Abstract
Background and aims
Health care workers (HCWs) are at increased risk of getting infected with Coronavirus disease 2019 (COVID-19) and suboptimal preventive practices have been identified as an important risk factor in this regard. This study was done to evaluate the preventive practices being followed by health care workers and identify reasons for suboptimal compliance.
Methods
A cross-sectional survey was done in HCWs belonging to various occupational roles and socio-cultural backgrounds across India through online platforms and telephonic interviews from July 30, 2020 to August 30, 2020. A scientifically designed and pre-validated questionnaire with good validity (CVR = 0.87, S-CVI/Av = 0.978) and internal consistency (Cronbach’s alpha coefficient = 0.85) was used.
Results
The responses of 956 participants were analysed. Various suboptimal practices like touching outer surface of masks, lack of social distancing in cafeteria and duty rooms, inability to wash hands for adequate duration and properly follow steps of hand hygiene, inability to don and doff PPE properly, carrying PPE to duty rooms before completely doffing, use of personal mobile phones during duty and improper sleep were identified. Lack of knowledge, long duty hours, shortage of PPE, high patient workload, and casual attitude regarding own safety were identified as important barriers. Resident doctors and paramedical staff in the age group 18–30 years reported lower adherence.
Conclusions
Suboptimal compliance in preventive practices like handling PPE, distancing in cafeteria/duty rooms and hand hygiene is not uncommon in HCWs. Certain barriers are identified which should be addressed to ensure adequate safety of HCWs against COVID-19.
Keywords: COVID-19, Pandemic, Prevention, Health care workers, Survey
Abbreviations: COVID-19, Coronavirus Disease 2019; HCWs, Healthcare workers; PPE, Personal Protective Equipment
1. Introduction
Being at the front line of the Coronavirus Disease (COVID-2019) pandemic, health care workers (HCWs) are at increased risk of getting infected due to occupational exposure to the SARS-Cov2 virus. The infection in HCWs further compromises the occupational health of the remaining workforce and reduces the capability of the system to cater to sick patients [1]. This issue is of vital importance to all HCWs, especially to those with older age and comorbidities like diabetes mellitus, underlying chronic organ dysfunction, etc.
The incidence of infection in HCWs has been reported up to 39% and HCWs are at least an 11-fold higher risk of getting infected compared to the general population [2,3]. Various studies have identified suboptimal handwashing, improper use and reuse of personal protective equipment (PPE), and working in high-risk department as important risk factors for infection [[3], [4], [5]]. Thus, adherence to proper preventive practices is crucial, especially in the absence of a vaccine. Several studies have been done to assess preventive practices of HCWs but there is a dearth of studies evaluating various aspects of these practices comprehensively and using validated tools to do so. Also, there is a dearth of studies dwelling into the reasons for suboptimal practices and none of the studies have been done in the Indian subcontinent so far.
Therefore, we undertook this cross-sectional survey to evaluate the adherence of various HCWs to preventive practices against COVID-19 in India and reasons for suboptimal compliance in them. It would also help in identifying loopholes in the system and recognizing vulnerable sections among HCWs. This will enable policymakers to take corrective steps to promote the workplace safety of HCWs and reduce the spread of COVID-19.
2. Materials and methods
A cross-sectional survey was conducted on HCWs across India after approval from the Ethics Committee of the institute (reference number: IECPG/246/6/2020). Informed consent was obtained from all the participants in the study.
2.1. Study design and setting
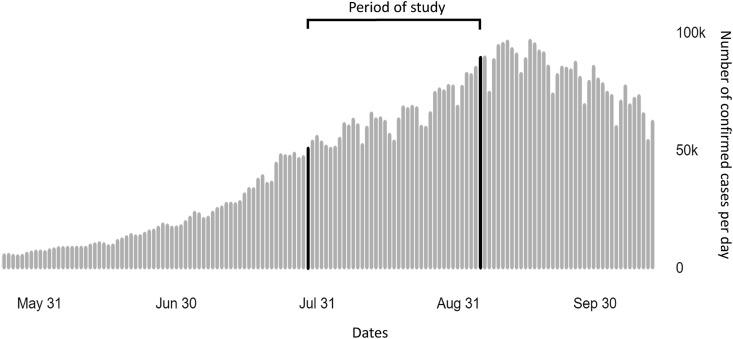
The cross-sectional survey was done among HCWs involved in direct patient care across India using web-based questionnaires and telephonic interviews from July 30, 2020 to August 30, 2020 (Fig. 1 ). An online questionnaire using Google forms was created by utilizing a pre-validated tool containing 56 items.
Fig. 1.
