Abstract
Objective
A resilient health system plays a crucial role in pandemic preparedness and response. Although the World Health Organization (WHO) has required all states parties to strengthen core capacities to respond to public health emergencies under the International Health Regulations (2005), the actions of most countries to combating coronavirus disease 2019 (COVID-19) has showed that they are not well-prepared. This cross-sectional study aimed to examine the health system resilience of selected countries and analyze their strategies and measures in response to the COVID-19 pandemic.
Methods
This study selected five countries including the Iran, Japan, Republic of Korea (South Korea), the U.K., and the U.S., based on the severity of the national epidemic, the geographical location, and the development level. Cumulative number of death cases derived from WHO COVID-19 dashboard was used to measure the severity of the impact of the pandemic in each country; WHO State Parties Self-Assessment Annual Reporting (SPAR) Scores and Global Health Security (GHS) Index were applied to measure the national health system resilience; and research articles and press materials were summarized to identify the strategies and measures adopted by countries during response to COVID-19. This study applied the resilient health systems framework to analyze health system resilience in the selected countries from five dimensions, including awareness, diversity, self-regulation, integration and adaptation.
Results
The SPAR Scores and GHS Index of the four developed countries, Japan, South Korea, the U.K. and the U.S. were above the global and regional averages; the SPAR Scores of Iran were above the global average while the GHI Index lain below the global average. In terms of response strategies, Japan, the U.K. and the U.S. invested more health resources in the treatment of severe patients, while South Korea and Iran had adopted a strategy of extensive testing and identification of suspected patients. In terms of specific measures, all the five countries adopted measures such as restrictions on entry and international travel, closure of schools and industries, lockdown and quarantine. Nevertheless, the effectiveness of implementing these measures varied across countries, based on the response strategies.
Conclusion
Although SPAR Scores and GHS Index have evaluated the national core capacities for preparedness and response, the actions to cope with the COVID-19 pandemic has revealed the fact that most countries still do not build resilient health systems in response to public health emergencies. Health system strengthening and health security efforts should be pursued in tandem, as part of the same mutually reinforcing approach to developing resilient health systems.
Keywords: Coronavirus disease 2019, COVID-19, Pandemic, Resilient health systems, Preparedness and response, Global health security, Health system strengthening
1. Introduction
The coronavirus disease 2019 (COVID-19) pandemic has posed a significant challenge to national health systems in terms of preparedness and response, where a resilient health system plays a vital role. A resilient health system can effectively prepare for and respond to pandemics while maintaining core functions, informed by lessons learned on an ongoing basis, and reorganize promptly if conditions require it.1, 2 Resilience helps bridge global health security and health system strengthening.3 The resilience of health systems has received widespread attention among policy makers and researchers in the aftermath of the Ebola virus outbreak in West Africa in 2014. Since the implementation of the International Health Regulations (IHR [2005]), the World Health Organization (WHO) has required all state parties to strengthen core capacities to respond effectively to public health emergencies.4 Global health security, as a result of achieving IHR (2005) core capacities and well-functioning health care delivery, should be an inherent part of a resilient health system.5 We thus aimed to investigate health system resilience with respect to the preparedness for and response to the COVID-19 pandemic.
The WHO announced the pandemic status of the COVID-19 outbreak on March 11, 2020.6 As of April 15, 1918,138 confirmed COVID-19 cases and 123,126 deaths had been reported worldwide.7 Following the COVID-19 outbreak in Asia in early January, countries such as China, Japan, Republic of Korea (South Korea), and Singapore imposed stringent measures to curb the spread of the disease.8 By the end of March, the pandemic had caused greater-than-anticipated infection and death cases in Europe and North America.9 The situation was grim even in countries with relatively well-developed health systems, including the U.K. and the U.S.10 The pandemic also caused a high death toll in developing countries, such as Iran. Such a situation reflects the failure of most countries to be equipped with a resilient health system to survive a pandemic.11, 12, 13
The present cross-sectional study aimed to examine the health system resilience of select countries and analyze their strategies and countermeasures in response to the COVID-19 pandemic, to identify the gaps in building resilient health systems, and to provide strategic policy recommendations for narrowing the gaps by embedding global health security measures into health system strengthening.
2. Methods
We analyzed the national health system resilience and COVID-19 response strategies in five countries, namely, Iran, Japan, South Korea, the U.K., and the U.S., taking into account the severity of their national epidemic, geographical location, and development level. Pandemic severity was measured based on the cumulative number of death cases at the national level. Data were derived from the WHO COVID-19 Dashboard, including all death cases recorded until 3:38 pm CEST, September 1, 2020.14 We also took into account the geographical location of the countries, with five countries located in the three continents most affected by the pandemic: Europe, North America, and Asia. We further considered the development level of each country; only Iran is a developing country and the other four are developed countries.
We adopted two indicators, the WHO State Parties Self-Assessment Annual Reporting (SPAR) Scores and Global Health Security (GHS) Index, to provide an overall view of national health system resilience. SPAR is a tool developed by the WHO to monitor and evaluate the progress in achieving IHR (2005) core capacities; it consists of 13 categories with 24 indicators, which are self-rated by countries and reported at the World Health Assembly annually.15 Iran's data are not included in the 2019 SPAR updated on March 15, 2020. Thus, we used the 2018 SPAR results to reflect Iran's national health system resilience, whereas the 2019 SPAR results were applied to the other four countries.16 Given that SPAR measures a country's preparedness capacity with limited consideration of demographic, political, socioeconomic, and environmental factors, we drew on the GHS Index to assess the combined impact of these factors on national health security.17 The GHS Index was jointly developed by the Nuclear Threat Initiative, Johns Hopkins Center for Health Security, and Economist Intelligence Unit to assess national health security through a total of 140 questions across six dimensions: prevention, detection and reporting, rapid response, health system, compliance with international norms, and risk environment. This study used the GHS Index of the five countries updated in October 2019.
