Abstract
Background
Individuals with multiple sclerosis (MS) are often plagued by the unpredictability of their disease and have to contend with uncertainty in their life and significant life changes. This can lead to high levels of stress, perceived lack of control, helplessness, and anxiety. Despite these circumstances, anxiety disorders are often overshadowed by depression, which can result in its presence being overlooked and undertreated by many medical professionals.
Methods
One hundred and eighty three individuals with MS completed a comprehensive online survey assessing depression and anxiety and the demographic and disease risk factors of such, including social support and substance use. Participants also completed measures of MS symptomatology, disease management, psychological well-being, and quality of life to determine the impact of depression and anxiety on outcomes associated with MS.
Results
Findings suggest that both depression and anxiety are prevalent in MS and related to many outcomes. However, based on comparisons of the associations and group comparisons, with a few exceptions, anxiety proved to more impactful than depression when examining these outcomes. When evaluating the risk factors/contributors of anxiety and depression, social support was a consistent predictor. Younger age and shorter disease duration were also associated with anxiety, while lower education and substance use were predictors of depression.
Conclusion
Findings suggest that attention to anxiety be given as much as depression as it plays a large role in individuals’ perceived health and well-being, which subsequently impacts the severity of symptoms and overall quality of life. Early identification of anxiety and potential substance use and increased social support also appear to be crucial for mitigating the impact of depression and anxiety.
Keywords: Anxiety, Depression, Social Support, Substance Use, Well-being
1. Introduction
Multiple sclerosis (MS), the leading cause of disability among middle-aged adults, affects women two to three times as often as men,1 with an age of diagnosis ranging from 20 to 50 years of age.2 The course of MS is variable and unpredictable. One’s disease may be fairly benign, with lifelong exacerbations and remissions. On the other hand, individuals may experience a progressive disease from onset, with steady decline over time. Many individuals (~50%) will transition from a relapsing-remitting course to a secondary progressive course over time (~11–19 years).3,4 Regardless of course, the host of physical, cognitive, and behavioral changes are known to greatly impact quality of life (QOL), psychological well-being, and everyday functioning. The unpredictable nature of the disease and lack of a known cure can lead to significant anxiety and depression regarding one’s future.
1.1. Depression in MS
Lifetime prevalence of depression in MS is 30% to 40%.5,6 Both biological and psychological etiologies have been proposed. Support for a biological etiology includes the involvement of lesions in the left arcuate fasciculus,7 temporal lobes,8,9 right temporal regions,10,11 and periventricular region and frontal lobes12 and greater severity in those with lesions of cerebral versus spinal cord involvement.13,14 Support for a psychological etiology includes the finding that depression in MS tends to be unrelated to disease severity2,15 and more linked to the unpredictability and unforeseen prognosis in MS.2 Support for this finding is that depression to has been found to be lower in individuals with a progressive course of MS compared with a relapsing remitting course.16 Some contend that this is due to the certainty that accompanies a progressive course as illness intrusiveness and uncertainty are known predictors of depression in MS.17 Other known psychosocial factors include younger age, lower education, shorter disease duration, and perceived limited social support.18,19 The consequences associated with depression in MS include worsening of MS symptoms,20,21 poor illness management,22 greater medical utilization, lower employment,23 reduced effectiveness of interventions,21 increased suicidal ideations and attempts,24 and decreased quality of life.25–27
1.2. Anxiety in MS
Anxiety disorders occur in 36% of individuals with MS,28 with 34% to 70% of early diagnosed individuals experiencing anxiety. Anxiety is also known to result from a combination of biological and psychosocial factors. Biological factors associated with anxiety, in general, points to abnormal neuronal circuity involving the amygdala, basal ganglia, and cerebral cortex and a host of neurotransmitter systems.29 With regard to psychosocial factors, individuals with MS who suffer from anxiety are more likely to be female, have a shorter disease duration, lower disability levels, younger age of onset, and a lifetime diagnosis of depression.23,30,31 A higher rate of substance abuse, greater social stress, and limited social support are also known contributors.28,31 The consequences of anxiety are similar to depression, particularly, decreased quality of life,32 poor adherence,33 and increased suicidal ideation.28
1.3. Comorbid Depression and Anxiety
Though anxiety and depression are detrimental to one’s health in their own right, it is important to acknowledge their role together as a comorbid diagnosis of anxiety and depression (CAD) is highly prevalent in people with chronic conditions.34 In the general population, it has been found that 57% of people diagnosed with depression also experience anxiety, and of those with anxiety 28% were found to have depression.35 Risk factors of CAD included being older, unemployed, less educated, and female.36 While there is limited research of CAD in MS, it has been shown that the consequences of CAD in patients with MS and other chronic conditions are much greater than the presence of only depression or anxiety, particularly with regard to quality of life, symptomology, increased thoughts of self-harm social, and greater social dysfunction.37,38
Despite their high comorbidity, research surrounding depression in MS is much more extensive. This may be in part due to the assumption that depression in MS has a greater biological etiology and is just “typical” as it has been reported as far back as Charcot’s descriptions of patients.39 However, anxiety has been purported to be highly underrated in MS, and overshadowed by depression.30 It is surprising that anxiety is not given as much consideration in MS as we know that stress,29 perceived negative consequences, and intolerance of uncertainty40 all lie at the foundation of the experience of anxiety. As stated earlier, by virtue of its nature, MS can greatly exacerbate these feelings given its uncertainty and variability – this may be particularly true early on in the disease process, which has been previously shown.31
Recently, in the Controversies in Multiple Sclerosis, the question arose as to whether or not anxiety was more important than depression in MS. Proponents for “no” contended that depression has long been “intertwined with the characteristics of the disease” and is a known factor in worsening MS symptoms. They also speak to the established link of depression with poor QOL and disease management and increased suicidal ideation.41 The counterargument was that anxiety, despite being significantly less studied in MS, has demonstrated the same negative impact in MS. Proponents of “yes,” noted that further research is needed as there has only been one intervention to specifically address anxiety in MS and it pertained to injection phobia. The authors contend that anxiety is an “invisible” symptom, likely to lead to greater health utilization and somatization, which may be confounded with MS symptoms and may, in part explain why it is overlooked. They add, the mere definition of anxiety, “a feeling of worry, nervousness or unease about something with an uncertain outcome” can certainly be aptly applied to something like living with MS.42 A recent study (2019), which looked into the simultaneous functional impact of depression and anxiety on MS, still suggested that depression take priority in studies as it was found to be associated with higher physical disability and lower employment, while anxiety was not.23
Jumping off from this “controversy,” the present study examines the differential impact of depression, anxiety, and CAD among a large sample in which disease symptomology, disease management, psychological well-being, and quality of life were assessed. We predict that while both anxiety and depression will have a substantial impact, anxiety may prove to be more detrimental. Based on the limited research available, we also propose that these outcomes will be worse in the presence of CAD. However, despite whether one is “greater” than the other it is important to also identify and understand how anxiety and depression are influenced by one’s level of social support and substance use, which as described above are known modifiable contributors to both. Finally, given less is known about the demographic and disease risk factors for anxiety in MS, the present study also explores the contributors to both.
