Abstract
Failure to address hypertension among people living with HIV (PLWH) may undermine the significant progress made toward reducing mortality among this high‐risk population in sub‐Saharan Africa (SSA). Here, the authors report hypertension prevalence, diagnosis, and treatment among patients enrolled in HIV care in Tanzania. Patients attending an HIV clinic were consecutively screened for hypertension. Hypertension was defined as follows: a single blood pressure measurement ≥160 mm Hg systolic or ≥100 mm Hg diastolic, two measurements at separate visits ≥140 mm Hg systolic or ≥90 mm Hg diastolic, or self‐reported hypertension diagnosis. The authors screened 555 patients, and 19.6% met hypertension criteria. Among a subset of 91 hypertensive participants, 44 (48.4%) reported previous blood pressure measurements, 32 (35.2%) were aware of diagnosis, 10 (11.0%) reported current antihypertensive use, and none had controlled blood pressure. Addressing barriers along the hypertension treatment cascade must be a top priority to improve cardiovascular outcomes among PLWH in SSA.
Keywords: high blood pressure, HIV, hypertension, Sub‐Saharan Africa, Tanzania
1. INTRODUCTION
Sub‐Saharan Africa (SSA) has the highest prevalence of hypertension in the world 1 ; however, inadequacies exist throughout the hypertension treatment cascade, which includes the screening, diagnosis, treatment, and control of hypertension. 2 Although data are limited, evidence suggests that hypertension prevalence among people living with HIV (PLWH) in SSA is approaching that of uninfected persons. 3 As hypertension is the leading risk for death worldwide this is of great concern. 4
While mortality among PLWH in SSA has declined significantly since the scale‐up of antiretroviral therapy, 5 this progress is now challenged by an increasing prevalence of non‐communicable diseases (NCDs), including hypertension and its associated cardiovascular comorbidity. 6 Failure to address hypertension may undermine the tremendous progress and efforts made toward reducing mortality among PLWH in SSA.
Understanding epidemiologic patterns of hypertension among PLWH in SSA is a critical first step for developing strategies to improve cardiovascular outcomes among this high‐risk population. Here, we report hypertension prevalence among a cohort of patients with HIV in northern Tanzania and describe patterns of hypertension awareness, treatment, and control.
2. METHODS
2.1. Study population
The study was conducted from October 16, 2018, through December 10, 2018, in Moshi, Tanzania, in a single government HIV clinic, which serves ~1200 adults (900 women and 300 men) with HIV per year. Individuals were eligible to participate whether over 18 years of age, not pregnant, and seeking HIV care at the study site. During routine HIV appointments, all patients were introduced to the study nurse by a member of the clinical staff and invited to be screened for hypertension.
2.2. Procedures
Screening for hypertension was conducted by the study nurse in a private room within the HIV clinic. All screened participants had height and weight measured, and completed a short demographic survey. Participants who met hypertension criteria were invited to consent for an additional survey, which included questions about previous hypertension history.
2.3. Measures
2.3.1. Hypertension
Blood pressure was measured twice in the right arm per the International Society of Hypertension guidelines, 7 with at least a 5‐minute interval between measures using an FDA approved automatic blood pressure monitor (Omron Healthcare) with an adult‐sized adjustable arm cuff. The blood pressure monitor was calibrated monthly. If at least one of two measurements was ≥140 mm Hg systolic or ≥90 mm Hg diastolic, the participant was invited to return to the clinic within one to 2 weeks for repeat blood pressure measurements.
Hypertension was defined as meeting any of the following criteria: (a) self‐reported diagnosis of hypertension, (b) a single blood pressure measurement ≥160 mm Hg systolic or ≥100 mm Hg diastolic, or (c) two measurements at separate visits obtained at least one week apart ≥140 mm Hg systolic or ≥90 mm Hg diastolic.
Blood pressure was further categorized by the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure VII (JNC‐VII) guidelines 8 based on the average of the two blood pressure measurements obtained at the initial visit for all screened participants.
2.3.2. Hypertension treatment cascade
All participants were asked about any previous blood pressure assessments. Participants who met hypertension criteria were asked if they had ever been told they had high blood pressure, if they had ever been prescribed medication for high blood pressure, and if they were currently using medication for high blood pressure. Hypertension control was identified if all blood pressure measurements obtained by the study nurse were <140 mm Hg systolic and <90 mm Hg diastolic.
