Abstract
Many Black men suffer symptoms of traumatic stress in the aftermath of traumatic injury, and they also often carry social concerns, including experiences of discrimination and stigma and a lack of financial resources. The objective of the present study was to understand how traumatic symptoms and social factors combine in complex ways toward the outcome of psychological help-seeking. We analyzed qualitative and quantitative data from 32 injured Black men admitted to a Level 1 trauma center. Qualitative interviews explored their attitudes toward seeking professional psychological help. We analyzed quantitative data, collected using validated instruments, on posttraumatic stress and depression symptoms, financial worry, and discrimination/stigma. Fuzzy-set qualitative comparative analysis (fsQCA) was conducted by calibrating each condition to fuzzy-set membership scores based on our knowledge of the causal conditions and the cases. We then constructed truth tables for QCA analysis using fsQCA software. Three causal pathways for psychological help-seeking were identified: Two pathways showed that severe trauma symptoms in the absence of financial worry were sufficient for seeking help, whereas the third showed that financial worry and discrimination in the absence of trauma symptoms were sufficient for help-seeking. We identified two causal pathways for negated help-seeking, in which low posttraumatic symptom severity and low levels of discrimination or financial worry were sufficient for not seeking psychological help. The QCA analysis revealed multiple pathways for psychological help-seeking among Black men who suffer trauma. These findings highlight the need for further research to understand complex pathways toward psychological help-seeking in this population.
Survivors of traumatic injury frequently experience psychological symptoms. Studies of hospitalized survivors of intentional and unintentional injury have found that up to 56% of these individuals suffer from posttraumatic stress disorder (PTSD; Vles et al., 2005; Zatzick et al., 2004; Zatzick, Russo, & Katon, 2003) and up to 31% experience depression (Holbrook, Anderson, Sieber, Browner, & Hoyt, 1998). These symptoms can persist beyond the period of physical recovery and are associated with significant disability in the year following injury (Richmond et al., 2009; Richmond, Kauder, Hinkle, & Shults, 2003). Although injury survivors are routinely referred for physical rehabilitation consistent with the severity of their physical wounds, evaluation and referral for psychological symptoms is often inconsistent or lacking altogether, leaving survivors with few alternatives for professional psychological support.
Despite their significant needs, underserved populations often have limited access to behavioral health care. In particular, urban victims of trauma and violence, such as Black men, frequently lack access to behavioral health services in the aftermath of an injury (Jiang, Webster, Robinson, Kassam-Adams, & Richmond, 2018; Savage et al., 2016). These patients have high rates of trauma-related symptoms that often meet the criteria for PTSD and depression (Corbin et al., 2013; Rich & Grey, 2005). Past studies have demonstrated that the use of behavioral health services may be facilitated among individuals with more severe symptoms of traumatic stress and those who have stable housing and employment (Alvidrez et al., 2008). Barriers to the use of behavioral health services include fear of stigma, difficulty expressing concerns, a preference for self-reliance, and difficulty accessing health care due to financial costs (Kantor, Knefel, & Lueger-Schuster, 2017; Salaheddin & Mason, 2016). Because of these barriers, many trauma survivors do not seek professional behavioral health care and instead rely on informal or alternative sources of care.
In a recent qualitative analysis, we explored how 32 Black male survivors of trauma articulated the factors that facilitated or hindered their help-seeking for psychological symptoms after injury (Jacoby, Rich, Webster, & Richmond, 2018). The study, which was embedded in a large mixed-methods, prospective cohort study of the psychological effects of traumatic injuries in urban Black men, explored the men’s experiences with and perceptions of help-seeking for psychological symptoms after injury. Several themes related to psychological help-seeking emerged from our analyses. Overall, men’s perceptions that their symptoms of PTSD and depression were severe and persistent facilitated help-seeking for psychological symptoms among those who expressed interest in professional mental health care. On the other hand, themes related to stigma (i.e., being viewed as “crazy”), racial discrimination, limited financial resources, and lack of access to health insurance were key barriers described by men who expressed disinterest in seeking psychological help. For some participants, the burden of multiple needs predisposed them to seeking help, whereas for others, these same factors posed barriers.
The aim of the present analysis was to explore, using both qualitative and quantitative data from a study of urban, Black, male trauma survivors, how symptoms of PTSD and depression may act together with discrimination, stigma, and financial stressors to either hinder or facilitate psychological help-seeking. Given past insights gleaned from qualitative studies of help-seeking behaviors in injured Black men, we hypothesized that these conditions combine in complex ways that either facilitate or hinder help-seeking and do so differently for different individuals. This question was difficult to explore through descriptive qualitative analysis alone or through traditional correlational approaches to quantitative data, which are designed to detect net effects using probabilistic methods. To better understand help-seeking among Black male survivors of traumatic injury, we applied qualitative comparative analysis (QCA), a set-theoretic analytic method that uses Boolean algebra to compare combinations of causal and outcome conditions between cases. Unlike correlational approaches that pay attention to net effects and estimating each variable’s separate impact on an outcome, QCA assumes combinations of conditions as the analytical starting point (Ragin & Fiss, 2017) and can help to identify patterns in the empirical data under circumstances in which correlational methods would be limited by the small number of cases (Haynes et al., 2017).
The QCA method uses the foundational concepts of set theory to unravel complex causation. There are several qualities that set QCA apart from other analytic approaches. One of the most important is equifinality, the concept that more than one combination of causal conditions can produce the same outcome. Another key characteristic of QCA is asymmetry: The combinations of conditions that make up the causal pathways that lead to the occurrence of an outcome, sometimes termed “causal recipes,” are not the exact opposite of the combinations that lead to the nonoccurrence of the outcome (Ragin, 2014; Schneider & Wagemann, 2012).
The “truth table” is core to the QCA analysis of whether a combination of conditions is sufficient to produce an outcome. The truth table displays all logically possible combinations of the causal conditions, then assigns each case to the truth table row of which it is a set member. Through a process called logical minimization, the rows are compared and reduced using Boolean algebra to produce the most simplified solutions, which express those combinations of the causal conditions that are sufficient to consistently produce the outcome.
The QCA method is well suited for identifying complex causal pathways in the association between injury and psychological help-seeking for Black men and can be used to identify multiple causal pathways to explain how facilitators or barriers may combine in complex ways for different groups of Black men. It is an emerging analytic approach that is often applied in social sciences research and has shown promising applications to complex problems in clinical and public health research. In particular, QCA is useful in exploring inequalities that entail the intersection of causal conditions such as race, gender, discrimination, poverty, and structural inequities (Fiss, Marx, & Cambré, 2013; Haynes et al., 2017; Spangaro et al., 2016; Walia, Belludi, Kulkarni, Darak, & Swamy, 2016)
Method
Participants
Potential participants for the present analysis were drawn from a cohort of 335 Black men admitted to a regional level 1 trauma center in Philadelphia, Pennsylvania, a large city in northeastern United States, who had a diagnosis of injury, were consecutively recruited between January 2013 and June 2015, and completed a 3-month follow-up interview. A sample of 75 of these participants was selected to participate in an in-depth qualitative interview. Qualitative analysis of the interviews was conducted to examine themes related to help-seeking for psychological symptoms. The research team identified content on help-seeking in 32 interviews, and these cases were included in the present study. Figure 1 displays the flow diagram for participants.
Figure 1.