The study was conducted during the rise of COVID-19 in India with transmission classification as cluster of cases. Source: WHO Coronavirus Disease (COVID-19) dashboard for India [6].
2.2. Study participants
The HCWs belonging to various occupational cadres and diverse socioeconomic backgrounds were recruited using purposive and snowball sampling techniques. The HCWs working in both government and non-government sectors were recruited from various states across India. All HCWs involved in patient care in various settings viz. inpatient, outpatient, and laboratory services were included. The HCWs not involved in direct patient management like pharmacists, administrative staff, and undergraduate students, etc. along with those who didn’t give consent were excluded.
2.3. Data collection
Based on the social network of authors and the participants, frontline HCWs were contacted through email, WhatsApp messenger, and phone calls. The weblink of the online questionnaire was then sent to them. For participants facing technical difficulty in filling the questionnaire online, it was administered through telephonic interviews by the authors and the data was entered on the online form simultaneously. Adequate representation of participants was ensured from all zones of India. The questionnaire was also translated into regional languages to facilitate the survey.
2.4. Variables
The independent variables were age, gender, marital status, occupational role, area of posting, and type of patients being seen. The outcome measures (dependent variables) included the extent of preventive practices being followed and reasons for deficiencies in the practices.
2.5. Study tool
A scientifically designed and pre-validated questionnaire developed on the Indian population was used in the study [7]. The questionnaire has good validity (CVR = 0.87, S-CVI/Av = 0.978) and internal consistency (Cronbach’s alpha coefficient = 0.85). The questionnaire contains 56 items arranged in 2 sections: Section A consists of 29 items for assessment of preventive practices in major areas viz. hand hygiene, social distancing, proper use of personal protective equipment (PPE), fomites, exposure, and lifestyle while section B consists of 27 items for evaluation of reasons for deficiencies in the suboptimal preventive practices. Socio-demographic details including age, gender, marital status, occupational role, residence, place of posting (viz. outpatient department/ward/intensive care unit/Operation Theatre/laboratory/emergency), area of posting (whether COVID-19 designated area or not), and type of patients being seen (COVID-19 positive/suspect or negative) were also asked from the participants.
2.6. Sample size
Based on the previous study observing 10.3% of the population to be following suboptimal preventive practices [8], the sample size required for the precision of 2% at 95% confidence interval was calculated to be 887. Thus, enrolment of at least 887 participants was targeted.
2.7. Statistical analysis
The data collected through Google forms were cleaned and coded using Microsoft Excel 2019. The responses of the participants were scored from 1 to 5 based on scoring instructions of the questionnaire with 1 point being given to the option associated with the worst compliance and 5 points being given to the option associated with the best compliance with preventive practices. The coded data were subsequently analysed using IBM® SPSS® Statistics version 20.0 and STATA® 14 software.
Descriptive statistics were used for the description of the demographic details of the participants. Categorical variables were presented as absolute and relative frequencies while quantitative variables were presented as mean and standard deviations. Relevant statistical tests like Student’s t-test, Analysis of variance (ANOVA) followed by post hoc analysis with Bonferroni test and Kruskal Wallis test followed by multiple comparisons using Dunn test with Bonferroni correction as appropriate were employed to find out statistically significant association between dependent and independent variables. Univariate and multivariable stepwise linear regression was done to find the independent associated factors of adherence to preventive practices. P-value <0.05 was considered as statistically significant.
3. Results
3.1. Study population
A total of 1132 HCWs belonging to various occupational roles and socio-cultural backgrounds all over India completed the survey. 76 participants were excluded as per the exclusion criteria. The details of the remaining 956 participants are given in Table 1 . The mean age of the participants was 33.5 years with about half of the participants under 30 years. Overall, there were a slightly greater number of male (55.86%) and married participants (53.14%). The HCWs were posted mostly in the outpatient department and wards with many of them being posted at multiple places. The majority of them catered to COVID-19 positive/suspect cases (54.92%) with few of them posted in specially designated COVID-19 areas (8.05%)
Table 1.