2. Material & Methods
2.1. Participants
All participants were diagnosed with clinically definite MS and enrolled in a longitudinal investigation examining employment status in MS. They completed their assessment between January 2014 and March 2017. Eligibility criteria included age ranging from 20 to 64, absence of other neurological disorders, and presently employed. Individuals were recruited on a national level through the National Multiple Sclerosis Society website and local MS clinics. All participants completed an online survey, approved by the Institutional Review Board. Informed consent was obtained from all participants.
2.2. Measures
The State Trait Anxiety Inventory (STAI) 43 was used to assess anxiety. Individuals are asked to rate how the feel at this moment (state anxiety) as well as how they generally feel (trait anxiety). Scores on trait anxiety were used in the present study. A cutoff of 1.5 standard deviation was used to identify those with elevated anxiety.
Depression was assessed by the Chicago Multiscale Depression Inventory (CMDI), 44 a measure designed specifically to assess depression in MS and other medically-ill groups. It consists of three subscales: Evaluative, Mood, and Vegetative. A cutoff of 22 on the CMDI evaluative scale was used to identify those with elevated depression.45 The mood scale was used for all other analyses.
Modified Social Support Scale (MSSS) assessed one’s level of social support. This is an 18 item questionnaire that consists of four subscales to measure tangible support, emotional/informational support, affectionate support, and positive social interactions.
The COPE inventory46 assesses different ways individuals respond to stress. It consists of scales to measure problem- and emotion-focused coping, and three less adaptive coping styles. Three items also measure Substance Use, which was used to assess one’s proclivity to engage in substance use.
The Modified Fatigue Impact Scale (MFIS) is a modified form of the Fatigue Impact Scale 47 based on 21 items derived from interviews with MS patients concerning how fatigue impacts their lives. It consists of three subscales: physical, cognitive, and psychosocial functioning. The physical scale was used in the present study.
Sleep was assessed by the Pittsburgh Sleep Quality Index (PSQI),48 a measure of sleep quality consisting of several domains of sleep. It consists of 19 items rated by the individual and five by a bed partner.
The MOS Pain Effects Scale (MOS-PES), a brief measure assessing the experience and impact of pain that is part of the Multiple Sclerosis Quality of Life Inventory 49 was used to assess pain.
Disease management and perceived self-efficacy in managing one’s MS was assessed by the Multiple Sclerosis Self-Management Scale (MSSM-R)50 and Disability Management Self-Efficacy Scale (DMSES), respectively. The MSSM-R assesses one’s level of self-management, in general, as well as aspects of self-management specific to the experiences of persons with MS. The DMSES was developed to assess how an individual with MS handles or feels they can manage their illness.
Psychological well-being was assessed by the Ryff Scales of Psychological Well-being. This measure consists of six subscales: personal relationships, autonomy, personal growth, purpose in life, environmental mastery, and self-acceptance.
The Satisfaction with Life Scale,51 Flourishing Scale (FS)52 and Perceived Stress Scale (PSS)53 were administered to assess one’s overall satisfaction with life and level of everyday stress, respectively. All are brief, five, eight, and 10 items, respectively.
2.3. Statistical Analyses
All statistical analyses were conducted using SPSS version 26.0. Initial correlations and Student’s t-tests were conducted among the contributing factors (i.e., age, gender, education, disease course, disease duration, age of onset, social support, and substance use). Subsequent stepwise regression analyses were then conducted to determine their relative contribution.
Bivariate correlation analyses were conducted with depression and anxiety with MS disease symptoms, disease management, psychological well-being, and quality of life. To compare the associations, r to z transformations within a dependent sample were conducted. Finally, to determine the differential impact of depression, anxiety, and CAD on outcomes, group comparisons with a Bonferroni adjustment were made among the following four groups: (1) those with no significant depression or anxiety; (2) those with only significant depression; (3) those with only significant anxiety; and (4) those with both significant depression and anxiety (CAD).
3. Results
3.1. The Sample
The present study consisted of 183 individuals with MS. Approximately 90% were women and 95% had a relapsing-remitting course. The mean age of the sample was 44.09 (SD=9.51) and mean disease duration was 8.63 (SD=6.66). Approximately 24% of the sample had significantly elevated depression and 22% were experiencing significant anxiety. Of those depressed, 55% were also experiencing significant anxiety and of those who were anxious, 60% endorsed significant depression, suggesting a significant level of comorbidity. In sum, 123 (67%) reported no significant depression or anxiety; 20 (11%) were depressed; 16 (9%) were anxious, and 24 (13%) had comorbid anxiety and depression (CAD). There were no differences in gender, age, education, disease course, or disease duration among the groups (See Table 1).
Table 1.
Participant demographics
| Mean (SD) or Frequency | ||||||
|---|---|---|---|---|---|---|
| Entire Sample (N = 183) | Non (N = 123) | Depressed (N = 20) | Anxious (N = 16) | CAD (N = 24) | F, sig. | |
| Age | 44.09 (9.51) | 44.48 (9.69) | 43.05 (8.02) | 41.31 (10.00) | 44.83 (9.58) | F(3,179)=.648, .585 |
| Gender | 19M/164F (90%) | 13M/110F | 4M/16F | 16F | 2M/22F | X2=3.96, .266 |
| Education | 15.79 (2.17) | 16.02 (2.19) | 15.85 (1.66) | 15.44 (2.34) | 14.83 (2.16) | F(3,179)=2.19, .091 |
| Disease | 173RR (95%) | 115RR | 19RR/1SP | 16RR | 23RR/1PP | X2=1.27, .737* |
| Course | 5PP/4SP/1PR | 4PP/3SP/1PR | ||||
| Disease Duration | 8.63 (6.66) | 8.93 (6.83) | 7.70 (6.24) | 7.25 (5.15) | 8.76 (7.21) | F(3,179)=.441, .724 |
Note. Non = Non-depressed, non-anxious; CAD = Comborbid anxiety and depression; RR=Relapsing remitting; PP=Primary progressive; SP=Secondary progressive; PR=Progressive relapsing
Computed between relapsing remitting and all other disease courses
3.2. Risk factors of depression and anxiety
Higher levels of anxiety was related to younger age (r = −.20, p = .007) and shorter disease duration (r = −.18, p = .016). There was a trend for reports of higher depression associated with lower education (r = −.14, p = .053). There were no differences with regard to gender for anxiety or depression. However, analyses were likely underpowered given the large majority of women. Similarly, there were no significant differences with regard to disease course, but there was a trend for greater anxiety being observed in those with a relapsing-remitting course (p=.062). This result may have been significant but was likely underpowered given the small sample of progressive MS (N=10) (See Table 2).