This study applied the resilient health systems framework to analyze health system resilience in the selected countries from five dimensions, namely, awareness, diversity, self-regulation, integration, and adaptation.1 Meanwhile, the national strategies and interventions to counter the COVID-19 pandemic in the five countries were synthesized from research articles, news articles, and reports. Data sources included academic databases, official websites of governments and international organizations, and authoritative media organizations, such as CNN, BBC News, The New York Times, and The Economist.
3. Results
3.1. COVID-19 pandemic in the selected countries
With cumulative death cases of 21,571, Iran has recorded one of the largest death numbers among all countries. The first death case in Iran was reported on February 19. The cumulative number of death cases in Iran has risen markedly since March, increasing at more than 100 cases beginning in March 15. Meanwhile, the cumulative deaths in Japan and South Korea were lower compared with the other three countries, at 1296 and 324 cases, respectively. The first death case in Japan was reported on February 13, and that in South Korea, on February 20. As of September 1, the U.K. reported 41,501 COVID-19 deaths. Meanwhile, the U.S. ranked as the country with the most cumulative deaths worldwide, at 124,811. The first death case in the U.K. was reported on March 6, and that in the U.S., on March 3. Both countries showed an increase in, and ongoing, cumulative number of deaths after March 20. Death case growth in the U.K. slowed down after July.
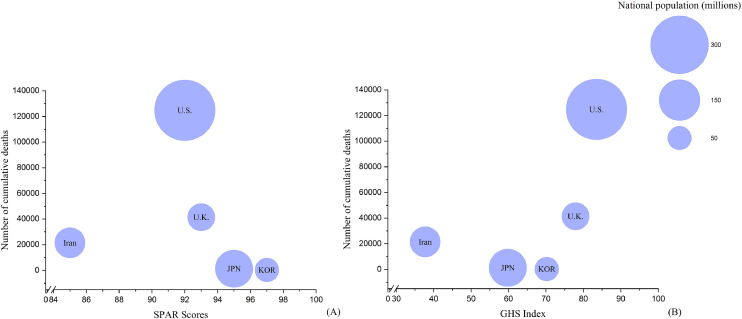
In the analysis of the SPAR Scores, there were small differences in health security capabilities among countries. Japan and South Korea appeared in the lower right corner of the graph because of their high SPAR scores and low cumulative deaths. The U.S. with a large population and a high number of deaths, occupied a large position in the middle of the map. However, overall, the bubble size in the similar areas did not show a good consistency, and the number of cumulative deaths and SPAR Scores did not show an obvious correlation (Fig. 1 A). As for GHS Index, there were wide variations in health security capability scores across countries. In addition, cumulative deaths showed a positive correlation with the GHS Index score in the five countries. Iran, with a lower GHS Index score and a lower death, appeared in the lower left corner of the graph, while the U.S, with a higher GHS score and a higher death, appeared in the upper right corner. However, because the consistency of bubble size is still poor, it was difficult to estimate the influence of national population (Fig. 1B).
Fig. 1.
Cumulative number of deaths and the SPAR Scores and GHS Index. (A) Cumulative number of deaths and the SPAR Scores; (B) Cumulative number of deaths and the GHS Index.
The horizontal axis reflects the SPAR Scores and GHI index for each country. The vertical axis reflects the cumulative number of deaths for each country. The value of vertical axis corresponding to the center of the bubble is the cumulative number of deaths. Area of circles is proportional to national population based on United Nations 2019 country census data. The closer to the bottom right of the figure with the larger area, the more resilient the country's health system is. Iran: Islamic Republic of Iran; JPN: Japan; KOR: Republic of Korea; U.K.: the United Kingdom of Great Britain and Northern Ireland; U.S.: the United States of America; SPAR: State Parties Self-Assessment Annual Reporting; GHS: Global Health Security.
3.2. National core capacities for preparedness and response
Table 1 showed the combined SPAR Scores of the Iran, Japan, South Korea, the U.K., and the U.S. were 85, 95, 97, 93, 92, respectively, all of which were higher than the global average and each country's regional average. As for the 13 core capacity scores, Iran scored lower than the average at the global and Eastern Mediterranean levels for Zoonotic events and Human–animal interface. Japan scored below the Western Pacific average for Risk Management but was in line with the global average in this category. All of South Korea's core capacity scores exceeded the global and Western Pacific average. The U.K. scored below the global and European average for points of entry. The U.S. scored below the global average and that of the Americas for the human resource capacity.
Table 1.
