Abstract
Little is known whether topical analgesic creams, whose natural products enter the blood stream after application, affect myocardial infarct size. Here we tested whether topical analgesic creams can trigger remote cardioprotection and the mechanism involved.
Male Sprague Dawley rats were used for an in vivo rodent model consisting of 30 minutes left anterior descending coronary artery ischemia and 2 hours of reperfusion followed by infarct size assessment. The topical analgesic IcyHot, applied to the abdomen prior to ischemia, reduced myocardial infarct size versus control (41±3* versus 62±1, n=6/group, *P<0.001). In contrast, the topical analgesic creams Preparation H, Aspercreme Heat, or Tiger Balm did not alter infarct size. IcyHot, unlike Preparation H, increased circulating methyl salicylate levels during reperfusion (3.0± 0.6 versus 0.4±0.2 mg/dL, n=6, *P<0.001, measured at the internal jugular vein). Methyl salicylate (10μM) applied to isolated adult cardiac myocytes during reoxygenation reduced cell death when compared to vehicle (21±2%* versus 30±2% of trypan blue positive cells, n=9/group, *P<0.01).
Further, treatment with the TRPA1 inhibitors TCS-5861528 (1μM) or AP-18 (1μM) blocked the methyl salicylate-induced protective effect in isolated adult cardiomyocytes. In intact rodents, either of the TRPA1 inhibitors (1mg/kg, intravenous) given prior to IcyHot topical application blocked IcyHot-induced infarct size reduction. IcyHot also reduced infarct size when applied 24 hours prior to myocardial ischemia or during myocardial ischemia versus control. Together, these findings support IcyHot analgesic cream can trigger remote cardioprotection through releasing methyl salicylate into the bloodstream with cardioprotection occurring by a TRPA1-dependent mechanism.
Keywords: opioids, methyl salicylate, IcyHot, infarct size, cardioprotection, heart
Introduction:
Opioid abuse and addiction are important problems in our society today. As such, there is a societal shift to reduce opioid use. Compared to stronger medications such as opioids, topical ointments are widely used over-the-counter solutions for pain relief which are popular for their easy accessibility and mild side-effects. This is evident since over-the-counter pain relief ointments, according to 2016 Nielsen data, produce an annual revenue of ~$7.48 billion globally [26]. However, not much is known regarding the off-target effects of these topical non-opioid analgesics.
Analgesics are known to impact the cardiovascular system, as cross-talk exists between cellular pathways which signal pain (nociception) and those reducing cellular injury from a heart attack [36]. As for opioids, administration can provide pain relief while concurrently reducing cellular injury from a heart attack [15]. However, little is known about the cardiovascular effects of topical over-the-counter analgesic creams. Therefore, it is important to determine whether over the counter pain relieving creams, frequently accessible without a drug prescription, may be beneficial or perhaps detrimental to the heart during heart attack injury.
The active ingredients of over-the-counter analgesics are typically naturally occurring compounds such as menthol, camphor, and methyl salicylate. In particular, medicinal uses of methyl salicylate (wintergreen oil) are wide-ranging including to reduce inflammation and as a treatment for headaches, pain, and irritable bowel syndrome [29]. Therefore, we tested the hypothesis whether topically applied over-the-counter analgesic creams can reduce myocardial infarct size when administered remotely and the mechanism involved in cardioprotection.
Materials and methods:
Procedures and protocols were approved by the Animal Care and Use Committee at Stanford University, Stanford, California. All animal studies conformed to the National Institute of Health Guide for the Care and Use of Laboratory Animals (NIH Publications No. 85–23 revised in 1996). All animal studies have been approved by the appropriate ethics committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Eight to 10 week old male Sprague-Dawley rats (Charles River) were used for the studies outlined.
Pharmacological Agents Used:
Over the counter analgesics were selected considering the active components and based on the availability at the local grocery store (Safeway, Menlo Park, CA). These included IcyHot, Preparation H, Aspercreme Heat, and Tiger Balm (6g/kg). A number of formulations for each brand name exist, so images of the analgesic creams tested and the active ingredients listed on each label are provided (Figure 1). For additional studies, methyl salicylate (Catalog PHR1214, Sigma) and the TRPA1 receptor antagonists, TCS 5861528 (TCS, 1 mg/kg, Tocris) and AP 18 (AP, 1 mg/kg, Tocris), were dissolved in DMSO. The TRPA1 inhibitor doses used were based upon a prior study [23].
Figure 1. Analgesic creams available without prescription.

A. Images of analgesic creams tested for the study. B. Table of active ingredients in each analgesic cream tested. For each brand name, several different formulations exist. The active ingredients were listed for each cream.
In Vivo Myocardial Infarction Rodent Model:
The model is described in a number of publications [18,19]. After obtaining body weight, rats were anesthetized with Inactin (thiobutabarbital, 100mg/kg intraperitoneal, Sigma, Saint Louis, Missouri). A tracheotomy was performed in addition to cannulation of the carotid artery and internal jugular vein to measure blood pressure and to administer drugs, respectively. Rats were placed on a ventilator (30–40 breaths per minute, tidal volume 8mL/kg) and adjusted to maintain a normal pH (7.35–7.45) and end tidal CO2 (35–45mmHg) by a blood gas machine (Radiometer ABL-80, Cleveland, Ohio). Body temperature was monitored with a rectal thermometer (Thermalert TH-5) and maintained at 36–38°C by heating pads and heat lamps. The heart was exposed by an incision in the fourth intercostal space, the pericardium excised and a suture was placed around the left anterior descending coronary artery (6–0 prolene, Ethicon, Somerville, New Jersey). After surgical manipulation and adjustment of the ventilator settings based upon blood gas analysis, rodents were allowed to stabilize for 30 minutes prior to initiation of the experimental protocol.
The experimental protocol had 13 treatment groups, which are described in detail throughout the manuscript (Figures 2A, 5A, 6A, and 7A). For rodents receiving topical analgesic creams, the abdomen was shaved free of fur in the T10 region. The area of application was 4cm in width (across the abdomen) and 2cm in length with 6g/kg of cream applied to the abdomen. For rodents not treated with analgesic creams, the abdominal region was also shaved as a control. All rats were subjected to 30 minutes of left anterior descending (LAD) coronary artery occlusion followed by 2 hours of reperfusion. Following reperfusion, the LAD was again occluded and the heart negatively stained for the area at risk by injection of patent blue dye (Sigma, St. Louis, Missouri) given through the internal jugular vein. The heart was then excised, both atria and the right ventricle were removed, and the left ventricle was cut into 5 equal slices to create cross-sections from apex to base. The slices were separated into normal zone and area at risk, followed by incubation in 1% TTC to measure viability of myocardial tissue. Viable tissue stained red, while non-viable tissue remained unstained or white. Infarct size as a percentage of area at risk was determined by dissection and weighing of the heart tissue. Heart rate, blood pressure, and rate pressure product were monitored and calculated throughout the experimental protocol using a PowerLab monitoring system (AD Instruments, MLS060/8 PowerLab 4/35).
Figure 2. The effect of analgesic creams on myocardial infarct size in intact rodents.