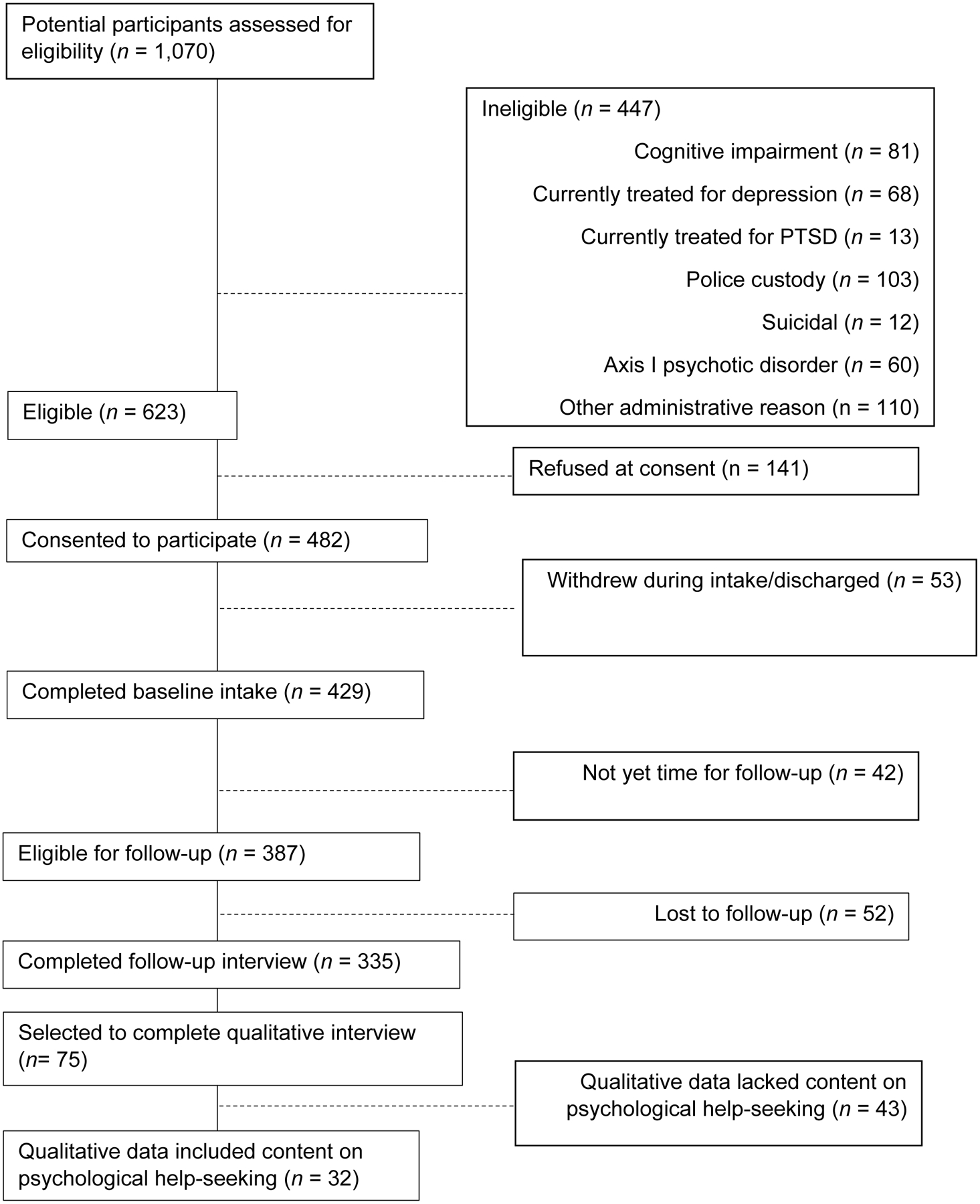
Participant flow diagram. PTSD = posttraumatic stress disorder
To be eligible for inclusion, patients needed to identify as male and Black, reside within the greater Philadelphia metropolitan area, and be hospitalized for an acute traumatic injury. Patients were excluded if they had a preexisting mental status dysfunction, central nervous system injury, or acute psychotic disorder, or if they were currently being treated for PTSD and/or depression. A registered nurse screened all potential participants to determine if their level of consciousness, current mental status, or history of mental health diagnoses would render them ineligible to consent to study participation. Participants with drug and alcohol abuse were excluded unless they had evidence of psychosis.
Selected characteristics of study participants are shown in Table 1. There were no significant differences between the 32 participants included in this QCA analysis and the 43 other participants who were randomly selected for qualitative interviews on measures of age (M age: 38.83 years vs. 37.33 years, p = .669, intentional injury (65.6% vs. 58.1%, p = .514), PTSD symptoms (M Posttraumatic Stress Disorder Checklist for DSM-5 [PCL-5] score: 36.45 vs. 28.86 p = .111), depression symptoms (M Quick Inventory of Depressive Symptomatology [QIDS] score: 12.81 vs. 10.40, p = .111), discrimination/stigma (M Perceived Ethnic Discrimination Questionnaire [PEDQ-CV] score: 37.51 vs. 37.50, p = .996), or financial worry (M score: 3.13 vs. 3.56, p = .282). There were a number of significant differences between the 32 participants in this analysis and the other 303 participants who completed the 3 month follow-up interview, with current participants showing higher levels of PTSD symptoms (M PCL-5 score 36.45 vs. 22.90, p < .001) and depression symptoms (M QIDS score: 12.81 vs. 8.45, p < .001) and more financial worry (M score: 3.13 vs. 3.90, p = .008); there were no significant differences in age (M = 38.84 years vs. 36.68, p = .455), intentional injury (65.6% vs. 49.5%, p = .084), or discrimination and stigma (M PEDQ-CV score: 37.51 vs. 32.77, p = .056). Among the 32 participants in the present study, there were no significant differences between those who suffered intentional and unintentional injuries, respectively, with regard to depression symptoms (M QIDS score: 13.29 vs. 11.91, p = .580) or PTSD symptoms (M PCL-5 score: 37.67 vs. 33.45, p = .569.)
Table 1.
Participant Characteristics
| Characteristic | % | n | M | SD |
|---|---|---|---|---|
| Type of injury | ||||
| Intentional | 65.6 | 21 | ||
| Unintentional | 34.4 | 11 | ||
| Age (years) | 38.70 | 14.26 | ||
| PTSD score (PCL-5) | 36.22 | 19.46 | ||
| Score < 33 | 46.9 | 15 | ||
| Score ≥ 33a | 53.1 | 17 | ||
| Depression score (QIDS) | 12.81 | 6.54 | ||
| 0–5 (no depression) | 15.6 | 5 | ||
| 6–10 (mild depression) | 18.8 | 6 | ||
| 11–15 (moderate depression) | 25.0 | 8 | ||
| 16–20 (severe depression) | 28.1 | 9 | ||
| 21–27 (very severe depression) | 12.5 | 4 | ||
| Financial worry scoreb | 3.13 | 1.81 | ||
| 1 (always) | 34.3 | 11 | ||
| 2 (usually) | 9.4 | 3 | ||
| 3 (sometimes) | 6.3 | 2 | ||
| 4 (rarely) | 9.4 | 3 | ||
| 5 (never) | 40.6 | 13 | ||
| Discrimination Score (PEDQ) | 37.61 | 13.19 |
Note. N = 32. PTSD = posttraumatic stress disorder; PCL-5 = PTSD Checklist for DSM-5; QIDS = Quick Inventory of Depressive Symptomatology; PEDQ-CV = Perceived Ethnic Discrimination Questionnaire–Community Version.
Provisional PTSD.
Participans were asked “How many times in the past 12 months were you worried or stressed about paying your rent?”