Six countries' self-assessment annual reporting scores of total and per capacities.
| Item | Japan (2019) | South Korea (2019) | Western Pacific average (2019) | U.K. (2019) | European average (2019) | U.S. (2019) | Americas Average (2019) | Global average (2019) | Iran (2018)* | Eastern Mediterranean average (2018) | Global average (2018) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total SPAR Scores | 95 | 97 | 71 | 93 | 75 | 92 | 71 | 63 | 85 | 65 | 61 |
| Legislation and financinga | 100 | 100 | 76 | 100 | 81 | 100 | 74 | 66 | 100 | 61 | 62 |
| IHR Coordination and National IHR Focal Point Functionsb | 100 | 80 | 72 | 90 | 83 | 100 | 78 | 70 | 80 | 73 | 67 |
| Zoonotic events and the human-animal interfacec | 100 | 100 | 65 | 100 | 81 | 80 | 72 | 67 | 60 | 74 | 63 |
| Food safetyd | 100 | 100 | 75 | 100 | 77 | 100 | 78 | 64 | 80 | 64 | 61 |
| Laboratorye | 100 | 100 | 81 | 100 | 81 | 100 | 79 | 71 | 100 | 71 | 70 |
| Surveillancef | 100 | 100 | 84 | 100 | 79 | 100 | 78 | 73 | 80 | 77 | 71 |
| Human resourcesg | 80 | 100 | 68 | 100 | 71 | 60 | 70 | 63 | 80 | 71 | 63 |
| National health emergency frameworkh | 100 | 100 | 75 | 100 | 73 | 100 | 73 | 62 | 100 | 68 | 59 |
| Health service provisioni | 100 | 100 | 70 | 100 | 79 | 100 | 64 | 62 | 100 | 64 | 60 |
| Risk communicationj | 60 | 80 | 69 | 100 | 66 | 100 | 68 | 60 | 80 | 60 | 57 |
| Points of entryk | 100 | 100 | 70 | 40 | 62 | 100 | 70 | 56 | 60 | 55 | 52 |
| Chemical eventsl | 100 | 100 | 70 | 80 | 69 | 80 | 60 | 54 | 100 | 53 | 50 |
| Radiation Emergenciesm | 100 | 100 | 54 | 100 | 78 | 80 | 59 | 55 | 80 | 60 | 52 |
Here the 2018 SPAR Score is used to reflect the resilience of Iran's national health system due to Iran's data are not included in the 2019 SPAR Scores updated on March 15, 2020.
This refers to States Parties’ capacity to have an adequate legal framework to support and enable implementation of all of their obligations and rights;
This refers to States parties’ capacity to coordinate nationwide resources, including the designation of an National IHR Focal Point;
This refers to States parties’ capacity to detect and respond to zoonotic events of national or international concern;
This refers to States parties’ capacity to detect and respond to food safety events that may constitute a public health emergency of national or national or international concern;
This refers to States parties’ capacity to establish mechanisms that assure the reliable and timely laboratory identification of infectious agents and other hazards likely to cause public health emergencies of national and international concern, including shipment of specimens to the appropriate laboratories if necessary;
This refers to States parties’ capacity of rapid detection of public health risks, as well as the prompt risk assessment, notification, and response to these risks;
This refers to States parties’ capacity to strengthen the skills and competencies of public health personnel;
This refers to States parties’ capacity to facilitate the coordination and management of outbreak operations and other public health events, and capacity to develop national, intermediate and community/primary response level public health emergency response plans for relevant biological, chemical, radiological and nuclear hazards;
This refers to States parties’ capacity to provide high-quality health service;
This refers to States parties’ capacity to help stakeholders define risks, identify hazards, assess vulnerabilities and promote community resilience, and disseminate information to the public about health risks and events;
This refers to States parties’ capacity to establish effective surveillance and reponse at points of entry, and fulfill general obligation;
This refers to States parties’ capacity to detect and respond to chemical events of national and international public health concern;
This refers to States parties’ capacity to detect and respond to radiological and nuclear emergencies that may constitute a public health event of national or international concern. SPAR: WHO State Parties Self-Assessment Annual Reporting; IHR: International Health Regulation.
Table 2 showed the GHS Index for the Iran, Japan, South Korea, the U.K., and the U.S. were 37.7, 59.8, 70.2, 77.9, and 83.5, respectively. With the exception of Iran, the selected countries ranked relatively high on the global scale, with the U.S. and U.K. being the top two countries with the best scores. The U.S., U.K., South Korea and Japan scored above the global average in all six dimensions, and the U.S. ranked highest in four dimensions: prevention, detection and reporting, health system, and compliance with international norms. The U.K. ranked highest for the rapid response dimension. Iran's GHS Index was below the global average, ranking 97th worldwide. It also scored below the corresponding global average in the four dimensions of detection and reporting, rapid response, compliance with international norms, and risk environment.
Table 2.
Global Health Security (GHS) Index of target countries (2019)*.
| Item | Japan | South Korea | U.K. | U.S. | Iran | Global average |
|---|---|---|---|---|---|---|
| Index score | 59.8 | 70.2 | 77.9 | 83.5 | 37.7 | 40.2 |
| Preventiona | 49.3 | 57.3 | 68.3 | 83.1 | 44.7 | 34.8 |
| Detection and reportingb | 70.1 | 92.1 | 87.3 | 98.2 | 37.7 | 41.9 |
| Rapid responsec | 53.6 | 71.5 | 91.9 | 79.7 | 33.7 | 38.4 |
| Health systemd | 46.6 | 58.7 | 59.8 | 73.8 | 34.6 | 26.4 |
| Compliance with international normse | 70 | 64.3 | 81.2 | 85.3 | 28.7 | 48.5 |
| Risk environmentf | 71.7 | 74.1 | 74.7 | 78.2 | 50.3 | 55.0 |
GHS Index was developed by the project team jointly with an international advisory panel of 21 experts from 13 countries. A detailed and comprehensive framework of 140 questions across 6 categories, including 34 indicators and 85 subindicators was applied to assess a country's capability to prevent and response to public health threats, and capacity to reduce global catastrophic biological risks. Data of each country was relied on open-source information.
Prevention of the emergence or release of pathogens;
Early detection and reporting for epidemics of potential international concern;
Rapid response to and mitigation of the spread of an epidemic;
Sufficient and robust health system to treat the sick and protect health workers;
Commitments to improving national capacity, financing plans to address gaps, and adhering to global norms;
Overall risk environment and country vulnerability to biological threats.