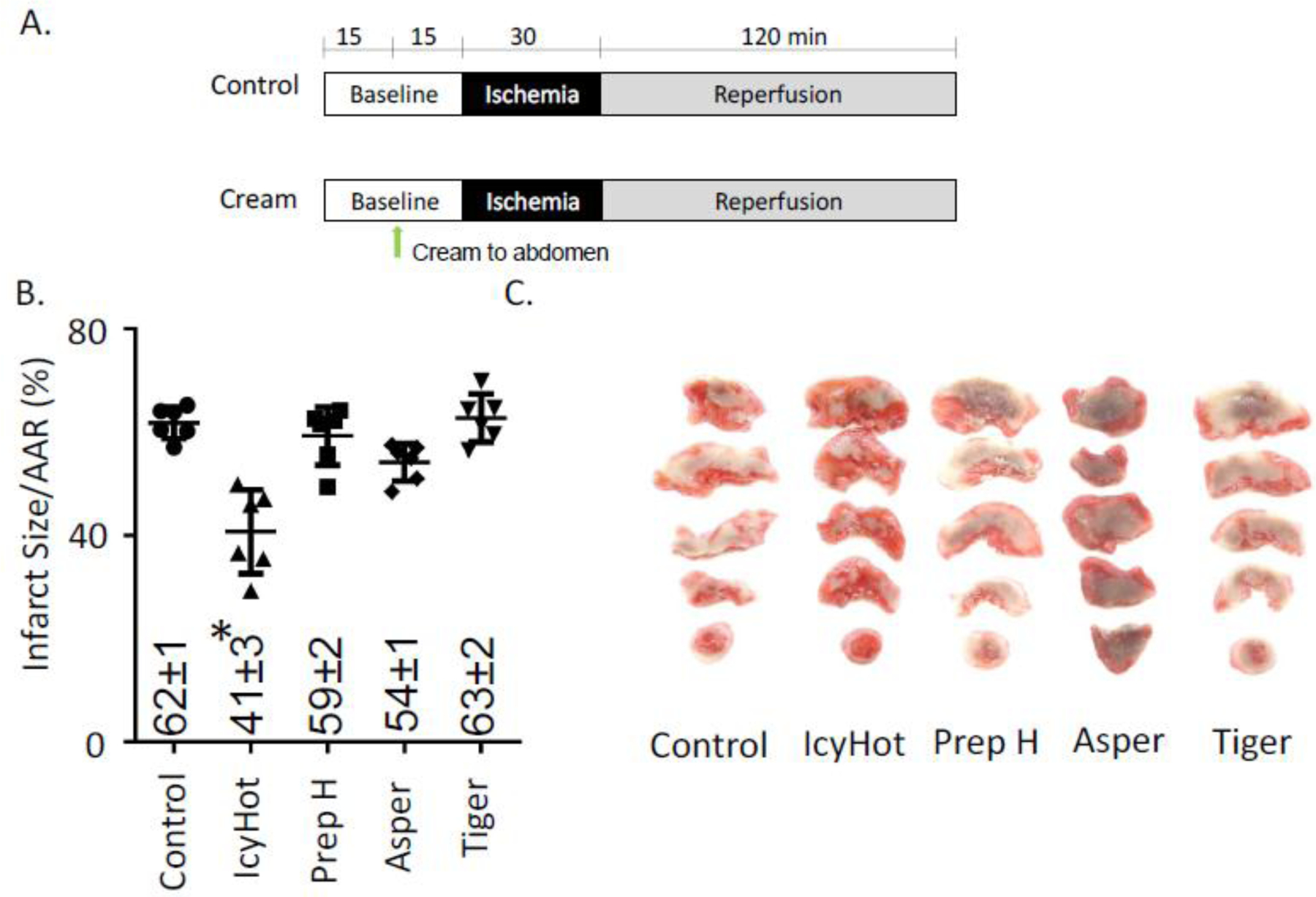
A. Experimental protocol with analgesic cream applied to the abdomen 15 minutes prior to ischemia. B. Infarct size over area at risk percentage for each experimental group. Individual data points for each experiment shown. C. Representative images for area at risk for each experimental group. Infarcted tissue remains unstained (white) while viable tissue is stained red. n=6/group, *P<0.01 versus control using one-way ANOVA with Bonferroni correction.
Figure 5. Dependence of IcyHot-induced myocardial infarct size reduction on TRPA1 in intact rodents.
A. Experimental protocol. B. Infarct size over area at risk percentage for each experimental group. Individual data points for each experiment are shown. A dotted line was drawn to show the effect of IcyHot treatment alone, which was presented in Figure 2B. C. Representative images for area at risk for each experimental group. Infarcted tissue remains unstained (white) while viable tissue is stained red. n=6/group #P<0.01 versus IcyHot using 1-way ANOVA with Bonferroni correction.
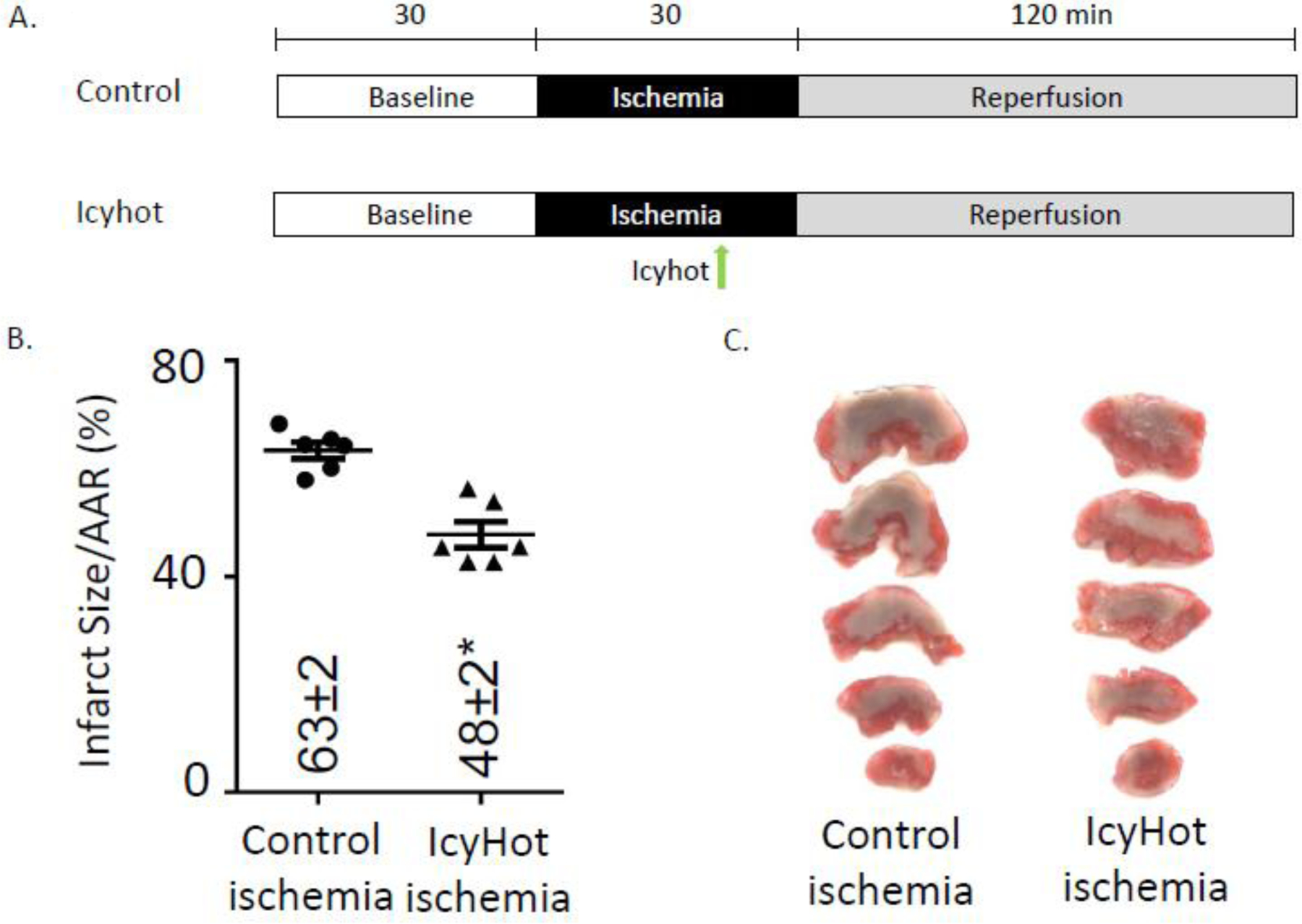
Figure 6. Effect of IcyHot cream on myocardial infarct size when given during ischemia.