Demographic details of the participants.
| Demographic characteristics | Respondents (n = 956) |
|---|---|
| Age (Mean 33.58 ± 11.68 SD) | |
| 18–30 | 492 (51.46%) |
| 31–45 | 258 (26.99%) |
| 46 and above | 206 (21.54%) |
| Gender | |
| Male | 534 (55.86%) |
| Female | 422 (44.14%) |
| Marital status | |
| Single | 442 (46.23%) |
| Married | 508 (53.14%) |
| Others (divorced, etc) | 6 (0.63%) |
| Occupation | |
| Doctor (faculty/specialist) | 357 (37.34%) |
| Doctor (residents) | 172 (17.99%) |
| Nurses | 240 (25.10%) |
| Other Paramedical staffa | 187 (19.56%) |
| Area of residence | |
| Northern part of India (Delhi, Uttarakhand, others) | 175 (18.30%) |
| Central part of India (Maharashtra, Madhya Pradesh, others) | 179 (18.72%) |
| Eastern part of India (West Bengal, Bihar, Uttar Pradesh, others) | 216 (22.59%) |
| Western part of India (Rajasthan, Punjab, Others) | 96 (10.04%) |
| Southern part of India (Tamil Nadu, Karnataka, others) | 290 (30.38%) |
| Place of posting | |
| OPD | 424 (44.35%) |
| Ward | 423 (44.24%) |
| Operation theatre | 160 (16.73%) |
| ICU | 117 (12.23%) |
| Laboratory | 33 (3.45%) |
| Emergency | 11 (1.15%) |
| Others | 67 (7.00%) |
| Area of posting | |
| COVID-19 designated area | 77 (8.05%) |
| Others | 879 (91.95%) |
| Types of patients being seen | |
| COVID-19 positive/suspect | 525 (54.92%) |
| COVID-19 negative | 431 (45.08%) |
other paramedical staff includes health assistants, sanitation assistants, Lab and operation theatre technicians, audiologists, optometrists, etc.
3.2. Preventive practices
The responses of the participants to section A are given in Table 2 and those to section B are given in supplementary Tables 1 and 2
Table 2.
Responses to section A of the questionnaire.
| S No. | Item | Frequency of scores (%) |
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | ||
| Hand Hygiene | ||||||
| 1 | I shake hands while meeting colleagues. | 80 (8.37) | 35 (3.66) | 41 (4.29) | 49 (5.13) | 751 (78.56) |
| 2 | I sanitize my hands after contact with each patient and/or his/her surroundings. | 24 (2.51) | 34 (3.56) | 75 (7.85) | 174 (18.20) | 649 (67.89) |
| 3 | I ensure that I wash/sanitize my hands for at least 20 s. | 23 (2.41) | 46 (132) | 132 (13.81) | 247 (25.84) | 508 (53.14) |
| 4 | I properly follow the steps of washing/sanitizing hands. | 19 (1.99) | 44 (4.60) | 105 10.98) |
283 (29.60) | 505 (52.82) |
| 5 | I touch my eyes, nose, or mouth without washing/sanitizing my hands. | 72 (7.53) | 47 (4.92) | 75 (7.85) | 162 (16.95) | 600 (62.76) |
| Social distancing | ||||||
| 6 | I maintain at least 1-m distance with family members | 184 (19.25) | 135 (14.12) | 145 (15.17) | 233 (24.37) | 259 (27.09) |
| 7 | I maintain at least 1-m distance with co-workers at the hospital. | 36 (3.77) | 80 (8.37) | 155 (16.21) | 280 (29.29) | 405 (42.36) |
| 8 | I maintain at least 1-m distance while eating food with my colleagues. | 65 (65.80) | 91 (9.52) | 126 (13.18) | 227 (23.74) | 447 (46.76) |
| 9 | I maintain at least 1-m distance while talking to my colleagues in the duty rooms. | 49 (5.13) | 100 (10.46) | 130 (13.60) | 276 (28.87) | 401 (41.95) |
| 10 | I maintain at least 1-m distance with others in public spaces (e.g. shopping, social gatherings, etc). | 19 (1.99) | 36 (3.77) | 90 (9.41) | 233 (24.37) | 578 (60.46) |
| 11 | I have attended social gatherings (Like meeting friends, going to religious places, visiting theatres, etc) in the past two months. | 48 (5.02) | 26 (2.72) | 88 (9.21) | 122 (12.76) | 672 (70.29) |
| 12 | I avoid going out of the house unnecessarily. | 66 (6.90) | 33 (3.45) | 78 (8.16) | 195 (20.40) | 584 (61.09) |
| Personal Protective Equipment (PPE) | ||||||
| 13 | I follow the steps of donning and doffing properly. | 40 (4.18) | 44 (4.60) | 108 (11.30) | 213 (22.28) | 551 (57.64) |
| 14 | I wear adequate PPE during duty (according to guidelines for my ward and patients). | 51 (5.33) | 61 (6.38) | 79 (8.26) | 199 (20.82) | 566 (59.21) |
| 15 | I wear a mask inside the hospital premises. | 13 (1.36) | 15 (1.57) | 15 (1.57) | 67 (7.01) | 846 (88.49) |
| 16 | I cover both nose and mouth with a mask while wearing it. | 15 (1.57) | 16 (1.67) | 25 (2.62) | 69 (7.22) | 831 (86.92) |
| 17 | I touch the outer surface of the mask while wearing it. | 141 (14.75) | 96 (10.04) | 107 (11.19) | 201 (21.03) | 411 (42.99) |