3.3. Actions for pandemic preparedness and response
In terms of response strategies, the U.S., the U.K., and Japan invested more health resources in the treatment of severe patients, with home isolation for mild patients, and discouraged or restricted testing for mild patients. South Korea and Iran had adopted a strategy of extensive testing and identification of suspected patients and people in close contact, and endeavored to treat and manage all severe and mild cases, despite the constraints by the capacity of the health system. In terms of specific measures, the five countries adopted several similar measures in preparedness and response, including restrictions on traffic and international travel; reinforcement of sanitary and quarantine measures at national borders; shutdown of work, school, and production; closure management measures for different areas at the community, regional, and national levels; and promotion of personal protection and hygiene measures, such as increased social distance. The intensity of implementing the above measures varied among countries and was based on their respective response strategies.
The Iranian government had canceled all flights from and to China since January 31.18 On February 23, the government established the National Taskforce on combatting COVID-19, chaired by the president.19 On March 5, the government launched a national mobilization plan to close all educational institutions and suspend all artistic and religious activities.20 On March 26, the government announced a ban on cross-city travel.21 The government disinfected public places on a daily basis and conducted a national program for universal virus testing. In addition, the central government mobilized all local and district governments as well as the military force and fire and special police agencies to take part in the preparedness and response efforts.22 Nevertheless, policy contradictions within the government in the early stage of the pandemic led to a lack of attention to the spread of cases across Iran and its border to several other countries.23 The Iranian government recognized its shortage in domestic medical resources, including testing reagents, hospital beds, ventilators, and personal protective equipment, and received support from China, the U.K., other countries, the WHO, and a number of international enterprises.24 – 25 On March 4 and 5, the government announced that masks and sanitizers would be allocated for free to citizens and that provinces hit severely by the pandemic would be given priority.26
Japan had adopted strict border surveillance measures at an earlier stage, strengthening airport entry quarantine in mid-January, imposing entry restrictions on February 1, and expanding denial of entry following the first death reported on February 13.27 On February 25, the Japanese government released the “Basic Policies for Novel Coronavirus Disease Control” as a guiding document for preparedness and response efforts.28 The strategy prioritized the treatment of patients with severe symptoms as well as those with underlying diseases, older adults, and pregnant women. NAT was used only for severe patients with fever of over 37.5 °C lasting for at least four consecutive days, accompanied by respiratory symptoms. On February 25, the Prime Minister of Japan called for a nationwide shutdown of primary and secondary schools and a suspension of major events, to encourage people to reduce unnecessary outings.29 The implementation of measures depended mainly on local governments and the citizens themselves.
South Korea's government at all levels responded promptly to the outbreak: on January 22, central and local governments established emergency response teams; on January 27, the government raised the alert level for COVID-19 to “alert” then to the highest level of “severe” on February 23.30 South Korea also implemented strict border surveillance measures in the early period. On February 4, it imposed a total ban on the entry of foreigners who had visited China's Hubei Province within 14 days.31 The government had taken stringent lockdown measures in Daegu and Gyeongsangbuk-do, which were heavily affected by the outbreak, and had adopted restrictions on gatherings and delayed the opening of schools.32 The government implemented large-scale testing at an earlier stage, starting the testing in seven first-tier administrative districts on January 22 and expanding the coverage of testing on February 20, and then introducing rapid, drop-off-free testing on February 26.33 – 34 In terms of the allocation of medical resources, the government prioritized the admission of severe patients to hospitals to tackle the shortage of beds; patients with mild symptoms were treated in daycare centers.35 The government encouraged people to wear masks and ensured both availability and accessibility by stabilizing prices, banning exports, restricting purchase to avoid hoarding, and allocating to vulnerable people free of charge.36
The U.K. government took steps to prevent the import of cases before March, including strengthening border testing and developing health protection regulations for COVID-19.37 On March 3, the U.K. government initiated a four-stage response plan, named “containment–delay–research–mitigate”, and announced that the U.K. entered the “delay” stage on March 10.38 On March 13, the Prime Minister announced that the government would adopt the herd immunity strategy, targeting the slow progress of the epidemic under the expectation that most people would be asymptomatic or only with mild symptom after an anonymous infection and would lead to universal immunity among the population.39 The U.K. government also declared that citizens with COVID-19 symptoms, such as a continuous cough or high temperature, must stay at home for seven days before going to a clinic. This measure was followed by the gradual imposition of prohibition on assemblies, school closures, and country lockdown.40 In terms of consolidating medical supplies and expanding the capacity of the health system to accommodate patients, the U.K. government took measures such as calling on enterprises to produce ventilators, subsidizing discharged patients to release hospital beds, and building new emergency hospitals.41 – 42
The U.S. government responded to the epidemic at an early stage by adopting strict border control measures in January, issuing the highest level of travel warning (“Do not travel to China”) and declaring a national health emergency on January 31.43 Nevertheless, in terms of testing, it was not until February 27 that the U.S. Centers for Disease Control and Prevention (CDC) lifted the requirement of “having been in an outbreak area or been exposed to a confirmed case in the past 14 days” to allow patients with suspected symptoms to get nucleic acid testing (NAT) and further eased the requirement with physician approval on March 4.44 At this time, the epidemic entered the community transmission phase, and the actual infected population was grossly underestimated. On March 13, the President of the U.S. declared a national emergency concerning the COVID-19 pandemic, and launched several financial incentives and activated wartime laws to strengthen the supply of medical materials.45 However, the U.S. federal government did not introduce a nationwide response strategy or measure, and played a rather limited part in the coordination and allocation of resources, with state governments implementing their own measures to respond to the COVID-19 pandemic.46 – 47
4. Discussion