Table 2.
Correlations and mean differences of depression and anxiety for suspected risk factors
| Depression | Anxiety | |||||
| Age | r = −.01, p = .893 | r = −.20, p = .007 | ||||
| Education | r = −.14, p = .053 | r = −.10, p = .199 | ||||
| Age of Onset | r = .02, p = .746 | r = −.08, p = .305 | ||||
| Duration | r = −.05, p = .521 | r = −.18, p = .016 | ||||
| Social Support | r = −.45, p <.001 | r = −.37, p <.001 | ||||
| Substance Use | r = .23, p = .002 | r = .18, p = .017 | ||||
| Men N=19 | Women N=164 | Sig. | Men N=19 | Women N=164 | Sig. | |
| Gender | 23.00 (10.14) | 23.74 (12.20) | .800 | 36.05 (11.07) | 40.14 (12.35) | .169 |
| RR N=173 | PP/SP/PR N=10 | RR N=173 | PP/SP/PR N=10 | |||
| Course | 23.81 (12.05) | 21.10 (11.01) | .488 | 40.12 (12.20) | 32.70 (11.59) | .062 |
Note. Duration = Disease duration in years; Course = Disease course; RR = Relapsing Remitting; PP = Primary Progressive; SP = Secondary Progressive; PR = Progressive Relapsing
When taking into consideration these associations and including social support and substance, regression analyses revealed that social support and age were the greatest predictors of anxiety, accounting for 17% of the variance. Social support, substance use, and education reigned as the most significant contributors of depression, accounting for 24% of the variance (See Table 3).
Table 3.
Forward stepwise regression predicting anxiety and depression
| Anxiety | |||
| B | sig. | Adjusted R2 | |
| Model 1 | |||
| Social Support | −1.10 | .000 | .13 |
| Model 2 | |||
| Social Support | −1.11 | .000 | |
| Age | −.267 | .003 | .17 |
| Depression | |||
| B | sig. | Adjusted R2 | |
| Model 1 | |||
| Social Support | −1.31 | .000 | .20 |
| Model 2 | |||
| Social Support | −1.25 | .000 | |
| Substance Use | .863 | .010 | .23 |
| Model 3 | |||
| Social Support | −1.25 | .000 | |
| Substance Use | .830 | .013 | |
| Education | −.708 | .049 | .24 |
3.3. Associations of depression and anxiety with outcomes
Both anxiety and depression were significantly associated with all outcomes with correlations for depression ranging from .34 to .72 and for anxiety, ranging from .35 to 85. Comparable associations were found for anxiety and depression with disease symptoms and disease management. The strongest correlations with anxiety were observed with aspects of psychological well-being and quality of life that pertain to self-acceptance, environmental mastery, purpose in life, satisfaction with life, flourishing, and perceived stress. These associations, as well as personal growth were found to be significantly greater than the association with depression. Depression demonstrated the strongest correlation with perceived stress, environmental mastery, and satisfaction with life, but the association with anxiety was still significantly greater. See Table 4.
Table 4.
Correlations of depression and anxiety with disease symptoms, disease management, psychological well-being, and quality of life with and r-z transformation for comparison of correlations
| Depression | Anxiety | z, sig. | |
|---|---|---|---|
| Disease Symptoms | |||
| Fatigue | .37** | .39** | −.42, .336 |
| Pain | .54** | .50** | .93, .177 |
| Sleep | .40** | .45** | –1.09, .139 |
| Disease Management | |||
| Disease Self-management | −.34** | −.35** | .21, .418 |
| MS Self-efficacy | −.46** | −.44** | −.44, .330 |
| Psychological Well-being | |||
| Self-acceptance | −.66** | −.82** | 5.13, >.001 |
| Environmental Mastery | −.62** | −.79** | 5.07, .001 |
| Purpose in Life | −.55** | −.69** | 3.63, >.001 |
| Personal Relationships | −.58** | −.61** | .75, .227 |
| Autonomy | −.41** | −.48** | 1.54, .062 |
| Personal Growth | −.37** | −.49** | 2.62, .004 |
| Quality of Life | |||
| Satisfaction with Life | −.60** | −.71** | 2.98, .001 |
| Flourishing Scale | −.52** | −.62** | 2.44, .007 |
| Perceived Stress | .72** | .85** | −4.65, >.001 |
3.4. Group comparisons based on presence of depression, anxiety, and CAD
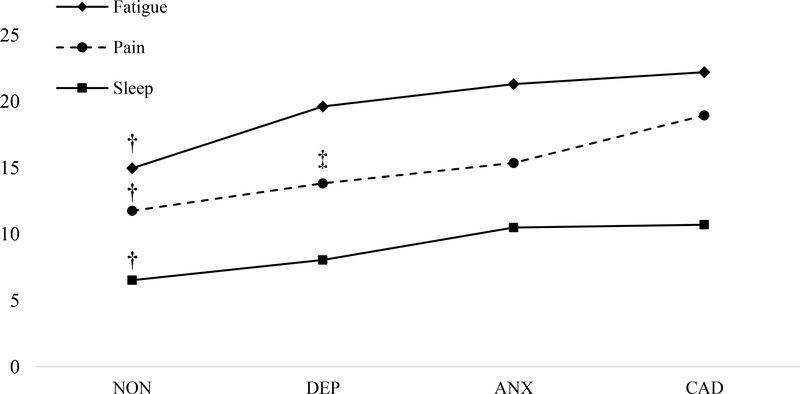
Group comparisons revealed that anxiety has a greater impact than depression on disease symptoms. More specifically, while comparably associated with disease symptoms, group differences on fatigue, pain, and sleep suggest that depressed individuals do not differ from those with neither depression nor anxiety. However, anxious individuals or those with CAD experience significantly more fatigue, pain, and sleep problems. There was also a significant increase in pain between depressed individuals and those with CAD suggesting that the comorbidity of anxiety is greater than depression alone (See Table 5 and Figure 1).
Table 5.