| 18 | I keep my mask properly in a separate bag/dustbin after using it. | 32 (3.35) | 49 (5.13) | 82 (8.58) | 164 (17.15) | 629 (65.79) |
| 19 | I reuse my gowns/PPE during my single duty shift. | 149 (15.59) | 91 (9.52) | 75 (7.85) | 91 (9.52) | 550 (57.53) |
| 20 | I carry face shields/gowns/PPE to my duty room in the ward before completely doffing. | 296 (30.96) | 121 (12.66) | 95 (9.94) | 86 (9.00) | 358 (37.45) |
| 21 | I dispose of PPE in specified colored dustbins after use according to guidelines. | 33 (3.45) | 36 (3.77) | 50 (5.23) | 122 (12.76) | 715 (74.79) |
| 22 | I take chemoprophylaxis against COVID-19 (e.g. Hydroxychloroquine). | 448 (46.86) | 59 (6.17) | 165 (17.26) | 73 (7.64) | 211 (22.07) |
| Fomites | ||||||
| 23 | I use my personal items like mobile phones, etc during duty in the hospital. | 233 (24.37) | 164 (17.15) | 145 (15.17) | 155 (16.21) | 259 (27.09) |
| 24 | I sanitize my personal items like mobile phones, pens, etc with sanitizer after my duty. | 52 (5.44) | 69 (7.22) | 107 (11.19) | 171 (17.89) | 557 (58.26) |
| 25 | I take precautions while buying things to avoid contamination with COVID-19. | 32 (3.35) | 43 (4.50) | 88 (9.21) | 216 (22.59) | 577 (60.36) |
| Lifestyle | ||||||
| 26 | I take adequate sleep (6–8 h) daily. | 37 (3.87) | 52 (5.44) | 106 (11.09) | 259 (27.09) | 502 (52.51) |
| 27 | I stay updated regarding coronavirus disease by watching the news or reading guidelines. | 36 (3.77) | 53 (5.54) | 110 (11.51) | 289 (30.23) | 468 (48.95) |
| Exposure | ||||||
| 28 | How many times did you have high-risk exposure to COVID-19 positive/suspect cases? | 165 (17.26) | 36 (3.77) | 116 (12.13) | 180 (18.83) | 459 (48.01) |
| 29 | How many times were you quarantined? | 22 (2.30) | 10 (1.05) | 55 (5.75) | 185 (19.35) | 684 (71.55) |
The items are scored as (5) Always (more than 90% times), (4) Mostly (approx. 75% times), (3) Commonly (approx. 50% times), (2) Occasionally (approx. 25% times), (1) Rarely (less than 10% times), except for items 1,5,11,17,19,20,22,23,28,29. The items 1,5,17,19,20,23 are scored as (1) Always, (2) Mostly, (3) Commonly, (4) Occasionally and (5) Rarely. The items 11, 28 and 29 are scored as (5) Never, (4) Once, (3) Twice, (2) Thrice, (1) More than three times. Item 22 is scored as (5) Yes, taking regularly, (4) Yes, taking regularly but missed some doses, (3) Yes, took initially and then left, (2) Don’t remember, (1) No.
3.3. Hand hygiene
The majority of participants didn’t shake hands while meeting colleagues (78.56%) while others reported a lack of knowledge and the social etiquette of shaking hands so as not to look rude as the reasons for doing so. The majority of them sanitized their hands after contact with patients and their surroundings (67.89%). Only around half of the HCWs properly followed the steps of hand hygiene (52.82%) and ensured that they washed hands for at least 20 s (53.14%). Other participants cited lack of knowledge, shortage of time due to a large number of patients, cumbersome nature of sanitizing hands a lot of times, and inability to check the time while washing hands as main reasons for not doing so properly. A slightly larger number of participants (62.76%) didn’t touch their facial parts (eyes, nose, and mouth) without sanitizing hands. The remaining participants cited difficulty in changing habits and lack of knowledge as the main reasons for doing so.
3.4. Social distancing
Less than half of the participants maintained social distancing while talking to colleagues in duty rooms (41.95%), working (42.36%), or eating food (46.76%). The main reasons cited for not being able to do so were lack of space, difficulty in talking to others in PPE, difficulty in changing habit, and lack of knowledge. Compared to it, most of the participants always maintained at least 1-m distance in public spaces (60.46%). A large majority of them (70.29%) never attended a social gathering in the past 2 months and most of them (61.09%) avoided going out of the house unnecessarily. HCWs mainly went out of their homes for work, buying groceries, and walking/exercising while a minority (around 3%) of them went out for socializing, entertainment, and visiting religious places. Around half of the participants (51.46%) maintained at least 1-m distance with family members most of the time.