4.1. Gaps in building resilient health systems under the resilient health system framework
As of April 15, the COVID-19 pandemic had spread from Asia to Europe and North America, where it caused a greater number of infections and deaths than in Asian countries. Countries have used the SPAR and GHS Index to evaluate their national core capacities for preparedness and response. However, the actions to cope with the COVID-19 pandemic have revealed that most countries continue to lack resilient health systems in response to public health emergencies. Our study analyzed health system resilience in five selected countries in terms of the five dimensions under the resilient health systems framework, namely, awareness, diversity, self-regulation, integration, and adaptation.1
We found several gaps in the building of resilient health systems:
The first relates to the perceptions of the strengths and weaknesses of national health systems, and the identification of the factors that may threaten the health of the population. The SPAR and GHS Index are considered as subjective and objective indicators, respectively, and the difference between the two indicators reflects, to some extent, the perception of the strengths and deficiencies of the national health system. Iran's SPAR scores was above the global average, whereas its GHS Index was the opposite. Its SPAR Scores was higher than its GHS Index in the aspects of surveillance, rapid response, and risk management. For the other four countries, their SPAR Scores was lower than their GHS Index score in some categories, such as entry surveillance and control for the U.K., human resources for the U.S., and risk communication for Japan. This discrepancy can be explained by the fact that countries with relatively well-developed health systems tend to pay more attention to their shortcomings, which in turn leads to conservative self-assessment results. In health resource management, Japan, the U.K., and the U.S. had adopted the strategy of distributing medical resources to severe patients, along with encouraging enterprises to manufacture medical and personal protective equipment to alleviate supply shortage. As for Iran, although the government intended to identify patients with COVID-19 by large-scale testing, this was made without considering the availability of medical resources. Therefore, screening has not been effectively carried out owing to the lack of necessary medical supplies, such as testing reagents.48 In contrast, South Korea had comparatively adequate medical supplies to conduct extensive testing, and had reserved hospital beds for severe cases; mild cases were managed and cared for by health care centers.49 Patient triage was achieved well in this way, avoiding the overburdening and collapse of the health system. In terms of surveillance of disease and other factors threatening the health of the population, evidence suggests that the U.S. CDC had identified the threat of COVID-19 in December 2019 through its well-developed global disease surveillance networks.50 Nevertheless, no further investigation or response was made owing to a variety of reasons. In addition, although China and WHO have made case data available since the early stage of the outbreak, all five selected countries had low-risk perceptions of COVID-19. In the U.S., where the outbreak was better controlled at the early stage owing to entry restrictions, no further preventive measures were taken to strengthen disease control until a domestic outbreak was observed. For most European and North American countries, despite the significant window of time for epidemic preparedness, the failure to prioritize the outbreak resulted in inadequate resource availability.
Second, a resilient health system should respond effectively to the health needs of the population and ensure the adequacy of government health expenditure and financial protection. During the response to the COVID-19 pandemic, the main health needs included medical materials (e.g., medical protective equipment and testing reagents), medical equipment (e.g., hospital beds and ventilators), and human resources (i.e., health care workers at all levels of the health system). For Iran and other developing countries, the lack of material reserves and productive capacity as well as the low density of health care workers made it impossible for the health system to address the people's needs and respond effectively to the pandemic, relying instead on external assistance, which was a major obstacle to preparedness and response for COVID-19.51 For the other four developed countries, the domestic productive capacity and import trade of medical materials were relatively stable. Nevertheless, many developed countries, including Japan, the U.K., and the U.S., had suffered a shortage of hospital beds to accommodate all severe patients as well as a deficiency of health care workers.52 Although health systems and health insurance schemes are known to vary across countries, the abovementioned shortages are largely due to the fact that primary health care workers, represented by general practitioners, are responsible for the majority of outpatient services and hospitals are dominated by the provision of comprehensive inpatient services, resulting in a serious shortage of hospital beds and medical equipment.53 As such, the governments of Japan, the U.K., and the U.S., had adopted a strategy that prioritizes the admission of severe patients.53 Nevertheless, the predominance of home observation for patients with mild to moderate symptoms posed significant challenges for community control and management.54 – 55 The U.K. government took steps to build new hospitals for infectious diseases, but this initiative was unlikely to be effective in containing the pandemic in the short term compared with the rapid transmission of COVID-19.56
Third, the capabilities to isolate threats and maintain core functions and to leverage outside capacity through collaboration with regional and global partners are crucial for a resilient health system. Owing to the vulnerability of its health system, Iran could not effectively respond to the COVID-19 outbreak, resulting in a great number of cases spreading to countries in the neighboring regions and globally. The other four countries have not exhibited a significant export of cases, but they had cases of spreading to other districts and cross-country as a result of insufficient control measures in the prior high-burden areas. Strengthened international cooperation and public–private partnerships are vital in the response to COVID-19. Many European and North American governments, including the U.K. and the U.S., had called on enterprises to adjust their production lines to participate in the production of necessary medical materials, which had received positive feedback. However, the attitudes of countries toward bilateral and multilateral international cooperation were inconsistent. The influence of geopolitics and trade war had pushed some Western countries, such as the U.S., to show no intention to reinforce cooperation with the Chinese government to combat the COVID-19 pandemic.56 In terms of multilateral cooperation, the U.S. government had continued to impose pressure on the WHO and failed to take the leadership in global health governance as it had previously taken in dealing with the Ebola, Zika, and H1N1 epidemics. This was not only detrimental to the U.S. efforts to build a resilient national health system and strengthen national health security but was also a loss of a unified global effort to combat the COVID-19 pandemic.