Procedure
The study protocol was approved by the institutional review board of the Hospital University of Pennsylvania. The purpose and procedures of the study were explained to eligible patients who met inclusion criteria; patients who agreed signed an informed consent form. All interviews were conducted by trained research staff. Participants were interviewed in a private room in the hospital for their initial interviews, which included a number of survey items capturing demographic characteristics, injury descriptors, assessments of acute stress symptoms, and subjective experiences surrounding the injury. Participants were interviewed again 3 months after hospital discharge. The second interview included assessments of traumatic stress symptoms, depression symptoms, discrimination and stigma, and financial worry. The second interview also included a semistructured interview, which explored participants’ experiences after their injury as well as the aspects of their experiences they felt enhanced or impaired their recovery. Consistent with qualitative research best practices, the interview guide was not static but rather evolved to incorporate themes that emerged during early interviews, which could then be explored in subsequent interviews (Dowding, 2013). One such concept was help-seeking for psychological symptoms or distress after injury. If a participant indicated that he was experiencing any emotional distress and was willing to talk about it, narratives about seeking psychological help were elicited with the question: “Has there ever been a time when you’ve considered talking to a professional about these experiences [referring to emotional distress and psychological symptoms]?” Participants were also asked about barriers to help-seeking as well as which characteristics of care providers, healthcare settings, and financial and/or logistical access that they regarded as most helpful. Interviews were digitally recorded and transcribed verbatim using standardized transcription rules. Names and other personal identifiers were removed to protect participants’ anonymity.
Interview data were analyzed using both thematic and structural narrative analysis. Members of the research team independently reviewed all 32 interview transcripts to identify codes and themes related to help-seeking. The research team first categorized the interview data based on how the narrative showed help-seeking intent (i.e., whether the participant would or would not consider seeing a professional after injury). For cases in which team members had coded content differently, the team discussed different themes and came to a group consensus about the final coding. The team then analyzed the interviews to identify and describe the underlying facilitators and barriers to help-seeking intent. Similar to, but distinct from, qualitative content analysis, in which rigor is often measured through interrater reliability or interrater agreement, in a thematic analytic approach, reliability and analytic rigor are evaluated and interpreted through debriefing, researcher triangulation, and consensus-building discussion (Fereday & Muir-Cochrane, 2006; Nowell, Norris, White, & Moules, 2017). Qualitative data were analyzed using NVivo (Version 10; QSR International, 2014).
Measures
Demographic and injury-related characteristics.
Demographic and injury-associated information was obtained via self-report during the initial interview, which included self-report assessments of acute stress responses as well as risk and protective factors, such as discrimination/stigma and financial resources. Outcome interviews took place 3 months after hospital discharge, primarily in the participant’s home, and included qualitative interviews as well as assessments of PTSD and depression symptoms. All interviews were conducted by the full-time research staff.
Injury recovery and help-seeking intent.
Using a semistructured guide, the research staff asked participants to describe their experiences after injury as well as the ways in which they navigated circumstances they felt enhanced or impaired their recovery. The interviewer elicited perceptions of psychological help-seeking using the question “Has there ever been a time when you’ve considered talking to a professional about these experiences?” If a participant indicated that they had considered talking to a professional, they were asked to identify from whom and where they would seek this kind of psychological care. If they had not or would not consider talking to a professional, participants were asked what prevented them from seeking help. They were then asked to describe the characteristics of care providers, health care settings, and financial and/or logistical access that would make help-seeking more likely.
Depression symptoms.
Depression is a well-described consequence of trauma (Corbin et al., 2016; Richmond et al., 2009, 2010, 2011, 2014). We used the QIDS (Rush et al., 2003) to measure depression symptom severity in the present sample. The QIDS is a well-validated scale that has demonstrated strong internal consistency (Cronbach’s α = .86; Rush et al., 2003). The QIDS consists of 16 items reflecting nine domains related to past-week depression symptoms, such as suicidal thoughts (“I feel that life is empty or wonder if it’s worth living”) and energy level (“I really cannot carry out most of my usual daily activities because I just don’t have the energy.” Three domains have multiple items, but only the highest score from the set is recorded. Total QIDS scores range from 0 to 27 and correspond to levels of depression symptoms as follows: scores of 1–5 indicate no depression, 6–10 indicate mild depression, 11–15 indicate moderate depression, 16–20 indicate severe depression, and 21–27 indicate very severe depression (Rush et al., 2003). In the present sample, the Cronbach’s alpha value was .82.
PTSD symptoms.
To assess symptoms of PTSD, we used the PCL-5 (Blevins, Weathers, Davis, Witte, & Domino, 2015), a 20-item survey that includes items related to past-month presence and severity of four categories of symptoms, based on the diagnostic criteria in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5): reexperiencing, avoidance, hyperarousal, and negative alterations in cognition or mood. The PCL-5 asks respondents to rate how bothered they have been in the past month by such experiences as “feeling jumpy or easily startled” or “trouble falling or staying asleep” using a 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). Total PCL-5 scores range from 0 to 80, with higher scores reflecting more severe PTSD symptoms. A cutoff of 33 was found to be consistent with a provisional diagnosis of PTSD in military veterans (Dickstein et al., 2015). In the present sample, the Cronbach’s alpha value was .94.
Discrimination and stigma.
The community version of the PEDQ (PEDQ-CV) was used to assess stigma and experiences of discrimination based on race. The PEDQ-CV is a 17-item scale that assesses police and workplace discrimination as well as stigmatization, threat, and harassment (Brondolo et al., 2005). Sample items include “Have you been treated unfairly by coworkers or classmates?” and “Have others hinted that you are dishonest or can’t be trusted?” Respondents rate each item using a scale of 1 (never) to 5 (very often). Total PEDQ-CV scores range from 17 to 85. In the present sample, Cronbach’s alpha was .91.
Financial worry.
In our qualitative analysis, we found that financial concerns such as poverty, lack of health insurance, and cost of therapy were key concerns for Black men who survived traumatic injury (Jacoby, et al., 2018). Our database contained several possible quantitative measures for assessing financial concerns, including reported annual income, whether the respondent had health insurance (yes or no), and an item asking “How many times in the past 12 months were you worried or stressed about paying your rent?” Because a substantial proportion (24.5%) of participants declined to disclose their annual income and the health insurance item only assessed the presence or absence of insurance, we selected the housing insecurity item about worry in paying rent or mortgage as a reflection of the emotional impact of financial issues extending beyond health care alone. Studies have shown that this measure of housing insecurity is associated with frequent mental distress, poor or fair health status, and avoidance of medical care costs (Liu, Njai, Greenlund, Chapman, & Croft, 2014; Stahre, VanEenwyk, Siegel, & Njai, 2015). Participants were asked to respond to the financial worry item using a scale ranging from 1 (always) to 5 (never), with possible scores ranging from 1 to 5, with lower scores reflecting a higher degree of worry.
Data Analysis
We used QCA to explore the set-theoretic relations between trauma-related conditions and the outcome of help-seeking for psychological distress among Black, male trauma survivors. The QCA method is intersectional and uses Boolean algebra to assess how different conditions combine to produce a given outcome. It is a useful method with which to study complex problems that include multiple possible pathways to an outcome, particularly when applied to case studies of 10–100 cases for which researchers have in-depth knowledge of the individual cases but detection of cross-case patterns using qualitative methods alone would present a challenge.