3.5. Personal protective equipment (PPE)
The highest adherence was seen in the practice of wearing masks- 88.49% of participants always wore masks inside health care settings and most of them (86.92%) covered both mouth and nose while wearing it. But a significant proportion of participants (35.98%) commonly touched the outer surface of masks while wearing it. The common reasons cited for it were to remove the mask for eating food and water (28%), readjusting it due to loose fit (22%), lack of knowledge (11%), and uncomfortable nature of the mask (10%). Around 57% of participants always followed the steps of donning and doffing properly. The remaining participants couldn’t do so due to lack of a helping person/mirror (14%), lack of knowledge (12%), and absence of a dedicated doffing area (10%). Around 60% wore adequate PPE during duty. Common reasons cited for not doing so were long duty hours, shortage of PPE, feeling uncomfortable while wearing it, and lack of knowledge and institutional guidelines. The majority of participants (53.56%) carried PPE to their duty rooms before completely doffing. Around one-third of participants (32.96%) reused their PPE commonly due to a shortage of PPE and long duty hours. A majority of participants (74.79%) always disposed of PPE in specified dustbins while a smaller number of participants (65.79%) disposed of masks properly. Others couldn’t do so due to lack of knowledge, lack of dustbins/doffing areas for PPE, and lack of a suitable place/bag to keep masks.
Around half of the participants (46.86%) never took any chemoprophylaxis like hydroxychloroquine, ivermectin, etc against COVID-19 and many participants left it after taking the initial few doses. Only 22% of HCWs reported regular intake of chemoprophylaxis for COVID-19.
3.6. Gadgets/fomites
More than half of the participants (58.47%) commonly used personal items like mobile phones, etc during duty for patient management and communication with colleagues and family. A majority of them sanitized these items at the end of the duty. Others believed that using sanitizers on personal items will damage them or felt too tired to do so.
3.7. Lifestyle and exposure
Most of the participants (60.36%) always took precautions while buying things to prevent contamination with SARS-CoV-2. Most of them wore face masks (59.31%) and carried hand sanitizers while shopping (44.46%). They went out when it was less busy (34.32%) and bought 1–2 weeks of groceries at a time (40.17%). Many opted for home delivery (40.90%) and cashless payments (40.17%).
Only half of the participants (52.51%) reported taking adequate sleep regularly in the past 2 weeks. The remaining participants cited lack of time, anxiety, and disturbed sleep-wake cycle due to shift work as common reasons. Less than half of the participants regularly updated themselves regarding COVID-19 by reading guidelines or watching the news. The remaining participants reported that the news was distressing (13.07%) and it was difficult to find relevant information. More than half of the participants (52%) reported one or more high-risk exposure to COVID-19 positive patients and around 30% of participants went to quarantine.
Many participants reported that lack of awareness, carelessness of HCWs for their safety, shortage of manpower and PPE, asymptomatic cases not detected by RT-PCR test in early stages, and increased exposure to patients were important reasons for the large number of HCWs getting infected with COVID-19 (supplementary Table 2).
The summary of adherence of participants to various preventive practices is given in Table 3 .
Table 3.
Adherence to preventive practices by participants.
| Frequency of responses to items | No. of items | Questions |
|---|---|---|
| >80% participants giving ideal response | 3 | 15,16,21 |
| 60–80% participants giving ideal responses | 9 | 1,2,5,10,11,12,18,25,29 |
| 40–59.9% participants giving ideal responses | 13 | 3,4,7,8,9,13,14,17,19,24,26,27,28 |
| <40% participants giving ideal responses | 4 | 6, 20, 22, 23 |
3.8. Association between dependent and independent variables
It was analysed that the age, gender, and occupational roles of HCWs were associated with the extent of their adherence to preventive practices (Table 4 ). It was found that HCWs aged 18–30 years were associated with lower compliance with preventive practices compared to those more than 31 years of age (p-value <0.001). Female HCWs reported better adherence to preventive practices (p-value <0.001). Resident doctors and other paramedical staff (like ward boys, sweepers, OT and lab technicians, optometrists, etc) had lower adherence to preventive practices compared to nurses and senior doctors (p-value <0.001). No statistically significant association was observed with the posting of HCWs in COVID-19 designated areas or types of patients being seen (COVID-19 positive/suspect).
Table 4.