Comparisons on disease symptoms between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
| Reference Group | F, sig. | Mean Difference | Sig. |
|---|---|---|---|
| Fatigue | F [3,178] = 7.96, p < .001 | ||
| NON | DEP | −4.66 | .129 |
| ANX | −6.34 | .023 | |
| CAD | −7.24 | .001 | |
| DEP | ANX | −1.68 | 1.00 |
| CAD | −2.58 | 1.00 | |
| ANX | CAD | −.90 | 1.00 |
| Pain | F [3,178] = 14.84, p < .001 | ||
| NON | DEP | −2.08 | .579 |
| ANX | −3.61 | .046 | |
| CAD | −7.19 | .000 | |
| DEP | ANX | −1.53 | .577 |
| CAD | −5.11 | .007 | |
| ANX | CAD | −3.58 | .174 |
| Sleep | F [3,178] = 12.53, p < .001 | ||
| NON | DEP | −1.52 | .573 |
| ANX | −3.97 | .000 | |
| CAD | −4.18 | .000 | |
| DEP | ANX | −2.45 | .313 |
| CAD | −2.66 | .121 | |
| ANX | CAD | −.21 | 1.00 |
Figure 1.
Comparisons on disease symptoms between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
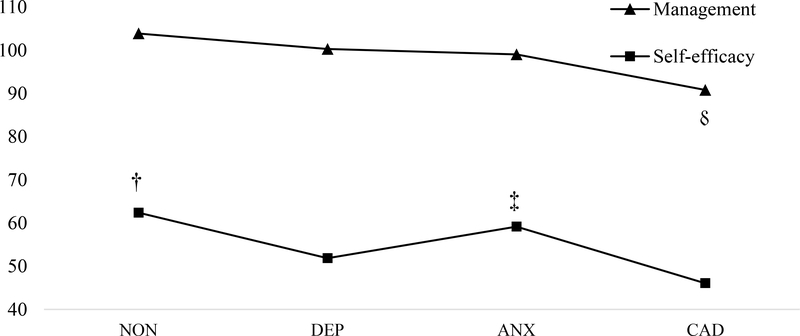
With regard to disease management, depression appeared to have a greater impact. Specifically, depressed individuals or those with CAD reported significantly lower self-efficacy compared to those with neither. There was no difference for anxious individuals. Individuals with CAD also reported significantly lower self-efficacy than anxious individuals. Poor self-management was worse among those with CAD and significantly differed from those with depression or neither. No differences were observed for the anxious group (See Table 6 and Figure 2).
Table 6.
Comparisons on disease management between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
| Reference Group | F, sig. | Mean Difference | Sig. |
|---|---|---|---|
| Disease Management | F [3,179] = 8.78, p < .001 | ||
| NON | DEP | 3.60 | 1.00 |
| ANX | 4.85 | .710 | |
| CAD | 13.05 | .000 | |
| DEP | ANX | 1.25 | 1.00 |
| CAD | 9.46 | .047 | |
| ANX | CAD | 8.21 | .179 |
| MS Self-efficacy | F [3,179] = 10.95, p < .001 | ||
| NON | DEP | 10.54 | .013 |
| ANX | 3.27 | 1.00 | |
| CAD | 16.35 | .000 | |
| DEP | ANX | 7.28 | .743 |
| CAD | 5.81 | 1.00 | |
| ANX | CAD | 13.08 | .026 |
Figure 2.
Comparisons on disease management between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
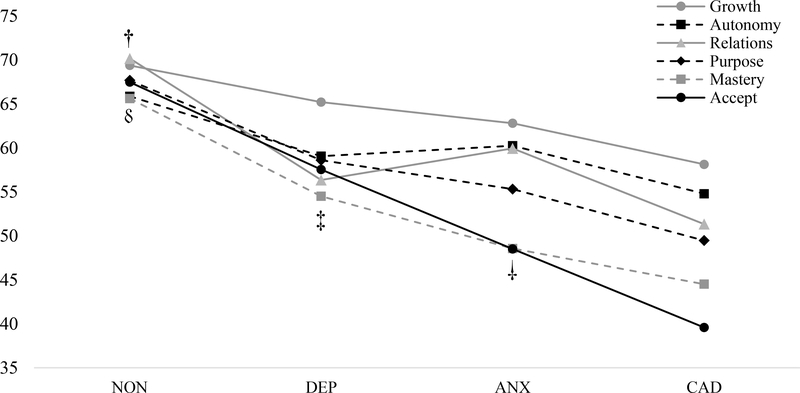
On a measure of psychological well-being, a consistent finding was observed for many of the domains. Specifically, feelings of self-acceptance, environmental mastery, purpose in life, personal relationships, and personal growth were all greatly impacted by both depression and anxiety as evident in their both being significantly less than among those with neither. While not statistically significant, there was a linear progression with added comorbidity, with those with CAD reporting the least sense of well-being compared to those with neither in these five domains. Differences were also seen between depressed individuals and those with CAD on domains of self-acceptance, environmental mastery, purpose in life, and personal growth, suggesting that anxiety, whether alone or in combination with depression may have a greater impact on these domains of well-being. Acceptance demonstrated a significant drop from those with anxiety and those with CAD. Finally, autonomy seems to be more impacted by depression with significantly less feelings of autonomy among those with depression or CAD (See Table 7 and Figure 3).
Table 7.
Comparisons on psychological well-being between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
| Reference Group | F, sig. | Mean Difference | Sig. |
|---|---|---|---|
| Self-acceptance | F [3,179] = 58.89, p < .001 | ||
| NON | DEP | 9.92 | .001 |
| ANX | 18.97 | .000 | |
| CAD | 27.89 | .000 | |
| DEP | ANX | 9.05 | .059 |
| CAD | 17.97 | .000 | |
| ANX | CAD | 8.92 | .050 |
| Environmental Mastery | F [3,179] = 43.48, p < .001 | ||
| NON | DEP | 11.11 | .000 |
| ANX | 17.05 | .000 | |
| CAD | 21.11 | .000 | |
| DEP | ANX | 5.94 | .422 |
| CAD | 10.00 | .005 | |
| ANX | CAD | 4.06 | 1.00 |
| Purpose in Life | F [3,179] = 30.10, p < .001 | ||
| NON | DEP | 9.07 | .001 |
| ANX | 12.35 | .000 | |
| CAD | 18.21 | .000 | |
| DEP | ANX | 3.29 | 1.00 |
| CAD | 9.14 | .012 | |
| ANX | CAD | 5.85 | .370 |
| Personal Relationships | F [3,179] = 29.76, p < .001 | ||
| NON | DEP | 13.82 | .002 |
| ANX | 10.23 | .000 | |
| CAD | 18.84 | .000 | |
| DEP | ANX | −3.59 | 1.00 |
| CAD | 5.02 | .678 | |
| ANX | CAD | 8.60 | .067 |
| Autonomy | F [3,179] = 11.45, p < .001 | ||
| NON | DEP | 5.62 | .019 |
| ANX | 6.82 | .158 | |
| CAD | 11.08 | .000 | |
| DEP | ANX | −1.20 | 1.00 |
| CAD | 4.26 | .827 | |
| ANX | CAD | 5.46 | .449 |
| Personal Growth | F [3,179] = 11.13, p < .001 | ||
| NON | DEP | 9.07 | .001 |
| ANX | 12.35 | .000 | |
| CAD | 18.21 | .000 | |
| DEP | ANX | 3.29 | .422 |
| CAD | 10.00 | .005 | |
| ANX | CAD | 4.06 | 1.00 |
Figure 3.