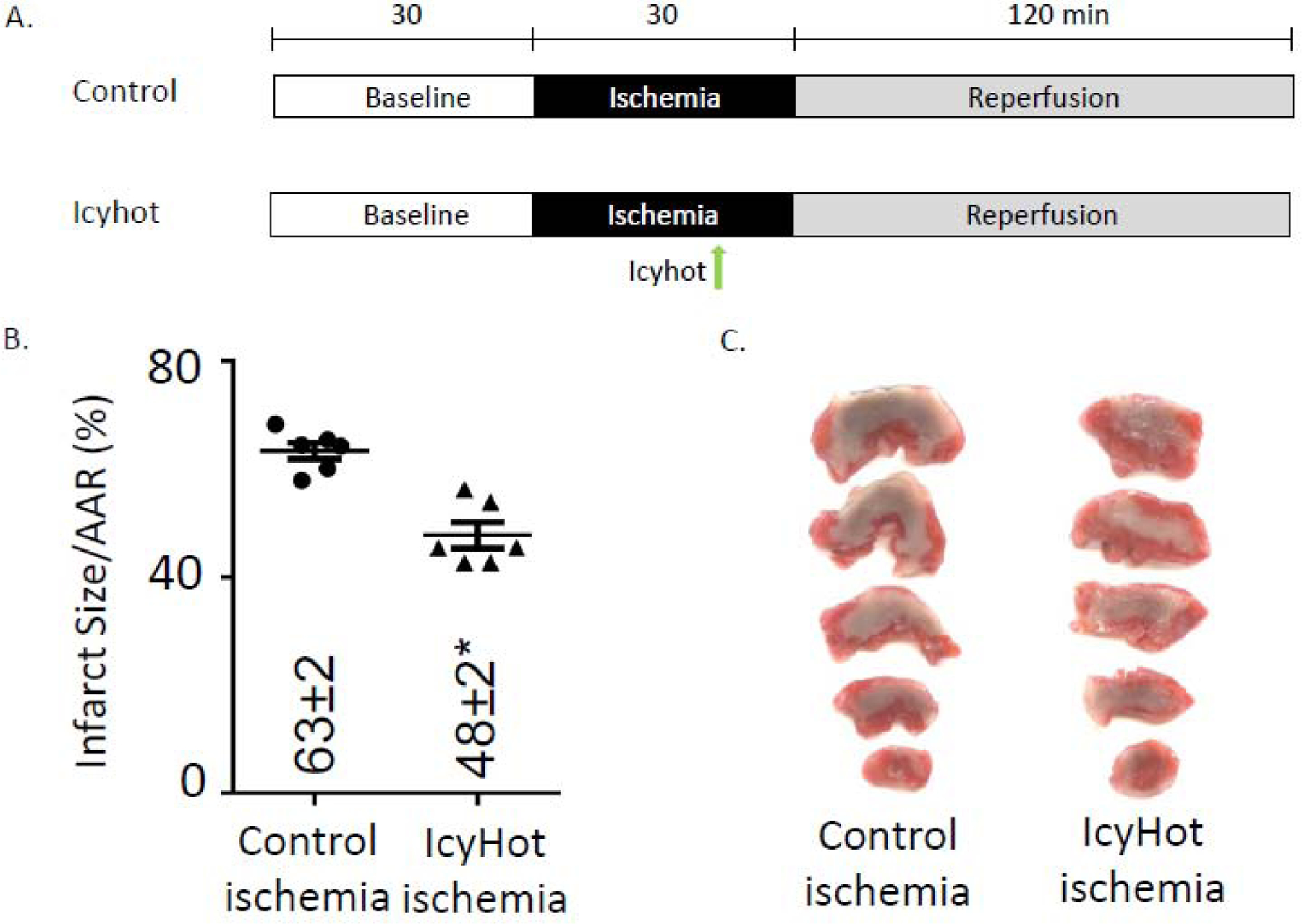
A. Experimental protocol B. Infarct size over area at risk percentage for each experimental group. Individual data points for each experiment shown. C. Representative images for area at risk for each experimental group.
Figure 7. Delayed cardioprotective effect of IcyHot cream on myocardial infarct size when given 24 hours prior to ischemia.
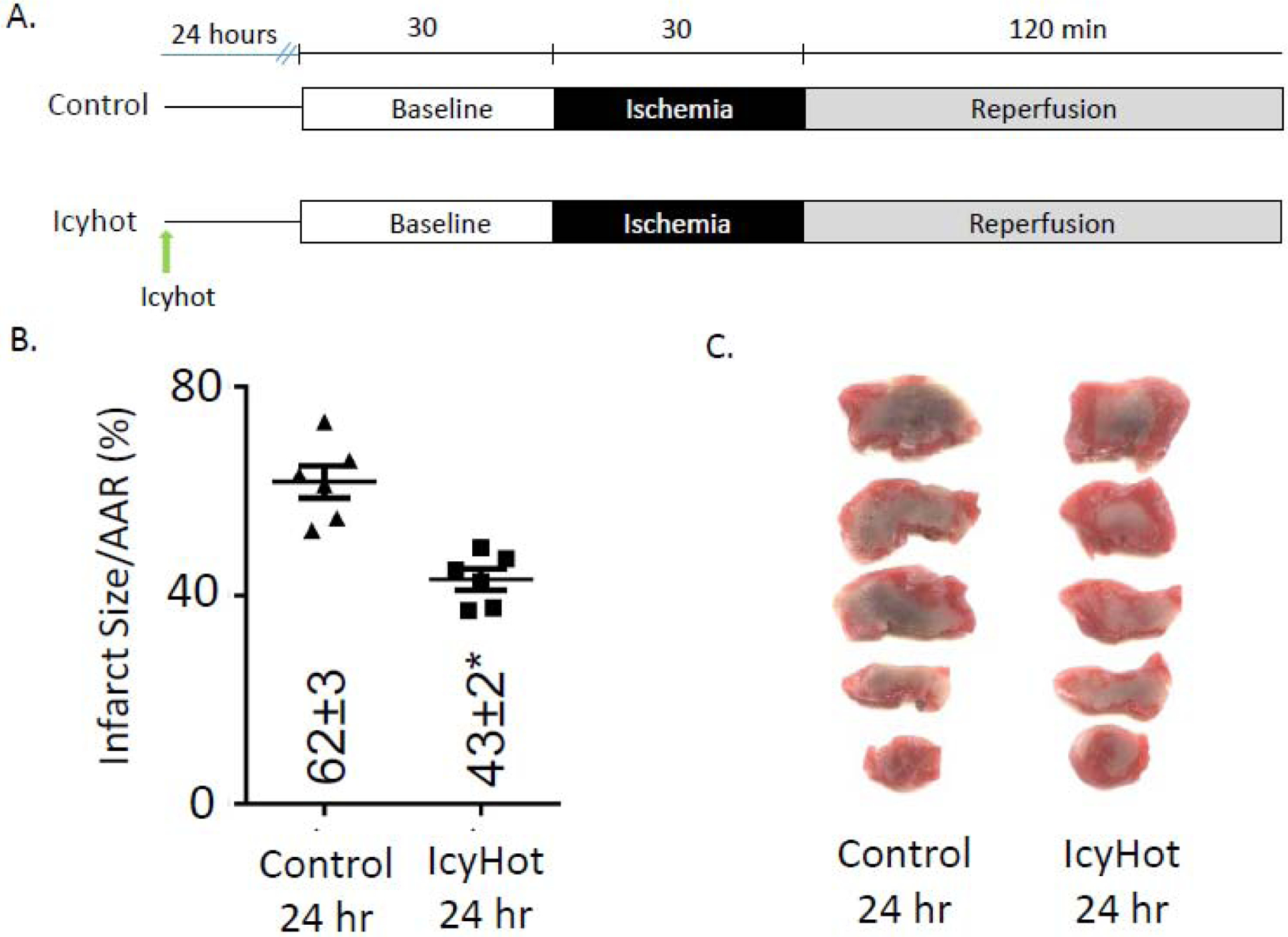
A. Experimental protocol B. Infarct size over area at risk percentage for each experimental group. Individual data points for each experiment shown C. Representative images for area at risk for each experimental group. n=6/group. *P<0.01 versus control using a two-tailed unpaired Student’s t-test.
Measurement of Methyl Salicylate Blood Levels:
Additional rats receiving Icyhot or Preparation H were subjected to 30 minutes of LAD coronary artery occlusion followed by 2 hours of reperfusion. Approximately 0.3 ml of blood was withdrawn at the time of baseline, 15 minutes after application of cream, 5 minutes of reperfusion and 120 minutes of reperfusion. Each blood sample was placed into a heparinized Eppendorf tube for centrifugation at the speed of 3000 r/min for 15 minutes. Separated plasma was frozen at −80°C for assays. Salicylate concentrations were measured using a salicylate ELISA kit (Catalog 133619, Neogen) as per manufacturer instructions.
In Vitro cardiac myocyte hypoxia and reoxygenation injury model:
Adult rat primary cardiac myocytes were isolated from male Sprague-Dawley rat hearts by enzymatic dissociation as previously described [27]. The isolated cardiac myocytes were plated in 4% FBS Medium 199 on laminin coated plates (2μg/cm2) for 2 hours. The plating medium was changed to serum free Medium (1% BSA Medium 199) to remove non-myocytes and cardiomyocytes were incubated at 37 °C in 5% CO2 24 hours prior to experiments in 24 well plates with a seeding density of 5×104.
