pdf Accessed July 5, 2019.
- 2.Burgess S, Shaw E, Ellenberger K, Thomas L, Grines C, Zaman S. Women in medicine: addressing the gender gap in interventional cardiology. J Am Coll Cardiol. 2018;72:2663–2667. doi: 10.1016/j.jacc.2018.08.2198 [DOI] [PubMed] [Google Scholar]
- 3.Data and Reports - Workforce - Data and Analysis 2008–2018 - AAMC https://www.aamc.org/data/workforce/reports/ Accessed July 5, 2019.
- 4.Modena MG, Lalla M, Molinari R. Determinants of career structure and advancement among Italian cardiologists. An example of segregation and discrimination against women? SCIC Group. Studio Condizione Italiana Cardiologi. Eur Heart J. 1999;20:1276–1284. doi: 10.1053/euhj.1999.1579 [DOI] [PubMed] [Google Scholar]
- 5.Andreotti F, Crea F. Women in cardiology: a European perspective. Heart. 2005;91:275–276. doi: 10.1136/hrt.2004.054593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Timmis AD, Baker C, Banerjee S, Calver AL, Dornhorst A, English KM, Flint J, Speechly-Dick ME, Turner D; Working Group of the British Cardiac Society. Women in UK cardiology: report of a Working Group of the British Cardiac Society. Heart. 2005;91:283–289. doi: 10.1136/hrt.2004.047340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeFilippis EM, Lau ES, Wei J, Hayes SN, Wood MJ. Where are the women in academic cardiology? Lancet. 2018;392:2152–2153. doi: 10.1016/S0140-6736(18)32618-7 [DOI] [PubMed] [Google Scholar]
- 8.ACGME Data Resource Book. https://www.acgme.org/About-Us/Publications-and-Resources/Graduate-Medical-Education-Data-Resource-Book Accessed June 27, 2019.
- 9.Baerlocher MO, Newton M, Gautam T, Tomlinson G, Detsky AS. The meaning of author order in medical research. J Investig Med. 2007;55:174–180. doi: 10.2310/6650.2007.06044 [DOI] [PubMed] [Google Scholar]
- 10.Blumenthal DM, Olenski AR, Yeh RW, DeFaria Yeh D, Sarma A, Stefanescu Schmidt AC, Wood MJ, Jena AB. Sex differences in faculty rank among academic cardiologists in the United States. Circulation. 2017;135: 506–517. doi: 10.1161/CIRCULATIONAHA.116.023520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lerchenmüller C, Lerchenmueller MJ, Sorenson O. Long-term analysis of sex differences in prestigious authorships in cardiovascular research supported by the National Institutes of Health. Circulation. 2018;137:880–882. doi: 10.1161/CIRCULATIONAHA.117.032325 [DOI] [PubMed] [Google Scholar]
- 12.Albert MA. #Me_who anatomy of scholastic, leadership, and social isolation of underrepresented minority women in academic medicine. Circulation. 2018;138:451–454. doi: 10.1161/CIRCULATIONAHA.118.035057 [DOI] [PubMed] [Google Scholar]
- 13.Data and Analysis - AAMC. https://www.aamc.org/data/493922/reporton-residents-2018-b3table.html Accessed July 5, 2019.
- 14.Crespo-Leiro MG. Heart failure is taking center stage. Circ Heart Fail. 2019;12:e006025. doi: 10.1161/CIRCHEARTFAILURE.119.006025 [DOI] [PubMed] [Google Scholar]
- 15.Moayedi Y, Hershman SG, Ross HJ, Khush KK, Teuteberg JJ. Perceived generational, geographic, and sex-based differences in choosing a career in advanced heart failure. Circ Heart Fail. 2019;12:e005754. doi: 10.1161/CIRCHEARTFAILURE.118.005754 [DOI] [PubMed] [Google Scholar]
- 16.Heart Failure Collaboratory https://www.hfcollaboratory.com/ Accessed August 2019.