Fourth, internal collaboration within the health system, including the integration of public health and medical services, coordination with non-health actors, public engagement, and communication to build trust, all contribute to the resilience of health systems. The announcement of herd immunization strategy by the U.K. Prime Minister had caused public panic.57 The inconsistency of preparedness and response strategies between the federal and state governments in the U.S. as well as the debates between the U.S. President and some state governors over inconsistent views on COVID-19 prevented the public from having an accurate picture of the pandemic and hampered the implementation of specific measures. The South Korean government made early suggestions to the public to reduce gatherings, but owing to inappropriate communication strategies and the lack of public trust in the government, large-scale religious gatherings were not stopped, resulting in community transmission of COVID-19 and consequently posing a significant challenge to preparedness and response efforts. The same situation was observed in Iran. Iran's government delivered inconsistent messages to the public on the severity of COVID-19, resulting in the public's low attention to the pandemic.58
Fifth, another characteristic of a resilient health system is its ability to develop preparedness and response strategies and related measures promptly, and to track progress and evaluate health system performance for improvement. Each of the five selected countries put in place its response strategy or action plan. However, they were not consistent in adjusting the strategies as the pandemic progressed. Japan revised its action plan in light of the situation of the domestic pandemic situation. As of April 15, the U.S. federal government had not yet responded to the request for it to coordinate the distribution of medical supplies among the states based on the fact that medical supplies held by the states did not meet the demand. In addition, most Western governments had not been fully prepared to respond based on the situation reports issued by the WHO and other countries, including China. Making timely adjustments according to the pandemic progress requires health systems to have not only well-preformed surveillance and feedback mechanisms to identify problems and challenges, but also a flexible management and implementation framework that allows adjustments to existing strategies and measures with rapid action.
4.2. Minding the gaps: embedding IHR core capability building into health system strengthening
The COVID-19 pandemic exposed the fact that most countries, developed or developing, still have not built a resilient health system to respond to public health emergencies. For developed countries, such as Japan, South Korea, the U.K., and the U.S., the main problems highlighted in this pandemic are insufficient actions and inconsistent mechanisms for preparedness and response, including the lack of timely response to early surveillance results, inadequacy in the management and allocation of emergency supplies, and poor coordination. For developing countries, such as Iran, the priority should be to ensure adequate investment in medical resources and to identify the shortcomings in IHR core capacities and take the steps toward improvement. The five countries in this study should also strengthen communication with the public, enhance public trust in the health system, and engage society in tackling public health emergencies.
There is a new understanding that strengthening the health system and taking health security efforts for pandemic preparedness and response should be pursued in tandem, as part of the same mutually reinforcing approach to developing resilient health systems. Although state parties have committed to providing domestic resources to build core capacities, national budgets often neglect this fundamental commitment under the IHR. Many countries with limited resources have had little bandwidth to prioritize building sustainable systems for unknown threats as they have struggled to meet basic population health needs. Therefore, IHR core capability building must be embedded in health system strengthening to bridge the gap in building resilient health systems under the resilient health system framework. Studies have demonstrated the need to embed IHR core capacities in health systems across the six health system functions, where the leadership and governance function may be the most important to improving implementation.
Our study has two major limitations. First, owing to the lack of news reports and academic research results, we could not compare the effectiveness of the control measures taken by the five countries. There may be differences in the scope and stringency of the quarantine measures adopted by the five countries that, in turn, may lead to differences in the effectiveness of these measures on disease prevention and control. Second, this study only reflected the resilience of the health system in the early stage (six months) of the outbreak in the selected countries. Follow-up studies are needed to explore further the resilience of different countries’ health system at a longer time scale, covering different stages of the COVID-19 pandemic.
5. Conclusion
The recognition that resilient health systems are the front line for dealing with potential threats to global health security sheds light on the urgency of strengthening them and draws novel insights. The integration of health system strengthening and global health security will become more important given their shared objective of creating resilient health systems. Combining health system resilience and health security is a new approach to strengthening national capabilities for pandemic preparedness and response.
Author contributions
Zhebin Wang: conceptualization, writing - original draft, data curation. Yuqi Duan: writing - review & editing, data curation. Yinzi Jin: conceptualization, writing - review & editing, data curation. Zhi-Jie Zheng: conceptualization, writing - review & editing.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Funding
This paper was supported by the National Natural Science Foundation of China (No. 72042014).
References
- 1.Kruk M, Ling E, Bitton A. Building resilient health systems: a proposal for a resilience index. BMJ. 2017;357:j2323. doi: 10.1136/bmj.j2323. [DOI] [PubMed] [Google Scholar]
- 2.Kruk M, Myers M, Varpilah S, Dahn B. What is a resilient health system? Lessons from Ebola. Lancet. 2015;385(9980):1910–1912. doi: 10.1016/S0140-6736(15)60755-3. [DOI] [PubMed] [Google Scholar]
- 3.Kieny M, Dovlo D. Beyond Ebola: a new agenda for resilient health systems. Lancet. 2015;385(9963):91–92. doi: 10.1016/S0140-6736(14)62479-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . World Health Organization; Geneva: 2006. International Health Regulations (2005) [Google Scholar]
- 5.Heymann DL, Chen L, Takemi K. Global health security: the wider lessons from the West African Ebola virus disease epidemic. Lancet. 2015;385(9980):1884–1901. doi: 10.1016/S0140-6736(15)60858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report-51. https://apps.who.int/iris/bitstream/handle/10665/331475/nCoVsitrep11Mar2020-eng.pdf?sequence=1&isAllowed=y. Accessed November 19, 2020.