There are two main forms of QCA: crisp set and fuzzy set. In crisp-set QCA, each case is assigned a set membership score for each condition and each outcome of either full-set membership (1) or full-set nonmembership (0). In fuzzy-set QCA (fsQCA), each condition or outcome can be assigned a set membership value ranging between 0 and 1, allowing for partial membership in one or more sets. For the present analysis, we used fsQCA to create a bridge between the quantitative and qualitative data and answer the question: What combination(s) of conditions lead to help-seeking among injured, Black, male trauma survivors admitted to the hospital?
We first conducted a necessity analysis to identify any causal conditions that must be present for the outcome to occur. In set-theoretic terms, a necessary condition is one for which the outcome is a subset of the condition. To evaluate necessity, we calculated the consistency score by comparing each causal condition against the outcome (i.e., help-seeking). The consistency score for a necessary condition is computed as the number of cases that share both the causal condition (X) and the outcome (Y), divided by the number of cases with the outcome (Y). We used the consistency level of .90 or above as the threshold for determining that a causal condition was necessary (Schneider & Wagemann, 2012).
We conducted a subset/superset analysis to assess all possible subsets of multiple causal conditions for inclusion in the sufficiency analysis. The subset/superset analysis provides consistency and coverage scores for different configurations of causal conditions. Combinations that display high consistency (i.e., .90 or higher) were advanced to the sufficiency analysis. We then conducted a sufficiency analysis to assess which causal condition or combination of causal conditions consistently produced an outcome. For the sufficiency analysis, the consistency score is the measure of the degree to which the causal condition, or combination of causal conditions, is sufficient to produce the outcome. In set-theoretic terms, a sufficient condition is one in which the condition, or combination of conditions, is a subset of the outcome. The consistency score for a sufficient condition is computed as the number of cases that share both the causal condition (X) and the outcome (Y), divided by the number of cases with the causal condition (X). We set the threshold at .80 or above for a combination of causal conditions to be considered as sufficient to produce the outcome. We used Fuzzy-Set/Qualitative Comparative Analysis (Version 3.0) software (fsQCA software; Ragin & Davey, 2016) to perform set-based analyses to assess first for necessity and then for sufficiency, by logically minimizing the sufficiency statements contained in the truth table, using the Quine-McCluskey algorithm (Schneider & Wagemann, 2012).
We conducted sufficiency analyses by constructing truth tables that displayed all logically possible combinations of causal conditions. One challenge of the truth table method in QCA is that not all logically possible combinations of the causal conditions, represented by the rows of the truth table, will have corresponding cases. This problem, called “limited diversity,” may occur because (a) cases may naturally cluster together in a given row, (b) some combinations are simply implausible, or (c) there are more possible combinations of causal conditions than there are cases. Because the number of possible combinations equals 2k, where k is the number of causal conditions, the more causal conditions included in the analysis, the more limited diversity (Schneider & Wagemann, 2012). For this reason, we chose to limit the number of causal conditions to those that we believed could theoretically contribute to the outcome. Although limited diversity is a common problem, the logical minimization procedure in QCA employs those rows without any cases, known as “logical remainders,” for counterfactual arguments that then inform the solutions (Schneider & Wagemann, 2012).
All truth tables were constructed using four causal conditions; this resulted in 16 rows, representing the number of possible combinations, which were then sorted by level of consistency. The truth table was then recoded, using .80 as the minimum consistency threshold for determining that a combination of causal conditions was sufficient to produce the outcome. For the help-seeking intent outcome, rows with a consistency of .80 or higher were assigned a set membership value of 1, and rows with consistency lower than .80 were assigned a set membership value of 0. Rows without cases were analyzed as logical remainders.
Standard analysis was then applied to each truth table. The standard analysis uses Boolean algebra to compare the combinations in the rows of the truth table that are associated with the outcome, in order to reduce these recipes to their simplest form. The standard analysis delivers three different solutions—complex, parsimonious, and intermediate—which differ from one another regarding the extent to which they make use of logical remainders to arrive at the simplest solution. The complex solution does not use the logical remainders to simplify the truth table, the parsimonious solution uses all of the remainders to logically minimize the truth table, and the intermediate solution uses only those logical remainders that are consistent with the expected effect that the causal condition will have on the outcome (i.e., simplifying assumptions) based on substantive knowledge about the cases. For this analysis, we utilized the recipes generated by the intermediate solution. (Schneider & Wagemann, 2012, p. 160).
We evaluated the solutions based first on their consistency scores. For solutions with a consistency score of .80 or above, we assessed coverage scores. Coverage scores express how much of the outcome is covered, or explained, by a causal condition or combination of causal conditions (Schneider & Wagemann, 2012, p. 129.) Raw coverage expresses how much of the outcome is covered by a given solution, even if that coverage overlaps with other solutions. Unique coverage expresses how much of the outcome is covered uniquely by a given solution. In general, the higher the overall coverage of a combination of causal conditions, the larger the number of cases to which it applies.
For this analysis, we were interested in the way trauma-related symptoms (i.e., PTSD and depression) combined with discrimination/stigma and financial worry to either facilitate or inhibit help-seeking intent among Black, male victims of trauma. We identified these four conditions based on our in-depth analysis of qualitative interviews. We then identified constructs in our quantitative database that corresponded as closely as possible to the themes identified in the qualitative study (Jacoby, et al., 2018). We chose the following causal conditions to include in our sufficiency analysis: (a) depression symptoms as measured by the QIDS (i.e., depression symptoms); (2) PTSD symptoms as measured by the PCL-5 (i.e., PTSD symptoms); (c) discrimination/stigma as measured by the PEDQ, which includes items assessing both stigma and discrimination based on race (i.e., discrimination); and (d) financial worry as measured by a single item assessing worry or stress about paying mortgage or rent in the past 12 months (i.e., financial worry). Data were available for all 32 cases, and there were no missing data. We assessed each of these causal conditions in relation to the outcomes of psychological help-seeking and negated psychological help-seeking, based on our qualitative analysis (Furnari, Greckhamer, & Fiss, 2018).
Calibration is the process of assigning membership scores to cases based on empirical and theoretical knowledge (Legewie, 2017). The primary outcome, help-seeking, was calibrated based on our qualitative analysis of the cases and their assignment into groups that represented different degrees of membership in help-seeking set, from fully in (1) to fully out (0), as follows: participant wants or has already welcomed professional help (1), participant wants professional help but cites potentially resolvable social challenges or expresses concerns about stigma (0.75), participant not interested in seeking help due to lack of access to insurance or financial resources or expresses concerns about stigma or sociocultural issues (0.25), participant expresses that he does not want or need help (0; Legewie, 2017; Ragin, 2009).
For each of the results based on quantitative scales, we conducted direct calibration (Ragin & Fiss, 2017). We first determined the value of the interval scale measure score at which a case is “fully in” a specified set (i.e., set membership score .95); the crossover point, or the threshold for maximum ambiguity or at which point the case membership score is 0.5 in the set and 0.5 out of the set; and, finally, the value at which a case is “fully out” of a set (i.e., set membership score .05). We then transformed the original interval scale values into fuzzy-set membership scores by transforming these data based on the log odds of full membership, using fsQCA software (Ragin & Davey, 2016). We conducted dual calibration of the four causal conditions based on ordinal score values for scales of depression symptoms (QIDS), PTSD symptoms (PCL-5), discrimination (PEDQ-CV), and financial worry. In dual calibration, more than one fuzzy set is created from a single source variable. For the present study study, we chose to use a dual calibration of the causal condition, such as “high depression” and “low depression,” rather than a single calibration of “depression.” We took this approach based on QCA literature, which argues that adding an adjective (e.g., “high” depression) “distinguishes a specific category or range of cases and, thus, is a good starting point for constructing a fuzzy set” (Ragin & Fiss, 2017). The following sets were constructed: high depression symptoms, low depression symptoms, high PTSD symptoms, low PTSD symptoms, high financial worry, low financial worry, high discrimination and low discrimination; different full membership, crossover, and full nonmembership thresholds were then established, as shown in Table 2.