Comparisons on psychological well-being between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
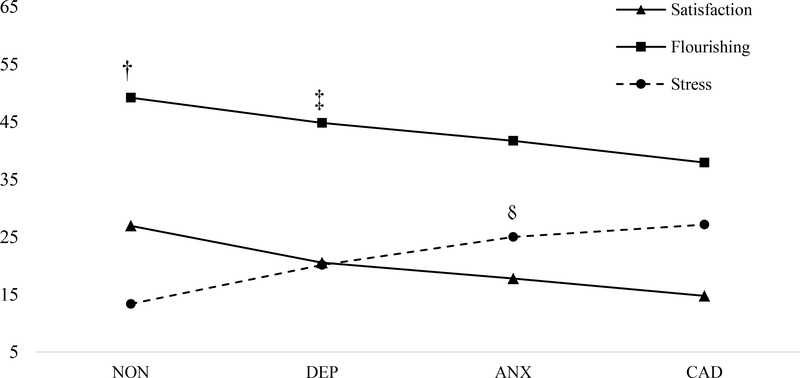
The last outcome of interest, QOL, demonstrated a significant effect for group similar to the majority of indices of well-being. In particular, depressed and anxious individuals reported lowered QOL and increased stress. Those with CAD proved to have the worst QOL and most perceived level of stress. Those with CAD had significantly worse QOL and greater stress compared to depressed individuals, suggesting again the greater impact of comorbid anxiety (See Table 8 and Figure 4).
Table 8.
Comparisons on quality of life between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
| Reference Group | F, sig. | Mean Difference | Sig. |
|---|---|---|---|
| Satisfaction with Life | F [3,179] = 42.42, p < .001 | ||
| NON | DEP | 6.42 | .000 |
| ANX | 9.17 | .000 | |
| CAD | 12.17 | .000 | |
| DEP | ANX | 2.75 | .862 |
| CAD | 5.75 | .005 | |
| ANX | CAD | 3.00 | .586 |
| Flourishing | F [3,179] = 24.81, p < .001 | ||
| NON | DEP | 4.39 | .031 |
| ANX | 7.50 | .000 | |
| CAD | 11.27 | .000 | |
| DEP | ANX | 3.11 | .907 |
| CAD | 6.88 | .003 | |
| ANX | CAD | 3.77 | .427 |
| Perceived Stress | F [3,179] = 59.96, p < .001 | ||
| NON | DEP | −6.75 | .000 |
| ANX | −11.65 | .000 | |
| CAD | −13.78 | .000 | |
| DEP | ANX | −4.90 | .047 |
| CAD | −7.03 | .000 | |
| ANX | CAD | −2.13 | 1.00 |
Figure 4.
Comparisons on quality of life between non-depressed, non-anxious (NON), depressed (DEP), anxious (ANX), and depressed and anxious (CAD).
4. Discussion
In the present study, we sought to determine: (1) The risk factors associated with depression and anxiety; and (2) the impact of depression, anxiety, and CAD on outcomes in MS. Risk factors for anxiety included younger age, shorter disease duration, and to an extent, a relapsing-remitting course. None of the purported demographic and disease risk factors for depression reached significance, but there was a trend for lower education. Social support and substance use were significantly associated with both depression and anxiety. When taken together, social support consistently reigned as the most significant predictor of both, accounting for 13% and 20% of the variance, respectively.
These findings speak to the importance of assessing and identifying anxiety early on in the disease course when anxiety may be at its worse and greatly suggests that it is important to target social support as a therapeutic agent in treating and preventing both anxiety and depression symptoms. Future studies looking into the effects of providing social support to decrease the impact of anxiety and depression risk factors, as way of managing MS symptomology and improving QOL could be beneficial. This finding is not new – social support in MS has been shown to produce positive effects on both mental and physical health.54,55
With regard to the finding of younger age being associated with anxiety, this is true for the general population as well. Older individuals often report a higher sense of self well-being compared to younger individuals and we have shown the same pattern exists in people with MS.56 This pattern is suggestive of the uncertainty many young individuals already face in regards to their employment status, career, and relationships. This uncertainty is likely to increase with a diagnosis of a major chronic disease, like MS where inconsistent flare-ups of the disease can lead to higher levels of anxiety.57 Along with age, negative coping methods also serve as risk factors for psychological symptoms. Substance use is a common avoidance coping strategy that has consistently been linked to depression and anxiety, described as being used as a distraction during relapse or a way to deal with the unpredictability of the disease.58–60 In contrast, positive coping strategies have been shown to be associated with a higher level of education and a predictor of positive health-related habits such as diet and exercise.61,62 The combination of substance use and lower education predicting depression in the present sample confers this. Therefore, clinicians should take time to educate and provide information on positive coping strategies to individuals with MS, especially among those who may be less educated in order to prevent or decrease depressive symptoms.
When examining the impact of depression and anxiety, anxiety was, for the most part, more impactful than depression, particularly for disease symptoms, with depressed individuals not differing from those with no depression or anxiety. The presence of anxiety or CAD resulted in significant fatigue, pain, and sleep problems. These findings are somewhat consistent with Beiske et al. (2008) in which the odds for fatigue were three times higher for those with depression, but as high as five times higher for anxiety. They also found that those with anxiety were four times more likely to report pain with no association with depression.
With regard to psychological well-being and QOL, a consistent finding was found for the majority of domains. Specifically, depressed, anxious, and CAD groups all differed from those with no depression or anxiety. While not statistically significant, a linear progression of decreased psychological well-being and QOL starting among the depressed group and declining with the presence of anxiety and ultimately being the worse among those with CAD.