- 7.World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report-86. https://apps.who.int/iris/bitstream/handle/10665/331784/nCoVsitrep15Apr2020-eng.pdf?sequence=1&isAllowed=y. Accessed November 19, 2020.
- 8.Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coronavirus Disease 2019 (COVID-19): Situation Report-71. https://apps.who.int/iris/bitstream/handle/10665/331684/nCoVsitrep31Mar2020-eng.pdf?sequence=1&isAllowed=y. Accessed November 19, 2020.
- 10.Legido-Quigley H, Asgari N, Teo YY. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395(10227):848–850. doi: 10.1016/S0140-6736(20)30551-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Legido-Quigley H, Mateos-García JT, Campos VR, Gea-Sánchez M, Muntaner C, McKee M. The resilience of the Spanish health system against the COVID-19 pandemic. Lancet Public Health. 2020;5(5):e251–e252. doi: 10.1016/S2468-2667(20)30060-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heymann DL, Shindo N. WHO scientific and technical advisory group for infectious hazards. COVID-19: what is next for public health? Lancet. 2020;395(10224):542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hick JL, Biddinger PD. Novel Coronavirus and Old Lessons - Preparing the Health System for the Pandemic. N Engl J Med. 2020;382(20):e55. doi: 10.1056/NEJMp2005118. [DOI] [PubMed] [Google Scholar]
- 14.Coronavirus Disease (COVID-19) Dashboard. World Health Organization website. https://covid19.who.int/. Accessed November 19, 2020.
- 15.Checklist and Indicators for Monitoring pRogress in the Development of IHR Core Capacities in States Parties. World Health Organization website. https://www.who.int/ihr/checklist/en/. Accessed November 19, 2020.
- 16.World Health Organization. e-SPAR State Party Annual Report. https://extranet.who.int/e-spar. Accessed November 19, 2020, WHO.
- 17.2019 Global Health Security Index: Building Collective Action and Accountability. Global Health Security Index website. https://www.ghsindex.org/wp-content/uploads/2019/10/2019-Global-Health-Security-Index.pdf. Accessed November 19, 2020.
- 18.Iran Suspends Flights to and from China Amid Coronavirus Spread Concerns. PressTV Website. https://www.presstv.com/Detail/2020/01/31/617555/coronavirus-Saeed-Namaki-Iran-flights-China. Accessed November 19, 2020.
- 19.President at the Meeting of Heads of Committees of Coronavirus Task Force. Official website of the President of the Islamic Republic of Iran. http://www.president.ir/en/115065. Accessed November 19, 2020.
- 20.Iran: Schools, Social Events Shut Down in Iran Over Coronavirus Fears – CNN Video. CNN website. https://edition.cnn.com/videos/world/2020/02/24/coronavirus-iran-life-shutdown-mostaghim-lkl-intl-hnk-vpx.cnn. Accessed November 19, 2020.
- 21.Coronavirus: Iran bans internal travel to avert 'second wave'. BBC News website. https://www.bbc.com/news/world-middle-east-52039298. Accessed November 19, 2020.
- 22.Iran declares national mobilization plan after 107 total deaths confirmed. CNN website. https://edition.cnn.com/asia/live-news/coronavirus-outbreak-03-05-20-intl-hnk/h_2f932dfb4b9832eea08a8449062c0305. Accessed November 19, 2020.
- 23.Abdi M. Coronavirus disease 2019 (COVID-19) outbreak in Iran: actions and problems. Infect Control Hosp Epidemiol. 2020;41(6):754–755. doi: 10.1017/ice.2020.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xi says China Ready to Provide Further Assistance for Iran Against COVID-19 Epidemic. Xinhuanet website. http://www.xinhuanet.com/english/2020-03/14/c_138877556.htm. Accessed November 19, 2020.
- 25.€5 million to Help Fight Coronavirus in Iran: E3 Statement, March 2020. GOV.UK website. https://www.gov.uk/government/news/e3-statement-on-5-million-to-help-fight-coronavirus-in-iran-02-march-2020. Accessed November 19, 2020.
- 26.Iran Using Tent Hospitals as it Faces Shortage of Beds. CNN website. https://edition.cnn.com/asia/live-news/coronavirus-outbreak-03-04-20-intl-hnk/h_4ef375682e9bb07bc64a2220a7f7f136. Accessed November 19, 2020.
- 27.Japan Tightens Border Controls Over COVID-19, but Power to Quarantine Limited. The Japan Times website. https://www.japantimes.co.jp/news/2020/03/09/national/japan-border-controls-coronavirus/. Accessed November 19, 2020.
- 28.Basic Policies for Novel Coronavirus Disease Control by the Government of Japan (Summary). Website of Ministry of Health, Labour and Welfare, Japan. https://www.mhlw.go.jp/content/10900000/000617686.pdf. Accessed November 19, 2020.
- 29.Japan Orders Nationwide Shutdown of Schools Over Coronavirus. France 24 website. https://www.france24.com/en/20200227-japan-orders-nationwide-shutdown-of-schools-over-coronavirus. Accessed November 19, 2020.
- 30.Ha KM. Emergency response to the outbreak of COVID-19: the Korean case. Microbes Infect. 2020;22(4–5):159–161. doi: 10.1016/j.micinf.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.South Korea Raises Threat Alert Level. Nytimes website. https://www.nytimes.com/2020/02/23/world/asia/china-coronavirus.html. Accessed November 19, 2020.