Association between various characteristics and compliance with preventive practices.
| Groups | Responses | P-value | Unadjusted regression coefficient (95% CI) | Adjusted regression coefficient (95% CI) |
|---|---|---|---|---|
| Age | ||||
| 18–30 | 115.14 ± 14.53 | <0.001 | ||
| 31–45 | 119.97 ± 13.29 | 4.8 (2.76,6.92) | 4.8 (2.50,7.14) | |
| 46 and more |
122.20 ± 12.54 |
7.1 (4.82, 9.31) |
6.1 (3.19, 9.08) |
|
| Gender | ||||
| Male | 116.27 ± 14.97 | <0.001 | ||
| Female | 120.11 ± 12.64 | 3.8 (2.05, 5.63) | 4.5 (2.68, 6.34) | |
| Marital status | ||||
| Single | 115.57 ± 14.68 | <0.001 | ||
| Married | 120.08 ± 13.31 | 4.5 (2.73, 6.29) | – | |
| Others |
115.50 ± 7.92 |
−0.7 (−11.32, 11.17) |
||
| Occupation | ||||
| Doctors (faculty/specialist) | 121.48 ± 10.96 | <0.001 | ||
| Doctor (residents) | 114.56 ± 13.65 | −6.9 (−9.42, −4.42) | −3.2 (−6.27, −0.22) | |
| Nurses | 118.87 ± 13.85 | −2.6 (−4.85, −0.36) | −0.4 (−3.27, 2.42) | |
| Other paramedical staff | 113.25 ± 17.79 | −8.2 (−10.66, −5.80) | −5.1 (−7.88, −2.35) | |
| Area of posting | ||||
| COVID designated area | 118.73 ± 1.57 | 0.6224 | ||
| Other | 117.90 ± 0.48 | −0.8 (−4.12, 2.47) | – | |
| Type of patients being seen | ||||
| COVID-19 positive/suspect | 118.69 ± 0.58 | 0.0792 | ||
| COVID-19 negative cases | 117.08 ± 0.72 | −1.6 (−3.41, 0.19) | – | |
4. Discussion
COVID-19 has swiftly become a global pandemic infecting millions of frontline HCWs with thousands among them succumbing to it [5]. This alarming rate of infection is attributable to the overburdening of healthcare systems with the rapid surge of patients, shortage of PPE, increased psychosocial stress and lifestyle-related factors, and suboptimal adherence to preventive measures like hand washing and PPE use [[3], [4], [5],9,10].
We analysed the compliance of HCWs to an array of preventive practices ranging from hand hygiene to lifestyle. This was followed by a scrutiny of reasons for lower compliance with these practices and whether individual sections of HCWs were more vulnerable to lower compliance. To our knowledge, this is one of the first studies to assess preventive practices comprehensively in various sections of HCWs to date. It not only identifies suboptimal practices but also identifies reasons for them.
We find that compliance with preventive practices like hand hygiene has increased slightly during the COVID-19 pandemic, though more efforts are required to ensure that HCWs follow all steps of hand hygiene for adequate time [11]. This is important because suboptimal hand washing has been observed as a significant risk factor for COVID-19 [3,4]. We also find that certain preventive practices are being followed less stringently in comparison to others. Although HCWs are wearing masks regularly, touching the outer surface of masks is common. Likewise, many HCWs report inabilities to follow social distancing within wards and duty rooms due to the lack of adequate space and difficulty in talking. Due to a shortage of PPE, lack of knowledge, and behavioral reasons, HCWs don’t wear all components of PPE (all the time), reuse it, or carry it to duty rooms and don’t don or doff properly. Also, a major proportion of HCWs are not able to take care of their holistic well-being like taking adequate sleep due to lack of time, anxiety, and disturbed sleep-wake cycle owing to shift duties. Various studies have assessed the changes in lifestyle-related behavior in COVID-19 and have found an increase in stress and anxiety [[12], [13], [14]]. We also observed the widespread use of mobiles in healthcare settings and its potential role as a fomite in the transmission of COVID-19 [15]. However, the majority of HCWs sanitized them at the end of the duty, which is higher compared to the pre-COVID era [16]. More than half of the participants reported one or more high-risk exposure to COVID-19 positive patients, but fewer number among them went into quarantine. This is worrisome as many of them with mild or no symptoms might transmit the infection to others. Around half of the participants never took any chemoprophylaxis like hydroxychloroquine, ivermectin, etc against COVID-19 and many participants left it after taking the initial few doses. This is attributable to the debated role of hydroxychloroquine, etc as pre-exposure prophylaxis against COVID-19 [17]. During the COVID-19 pandemic, the compliance to preventive practices was higher in HCWs when compared to the general population in areas of hand hygiene and social distancing in public places [18].