Table 2.
Fuzzy-Set Calibration of Causal Conditions and Outcome
| Condition | Fuzzy Sets | Fuzzy-Set Score | Fully in | Crossover | Fully out | ||
|---|---|---|---|---|---|---|---|
| Help-seeking: Help-seeking was calibrated based on analysis of the qualitative interviews. Participants were asked “Has there ever been a time when you’ve considered talking to a professional about these experiences?” Based on their response to this question, their membership in the outcome set help-seeking was calibrated using the indirect methods. | Fully in: Wants help or has already welcomed help. | 1 | |||||
| More in than out: Participant cites social challenges that participant feels could be overcome, notes that past therapy was not helpful or expresses fears of stigma (“Someone telling me I’m crazy”.) | 0.75 | ||||||
| Crossover point | 0.5 | ||||||
| More out than in: Participant cites social challenges that prevent seeking help (such as lack of insurance), identifies alternative sources of support or expresses concerns about larger social stigma (“Our community does not do that.”). | 0.25 | ||||||
| Fully out: Participant responds “No” or “I do not need help.” | 0 | ||||||
| Depression: Depression symptoms were measured using the (QIDS) total score range of 0 to 27. For the fuzzy set for low depression symptoms, we set fully in at the midpoint for no depression, the crossover at 6.5, and fully out at the upper limit of mild depression. For high depression symptoms, we set fully in at the upper boundary of very severe depression, the crossover at the upper limit of moderate depression and fully out at the lower limit of moderate depression. | |||||||
| Low depression symptoms | 3 | 6.5 | 10.9 | ||||
| High depression symptoms | 21 | 14.9 | 11 | ||||
| PTSD: PTSD symptoms were measured using the PCL-5, total score range 0 to 80. For low PTSD, we set fully in at the equivalent of a response of “not at all” to half of the items and “a little bit” to half of the items, the crossover at the equivalent of “a little bit” on each item and fully out at the cutoff for provisional PTSD. For high PTSD, we set fully in at the equivalent of answering “quite a bit” to all items, the crossover at between “moderately” and “quite a bit” on each item and fully out at the cutoff for provisional PTSD. | |||||||
| Low PTSD symptoms | 10 | 20 | 33 | ||||
| High PTSD symptoms | 60.1 | 49.9 | 33 | ||||
| Discrimination: Discrimination was measured the PEDQ – CV, score range 17 to 85. For high discrimination, we set the fully out score at the equivalent of “rarely” on each item The crossover was set at halfway between “rarely” and “sometimes” and the fully in score at the equivalent of “sometimes” on each item. For low discrimination, we set the fully in score corresponding to “never/rarely,” the crossover score at just below the equivalent of “rarely,” and the fully out between “rarely’ and “sometimes.” | |||||||
| Low discrimination | 25 | 32.9 | 39 | ||||
| High discrimination | 51 | 42.5 | 34 | ||||
| Financial Worry: We used a single item asking: “How many times in the past 12 months were you worried or stressed about paying your rent?” Total scores on this item range 1 to 5. For high financial worry, we set the fully in score at “never”, the crossover at “usually” and the fully out score at “sometimes.” For low financial worry, we set the fully in score at “never”, the crossover at “rarely” and the fully out score at “sometimes”. | |||||||
| High financial worry | 1 | 1.9 | 3.1 | ||||
| Low financial worry | 5 | 3.9 | 3 | ||||
Note. PCL-5 = PTSD Checklist for DSM-5; QIDS = Quick Inventory of Depressive Symptomatology; PEDQ-CV = Perceived Ethnic Discrimination Questionnaire –Community Version.
Results
Necessity Analysis
To test for necessary conditions, we calculated consistency scores for each causal condition as a superset of the help-seeking outcome. The following results emerged: high depression symptoms (.61), low depression symptoms (.17), high PTSD symptoms (.46), low PTSD symptoms (.21), high discrimination (.50), low discrimination (.37), high financial worry (.45), and low financial worry (.46). No condition had a consistency score that met or exceeded the .90 threshold for necessity.
Sufficiency Analysis
Truth tables were constructed to evaluate whether combinations of the four causal conditions were sufficient to produce the outcome of interest. Consistent with best practices, we also report herein the characteristics of each truth table, including the number of rows and cases with consistency values of .80 or higher, the number of rows and cases with consistency values below .80, and the number of rows with no cases (see the Supplementary Materials). The subset/superset analysis, conducted using fsQCA software, revealed that the combination of high depression symptoms, high PTSD symptoms, low discrimination, and high financial worry had a consistency value higher than .90. We constructed a truth table using these four conditions and employed the standard analysis; this resulted in the intermediate solution, which incorporated the simplifying assumptions based on substantive knowledge that PTSD symptoms and depression symptoms act to facilitate help-seeking. The solution is shown in Table 3.
Table 3.
Simplified Solutions for Help-Seeking in Injured Black Men
| Solution | |||
|---|---|---|---|
| Causal condition | 1 | 2 | 3 |
| High depression symptoms | ● | ● | |
| High PTSD symptoms | ● | ⊗ | |
| Low discrimination | ⊗ | ||
| High financial worry | ⊗ | ● | |
| Consistency | 0.87 | 0.92 | 0.86 |
| Raw coverage | 0.35 | 0.43 | 0.23 |
| Unique coverage | 0.12 | 0.18 | 0.11 |
| Overall solution consistency | 0.87 | ||
| Overall solution coverage | 0.70 | ||
Note. PTSD = posttraumatic stress disorder. ● indicates the presence of the condition, ⊗ indicates the absence of the condition, and a blank space indicates that it does not matter if the condition is present or absent.
The consistency score is computed as the number of cases that share both the causal conditions and the outcome, divided by the number of cases with the causal conditions.
Raw coverage indicates how much of the outcome help-seeking is accounted for by the membership in a single solution.
Unique coverage indicates how much of the outcome help-seeking is uniquely accounted for by a single solution.
Coverage expresses how much of the outcome help-seeking is accounted for by all of the solutions taken together
The analysis revealed 3 solutions for help-seeking:
High depression symptoms AND not high financial worry OR
High depression symptoms AND high PTSD symptoms OR
High financial worry AND not low discrimination AND not high PTSD symptoms
Solution 1 indicated that the combination of severe depression symptoms in the absence of high levels of financial worry was sufficient for help-seeking. Solution 2 indicated that the combination of severe depression symptoms and severe PTSD symptoms was sufficient for help-seeking. Solution 3 indicated that the combination of high financial worry, absence of low discrimination (i.e., the presence of medium-to-high discrimination), and the absence of severe PTSD symptoms was sufficient for help-seeking. All three solutions exceeded the consistency threshold of .80 to conclude that they were sufficient to produce the help-seeking outcome.
We next conducted an analysis of a set negation of help-seeking, using the calibrated conditions (Greckhamer, Furnari, Fiss, & Aguilera, 2018). In the subset/superset analysis, the combination low PTSD symptoms, low depression symptoms, low discrimination, and high financial worry had a high level of consistency (.98) with the non–help-seeking outcome. We then constructed a truth table using these four causal conditions, and the standard analysis was applied to this truth table using fsQCA software, which in the intermediate solution shown in Table 4.