2.4. Data analysis
To examine hypertension prevalence, the proportion of all screened participants who met hypertension study criteria was determined. Participants who did not meet hypertension criteria at the initial visit but had a blood pressure measurement between 140 and 159 mm Hg systolic or 90 to 99 mm Hg diastolic and did not return for a repeat blood pressure measurement were excluded from the hypertension prevalence calculation. Continuous variables were expressed using the median and interquartile range (IQR). Categorical variables were expressed as frequencies. Data were analyzed using STATA version 16.0 (STATA Corp.).
2.5. Ethics
This study was approved by the Duke Health Institutional Review Board, the Kilimanjaro Christian Medical University College Ethics Committee, and the Tanzania National Institute for Medical Research Ethics Committee.
3. RESULTS
3.1. Participant characteristics
Over an 8‐week period, a total of 806 patients attended the HIV clinic, and 555 were screened for hypertension. The majority of screened participants were women (n = 436, 78.6%), with no observed association between sex and hypertension. Most participants had no more than a primary level school of education (n = 433, 79.4%). The median age of participants with hypertension was 50 (IQR 43‐57) years, compared to 42 (IQR 35‐49) years for normotensive participants. The median body mass index among participants with hypertension was 27 (IQR 24‐30), compared to 23 (IQR 20‐27) among normotensive participants.
3.2. Hypertension prevalence
Among the 555 participants screened, 74 met hypertension criteria at the initial visit and 31 met hypertension criteria at the second visit, making a total of 105 participants meeting hypertension criteria (Figure 1). Hypertension prevalence was 19.6% (20.3% among women and 16.8% among men).
FIGURE 1.
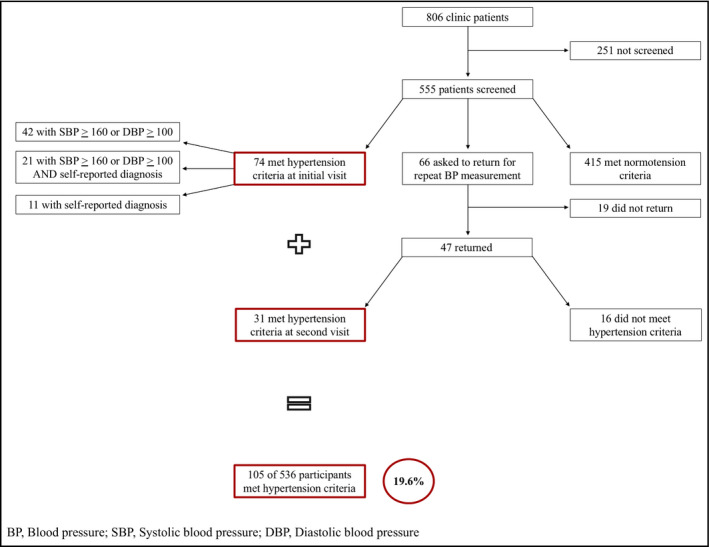
Flowchart describing hypertension screening and prevalence in an HIV treatment clinic in northern Tanzania, 2018
Using JNC‐VII categorization of hypertension, among all participants screened, 167 (30.3%) had prehypertension, 70 (12.7%) had stage I hypertension, and 42 (7.6%) had stage II hypertension.
3.3. Hypertension treatment cascade
Of the 555 screened participants, 226 (40.7%) reported prior blood pressure measurements. Among the participants who had prior blood pressure measurements, 68 (30.7%) reported having only one previous blood pressure measurement. The most frequent location for measuring blood pressure was an outpatient department (n = 123, 56.7%). Only 26 (11.5%) participants had ever had their blood pressure measured in the HIV clinic.
Of the 105 participants who met hypertension criteria, 91 consented to answer questions about hypertension history. Among these, 44 (48.4%) reported having a previous blood pressure measurement, 32 (35.2%) were aware of their hypertension diagnosis, 21 (23.1%) reported ever receiving antihypertensive drugs, 10 (11.0%) reported current antihypertensive use, and none had a controlled blood pressure (Figure 2).
FIGURE 2.