Besides, we find that lack of knowledge, long duty hours, shortage of PPE, high patient workload, and casual attitude regarding their safety are important barriers to the adoption of these practices. Earlier studies have also observed that long duty hours, inadequate knowledge, improper hand hygiene, inadequate access to PPE, and working in high-risk departments are associated with increased risk of COVID-19 [3,4,8]. Moreover, certain sections of HCWs are more likely to exhibit suboptimal practices. Resident doctors and paramedical staff along with male HCWs in the age group 18–30 years are associated with lower adherence to preventive practices. Consistent with previous studies, better adherence to preventive practices is observed in nurses and older staff while increased exposure to COVID-19 patients is not associated with better preventive practices [19,20].
Based on the published literature and findings of our study, we suggest the following mitigation strategies [21,22]. To improve knowledge and awareness, regular training of HCWs should be done particularly in areas of hand hygiene and PPE. For optimal hand hygiene practices, WHO hand hygiene posters should be pasted in handwashing areas, and practical easy-to-remember methods should be circulated for washing hands properly for adequate time. For ensuring better practice, regular monitoring and reinforcement of HCWs should be done. Administrative measures like provision of sufficient and comfortable PPE, optimization of the duty roster, modified operational protocols for surgery and robust institutional framework for surveillance should be implemented to ensure adequate patient care while ensuring the safety of HCWs [23]. In terms of infrastructure, the layout and ventilation of duty rooms and cafeteria should be optimized during the pandemic, and overcrowding in the wards should be avoided. Besides, HCWs should be encouraged to exercise and perform yoga, and adequate psychological support should be provided to them regularly. Considering the dearth of standard guidelines, there is a need to formulate a standardized protocol for disinfecting electronic gadgets in healthcare settings [15]. There is also a need for collaboration between healthcare and other industries to develop ergonomic masks and PPE.
4.1. Limitations
The study has limitations inherent to any online-based survey. There may be sampling bias due to the non-random technique which may limit the generalization of findings. There may be reporting bias attributable to the tendency of participants to give answers according to social desirability.
5. Conclusions
Suboptimal compliance to preventive practices like handling PPE, distancing in cafeteria/duty rooms and hand hygiene is not uncommon among young HCWs especially resident doctors and paramedical staff. The compliance to preventive practices is higher in HCWs during the COVID-19 pandemic compared to the general population and pre-COVID times. Certain barriers are identified which should be addressed to ensure adequate safety of HCWs against COVID-19.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Financial support. None reported.
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.dsx.2020.12.016.
Author contributions
AA and PR conceptualized the study. PR, ADU, AC and NV developed methodology. AA, PR AS, KK, VB, AS, and KBK did the investigation. AA curated the data. AA, PR, and ADU did the formal analysis. PR and NV supervised the project. AA and UB wrote the original draft which was reviewed, edited, and approved by all the authors.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Sim M.R. The COVID-19 pandemic: major risks to healthcare and other workers on the front line. Occup Environ Med. 2020;77(5):281–282. doi: 10.1136/oemed-2020-106567. [DOI] [PubMed] [Google Scholar]
- 2.Chou R., Dana T., Buckley D.I., Selph S., Fu R., Totten A.M. Epidemiology of and risk factors for Coronavirus infection in health care workers: a living rapid review. Ann Intern Med. 2020 21;173(2):120–136. doi: 10.7326/M20-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nguyen L.H., Drew D.A., Graham M.S., Joshi A.D., Guo C.-G., Ma W. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Publ Health. 2020 doi: 10.1016/S2468-2667(20)30164-X. Accessed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ran L., Chen X., Wang Y., Wu W., Zhang L., Tan X. Risk factors of healthcare workers with corona virus disease 2019: a retrospective cohort study in a designated hospital of Wuhan in China. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020 Mar 17 doi: 10.1093/cid/ciaa287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Protect Health Workers to Save Patients, WHO Reiterates on World Patient Safety Day. UN News; 2020. https://news.un.org/en/story/2020/09/1072612 Published 2020. Accessed. [Google Scholar]
- 6.India: WHO Coronavirus Disease (COVID-19) Dashboard. 2020. https://covid19.who.int/region/searo/country/in Accessed. [Google Scholar]