Additionally, those with CAD reported significant worse psychological well-being than those with only depression, suggesting anxiety may be an exacerbating factor. These findings suggest that greater attention be given to anxiety in MS when examining psychological well-being and QOL and may explain why some contend that anxiety does not always “reach significance” when studied in MS. In particular, most studies of depression in MS have taken a medical model, or deficit approach in which they look at the absence of good health (e.g. fatigue) and do not always include assessment of psychological well-being and aspects of flourishing, which is the presence of wellness, despite poor health. In this case, anxiety was a much greater factor for not achieving such and showed very strong correlations. Further studies examining anxiety in MS may benefit from not only looking at the “negative” (e.g., fatigue, pain, depression) but also the “positive.” In doing so, we may learn much more about the impact of anxiety in MS and its hindrance to living well with MS.
With regard to disease management, depression appeared to have a greater influence on one’s management and perceived self-efficacy over their disease. This was also shown with regard to autonomy from the psychological well-being scales. Such findings suggest that depression may play a larger role in one’s perceptions of their ability to exert an influence on their illness and being self-reliant regardless of others opinions or social pressures. This general sense of ineffectiveness, possible learned helplessness, and insecurity in one’s decisions may be more reflective of feelings of depression than anxiety and may explain its greater effect on this outcome.
It was no surprise to show that those who endorsed both anxiety and depression (CAD) had the worst reports in all constructs of symptomology, disease management, psychological well-being and QOL. This is a trend that is very common and has been seen in multiple studies within the general population,63 and people with MS.31 Due to the commonality, it is often questioned whether to consider and treat both conditions as the same or distinct. Based on our results, a clear distinction may be made between the role anxiety and depression have on the impact of an individual’s disease, psychological well-being, and QOL. Thus, supporting the importance of clinically diagnosing both disorders separately and considering their treatment in the context of the patient’s presentation and need for intervention. However, in the event that CAD is present, transdiagnostic therapies seem highly appropriate and are likely to result in significant improvement(s) as these individuals appear to have the worst outcomes, consistent with previous findings.
In sum, we hope that the present findings implore researchers and clinicians as to the importance of proper identification and effective treatment of both depression and anxiety in MS. Given the known impact, it is concerning to see that still, very few individuals receive treatment for their depression,64,65 and even less for their anxiety.28 We hope that our findings and the recent work of those referenced within continue to drive home the message that consideration of depression and anxiety in MS is paramount and likely to determine differing trajectories in health, well-being, and QOL for those living with MS.
Despite the study’s strengths, including the large sample size and several different constructs assessed, it is also important to address the limitations of this study. The sample size was primarily female, with a majority diagnosed with relapsing-remitting multiple sclerosis. Future studies with greater variation in disease course, duration, and gender may yield different results. Another limitation is the use of self-report measures of depression and anxiety. Structured clinical interviews would have been preferable. However, it should be noted that using the cutoff of 22 on the CMDI evaluative scale for instance resulted in a lower rates (24%), which has been shown to be more akin to the rates found when using clinical interviews.45,66
Nonetheless, the present study provides important information. While previous research focused on the significant correlations depression had with these constructs, this study identified anxiety as an equal and even greater variable in signaling a risk for worsening MS symptoms, decreased quality of life, and well-being. These results serve as an important reminder for clinicians to diagnose and treat anxiety symptoms, just as importantly as depression. Finally, this research also highlights the importance of educating people with MS on the benefits of providing social support, and consequences of substance use.
Highlights.
Depression and anxiety are both common in multiple sclerosis (MS).
Despite their high prevalence and comorbidity, greater attention has been given to depression in MS.
Much less is known about the impact and risk factors of anxiety in MS.
The present investigation was conducted to develop a better understanding of the impact of depression, anxiety and comorbid depression and anxiety on disease symptoms, disease management, psychological well-being, and quality of life in MS.
We also examined the demographic and disease-related risk factors associated with depression and anxiety and the role of social support and substance use.
Acknowledgments
DECLARATION OF CONFLICT OF INTEREST & FUNDING
This work was supported by the National Institutes of Health National Center for Medical Rehabilitation Research [grant number K23HD069494]
Footnotes
The Authors declare that there is no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Harbo HF, Gold R, Tintoré M. Sex and gender issues in multiple sclerosis. Therapeutic advances in neurological disorders 2013; 6(4): 237–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shnek ZM, Foley FW, LaRocca NG, Smith CR, Halper J. Psychological predictors of depression in multiple sclerosis. Neurorehabilitation and Neural Repair 1995; 9(1): 15–23. [Google Scholar]
- 3.Amato M, Ponziani G. A prospective study on the prognosis of multiple sclerosis. Neurological Sciences 2000; 21(2): S831–S8. [DOI] [PubMed] [Google Scholar]
- 4.Confavreux C, Vukusic S, Adeleine P. Early clinical predictors and progression of irreversible disability in multiple sclerosis: an amnesic process. Brain 2003; 126(4): 770–82. [DOI] [PubMed] [Google Scholar]