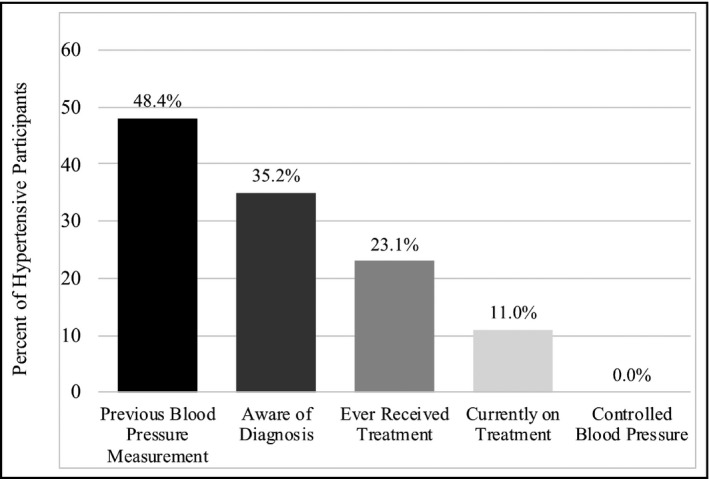
Hypertension treatment cascade among hypertensive participants attending an HIV treatment clinic in northern Tanzania, 2018 (n = 91)
4. DISCUSSION
This study identified a high prevalence of hypertension among a cohort of patients enrolled in HIV care in northern Tanzania. Yet, screening, treatment, and control were low. Our findings suggest that challenges across the hypertension treatment cascade lead to a high burden of uncontrolled hypertension, and may seriously undermine significant progress made toward reducing mortality among PLWH in SSA.
Hypertension prevalence among adults with HIV in the Kilimanjaro region was high (20% using our study criteria). Furthermore, approximately a third of all participants were categorized as pre‐hypertensive in our study. This is incredibly concerning as both pre‐hypertension and hypertension significantly increase the risk for cardiovascular mortality. 4 , 9 As people with HIV continue to age, 10 and trends toward urbanization and associated unhealthy lifestyle behaviors increase in SSA, the traditional risk factors associated with prehypertension and hypertension will almost certainly rise. 6 The growing burden of pre‐hypertension, hypertension, and associated cardiovascular co‐morbidities among PLWH will be a formidable challenge in SSA if not promptly addressed.
The data from this study shed light on the gaps in the hypertension treatment cascade. The proportion of hypertensive individuals who previously had their blood pressure measured and who were aware of their diagnosis, treated. and controlled was unacceptably low. This lack of awareness and ineffective hypertension treatment is similar to findings from other studies in SSA. 2 , 11 Furthermore, only a few patients in our study reported having their blood pressure measured in the HIV clinic. In a previous study examining barriers faced by patients with HIV and hypertension in northern Tanzania, participants reported they did not discuss blood pressure with their HIV providers, and hypertension was often not addressed at all in the HIV clinic (P. Manavalan, L. Minja, L. Wanda, et al, unpublished results). However, the HIV clinic could be leveraged to fully integrate hypertension care into routine HIV appointments. The response to the HIV epidemic prompted the first large chronic disease program in SSA, and HIV clinics now serve as potential platforms for health systems strengthening beyond HIV. 12 , 13 , 14 People engaged in HIV care in SSA routinely attend dedicated HIV clinics that serve PLWH. HIV appointments could be further utilized for hypertension screening and long‐term management to improve outcomes along the hypertension treatment cascade. 12
Our study had several limitations. Notably, this study was conducted in one HIV clinic in an urban area in northern Tanzania. Thus, our findings may not be generalizable to other settings in SSA. In addition, there may have been some selection bias as we were only able to screen 555 of the 806 patients who attended the HIV clinic. However, our screening methods attempted to reduce selection bias by screening consecutive patients on all clinic days.
In conclusion, hypertension is prevalent among adults with HIV in northern Tanzania. Despite this high burden of disease, rates of screening, awareness, treatment, and control are alarmingly low. High‐quality, evidence‐based interventions that address challenges along the hypertension treatment cascade in SSA must be a top priority. The HIV clinic in SSA represents a unique opportunity to engage patients in hypertension care and should be leveraged to improve the delivery of NCD services among PLWH.