- 17.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, et al. ; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–e327. doi: 10.1161/CIR.0b013e31829e8776 [DOI] [PubMed] [Google Scholar]
- 18.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Colvin MM, Drazner MH, Filippatos GS, Fonarow GC, Givertz MM, et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2017;136:e137–e161. doi: 10.1161/CIR.0000000000000509 [DOI] [PubMed] [Google Scholar]
- 19.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, et al. ; Authors/Task Force Members; Document Reviewers. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016;18:891–975. doi: 10.1002/ejhf.592 [DOI] [PubMed] [Google Scholar]
- 20.Tahhan AS, Vaduganathan M, Greene SJ, Fonarow GC, Fiuzat M, Jessup M, Lindenfeld J, O’Connor CM, Butler J. Enrollment of older patients, women, and racial and ethnic minorities in Contemporary Heart Failure Clinical Trials: a systematic review. JAMA Cardiol. 2018;3:1011–1019. doi: 10.1001/jamacardio.2018.2559 [DOI] [PubMed] [Google Scholar]
- 21.Smith B Genderize.io | Determine the gender of a first name. https://genderize.io/ Accessed May 28, 2019.
- 22.Hart KL, Perlis RH. Trends in proportion of women as authors of medical journal articles, 2008–2018. JAMA Intern Med. 2019;179:1285–1287. doi: 10.1001/jamainternmed.2019.0907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Douglas PS, Williams KA Sr, Walsh MN. Diversity matters. J Am Coll Cardiol. 2017;70:1525–1529. doi: 10.1016/j.jacc.2017.08.003 [DOI] [PubMed] [Google Scholar]
- 24.Physician and Other Supplier Data CY 2016 - Centers for Medi-care & Medicaid Services [Internet]. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Provider-Charge-Data/Physician-and-Other-Supplier2016.html Accessed July 16, 2019.
- 25.Khan MS, Usman MS, Fatima K, Hashmani N, Siddiqi TJ, Riaz H, Khan AR, Khosa F. Characteristics of highly cited articles in interventional cardiology. Am J Cardiol. 2017;120:2100–2109. doi: 10.1016/j.amjcard.2017.08.030 [DOI] [PubMed] [Google Scholar]
- 26.Ouyang D, Sing D, Shah S, Hu J, Duvernoy C, Harrington RA, Rodriguez F. Sex disparities in authorship order of cardiology scientific publications. Circ Cardiovasc Qual Outcomes. 2018;11:e005040. doi: 10.1161/CIRCOUTCOMES.118.005040 [DOI] [PubMed] [Google Scholar]
- 27.Ouyang D, Harrington RA, Rodriguez F. Association between female corresponding authors and female co-authors in top contemporary cardiovascular medicine journals. Circulation. 2019;139:1127–1129. doi: 10.1161/CIRCULATIONAHA.118.037763 [DOI] [PubMed] [Google Scholar]
- 28.Asghar M, Usman MS, Aibani R, Ansari HT, Siddiqi TJ, Fatima K, Khan MS, Figueredo VM. Sex differences in authorship of academic cardiology literature over the last 2 decades. J Am Coll Cardiol. 2018;72:681–685. doi: 10.1016/j.jacc.2018.05.047 [DOI] [PubMed] [Google Scholar]
- 29.Wenneras C, Wold A. Nepotism and sexism in peer-review. Nature. 1997;387:341–343. doi: 10.1038/387341a0 [DOI] [PubMed] [Google Scholar]
- 30.Kaatz A, Gutierrez B, Carnes M. Threats to objectivity in peer review: the case of gender. Trends Pharmacol Sci. 2014;35:371–373. doi: 10.1016/j.tips.2014.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hitchcock MA, Bland CJ, Hekelman FP, Blumenthal MG. Professional networks: the influence of colleagues on the academic success of faculty. Acad Med. 1995;70:1108–1116. doi: 10.1097/00001888-199512000-00013 [DOI] [PubMed] [Google Scholar]
- 32.Fox MF. Women, science, and academia: graduate education and careers. Gender & Society. 2001;15:654–666. [Google Scholar]