Table 4.
Simplified Solutions for Negated Help-Seeking in Injured Black Men
| Solution | ||
|---|---|---|
| Causal Condition | 1 | 2 |
| Low depression symptoms | ● | |
| Low PTSD symptoms | ● | |
| Low discrimination | ● | |
| High financial worry | ⊗ | ⊗ |
| Consistency | 0.82 | 0.82 |
| Raw coverage | 0.37 | 0.21 |
| Unique coverage | 0.22 | 0.06 |
| Overall Solution Consistency | 0.81 | |
| Overall Solution Coverage | 0.42 | |
Note. PTSD = posttraumatic stress disorder. ● indicates the presence of the condition, ⊗ indicates the absence of the condition, and a blank space indicates that it does not matter if the condition is present or absent.
The consistency score is computed as the number of cases that share both the causal conditions and the outcome, divided by the number of cases with the causal conditions.
Raw coverage indicates how much of the outcome help-seeking is accounted for by the membership in a single solution.
Unique coverage indicates how much of the outcome help-seeking is uniquely accounted for by a single solution.
Coverage expresses how much of the outcome help-seeking is accounted for by all of the solutions taken together
The analysis revealed two causal pathways for not seeking help:
Low depression symptoms AND not high financial worry OR
Low PTSD symptoms AND low discrimination AND not high financial worry
The first pathway indicated that the combination of less severe depression symptoms in the absence of high financial worry was sufficient for not seeking help. The second pathway indicated that the combination of less severe PTSD symptoms, low discrimination, and the absence of high financial worry was also sufficient for not seeking help. In the negated outcome of help-seeking, overall coverage was low (.42), indicating that there are other pathways to not seeking help that are not accounted for by these pathways.
We performed robustness and sensitivity analyses to assess whether the findings were robust to different specifications of the crossover points for both the original and set negation analysis of sufficiency (Furnari et al., 2018). We varied the crossover points by plus and minus 10% for each of the four causal conditions (i.e., high depression symptoms, high PTSD symptoms, low discrimination, and high financial worry). Although we observed minor changes in the number of solutions and neutral permutations, the consistency and coverage of the solutions were essentially unchanged, as was the interpretation of our results (see the Supplementary Materials).
Discussion
In this fuzzy-set qualitative comparative analysis of the narratives of Black men who have experienced traumatic injury, we identified multiple pathways for help-seeking and several pathways to not help-seeking. The results of this study help to clarify how trauma symptoms and important contextual factors, such as financial worry and discrimination, combine to determine whether Black men are open to seeking psychological help after injury. By applying QCA to both qualitative and quantitative data, we found that these factors combine in ways that reflect a complex association between barriers and facilitators. The existence of these distinct pathways challenges the tendency to view factors individually and either as barriers or facilitators, supporting our view that causation is complex and often intersectional.
In the present study, we discovered that the presence of trauma-related symptoms in the absence of structural factors facilitated help-seeking (Solutions 1 and 2) but that the presence of discrimination and financial worry in the absence of severe PTSD symptoms was also a causal recipe for psychological help-seeking for men with chronic traumatic stress and/or alcohol addiction (Solution 3.) The presence of discrimination and financial worry in the absence of PTSD symptoms constitutes a subset of certain Black, male, help-seeking trauma survivors, with relatively high consistency.
Regarding non–help-seeing behavior, the analysis revealed two pathways: (a) low severity of depression symptoms in the absence of financial worry and (b) low severity of PTSD symptoms combined with low discrimination and the absence of financial worry. In these cases, low posttraumatic symptom severity did not facilitate psychological help-seeking. These recipes demonstrated that when severe posttraumatic symptoms are absent at the individual level and social issues are also low or absent, the combination of these conditions is sufficient to negate help-seeking.
Our results are consistent with research that has shown the importance of symptoms of PTSD and depression for compelling Black men to seek care (Alvidrez et al., 2008; Jacoby, et al., 2018). Research has shown that financial concerns, stigmatizing beliefs, and difficulty accessing help, which is often due to inability to afford financial costs, can be important factors in help-seeking among trauma survivors (Kantor et al., 2017; Salaheddin & Mason, 2016). In addition, several studies have found low income, lower levels of educational attainment, and lower occupational status to serve as barriers to help-seeking (Cadaret & Speight, 2018; Lincoln, Taylor, Watkins, & Chatters, 2011).
Discrimination impacts help-seeking in Black men. Black men are significantly more likely than White men to be diagnosed with psychotic disorders, such as schizophrenia (Metzl, 2010). Studies have also found that Black men are less likely to access care for behavioral health issues, and when they do, they are more likely to receive inadequate care (Gonzalez et al., 2010). Mistrust of healthcare providers, a lack of health insurance, and limited availability of mental health services have also been identified as barriers to psychological help-seeking among Black men (Hudson, Eaton, Banks, Sewell, & Neighbors, 2018; Ward & Besson, 2013).
As a group, Black men experience racism to some degree throughout multiple facets of their lives. They share the structural weight of institutional, personally mediated, and internalized racism despite other resources or identities. These pressures impact their mental health and trust of systems and providers (Jones, 2000; Williams & Williams-Morris, 2000). The Black men who participated in the present study had the added stress of a traumatic injury, and, as a group, they experienced barriers to seeking help that were related to both structural factors and their own lived experiences. Traumatic stress, past trauma exposure, substance use, discrimination, and financial worry impact different Black men in different ways.
However, Black men are not a monolithic group nor are Black men who have experienced trauma, and they bring more than their race and gender to their experience of trauma exposure. The results of the present analysis demonstrate that even within a seemingly homogeneous group, causal conditions combine in ways that create either pathways to help-seeking or pathways to not seeking help. We believe that this perspective is critical in combating the tendency to see Black men only as part of a group, which is problematic from a research perspective given the specious nature of race itself but also constitutes a fundamental violation of human dignity (Link & Phelan, 2006; Mann, 1998). Using QCA, we were able to show that various causal conditions, some classically thought to be facilitators and others barriers, may combine in different ways toward the outcome of help-seeking among the Black men in this study.
Our study uniquely contributes to the prior literature by using fsQCA to describe causal complexity among the causal conditions that may affect help-seeking in Black men who are victims of trauma. Fuzzy-set QCA has demonstrated promising applications to research in health disparities. For example, rather than attributing Black and White differences in poverty to test scores, Ragin and Fiss (2017) used fsQCA to show how accumulated advantage favors White students and accumulated disadvantage disfavors Black students. Applying similar methods in health research could uncover important causal pathways for health inequalities rather than focusing on race or other demographic categories that are often investigated in isolation of their socioecologic context (Krieger, 2012).
The present sample consisted of 32 participant cases, which were drawn from a larger sample of 335 individuals. Although this number of cases is ideal for QCA, we considered four causal conditions, which were consistent with our conceptual framework. Because these cases emerged from a qualitative exploration of psychological help-seeking, the insights are applicable only to the participants in the qualitative study. As such, the results are not intended to be representative of the larger cohort.
Our sample also included participants who had suffered both intentional and unintentional injuries. Past studies have shown that survivors of trauma may experience traumatic symptoms regardless of circumstances of injury, although survivors of intentional injury may show a higher level of symptom severity (Jacoby, et al., 2018). Past qualitative studies have also suggested that intentionally injured Black men experience more persistent exposure to neighborhood violence and limited social support as compared to men with unintentional injuries (Jiang et al., 2018). Regarding seeking health for psychological symptoms, our qualitative analysis did not reveal thematic differences between men injured in these different ways. Future studies that use mixed methods may be needed to explore the complexity of injury intent and its impact on help-seeking behavior.