- 32.S. Korea to Take Maximum Quarantine Steps in Daegu, Surrounding Province Against Coronavirus. The Korea Herald website. http://www.koreaherald.com/view.php?ud=20200225000190. Accessed November 19, 2020.
- 33.Lee D, Lee J. Testing on the Move: South Korea’s rapid response to the COVID-19 pandemic. Transp Res Interdiscip Perspect. 2020;5:100111. doi: 10.1016/j.trip.2020.100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwon KT, Ko JH, Shin H, Sung M, Kim JY. Drive-through screening center for COVID-19: a safe and efficient screening system against massive community outbreak. J Korean Med Sci. 2020;35(11):e123. doi: 10.3346/jkms.2020.35.e123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.How South Korea Solved Its Acute Hospital-Bed Shortage. Wall Street Journal website. https://www.wsj.com/articles/how-south-korea-solved-its-acute-hospital-bed-shortage-11584874801. Accessed November 19, 2020.
- 36.COVID-19: lessons from South Korea - Health Systems Global. Health Systems Global website. https://www.healthsystemsglobal.org/blog/406/COVID-19-Lessons-from-South-Korea.html. Accessed November 19, 2020.
- 37.The Health Protection (Coronavirus, Restrictions) (England) Regulations 2020. Legislation. gov. uk website. http://www.legislation.gov.uk/uksi/2020/350/made. Accessed November 19, 2020.
- 38.What Does Britain Know About Coronavirus That the Rest of Europe Doesn't? CNN website. https://edition.cnn.com/2020/03/13/uk/uk-coronavirus-response-boris-johnson-intl-gbr/index.html. Accessed November 19, 2020.
- 39.Coronavirus: UK Still 'In Containment Phase' of Virus Response. BBC News website. https://www.bbc.com/news/uk-51781018. Accessed November 19, 2020.
- 40.Boris Johnson Issues Stay-at-home Order, Sending the UK into Lockdown to Fight Coronavirus Pandemic. CNN website. https://edition.cnn.com/2020/03/23/uk/uk-coronavirus-lockdown-gbr-intl/index.html. Accessed November 19, 2020.
- 41.Coronavirus: Nightingale Hospital Opens at London's ExCel centre. BBC News website. https://www.bbc.co.uk/news/uk-52150598. Accessed November 19, 2020.
- 42.Call for Businesses to Help Make NHS Ventilators. GOV. UK website. https://www.gov.uk/government/news/production-and-supply-of-ventilators-and-ventilator-components. Accessed November 19, 2020.
- 43.Secretary Azar Declares Public Health Emergency for United States for 2019 Novel Coronavirus. Website of U.S. Department of Health & Human Services. https://www.hhs.gov/about/news/2020/01/31/secretary-azar-declares-public-health-emergency-us-2019-novel-coronavirus.html. Accessed November 19, 2020.
- 44.Evaluating and Testing Persons for Coronavirus Disease 2019 (COVID-19). U.S. Centers for Disease Control and Prevention website. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-criteria.html. Accessed November 19, 2020.
- 45.Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak. The White House website. https://www.whitehouse.gov/presidential-actions/proclamation-declaring-national-emergency-concerning-novel-coronavirus-disease-covid-19-outbreak/. Accessed November 19, 2020.
- 46.States Cannot Fight Coronavirus Alone. The Federal Government Must Step up. Website of Fortune Media IP Limited. https://fortune.com/2020/03/21/coronavirus-state-federal-government-travel-tests/. Accessed November 19, 2020.
- 47.Covid-19 and America's Political System. The Economist website. https://www.economist.com/united-states/2020/04/02/covid-19-and-americas-political-system. Accessed November 19, 2020.
- 48.Davarpanah AH, Mahdavi A, Sabri A. Novel screening and triage strategy in iran during deadly coronavirus disease 2019 (COVID-19) epidemic: value of humanitarian teleconsultation service. J Am Coll Radiol. 2020;17(6):734–738. doi: 10.1016/j.jacr.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Song JY, Yun JG, Noh JY, Cheong HJ, Kim WJ. Covid-19 in South Korea – challenges of subclinical manifestations. N Engl J Med. 2020;382(19):1858–1859. doi: 10.1056/NEJMc2001801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.The White House v Covid-19. The Economist website. https://www.economist.com/united-states/2020/04/11/the-white-house-v-covid-19. Accessed November 19, 2020.
- 51.Gereffi G. What does the COVID-19 pandemic teach us about global value chains? The case of medical supplies. J Int Bus Policy. 2020;3(3):287–301. [Google Scholar]
- 52.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages – the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382(18):e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 53.Emanuel E.J., Persad G., Upshur R. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020;382(21):2049–2055. doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 54.Liu Y., Wang Z., Ren J. A COVID-19 risk assessment decision support system for general practitioners: design and development study. J Med Internet Res. 2020;22(6):e19786. doi: 10.2196/19786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hollander J.E., Carr B.G. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 56.Nelson B. Too little or too much? Missing the goldilocks zone of hospital capacity during covid-19. BMJ. 2020;369:m2332. doi: 10.1136/bmj.m2332. [DOI] [PubMed] [Google Scholar]
- 57.Coronavirus: Some Scientists Say UK Virus Strategy is 'Risking Lives'. BBC News website. https://www.bbc.com/news/science-environment-51892402. Published 2020. Accessed November 19, 2020.
- 58.Iran Cannot Fight Covid-19 with Conspiracy Theories. The Economist website. https://www.economist.com/leaders/2020/03/26/iran-cannot-fight-covid-19-with-conspiracy-theories. Accessed November 19, 2020.