- 33.Babcock L, Laschever S. Women Don’t Ask: Negotiation and the Gender Divide. Princeton, New Jersey: Princeton University Press; 2003. [Google Scholar]
- 34.Witteman HO, Hendricks M, Straus S, Tannenbaum C. Are gender gaps due to evaluations of or the science? A natural experiment at a national the applicant funding agency. Lancet. 2019;393:531–540. doi: 10.1016/S0140-6736(18)32611-4 [DOI] [PubMed] [Google Scholar]
- 35.Douglas PS, Rzeszut AK, Bairey Merz CN, Duvernoy CS, Lewis SJ, Walsh MN, Gillam L; American College of Cardiology Task Force on Diversity and Inclusion and American College of Cardiology Women in Cardiology Council. Career preferences and perceptions of cardiology among US internal medicine trainees: factors influencing cardiology career choice. JAMA Cardiol. 2018;3:682–691. doi: 10.1001/jamacardio.2018.1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Melloni C, Berger JS, Wang TY, Gunes F, Stebbins A, Pieper KS, Dolor RJ, Douglas PS, Mark DB, Newby LK. Representation of women in randomized clinical trials of cardiovascular disease prevention. Circ Cardiovasc Qual Outcomes. 2010;3:135–142. doi: 10.1161/CIRCOUTCOMES.110.868307 [DOI] [PubMed] [Google Scholar]
- 37.Mazure CM, Jones DP. Twenty years and still counting: including women as participants and studying sex and gender in biomedical research. BMC Womens Health. 2015;15:94. doi: 10.1186/s12905-015-0251-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vaduganathan M, Tahhan AS, Alrohaibani A, Greene SJ, Fonarow GC, Vardeny O, Lindenfeld J, Jessup M, Fiuzat M, O’Connor CM, et al. Do women and men respond similarly to therapies in contemporary heart failure clinical trials? JACC Heart Fail. 2019;7:267–271. doi: 10.1016/j.jchf.2018.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sugimoto CR, Ahn YY, Smith E, Macaluso B, Larivière V. Factors affecting sex-related reporting in medical research: a cross-disciplinary bibliometric analysis. Lancet. 2019;393:550–559. doi: 10.1016/S0140-6736(18)32995-7 [DOI] [PubMed] [Google Scholar]
- 40.Scott PE, Unger EF, Jenkins MR, Southworth MR, McDowell TY, Geller RJ, Elahi M, Temple RJ, Woodcock J. Participation of women in clinical trials supporting FDA approval of cardiovascular drugs. J Am Coll Cardiol. 2018;71:1960–1969. doi: 10.1016/j.jacc.2018.02.070 [DOI] [PubMed] [Google Scholar]
- 41.Ding EL, Powe NR, Manson JE, Sherber NS, Braunstein JB. Sex differences in perceived risks, distrust, and willingness to participate in clinical trials: a randomized study of cardiovascular prevention trials. Arch Intern Med. 2007;167:905–912. doi: 10.1001/archinte.167.9.905 [DOI] [PubMed] [Google Scholar]
- 42.Ngaage LM, Harris C, Gao C, Puthumana J, Crabill GA, Baglien B, Wu Y, Rosen C, Rada EM, Groves M, et al. Investigating the gender pay gap in industry contributions to academic neurosurgeons. World Neurosurg. 2019;130:516–522.e1. doi: 10.1016/j.wneu.2019.06.145 [DOI] [PubMed] [Google Scholar]
- 43.Jena AB, Khullar D, Ho O, Olenski AR, Blumenthal DM. Sex differences in academic rank in US Medical Schools in 2014. JAMA. 2015;314:1149–1158. doi: 10.1001/jama.2015.10680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O’Connor CM, Psotka MA, Fiuzat M, Lindenfeld J, Abraham WT, Bristow MR, Canos D, Harrington RA, Hillebrenner M, Jessup M, et al. Improving heart failure therapeutics development in the United States: the Heart Failure Collaboratory. J Am Coll Cardiol. 2018;71:443–453. doi: 10.1016/j.jacc.2017.11.048 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.