Experimental groups were divided into a normoxic control group and a hypoxia-reoxygenation group. In the hypoxia-reoxygenation group, cardiac myocytes were given DMSO, or methyl salicylate (0.1μM-1mM) with and without a TRPA1 antagonist (TCS, 1μM, AP, 1μM) immediately before reoxygenation (Figure 4A). For the normoxic control group, cardiac myocytes were also treated with DMSO. Hypoxia was induced by placing the plates into an anaerobic gas pouch (BD Biosciences, GasPak EZ Gas Generating Pouch Systems, Sparks, Maryland) for 2 hours. The pouch creates an anaerobic environment where the oxygen level within the pouch is less than 0.1% [21]. The cells were then removed from the anaerobic gas pouches and reoxygenated within the cell culture incubator for an additional 4 hours.
Figure 4. Isolated adult cardiac myocytes treated with methyl salicylate.
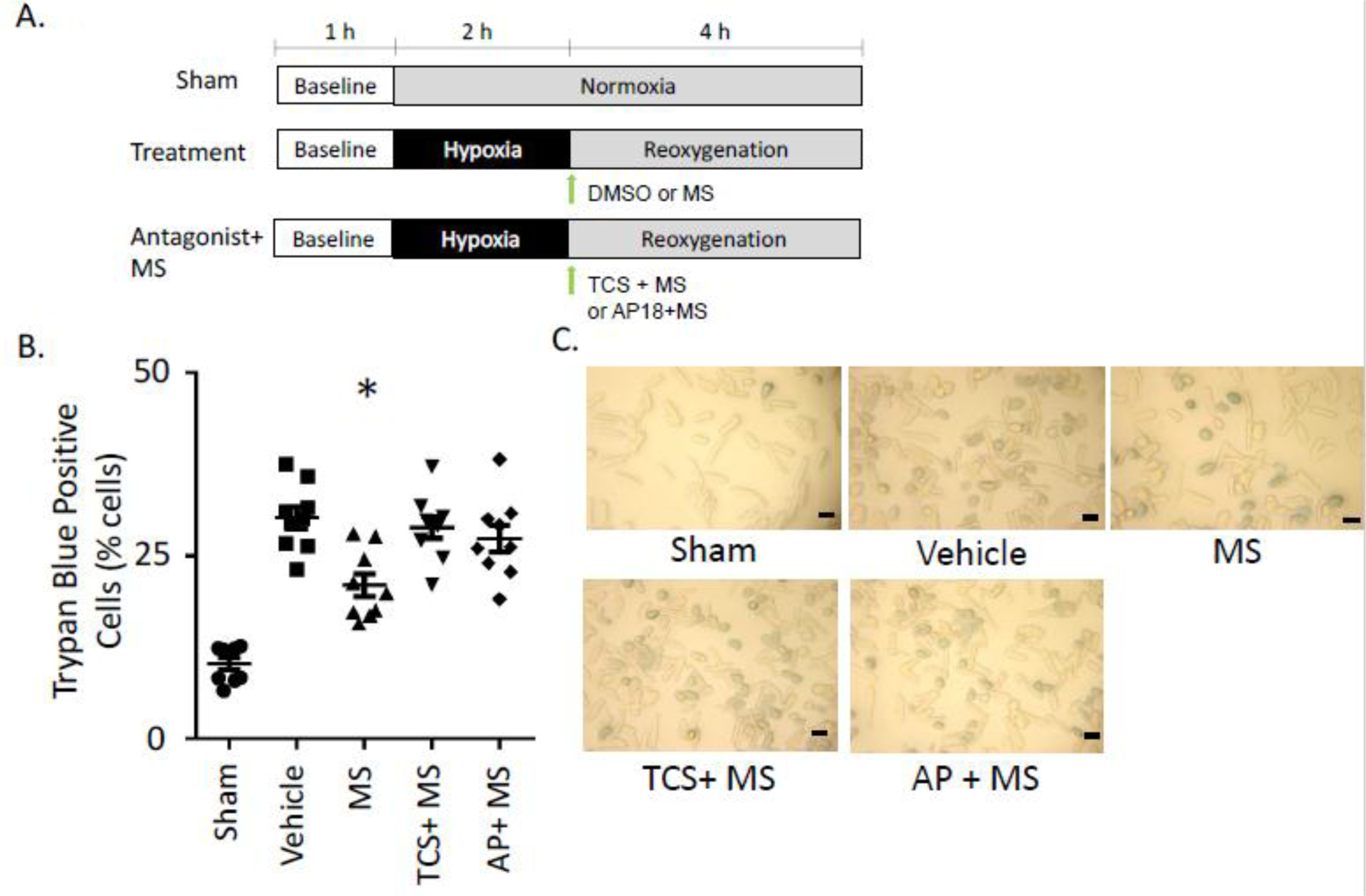
A. Experimental protocol. All agents were given at reoxygenation. B. Percentage of trypan blue positive cells for cardiac myocytes treated with vehicle, methyl salicylate, or a combination of methyl salicylate and TRPA1 inhibitors at reoxygenation C. Representative images of cardiac myocytes after trypan blue staining for each experimental group (black bar represents 50μm), n=9/group, *P<0.05 versus all other groups.
To determine cell death in this model, trypan blue exclusion was used. For the trypan blue experiments after 4 hours of reoxygenation, trypan blue was added to adult cardiac myocytes at a final concentration of 0.04%. To distinguish viable cells from dead cells, two digital images for each experiment were acquired using a camera (Nikon Coolpix 8800) attached to an adapter (MM99 adapter S/N: 1925, Martin Microscope Company, Easley, South Carolina) connected to the microscope (Motic AE21, Xiameng, China). All images were taken within three minutes of trypan blue application to minimize variability associated with changes in the ratio of stained/unstained cells over time. The number of trypan blue positive cells were counted and further expressed as a percentage of the total cells in the image. Approximately 250 cells were counted per well from 2 images.
Statistical Analysis:
All data were presented as mean ± SEM. Based upon our prior intact rodent studies and considering a power analysis with α = 0.05 and 80% power, a minimum of 6 experiments were required for meaningful data [17]. For analysis of in vivo and cardiac myocyte models of ischemia-reperfusion or ischemia-reoxygenation, a one-way ANOVA followed by Bonferroni correction for multiplicity was used in order to compare each group to the control group. A two-way ANOVA was used to determine significance for hemodynamic parameters compared both relative to control with each time point and to baseline measurements within groups. For differences between only two groups, a two tailed unpaired Students t-test was performed. Statistical analysis was performed using GraphPad Prism 6. P < 0.05 was considered statistically significant.
Results
A total of 101 rats were used for the study. 84 rats were used for the in vivo experiments for 78 successful experiments. 8 rats were excluded including 3 rats that died during surgical preparation before group assignment (1 rat secondary to anesthetic overdose and 2 rats secondary to blood loss during experimental preparation), 2 rats in the AP+IcyHot group (1 rat after bradycardia and ventricular fibrillation after injection of AP and the other after intractable ventricular fibrillation during reperfusion) and 1 rat in the group given IcyHot during ischemia (due to intractable ventricular fibrillation during reperfusion). Further, 9 additional rats were used to quantify blood levels of methyl salicylate in IcyHot treated rodents and Preparation H treated rodents for 8 successful experiments. One rat in the Preparation H group was excluded secondary to hypotension during reperfusion. Eight rats were used to isolate adult cardiac myocytes for ischemia-reoxygenation experiments for seven successful cardiomyocyte isolation preparations.
Initially, one of the four analgesic creams were applied to the rodent abdomen 15 minutes prior to ischemia (Figure 2A). IcyHot reduced myocardial infarct size when compared to control (Figure 2B: 41±3%* versus 62±1%, infarct size per area at risk, respectively, n=6/group, *P<0.01 vs control). In contrast, Preparation H, Aspercreme Heat, and Tiger Balm did not affect myocardial infarct size relative to control (Figure 2B: 59±2, 54±1, and 63±2, respectively). Representative images for the area at risk for the four creams and control tested are also presented (Figure 2C). Baseline hemodynamics were not significantly different between the groups relative to control. The rate pressure product in the Preparation H group was significantly greater compared to control at reperfusion, likely due to the systemic absorption of phyenylephrine (Supplemental Table 1). No differences between groups were noted when comparing the size of the area at risk to the left ventricle (Supplemental Figure 1).