- 5.Boeschoten RE, Braamse AM, Beekman AT, et al. Prevalence of depression and anxiety in multiple sclerosis: a systematic review and meta-analysis. Journal of the neurological sciences 2017; 372: 331–41. [DOI] [PubMed] [Google Scholar]
- 6.Marrie RA, Walld R, Bolton JM, et al. Estimating annual prevalence of depression and anxiety disorder in multiple sclerosis using administrative data. BMC research notes 2017; 10(1): 619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pujol J, Bello J, Deus J, Cardoner Ns, Martí-Vilalta JL, Capdevila A. Beck Depression Inventory factors related to demyelinating lesions of the left arcuate fasciculus region. Psychiatry Research: Neuroimaging 2000; 99(3): 151–9. [DOI] [PubMed] [Google Scholar]
- 8.Honer WG, Hurwitz T, Li DK, Palmer M, Paty DW. Temporal lobe involvement in multiple sclerosis patients with psychiatric disorders. Archives of Neurology 1987; 44(2): 187–90. [DOI] [PubMed] [Google Scholar]
- 9.Ron M, Logsdail S. Psychiatric morbidity in multiple sclerosis: a clinical and MRI study. Psychological medicine 1989; 19(4): 887–95. [DOI] [PubMed] [Google Scholar]
- 10.Berg D, Supprian T, Thomae J, et al. Lesion pattern in patients with multiple sclerosis and depression. Multiple sclerosis (Houndmills, Basingstoke, England) 2000; 6(3): 156–62. [DOI] [PubMed] [Google Scholar]
- 11.Zorzon M, Zivadinov R, Nasuelli D, et al. Depressive symptoms and MRI changes in multiple sclerosis. European journal of neurology 2002; 9(5): 491–6. [DOI] [PubMed] [Google Scholar]
- 12.Reischies F, Baum K, Bräu H, Hedde J, Schwindt G. Cerebral magnetic resonance imaging findings in multiple sclerosis: relation to disturbance of affect, drive, and cognition. Archives of neurology 1988; 45(10): 1114–6. [DOI] [PubMed] [Google Scholar]
- 13.Rabins PV, Brooks BR, O’donnell P, et al. Structural brain correlates of emotional disorder in multiple sclerosis. Brain 1986; 109(4): 585–97. [DOI] [PubMed] [Google Scholar]
- 14.Schiffer RB, Babigian HM. Behavioral disorders in multiple sclerosis, temporal lobe epilepsy, and amyotrophic lateral sclerosis: an epidemiologic study. Archives of neurology 1984; 41(10): 1067–9. [DOI] [PubMed] [Google Scholar]
- 15.Huber SJ, Rammohan KW, Bornstein RA, Christy JA. Depressive symptoms are not influenced by severity of multiple sclerosis. Neuropsychiatry, Neuropsychology, & Behavioral Neurology 1993. [Google Scholar]
- 16.Zabad RK, Patten SB, Metz LM. The association of depression with disease course in multiple sclerosis. Neurology 2005; 64(2): 359–60. [DOI] [PubMed] [Google Scholar]
- 17.Siegert R, Abernethy D. Depression in multiple sclerosis: a review. Journal of Neurology, Neurosurgery & Psychiatry 2005; 76(4): 469–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McGuigan C, Hutchinson M. Unrecognised symptoms of depression in a community–based population with multiple sclerosis. Journal of neurology 2006; 253(2): 219–23. [DOI] [PubMed] [Google Scholar]
- 19.Chwastiak L, Ehde DM, Gibbons LE, Sullivan M, Bowen JD, Kraft GH. Depressive symptoms and severity of illness in multiple sclerosis: epidemiologic study of a large community sample. American Journal of Psychiatry 2002; 159(11): 6. [DOI] [PubMed] [Google Scholar]
- 20.Strober LB, Arnett PA. An examination of four models predicting fatigue in multiple sclerosis. Archives of Clinical Neuropsychology 2005; 20(5): 631–46. [DOI] [PubMed] [Google Scholar]
- 21.Alschuler KN, Ehde DM, Jensen MP. The co-occurrence of pain and depression in adults with multiple sclerosis. Rehabilitation psychology 2013; 58(2): 217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lester K, Stepleman L, Hughes M. The association of illness severity, self-reported cognitive impairment, and perceived illness management with depression and anxiety in a multiple sclerosis clinic population. J Behav Med 2007; 30(2): 177–86. [DOI] [PubMed] [Google Scholar]
- 23.Gill S, Santo J, Blair M, Morrow SA. Depressive symptoms are associated with more negative functional outcomes than anxiety symptoms in persons with multiple sclerosis. The Journal of neuropsychiatry and clinical neurosciences 2019; 31(1): 37–42. [DOI] [PubMed] [Google Scholar]
- 24.Turner AP, Williams RM, Bowen JD, Kivlahan DR, Haselkorn JK. Suicidal ideation in multiple sclerosis. Archives of physical medicine and rehabilitation 2006; 87(8): 1073–8. [DOI] [PubMed] [Google Scholar]
- 25.Fernández-Jiménez E, Arnett PA. Impact of neurological impairment, depression, cognitive function and coping on quality of life of people with multiple sclerosis: A relative importance analysis. Multiple Sclerosis Journal 2015; 21(11): 1468–72. [DOI] [PubMed] [Google Scholar]
- 26.Frühwald S, Löffler-Stastka H, Eher R, Saletu B, Baumhackl U. Relationship between symptoms of depression and anxiety and the quality of life in multiple sclerosis. Wiener Klinische Wochenschrift 2001; 113(9): 333–8. [PubMed] [Google Scholar]
- 27.D’Alisa S, Miscio G, Baudo S, Simone A, Tesio L, Mauro A. Depression is the main determinant of quality of life in multiple sclerosis: a classification-regression (CART) study. Disabil Rehabil 2006; 28(5): 307–14. [DOI] [PubMed] [Google Scholar]
- 28.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Multiple Sclerosis Journal 2007; 13(1): 67–72. [DOI] [PubMed] [Google Scholar]
- 29.Bystritsky A, Khalsa SS, Cameron ME, Schiffman J. Current diagnosis and treatment of anxiety disorders. Pharmacy and Therapeutics 2013; 38(1): 30. [PMC free article] [PubMed] [Google Scholar]
- 30.Butler E, Matcham F, Chalder T. A systematic review of anxiety amongst people with Multiple Sclerosis. Multiple sclerosis and related disorders 2016; 10: 145–68. [DOI] [PubMed] [Google Scholar]
- 31.Beiske A, Svensson E, Sandanger I, et al. Depression and anxiety amongst multiple sclerosis patients. European journal of neurology 2008; 15(3): 239–45. [DOI] [PubMed] [Google Scholar]
- 32.Dubayova T, Krokavcova M, Nagyova I, et al. Type D, anxiety and depression in association with quality of life in patients with Parkinson’s disease and patients with multiple sclerosis. Quality of Life Research 2013; 22(6): 1353–60. [DOI] [PubMed] [Google Scholar]
- 33.Bruce JM, Hancock LM, Arnett P, Lynch S. Treatment adherence in multiple sclerosis: association with emotional status, personality, and cognition. Journal of behavioral medicine 2010; 33(3): 219–27. [DOI] [PubMed] [Google Scholar]
- 34.Scott KM, Bruffaerts R, Tsang A, et al. Depression–anxiety relationships with chronic physical conditions: results from the World Mental Health Surveys. Journal of affective disorders 2007; 103(1–3): 113–20. [DOI] [PubMed] [Google Scholar]