We used validated instruments to measure PTSD symptoms, depression symptoms, and discrimination. However, to assess financial worry, we used a single question that asked how often the participant worried about paying his mortgage or rent. This measure of housing insecurity was intended to capture the overall sense of financial stress experienced by the participant, but it did not capture the participant’s health insurance coverage for psychological services. Future research that uses more specific measures of access to and use of behavioral health care will be helpful in understanding how financial stress and insurance coverage impact help-seeking behavior for traumatic symptoms in this population.
Calibration is a critical step in the fsQCA process and results are sensitive to different calibrations of the causal conditions and of the outcomes. We provided transparent detail about how we arrived at these calibrations, which were based on our in-depth knowledge of the qualitative data and the quantitative scales. Nonetheless, as is often the case in mixed-methods research, other researchers who employ other frameworks or have other perspectives might construct different calibrations with different set membership parameters. To address this concern, we conducted a sensitivity analysis, altering the crossover points for each of the conditions, and the results of these changes did not substantially change the solutions nor did they substantially alter the consistency levels of the solutions.
Our study has implications for future research. Further research aimed at understanding different pathways to help-seeking behavior may identify new approaches to aiding Black men who are victims of trauma. Somewhat akin to a precision-medicine approach, future examination of these pathways may help to develop theories about utilization of behavioral health services for Black men that are based on their experiences rather than the assumption that all Black men who are trauma survivors have a single perspective on seeking help.
We conclude that QCA is a useful approach to identifying complex causal pathways for help-seeking behavior among Black men who survive traumatic experiences. The QCA method leverages the richness of mixed-methods approaches and case-study research methods to identify participant generated themes and assess how causal conditions intersect to create complex causal pathways. Our study revealed that severe posttraumatic symptoms create pathways to help-seeking among some Black men who survive trauma exposure, while for others, financial worry and discrimination combine in a pathway toward help-seeking in the absence severe symptoms of trauma.
Supplementary Material
Acknowledgments
The research reported in the present publication was supported by the National Institute of Nursing Research of the National Institutes of Health (R01NR013503; PI: Richmond). The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. No authors report no conflicts of interest.
References
- Alvidrez J, Shumway M, Kelly V, Smart S, Gelb M, Okin RL, … Boccellari A (2008). Which low-income urban crime victims use trauma-focused case management and psychotherapy services? Journal of Loss and Trauma, 13, 288–302. 10.1080/15325020701279782 [DOI] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. Journal of Traumatic Stress, 28, 489–498. 10.1002/jts.22059 [DOI] [PubMed] [Google Scholar]
- Brondolo E, Kelly KP, Coakley V, Gordon T, Thompson S, Levy E, …Contrada RJ (2005). The Perceived Ethnic Discrimination Questionnaire: Development and preliminary validation of a community version 1. Journal of Applied Social Psychology, 35, 335–365. 10.1111/j.1559-1816.2005.tb02124.x [DOI] [Google Scholar]
- Cadaret MC, & Speight SL (2018). An exploratory study of attitudes toward psychological help-seeking among African American men. Journal of Black Psychology, 44, 347–370. 10.1177/0095798418774655 [DOI] [Google Scholar]
- Corbin TJ, Harris E, Frisby B, Tabb L, Purtle J, & Rich JA (2016, November). Poor sleep quality among young urban victims of interpersonal violence: The role of post-traumatic stress and depression. Paper presented at the American Public Health Association Annual Meeting, Denver, CO. [Google Scholar]
- Corbin TJ, Purtle J, Rich LJ, Rich JA, Adams EJ, Yee G, & Bloom SL (2013). The prevalence of trauma and childhood adversity in an urban, hospital-based violence intervention program. Journal of Health Care for the Poor and Underserved, 24, 1021–1030. 10.1353/hpu.2013.0120 [DOI] [PubMed] [Google Scholar]
- Dickstein BD, Weathers FW, Angkaw AC, Nievergelt CM, Yurgil K, Nash WP, … Litz BT (2015). Diagnostic utility of the Posttraumatic Stress Disorder (PTSD) Checklist for identifying full and partial PTSD in active duty military. Assessment, 22(3), 289–297. 10.1177/1073191114548683 [DOI] [PubMed] [Google Scholar]
- Dowding D (2013). [Review of the book Best practices for mixed methods research in the health sciences by J. W. Creswell, A. C. Klassen, V. L. Plano Clark, & K. Clegg Smith]. Qualitative Social Work, 12, 541–545. 10.1177/1473325013493540a [DOI] [Google Scholar]
- Fereday J, & Muir-Cochrane E (2006). Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods, 5, 80–92. 10.1177/160940690600500107 [DOI] [Google Scholar]
- Fiss PC, Marx A, & Cambré B (2013). Chapter 1: Configurational theory and methods in organizational research: Introduction In Fiss PC, Cambre B, & Marx A (Eds.), Configurational theory and methods in organizational research (Vol. 38, pp. 1–22). Bingley, UK: Emerald. [Google Scholar]
- Furnari S, Greckhamer T, & Fiss P (2018, August). Studying configurations: Best practices for applying qualitative comparative analysis (QCA). Paper presented at the Academy of Management, Chicago, IL. [Google Scholar]
- Gonzalez HM, Vega WA, Williams DR, Tarraf W, West BT, & Neighbors HW (2010). Depression care in the United States: Too little for too few. Archives of General Psychiatry, 67, 37–46. 10.1001/archgenpsychiatry.2009.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greckhamer T, Furnari S, Fiss PC, & Aguilera RV (2018). Studying configurations with qualitative comparative analysis: Best practices in strategy and organization research. Strategic Organization, 16, 482–495. 10.1177/1476127018786487 [DOI] [Google Scholar]
- Haynes PL, Emert SE, Epstein D, Perkins S, Parthasarathy S, & Wilcox J (2017). The effect of sleep disorders, sedating medications, and depression on cognitive processing therapy outcomes: A fuzzy set qualitative comparative analysis. Journal of Traumatic Stress, 30, 635–645. 10.1002/jts.22233 [DOI] [PubMed] [Google Scholar]
- Holbrook TL, Anderson JP, Sieber WJ, Browner D, & Hoyt DB (1998). Outcome after major trauma: Discharge and 6-month follow-up results from the Trauma Recovery Project. Journal of Trauma and Acute Care Surgery, 45, 315–324. 10.1097/00005373-199808000-00018 [DOI] [PubMed] [Google Scholar]
- Hudson DL, Eaton J, Banks A, Sewell W, & Neighbors H (2018). “Down in the sewers”: Perceptions of depression and depression care Among African American men. American Journal of Men’s Health, 12, 126 10.1177/1557988316654864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacoby SF, Rich JA, Webster JL, & Richmond TS (2018). ‘Sharing things with people that I don’t even know’: help-seeking for psychological symptoms in injured Black men in Philadelphia. Ethnicity & Health, 1–19. https://10.1080/13557858.2018.1455811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang T, Webster JL, Robinson A, Kassam-Adams N, & Richmond TS (2018). Emotional responses to unintentional and intentional traumatic injuries among urban black men: A qualitative study. Injury, 49, 983–989. 10.1016/j.injury.2017.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CP (2000). Levels of racism: A theoretic framework and a gardener’s tale. American Journal of Public Health, 90, 1212–1215. 10.2105/ajph.90.8.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantor V, Knefel M, & Lueger-Schuster B (2017). Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: A systematic review. Clinical Psychology Review, 52, 52–68. 10.1016/j.cpr.2016.12.001 [DOI] [PubMed] [Google Scholar]