Since the analgesic cream IcyHot reducing myocardial infarct size had the natural product methyl salicylate, we quantified the blood concentration of methyl salicylate during the experimental procedure. Blood concentrations of methyl salicylate steadily rose during the experimental protocol when rodents were given IcyHot as opposed to the rodents who were treated with Preparation H (Figure 3, measurement at 5 minutes reperfusion: 3.0 ± 0.6* versus 0.4 ± 0.2 mg/dL and at 2 hours reperfusion: 5.2 ± 0.6* versus 0.3 ± 0.1 mg/dL, n=4/group, *P<0.01).
Figure 3. Salicylate plasma levels after IcyHot application.
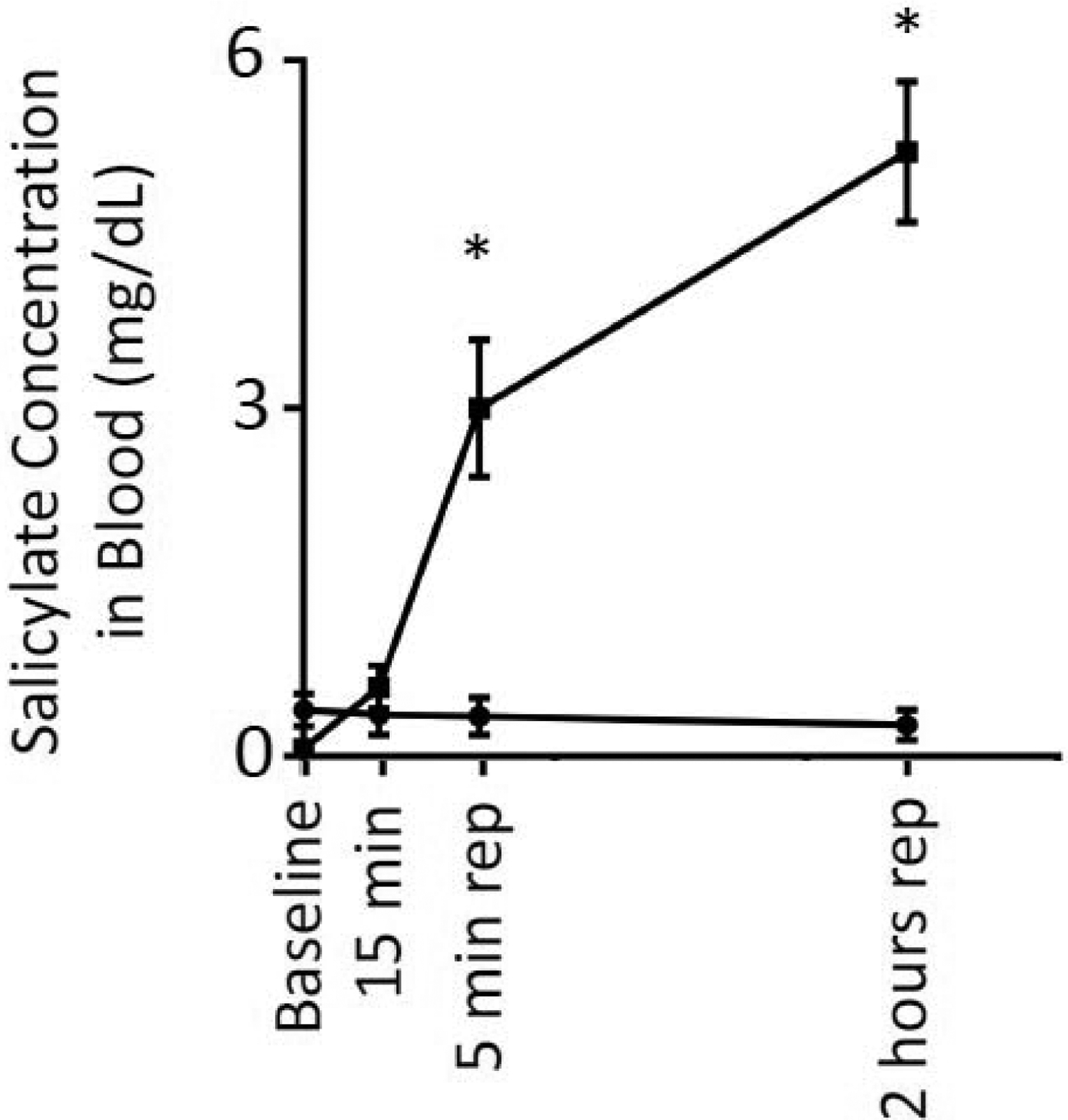
Measurement of plasma levels of methyl salicylate during the time course of the experimental protocol. Measurements were performed at baseline, 15 minutes after cream application, 5 minutes of reperfusion and 2 hours of reperfusion. As a control, plasma samples were obtained from rodents treated with preparation-H. n=4/group, *P<0.01 relative to Preparation H treated rodents for each time point using 2-way ANOVA with Bonferroni correction.
Based upon these concentrations measured, we next determined based on a dose-dependent response how methyl salicylate will affect cellular injury when applied directly to the cardiac myocyte at reoxygenation (Figure 4A). Methyl salicylate dose-dependently reduced the amount of cardiac myocyte cell death versus DMSO vehicle (Supplemental Figure 2: 0.1μM, 30±2%, 1μM 32±3%, 10μM, 23±2*% 100μM, 24±2*%, 1mM, 23±1*%, and 2mM, 22±1*%, versus DMSO, 37±2%, *P<0.01).
Methyl salicylate treatment (10μM, preceded by DMSO treatment) also resulted in nearly a 50% reduction in cell death when compared to DMSO and sham controls (Figure 4B: 21±2*% versus 30±2% and 11±1%, respectively, *P<0.01). This methyl salicylate-induced reduction in cellular injury was also blocked by TRPA1 inhibitors TCS or AP-18 (Figure 4B: 29±1% and 27±2%). Representative bright field for the cardiomyocytes after reoxygenation are also depicted (Figure 4C).
To further determine whether IcyHot reduces cellular injury by a TRPA1-dependent mechanism in vivo, we additionally performed experiments in the presence of TRPA1 inhibitors. Both TRPA1 inhibitors, TCS and AP, blocked the infarct size sparing effect when given intravenously prior to topical IcyHot application to the abdomen (Figure 5B: 62±6% and 58±3%, infarct size/area at risk%, respectively, n=6/group, #P<0.01 versus IcyHot). TCS or AP when given alone had no effect on infarct size compared to control rodents (Figure 5B: 64±2% and 64±2%, respectively). Representative images for the area at risk are also presented (Figure 5C). Baseline hemodynamics were not significantly different between the groups relative to control (Supplemental Table 2). No differences between groups were noted when comparing the size of the area at risk to the left ventricle (Supplemental Figure 3).
We further determined whether administration of IcyHot just prior to reperfusion reduces myocardial infarct size (Figure 6A). Interestingly, IcyHot when given prior to reperfusion reduced myocardial injury versus control (Figure 6B: 48±2* versus 63±2, n=6 per group, *P<0.001). Representative images for the area at risk for the groups are also presented (Figure 6C). We also tested whether IcyHot could provide delayed cardioprotection if applied 24 hours prior to ischemia. IcyHot applied 24 hours prior to ischemia also reduced myocardial infarct size when compared to control (Figure 7B: 43±2* versus 62±3, n=6 per group, *P<0.001). Representative images for the area at risk are also presented (Figure 7C). Baseline hemodynamics were not significantly different between the groups relative to control (Supplemental Table 3). No differences between groups were noted when comparing the size of the area at risk to the left ventricle (Supplemental Figure 4).
Discussion
Since ~81% of people use over the counter medications to treat illnesses and nearly one third of people in the United States have cardiovascular disease, the effects of topical analgesics on the cardiovascular system is important to discern [5, 11]. Our findings support that topical analgesics such as IcyHot have remote cardioprotective benefits in addition to the known benefit of pain relief. This finding is significant since it highlights that natural products in topical analgesics, such as methyl salicylate, can mitigate cell death caused by myocardial ischemia-reperfusion injury. Here, IcyHot is observed to have cardioprotective effects when applied either during myocardial ischemia, immediately prior to ischemia, or up to 24 hours before ischemia. Considering this reduction of cardiac injury has an extended therapeutic window, in addition to the ease of application, IcyHot may be used to develop a novel class of analgesics with an added benefit of remote organ protection.