- 35.Almeida OP, Draper B, Pirkis J, et al. Anxiety, depression, and comorbid anxiety and depression: risk factors and outcome over two years. International Psychogeriatrics 2012; 24(10): 1622–32. [DOI] [PubMed] [Google Scholar]
- 36.Choi KW, Kim Y-K, Jeon HJ. Comorbid anxiety and depression: clinical and conceptual consideration and transdiagnostic treatment Anxiety Disorders: Springer; 2020: 219–35. [DOI] [PubMed] [Google Scholar]
- 37.Brown LF, Kroenke K, Theobald DE, Wu J, Tu W. The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psycho-Oncology 2010; 19(7): 734–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feinstein A, O’connor P, Gray T, Feinstein K. The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. Multiple Sclerosis Journal 1999; 5(5): 323–6. [DOI] [PubMed] [Google Scholar]
- 39.Charcot J Lectures on the diseases of the nervous system delivered at La Salpetriere (translated by G. Sigerson). London: New Sydenham Society; 1877. [Google Scholar]
- 40.Counsell A, Furtado M, Iorio C, et al. Intolerance of uncertainty, social anxiety, and generalized anxiety: Differences by diagnosis and symptoms. Psychiatry research 2017; 252: 63–9. [DOI] [PubMed] [Google Scholar]
- 41.Turner AP, Alschuler KN. Anxiety is more important than depression in MS–No. Multiple Sclerosis Journal 2018; 24(4): 442–4. [DOI] [PubMed] [Google Scholar]
- 42.Morrow SA. Anxiety is more important than depression in MS–Yes. Multiple Sclerosis Journal 2018; 24(4): 440–1. [DOI] [PubMed] [Google Scholar]
- 43.Spielberger CD, Gorsuch RL. State-trait anxiety inventory for adults: Manual, instrument, and scoring guide: Mind Garden, Incorporated; 1983. [Google Scholar]
- 44.Nyenhuis DL, Luchetta T. The development, standardization, and initial validation of the Chicago Multiscale Depression Inventory. Journal of personality assessment 1998; 70(2): 386401. [DOI] [PubMed] [Google Scholar]
- 45.Strober LB, Arnett PA. Depression in multiple sclerosis: The utility of common self-report instruments and development of a disease-specific measure. Journal of clinical and experimental neuropsychology 2015; 37(7): 722–32. [DOI] [PubMed] [Google Scholar]
- 46.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of personality and social psychology 1989; 56(2): 267. [DOI] [PubMed] [Google Scholar]
- 47.Fisk JD, Ritvo PG, Ross L, Haase DA, Marrie TJ, Schlech WF. Measuring the functional impact of fatigue: initial validation of the fatigue impact scale. Clinical Infectious Diseases 1994; 18(Supplement 1): S79–S83. [DOI] [PubMed] [Google Scholar]
- 48.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research 1989; 28(2): 193–213. [DOI] [PubMed] [Google Scholar]
- 49.Ritvo P, Fischer J, Miller D, Andrews H, Paty D, LaRocca N. Multiple sclerosis quality of life inventory: a user’s manual. New York: National Multiple Sclerosis Society; 1997: 1–65. [Google Scholar]
- 50.Bishop M, Frain M. Development and initial analysis of multiple sclerosis self-management scale. International Journal of MS Care 2007; 9(2): 35–42. [Google Scholar]
- 51.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. Journal of personality assessment 1985; 49(1): 71–5. [DOI] [PubMed] [Google Scholar]
- 52.Diener E, Wirtz D, Tov W, et al. New well-being measures: Short scales to assess flourishing and positive and negative feelings. Social Indicators Research 2010; 97(2): 143–56. [Google Scholar]
- 53.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983; 24(4): 385–96. [PubMed] [Google Scholar]
- 54.Koelmel E, Hughes AJ, Alschuler KN, Ehde DM. Resilience mediates the longitudinal relationships between social support and mental health outcomes in multiple sclerosis. Archives of physical medicine and rehabilitation 2017; 98(6): 1139–48. [DOI] [PubMed] [Google Scholar]
- 55.Krokavcova M, van Dijk JP, Nagyova I, et al. Social support as a predictor of perceived health status in patients with multiple sclerosis. Patient Educ Couns 2008; 73(1): 159–65. [DOI] [PubMed] [Google Scholar]
- 56.Stern BZ, Strober L, DeLuca J, Goverover Y. Subjective well-being differs with age in multiple sclerosis: A brief report. Rehabilitation psychology 2018; 63(3): 474. [DOI] [PubMed] [Google Scholar]
- 57.Butler E, Thomas R, Carolan A, Silber E, Chalder T. ‘It’s the unknown’–understanding anxiety: from the perspective of people with multiple sclerosis. Psychology & health 2019; 34(3): 368–83. [DOI] [PubMed] [Google Scholar]
- 58.Holland D, Schlüter D, Young C, et al. Use of coping strategies in multiple sclerosis: Association with demographic and disease-related characteristics✰. Multiple sclerosis and related disorders 2019; 27: 214–22. [DOI] [PubMed] [Google Scholar]
- 59.Milanlioglu A, Özdemir PG, Cilingir V, Gülec TÇ, Aydin MN, Tombul T. Coping strategies and mood profiles in patients with multiple sclerosis. Arquivos de neuro-psiquiatria 2014; 72(7): 490–5. [DOI] [PubMed] [Google Scholar]
- 60.Tan-Kristanto S, Kiropoulos LA. Resilience, self-efficacy, coping styles and depressive and anxiety symptoms in those newly diagnosed with multiple sclerosis. Psychology, health & medicine 2015; 20(6): 635–45. [DOI] [PubMed] [Google Scholar]
- 61.Feinstein L, Sabates R, Anderson TM, Sorhaindo A, Hammond C. What are the effects of education on health. Proceedings of the Copenhagen Symposium” Measuring the Effects of Education on Health and Civic Engagement; 2006; 2006. [Google Scholar]
- 62.Strober LB, Becker A, Randolph JJ. Role of positive lifestyle activities on mood, cognition, well-being, and disease characteristics in multiple sclerosis. Applied Neuropsychology: Adult 2018; 25(4): 304–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mittal D, Fortney JC, Pyne JM, Edlund MJ, Wetherell JL. Impact of comorbid anxiety disorders on health-related quality of life among patients with major depressive disorder. Psychiatric Services 2006; 57(12): 1731–7. [DOI] [PubMed] [Google Scholar]
- 64.Sullivan MJ, Weinshenker B, Mikail S, Bishop SR. Screening for major depression in the early stages of multiple sclerosis. Canadian journal of neurological sciences 1995; 22(3): 228–31. [DOI] [PubMed] [Google Scholar]
- 65.Mohr DC, Hart S, Fonareva I, Tasch E. Treatment of depression for patients with multiple sclerosis in neurology clinics. Multiple Sclerosis Journal 2006; 12(2): 204–8. [DOI] [PubMed] [Google Scholar]
- 66.Strober L, Arnett P. Assessment of depression in multiple sclerosis: development of a “trunk and branch” model. The Clinical Neuropsychologist 2010; 24(7): 1146–66. [DOI] [PubMed] [Google Scholar]