- Krieger N (2012). Methods for the scientific study of discrimination and health: An ecosocial approach. American Journal of Public Health, 102, 936–944. 10.2105/AJPH.2011.300544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legewie N (2017). Anchored calibration: From qualitative data to fuzzy sets. Forum: Qualitative Social Research, 18, Article 14. 10.17169/fqs-18.3.2790 [DOI] [Google Scholar]
- Lincoln KD, Taylor RJ, Watkins DC, & Chatters LM (2011). Correlates of psychological distress and major depressive disorder among African American men. Research on Social Work Practice, 21, 278–288. 10.1177/1049731510386122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, & Phelan JC (2006). Stigma and its public health implications. The Lancet, 367(9509), 528–529. 10.1016/s0140-6736(06)68184-1 [DOI] [PubMed] [Google Scholar]
- Liu Y, Njai RS, Greenlund KJ, Chapman DP, & Croft JB (2014). Relationships between housing and food insecurity, frequent mental distress, and insufficient sleep among adults in 12 US States, 2009. Preventing Chronic Disease, 11, E37–E37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J (1998). Dignity and health: The UDHR’s revolutionary first article. Health and Human Rights, 3, 30–38. 10.2307/4065297 [DOI] [PubMed] [Google Scholar]
- Metzl JM (2010). The protest psychosis: How schizophrenia became a black disease. Boston, MA: Beacon Press. [Google Scholar]
- Nowell LS, Norris JM, White DE, & Moules NJ (2017). Thematic analysis: Striving to meet the trustworthiness criteria. International Journal of Qualitative Methods, 16(1). 10.1177/1609406917733847 [DOI] [Google Scholar]
- QSR International. (2014). NVivo qualitative data analysis software (Version 10) [Computer software]. Doncaster, Australia: Author. [Google Scholar]
- Ragin CC (2009). Redesigning social inquiry: Fuzzy sets and beyond. Chicago, IL: University of Chicago Press. [Google Scholar]
- Ragin CC (2014). Comparative method: Moving beyond qualitative and quantitative strategies. Berkeley, CA: University of California Press. [Google Scholar]
- Ragin CC, & Davey S (2016). Fuzzy-set/qualitative comparative Analysis (Version 3.0) [Computer software]. Irvine, CA: Department of Sociology, University of California, Irvine. [Google Scholar]
- Ragin CC, & Fiss PC (2017). Intersectional inequality: Race, class, test scores, and poverty. Chicago, IL: University of Chicago Press. [Google Scholar]
- Rich JA, & Grey CM (2005). Pathways to recurrent trauma among young Black men: Traumatic stress, substance use, and the “code of the street.” American Journal of Public Health, 95, 816–824. 10.2105/AJPH.2004.044560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond TS, Ackerson T, Ruzek J, Wiebe D, Winston F, & Kassam-Adams N (2010). A predictive screener for depression & PSTD after physical injury. Injury Prevention, 16(Suppl 1), A76–A77. 10.1136/ip.2010.029215.279 [DOI] [Google Scholar]
- Richmond TS, Amsterdam JD, Guo W, Ackerson T, Gracias V, Robinson KM, & Hollander JE (2009). The effect of post-injury depression on return to pre-injury function: A prospective cohort study. Psychological Medicine, 39, 1709–1720. 10.1017/S0033291709005376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond TS, Guo W, Ackerson T, Hollander J, Gracias V, Robinson K, & Amsterdam J (2014). The effect of postinjury depression on quality of life following minor injury. Journal of Nursing Scholarship, 46, 116–124. 10.1111/jnu.12064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richmond TS, Kauder D, Hinkle J, & Shults J (2003). Early predictors of long-term disability after injury. American Journal of Critical Care, 12, 197–205. 10.4037/ajcc2003.12.3.197 [DOI] [PubMed] [Google Scholar]
- Richmond TS, Ruzek J, Ackerson T, Wiebe DJ, Winston F, & Kassam-Adams N (2011). Predicting the future development of depression or PTSD after injury. General Hospital Psychiatry, 33, 327–335. 10.1016/j.genhosppsych.2011.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, … Keller MB (2003). The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biological Psychiatry, 54, 573–583. 10.1016/s0006-3223(02)01866-8 [DOI] [PubMed] [Google Scholar]
- Salaheddin K, & Mason B (2016). Identifying barriers to mental health help-seeking among young adults in the UK: A cross-sectional survey. British Journal of General Practice, 66, e686–e692. 10.3399/bjgp16X687313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage H, Murray J, Hatch SL, Hotopf M, Evans-Lacko S, & Brown JS (2016). Exploring professional help-seeking for mental disorders. Qualitative Health Research, 26, 1662–1673. 10.1177/1049732315591483 [DOI] [PubMed] [Google Scholar]
- Schneider CQ, & Wagemann C (2012). Set-theoretic methods for the social sciences: A guide to qualitative comparative analysis. New York, NY: Cambridge University Press. [Google Scholar]
- Spangaro J, Koziol-McLain J, Zwi A, Rutherford A, Frail M-A, & Ruane J (2016). Deciding to tell: Qualitative configurational analysis of decisions to disclose experience of intimate partner violence in antenatal care. Social Science & Medicine, 154, 45–53. 10.1016/j.socscimed.2016.02.032 [DOI] [PubMed] [Google Scholar]
- Stahre M, VanEenwyk J, Siegel P, & Njai R (2015). Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Preventing Chronic Disease, 12 Advance online publication. 10.5888/pcd12.140511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vles WJ, Steyerberg EW, Essink-Bot M-L, Van Beeck EF, Meeuwis JD, & Leenen LP (2005). Prevalence and determinants of disabilities and return to work after major trauma. Journal of Trauma and Acute Care Surgery, 58, 126–135. 10.1097/01.ta.0000112342.40296.1f [DOI] [PubMed] [Google Scholar]
- Walia K, Belludi SA, Kulkarni P, Darak P, & Swamy S (2016). A comparative and a qualitative analysis of patients’ motivations, expectations, and satisfaction with dental implants. Journal of Clinical and Diagnostic Research, 10, ZC23–ZC26. 10.7860/JCDR/2016/17004.7538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward EC, & Besson DD (2013). African American men’s beliefs about mental illness, perceptions of stigma, and help-seeking barriers. The Counseling Psychologist, 41, 359 10.1177/0011000012447824 [DOI] [Google Scholar]
- Williams DR, & Williams-Morris R (2000). Racism and mental health: The African American experience. Ethnicity & Health, 5, 243–268. 10.1080/713667453 [DOI] [PubMed] [Google Scholar]
- Zatzick D, Jurkovich G, Russo J, Roy-Byrne P, Katon W, Wagner A,D…Rivara F (2004). Posttraumatic distress, alcohol disorders, and recurrent trauma across level 1 trauma centers. Journal of Trauma, 57, 360–366. 10.1097/01.ta.0000141332.43183.7f [DOI] [PubMed] [Google Scholar]
- Zatzick D, Russo J, & Katon W (2003). Somatic, posttraumatic stress, and depressive symptoms among injured patients treated in trauma surgery. Psychosomatics, 44, 479–484. 10.1176/appi.psy.44.6.479 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