Based on the therapeutic window for IcyHot, IcyHot can be administered prior to surgeries for a more vulnerable population that are at a higher risk for myocardial infarction. This is important to consider since anywhere from 20–40% of patients that are at high risk for cardiovascular complications during surgery develop a myocardial infarction perioperatively [38]. Application of an analgesic cream 15 minutes before the start of surgery can be performed by an anesthesiologist in the operating room. IcyHot could also be given up to 24 hours prior to surgery by the staff caring for a patient on a hospital floor. IcyHot can also be effective when given during an acute myocardial infarction potentially in the emergency room while waiting for a patient undergo percutaneous coronary angioplasty. Additionally, application in these situations may also have an added benefit of providing analgesia.
Methyl salicylate (a primary active ingredient in IcyHot) when given directly to isolated adult primary cardiac myocytes is also effective in reducing myocardial injury. Generally, the mechanism of action for methyl salicylate is not well known. Previous studies established that 600μM methyl salicylate selectively activates TRPA1 without activating TRPV1 or TRPM8 in CHO cells [6]. In our study, administration of TRPA1 antagonists AP 18 or TCS 5861528 block intra-cellular calcium-mediated influx and the ability for IcyHot or methyl salicylate to reduce cardiac injury. Together, these findings support that the methyl salicylate within IcyHot activates TRPA1 to trigger cardioprotection through calcium-mediated influx.
Although initially TRPA1 was not detectable within the heart by Northern blot, several studies now report the TRPA1 receptor is present and functional within the heart by using PCR, Western blot, and calcium imaging [30, 2, 3, 13, 23]. In addition, TRPA1 agonists such as optovin or ASP 7663 given intravenously limit myocardial infarct size in rodents [23]. In addition, these agonists given to isolated adult cardiac myocytes also prevent cardiac myocyte cell death from hypoxia-reoxygenation, indicating a TRPA1 channel within the cardiomyocyte is important in reducing cellular injury [23]. After TRPA1 is activated in isolated adult cardiomyocytes, cardioprotection is initiated by phosphorylation of Akt [2]. This leads to subsequent triggering of downstream signaling cascades such as inhibiting GSK3β and limiting mPTP opening at the mitochondria; an established molecular basis for cardioprotection by ligands (such as opioids, insulin, adenosine, and bradykinin as well as ischemic preconditioning and postconditioning [16, 20, 37, 10, 31, 33]). Together, these studies support why IcyHot, which contains methyl salicylate, can trigger cardioprotection unlike the other topical analgesics tested that are without methyl salicylate. The mechanism of action likely occurs by triggering a classical pathway of cardioprotection through phosphorylating Akt and triggering the reperfusion injury salvage kinase (RISK) pathway [41].
Reactive aldehydes, such as 4-hydroxynonenal (4-HNE), are generated during myocardial ischemia-reperfusion injury that are detrimental to the cardiomyocyte [24]. The TRPA1 receptor is recognized to selectively respond to oxidative stress and lipid peroxidation products, including the reactive aldehyde 4-HNE [1,32]. Interestingly, the TRPA1 receptor response to oxidative stress is a basic biological mechanism conserved for both mammalian and plant TRPA1 receptors [4]. The TRPA1 receptor is also widely expressed within different cell types including endothelial cells [14]. As such, studies also indicate TRPA1 activation mitigates injury from stroke [28]. Thus, IcyHot cream could have broader applications than just the heart in protecting organs from reperfusion injury and could potentially be leveraged as a general mechanism to prevent organ injury.
In our study, blood levels of methyl salicylate are within the reported therapeutic range of 3–11mg/dL and achieved a value of 3mg/dL at 5 minutes of reperfusion [35]. Based on our data in Figure 3, applying IcyHot to the abdomen provided a continuous delivery of methyl salicylate in the bloodstream throughout the experiment. As such, the mechanism of IcyHot-induced remote cardioprotection is humoral as the depot of methyl salicylate at the abdomen is continuously being delivered to the blood stream to provide cardioprotection. This is supported from human data indicating ~2% of methyl salicylate is absorbed within 30 minutes of application to the skin and reaches 12–20% absorption after several hours with a peak serum concentration at 6 hours [22,25]. This is unlike other remote cardioprotective triggers, such as the neuronal trigger which occurs with an abdominal incision [18] or humoral factors released with remote ischemic preconditioning [34].
However, one concern is that overuse of topical creams containing methyl salicylate in humans (such as 26g of methyl salicylate is applied topically daily for 7 days) can result in salicylate toxicity, which produces symptoms such as metabolic acidosis and respiratory alkalosis secondary to salicylate toxicity [9, 35]. Symptoms of toxicity such as lethargy, tachypnea, diaphoresis, and hyperpyrexia occur when salicylate levels are above the therapeutic range and reported at levels of ~50mg/dL or greater [9, 35]. Since 5mL of purified methyl salicylate is estimated to contain ~7,000mg of salicylate, to avoid potential for toxicity, over the counter formulations typically contain 30% or less of methyl salicylate [12]. Although topical creams containing methyl salicylate are relatively safe to use, it is important to note our study does not encourage applying several tubes of IcyHot on people that actively have an acute myocardial infarction. Overuse of IcyHot may lead to secondary problems such as salicylate toxicity outlined here.
Remote conditioning of the myocardium continues to be an exciting research area since identifying that manipulations targeting the abdomen can reduce myocardial infarct size. Initially, this effect was observed with a surgical incision to the abdomen which reduced myocardial infarct size by 81% in mice termed remote preconditioning of trauma [39]. This was extended in a seminal study discovering that application of capsaicin cream also reduces infarct size by 85% reduction when applied to the abdomen in mice [40]. The infarct size sparing effects of remote preconditioning of trauma and capsaicin cream were also confirmed to occur in rats [18, 19]. Our results are important within the context of these prior findings since IcyHot belongs to a class of analgesic rubs widely used for musculoskeletal pain rather than capsaicin creams which are less commonly used and applied to joints to treat pain from arthritis.
Our study should be interpreted within the context of potential limitations. Although we did not test a methyl salicylate only formulation, the findings provided here are for topical analgesic creams which are available for use by people. A methyl salicylate only formulation is not sold or available to people. Although it cannot be excluded that the menthol in IcyHot could act synergistically with methyl salicylate to reduce myocardial infarct size, analgesic creams containing menthol were tested for our study (Tiger Balm and Aspercreme Heat) and failed to reduce myocardial infarct size. It is also well established that menthol activates TRPM8 and menthol given to TRPA1 knockout trigeminal neurons retain equivocal levels of calcium-mediated influx versus wild type TRPA1 rodents [8]. Therefore, it is unlikely menthol contributed to the infarct size sparing effect seen with IcyHot. Although we also did explore the timing of IcyHot cream administration relative to infarct size reduction for this study, we did not further delve into the molecular mechanism involved, including whether TRPA1 activation acts as a trigger or end effector when IcyHot was applied 24 hours prior to a myocardial infarction. Further, although we provide initial evidence suggesting the mechanism of IcyHot cream application is humoral, we cannot exclude the possibility that there is a neuronal component of this cardioprotection. To address this question, further studies will be needed that may eliminate neuronal signaling from the abdomen such as ligating the spinal cord prior to application of IcyHot cream to the abdomen as described in prior studies of remote cardioprotection [40].
In summary, here we describe how the analgesic cream IcyHot reduces myocardial injury remotely when applied to the abdomen 24 hours, just prior to, or during myocardial ischemia (Figure 8). These findings suggest that in addition to relieving pain, topical analgesic creams can provide the secondary benefit of reducing cellular injury during a heart attack. Using analgesic creams such as IcyHot for cardioprotection has promising translational potential for humans, as they are low-cost, widely available, and can easily be applied to the abdomen.
Figure 8. Summary Figure.