CONFLICTS OF INTEREST
The authors declare that they have no conflict of interests.
AUTHORS CONTRIBUTIONS
PM, NMT, and MHW conceived the study; PM, NMT, NLO, and MHW designed the study protocol; PM, BTM, and MHW implemented and supervised the study; PM and DBM performed the data analysis; PM drafted the manuscript; PM, DBM, JTH, NMT, NLO, BTM, and MHW critically revised the manuscript for content. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
We would like to thank all the staff of the Duke‐Kilimanjaro Christian Medical Centre collaboration, Kilimanjaro Clinical Research Institute, and Majengo Health Centre for their support and efforts. We appreciate support from the Duke Global Health Institute and the Duke Hubert Yeargan Center for Global Health. We give special thanks to Pilli Nyindo for her support in recruitment and data collection. We would like to thank all the patients who participated in our study.
Manavalan P, Madut DB, Hertz JT, et al. Hypertension burden and challenges across the hypertension treatment cascade among adults enrolled in HIV care in northern Tanzania. J Clin Hypertens. 2020;22:1518–1522. 10.1111/jch.13929
Funding information
This study received support from the US National Institutes of Health Fogarty International Center (grant number D43TW009337) and from the National Institutes of Health Ruth L. Kirschstein National Research Service Award (grant number 5T32AI007392). We appreciate support from the Duke Center for AIDS Research (grant number P30AI064518).
REFERENCES
- 1. WHO . Raised blood pressure. WHO. https://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/. Accessed November 7, 2019 [Google Scholar]
- 2. Geldsetzer P, Manne‐Goehler J, Marcus M‐E, et al. The state of hypertension care in 44 low‐income and middle‐income countries: a cross‐sectional study of nationally representative individual‐level data from 1·1 million adults. Lancet. 2019;394(10199):652‐662. 10.1016/S0140-6736(19)30955-9 [DOI] [PubMed] [Google Scholar]
- 3. Xu Y, Chen X, Wang K. Global prevalence of hypertension among people living with HIV: a systematic review and meta‐analysis. J Am Soc Hypertens. 2017;11(8):530‐540. 10.1016/j.jash.2017.06.004 [DOI] [PubMed] [Google Scholar]
- 4. GBD 2017 Risk Factor Collaborators . Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923‐1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. GBD 2017 HIV collaborators . Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV. 2019;6(12):e831–e859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Patel P, Rose CE, Collins PY, et al. Noncommunicable diseases among HIV‐infected persons in low‐income and middle‐income countries: a systematic review and meta‐analysis. AIDS. 2018;32(Suppl 1):S5‐S20. 10.1097/QAD.0000000000001888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community. J Clin Hypertens. 2014;16(1):14‐26. 10.1111/jch.12237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560‐2572. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 9. Huang Y, Su L, Cai X, et al. Association of all‐cause and cardiovascular mortality with prehypertension: a meta‐analysis. Am Heart J. 2014;167(2):160‐168.e1. 10.1016/j.ahj.2013.10.023 [DOI] [PubMed] [Google Scholar]
- 10. HIV and Aging. https://www.unaids.org/en/resources/documents/2013/20131101_JC2563_hiv‐and‐aging. Accessed January 20, 2020.
- 11. Peck RN, Shedafa R, Kalluvya S, et al. Hypertension, kidney disease, HIV and antiretroviral therapy among Tanzanian adults: a cross‐sectional study. BMC Med. 2014;12:125. 10.1186/s12916-014-0125-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chronic care of HIV and noncommunicable diseases: how to leverage the HIV experience. https://www.unaids.org/en/resources/documents/2011/20110526_JC2145_Chronic_care_of_HIV. Accessed November 22, 2019.
- 13. Letebo M, Shiferaw F. Adapting HIV patient and program monitoring tools for chronic non‐communicable diseases in Ethiopia. Global Health. 2016;12:26. 10.1186/s12992-016-0163-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Patel P, Speight C, Maida A, et al. Integrating HIV and hypertension management in low‐resource settings: Lessons from Malawi. PLoS Med. 2018;15(3):e1002523. 10.1371/journal.pmed.1002523 [DOI] [PMC free article] [PubMed] [Google Scholar]