- 7.Agarwal A., Ranjan P., Saikaustubh Y., Rohilla P., Kumari A., Prasad I., et al. Development and validation of a questionnaire for assessing preventive practices and barriers among health care workers in COVID-19 pandemic. Indian J Med Microbiol (In press). [DOI] [PMC free article] [PubMed]
- 8.Zhang M., Zhou M., Tang F., Wang Y., Nie H., Zhang L. Knowledge, attitude, and practice regarding COVID-19 among healthcare workers in Henan, China. J Hosp Infect. 2020 Jun;105(2):183–187. doi: 10.1016/j.jhin.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ranjan P., Bhattacharya A., Chakrawarty A. Association Between Self-Reported Adherence to Preventive Practices and Probability of Turning COVID-19 Positive: A Cross-Sectional Analytical Study. A Cross-Sectional Analytical Study. Cureus. 2020 Dec 01;12(12) doi: 10.7759/cureus.11815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ranjan P., Kumar A., Chowdhury S., Pandey S., Choudhary A., Bhattacharya A. Is excess weight a risk factor for the development of COVID 19 infection? A preliminary report from India. Diabetes Metab Syndr. 2020;14(6):1805–1807. doi: 10.1016/j.dsx.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yamini Jain A., Mandelia C., Jayaram S. Perception and practice regarding infection control measures amongst healthcare workers in district government hospitals of Mangalore, India. Int J Health Allied Sci. 2012 Apr 1;1(2):68. [Google Scholar]
- 12.Kumari A., Ranjan P., Vikram N.K., Kaur D., Sahu A., Dwivedi S.N. A short questionnaire to assess changes in lifestyle-related behaviour during COVID 19 pandemic. Diabetes Metab Syndr. 2020;14(6):1697–1701. doi: 10.1016/j.dsx.2020.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chopra S., Ranjan P., Malhotra A., Sahu A., Dwivedi S.N., Baitha U. Development and validation of a questionnaire to evaluate the impact of COVID on lifestyle related behaviors: eating habits, activity and sleep behavior. Publ Health Nutr. 2020 Nov 16:1–24. doi: 10.1017/S1368980020004656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chopra S., Ranjan P., Singh V., Kumar S., Arora M., Hasan M.S. Impact of COVID-19 on lifestyle-related behaviours- a cross-sectional audit of responses from nine hundred and ninety-five participants from India. Diabetes Metab Syndr. 2020;14(6):2021–2030. doi: 10.1016/j.dsx.2020.09.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Olsen M., Campos M., Lohning A., Jones P., Legget J., Bannach-Brown A. Mobile phones represent a pathway for microbial transmission: a scoping review. Trav Med Infect Dis. 2020 Jun;35:101704. doi: 10.1016/j.tmaid.2020.101704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brady R.R.W., Chitnis S., Stewart R.W., Graham C., Yalamarthi S., Morris K. NHS connecting for health: healthcare professionals, mobile technology, and infection control. Telemed J E Health Off J Am Telemed Assoc. 2012 May;18(4):289–291. doi: 10.1089/tmj.2011.0147. [DOI] [PubMed] [Google Scholar]
- 17.Agarwal M., Ranjan P., Baitha U., Mittal A. Hydroxychloroquine as a chemoprophylactic agent for COVID-19: a clinico-pharmacological review. Frontiers in Pharmacology. 2020 doi: 10.3389/fphar.2020.593099. 11:2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chakrawarty A., Ranjan P., Thrinath A., Aggarwal E., Isaac J.A., Berry P. Assessment of preventive practices followed by general public during COVID-19 pandemic - a cross-sectional survey from India. Cureus. 2020 Oct 31;12(10) doi: 10.7759/cureus.11274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lai X., Wang X., Yang Q., Xu X., Tang Y., Liu C. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob Resist Infect Contr. 2020 Jun 11;9(1):83. doi: 10.1186/s13756-020-00746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olum R., Chekwech G., Wekha G., Nassozi D.R., Bongomin F. Coronavirus disease-2019: knowledge, attitude, and practices of health care workers at Makerere university teaching hospitals, Uganda. Front Public Health. 2020;8:181. doi: 10.3389/fpubh.2020.00181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.WHO. Infection prevention and control during healthcare when COVID-19 is suspected: Interim guidance. WHO; 2020. https://apps.who.int/iris/bitstream/handle/10665/331495/WHO-2019-nCoV-IPC-2020.3-eng.pdf Accessed. [Google Scholar]
- 22.Houghton C., Meskell P., Delaney H., Smalle M., Glenton C., Booth A. Barriers and facilitators to healthcare workers’ adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020 21;4:CD013582. doi: 10.1002/14651858.CD013582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agarwal D., Chawla R., Varshney T., Shaikh N., Chandra P., Kumar A. Managing vitreoretinal surgeries during COVID-19 lockdown in India: experiences and future implications. Indian J Ophthalmol. 2020 Oct;68(10):2126–2130. doi: 10.4103/ijo.IJO_2140_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.