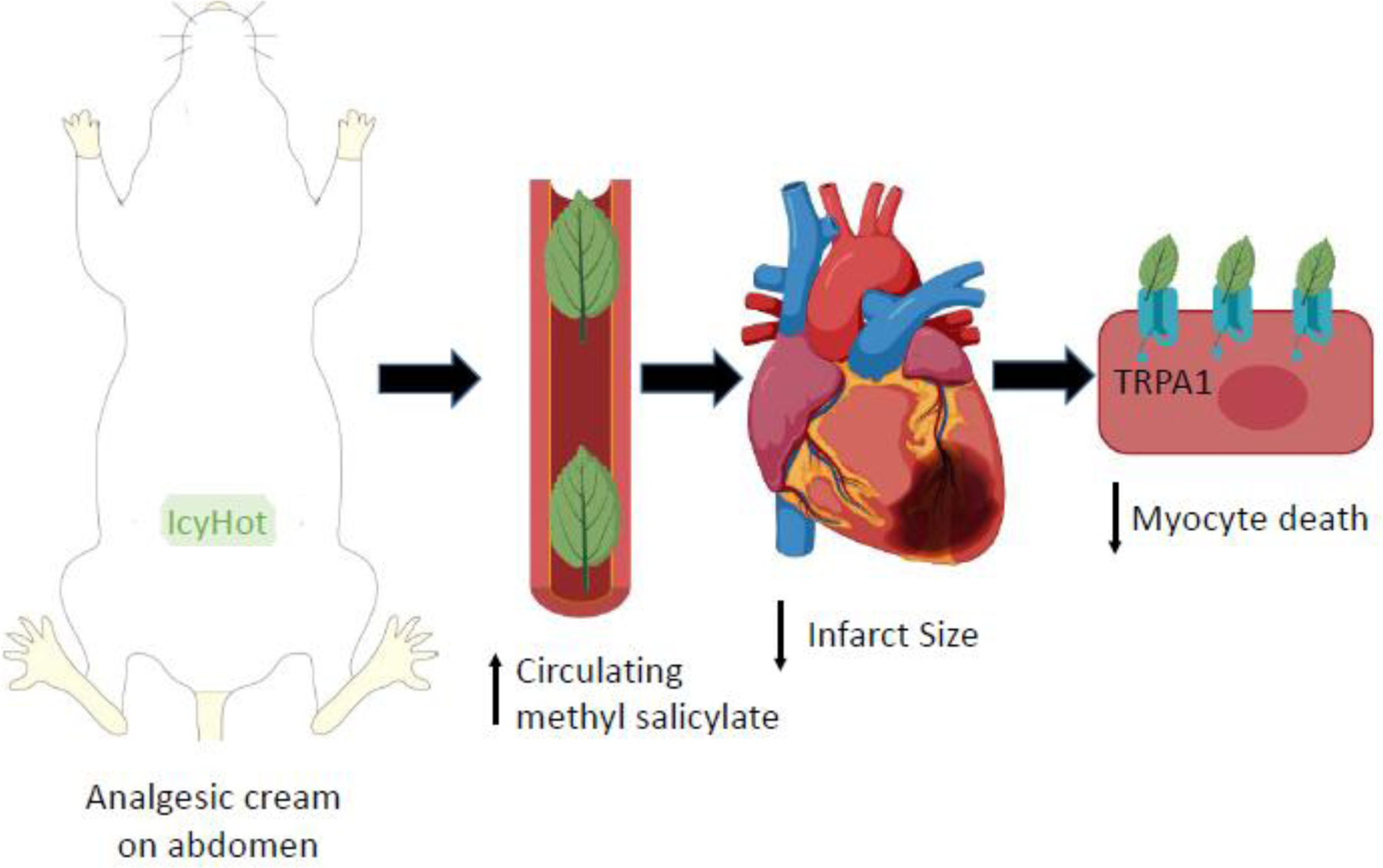
Applying IcyHot to the abdomen causes a depot of methyl salicylate to be absorbed and distributed to the bloodsteam for circulation. This results in a reduction in myocardial infarct size and occurs in a TRPA1-dependent mechanism.
Supplementary Material
Brief Commentary:
Background:
Over the counter topical analgesic creams are widely used and in 2019, ~725 million dollars of creams were sold in the United States. As there is a shift in using non-opioid therapies to treat pain secondary to the abuse and misuse of opioids, it is important to determine whether over the counter analgesics have off-target cardiovascular effects.
Translational Significance:
Using a rodent model of heart attack injury, we find the topical analgesic cream IcyHot reduces myocardial infarct size through the activation of TRP ankyrin 1 (TRPA1) indicating some topical analgesic creams may have unexpected cardiovascular benefits.
Acknowledgements:
Portions of the graphical abstract were created with Biorender. All authors declare no potential conflicts of interest and have read the journal’s authorship statement. All authors do not have any financial or personal relationships with organizations that could potentially influence this described research. This work was supported by the National Natural Science Foundation of China (81900316 to YW) and National Institutes of Health, National Institute of General Medical Sciences (GM119522 to ERG).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References:
- 1.Andersson DA, Gentry C, Moss S, Bevan S (2008) Transient receptor potential A1 is a sensory receptor for multiple products of oxidative stress. J Neurosci 28:2485–2494. doi: 10.1523/JNEUROSCI.5369-07.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrei SR, Ghosh M, Sinharoy P, Damron DS (2019) Stimulation of TRPA1 attenuates ischemia-induced cardiomyocyte cell death through an eNOS-mediated mechanism. Channels (Austin) 13:192–206. doi: 10.1080/19336950.2019.1623591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrei SR, Sinharoy P, Bratz IN, Damron DS (2016) TRPA1 is functionally co-expressed with TRPV1 in cardiac muscle: Co-localization at z-discs, costameres and intercalated discs. Channels (Austin) 10:395–409. doi: 10.1080/19336950.2016.1185579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arenas OM, Zaharieva EE, Para A, Vasquez-Doorman C, Petersen CP, Gallio M (2017) Activation of planarian TRPA1 by reactive oxygen species reveals a conserved mechanism for animal nociception. Nat Neurosci 20:1686–1693. doi: 10.1038/s41593-017-005-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Association of Consumer healthcare products, information on website https://www.chpa.org/MarketStats.aspx, assessed August 3, 2019.
- 6.Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, Earley TJ, Patapoutian A (2004) Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron 41:849–857. doi: 10.1016/S0896-6273(04)00150-3 [DOI] [PubMed] [Google Scholar]
- 7.Bang S, Kim KY, Yoo S, Kim YG, Hwang SW (2007) Transient receptor potential A1 mediates acetaldehyde-evoked pain sensation. Eur J Neurosci 26:2516–2523. doi: 10.1111/j.1460-9568.2007.05882.x [DOI] [PubMed] [Google Scholar]
- 8.Bautista DM, Jordt SE, Nikai T, Tsuruda PR, Read AJ, Poblete J, Yamoah EN, Basbaum AI, Julius D (2006) TRPA1 mediates the inflammatory actions of environmental irritants and proalgesic agents. Cell 124:1269–1282. doi: 10.1016/j.cell.2006.02.023 [DOI] [PubMed] [Google Scholar]
- 9.Bell AJ, Duggin G (2002) Acute methyl salicylate toxicity complicating herbal skin treatment for psoriasis. Emerg Med (Fremantle) 14:188–190. doi: 10.1046/j.1442-2026.2002.00316.x [DOI] [PubMed] [Google Scholar]
- 10.Bell RM, Yellon DM (2003) Bradykinin limits infarction when administered as an adjunct to reperfusion in mouse heart: the role of PI3K, Akt and eNOS. J Mol Cell Cardiol 35:185–193. doi: 10.1016/S0022-2828(02)00310-3 [DOI] [PubMed] [Google Scholar]
- 11.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, Vanwagner LB, Wilkins JT, Wong SS, Virani SS (2019) Heart Disease and Stroke Statistics—2019 Update: A Report From the American Heart Association. Circulation. 139:e56–e528 doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 12.Chan TY (1996) The risk of severe salicylate poisoning following the ingestion of topical medicaments or aspirin. Postgrad Med J 72:109–112. doi: 10.1136/pgmj.72.844.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conklin DJ, Guo Y, Nystoriak MA, Jagatheesan G, Obal D, Kilfoil PJ, Hoetker JD, Guo L, Bolli R, Bhatnagar A (2019) TRPA1 channel contributes to myocardial ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol 316:H889–H899. doi: 10.1152/ajpheart.00106.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earley S, Gonzales AL, Crnich R (2009) Endothelium-dependent cerebral artery dilation mediated by TRPA1 and Ca2+-Activated K+ channels. Circ Res 104:987–994. doi: 10.1161/CIRCRESAHA.108.189530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gross ER, Hsu AK, Gross GJ (2004) Opioid-induced cardioprotection occurs via glycogen synthase kinase beta inhibition during reperfusion in intact rat hearts. Circ Res 94:960–966. doi: 10.1161/01.RES.0000122392.33172.09 [DOI] [PubMed] [Google Scholar]
- 16.Gross ER, Hsu AK, Gross GJ (2007) GSK3beta inhibition and K(ATP) channel opening mediate acute opioid-induced cardioprotection at reperfusion. Basic Res Cardiol 102:341–349. doi: 10.1007/s00395-007-0651-6 [DOI] [PubMed] [Google Scholar]
- 17.Gross ER, Hsu AK, Gross GJ (2009) Acute methadone treatment reduces myocardial infarct size via the delta-opioid receptor in rats during reperfusion. Anes Analg 109:1395–1402. doi: 10.1213/ANE.0b013e3181b92201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gross ER, Hsu AK, Urban TJ, Mochly-Rosen D, Gross GJ (2013) Nociceptive-induced myocardial remote conditioning is mediated by neuronal gamma protein kinase C. Basic Res Cardiol 108:381. doi: 10.1007/s00395-013-0381-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurt CM, Lu Y, Stary CM, Piplani H, Small BA, Urban TJ, Qvit N, Gross GJ, Mochly-Rosen D, Gross ER (2016) Transient Receptor Potential Vanilloid 1 Regulates Mitochondrial Membrane Potential and Myocardial Reperfusion Injury. J Am Heart Assoc 26 5 doi: 10.1161/JAHA.116.003774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jonassen AK, Sack MN, Mjos OD, Yellon DM (2001) Myocardial protection by insulin at reperfusion requires early administration and is mediated via Akt and p70s6 kinase cell-survival signaling. Circ Res 89:1191–1198. doi: 10.1161/hh2401.101385 [DOI] [PubMed] [Google Scholar]
- 21.Keysar SB, Trncic N, Larue SM, Fox MH (2010) Hypoxia/reoxygenation-induced mutations in mammalian cells detected by the flow cytometry mutation assay and characterized by mutant spectrum. Radiat Res 173:21–26. doi: 10.1667/RR1838.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lotte C, Wester RC, Rougier A, Maibach HI (1993) Racial differences in the in vivo percutaneous absorption of some organic compounds: a comparison between black, Caucasian and Asian subjects. Arch Dermatol Res 284:456–459. doi: 10.1007/BF00373356 [DOI] [PubMed] [Google Scholar]
- 23.Lu Y, Piplani H, McAllister SL, Hurt CM, Gross ER (2016) Transient Receptor Potential Ankyrin 1 Activation within the Cardiac Myocyte Limits Ischemia-reperfusion Injury in Rodents. Anesthesiology 125:1171–1180. doi: 10.1097/ALN.0000000000001377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mali VR, Palaniyandi SS (2014) Regulation and therapeutic strategies of 4-hydroxy-2-nonenal metabolism in heart disease. Free Radic Res 48:251–263. doi: 10.3109/10715762.2013.864761 [DOI] [PubMed] [Google Scholar]
- 25.Morra P, Bartle WR, Walker SE, Lee SN, Bowles SK, Reeves RA (1996) Serum concentrations of salicylic acid following topically applied salicylate derivatives. Ann Pharmacother 30:935–940. doi: 10.1177/106002809603000903 [DOI] [PubMed] [Google Scholar]
- 26.Pallavi MS (2018) Topical Pain Relief Market by Therapeutic Class (Non-Opioids and Opioids), Type (Prescription Pain Relief and Over-the-Counter Pain Relief), Formulation (Cream, Gel, Spray, Patch, and Others) and Distribution Channel (Pharmacies & Drug Stores, e-Commerce, and Retail & Grocery Stores) - Global Opportunity Analysis and Industry Forecast, 2018–2025, Allied Market Research.
- 27.Patel HH, Head BP, Petersen HN, Niesman IR, Huang D, Gross GJ, Insel PA, Roth DM (2006) Protection of adult rat cardiac myocytes from ischemic cell death: role of caveolar microdomains and delta-opioid receptors. Am J Physiol Heart Circ Physiol 291:H344–350. doi: 10.1152/ajpheart.01100.2005 [DOI] [PubMed] [Google Scholar]
- 28.Pires PW, Earley S (2018) Neuroprotective effects of TRPA1 channels in the cerebral endothelium following ischemic stroke. Elife. pii: e35316. doi: 10.7554/eLife.35316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spirling LI, Daniels IR (2001) Botanical perspectives on health Peppermint: more than just an after-dinner mint. J R Soc Promot Helath 121:62–63. doi: 10.1177/146642400112100113 [DOI] [PubMed] [Google Scholar]
- 30.Story GM, Peier AM, Reeve AJ, Eid SR, Mosbacher J, Hricik TR, Earley TJ, Hergarden AC, Andersson DA, Hwang SW, McIntyre P, Jegla T, Bevan S, Patapoutian A (2003) ANKTM1, a TRP-like channel expressed in nociceptive neurons, is activated by cold temperatures. Cell 112:819–829. doi: 10.1016/s0092-8674(03)00158-2 [DOI] [PubMed] [Google Scholar]
- 31.Tong H, Chen W, Steenbergen C, Murphy E (2000) Ischemic preconditioning activates phosphatidylinositol-3-kinase upstream of protein kinase C. Circ Res 87:309–315. doi: 10.1161/01.res.87.4.309 [DOI] [PubMed] [Google Scholar]
- 32.Trevisani M, Siemens J, Materazzi S, Bautista DM, Nassini R, Campi B, Imamachi N, Andre E, Patacchini R, Cottrell GS, Gatti R, Basbaum AI, Bunnett NW, Julius D, Geppetti P (2007) 4-Hydroxynonenal, an endogenous aldehyde, causes pain and neurogenic inflammation through activation of the irritant receptor TRPA1. Proc Natl Acad Sci U S A 104:13519–13524. doi: 10.1073/pnas.0705923104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsang A, Hausenloy DJ, Mocanu MM, Yellon DM (2004) Postconditioning: a form of “modified reperfusion” protects the myocardium by activating the phosphatidylinositol 3-kinase-Akt pathway. Circ Res 95:230–232. doi: 10.1161/01.RES.0000138303.76488.fe [DOI] [PubMed] [Google Scholar]
- 34.Tsibulnikov SY, Maslov LN, Gorbunov AS, Voronkov NS, Boshchenko AA, Popov SV, Prokudina ES, Singh N, Downey JM (2019) A Review of Humoral Factors in Remote Preconditioning of the Heart. J Cardiovasc Pharmacol Ther 24:403–421. doi: 10.1177/1074248419841632 [DOI] [PubMed] [Google Scholar]
- 35.Wong A, Mac K, Aneman A, Wong J, Chan BS (2016) Modern Intermittent Haemodialysis (IHD) is an Effective Method of Removing Salicylate in Chronic Topical Salicylate Toxicity. J Med Toxicol 12:130–133. doi: 10.1007/s13181-015-0502-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu Y, Heymann HM, Gross ER (2018) Non-opioid analgesic use and concerns for impaired organ protection. Br J Anaesth 120:403–405. doi: 10.1016/j.bja.2017.11.070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang XM, Krieg T, Cui L, Downey JM, Cohen MV (2004) NECA and bradykinin at reperfusion reduce infarction in rabbit hearts by signaling through PI3K, ERK, and NO. J Mol Cell Cardiol 36:411–421. doi: 10.1016/j.yjmcc.2003.12.008 [DOI] [PubMed] [Google Scholar]
- 38.Flood C, Fleisher LA (2007) Preparation of the noncardiac patient for cardiac surgery. Am Fam Physician 75:656–665. [PubMed] [Google Scholar]
- 39.Ren X, Wang Y, Jones WK (2004) TNF-a is required for late ischemic preconditioning but not for remote preconditioning of trauma. Journal of Surgical Research 121: 120–129. doi: 10.1016/j.jss.2004.03.010 [DOI] [PubMed] [Google Scholar]
- 40.Jones WK, Fan GC, Liao S, Zhang JM, Want Y, Weintraub NL, Kranias EG, Schultz JE, Lorenz J, Ren X (2009) Peripheral nociception associated with surgical incision elicits remote nonischemic cardioprotection via neurogenic activation of protein kinase c signaling. Circulation 120: S1–S9. doi: 10.1161/CIRCULATIONAHA.108.843938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rossello X, Yellon DM. (2018) The RISK pathway and beyond. Basic Res Cardiol 113(1):2 doi: 10.1007/s00395-017-0662-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


