Abstract
Purpose
The current study aimed to compare the clinical and radiographic results of the 3D-printed artificial vertebral body (3DP-AVB) and titanium mesh cage (TMC) for the treatment of Kümmell’s disease (KD) complicated by neurological deficits.
Patients and Methods
From January 2014 to July 2018, 28 consecutive patients diagnosed with KD and nerve injuries in our department were treated by posterior vertebral column resection and internal fixation. The patients were divided into two groups (3DP-AVB group and TMC group) based on the different anterior column reconstruction implants. Clinical and radiographic parameters were used to evaluate the outcomes.
Results
The two groups achieved excellent clinical and radiographic results 1 month after surgery with no significant difference (P>0.05), while 3DP-AVB group showed better outcomes compared with TMC group during the follow-up after 6 months (P<0.05). The risk of subsidence in 3DP-AVB group was lower than that in TMC group (41.6% vs 87.5%, P<0.05), and severe subsidence (≥5 mm) was correlated with the recurrence of back pain and bad daily life function. No significant difference was found in the improvement of neurological function between the two groups (P>0.05). The blood loss and operation time in 3DP-AVB group were significantly less than both in TMC group (P<0.05).
Conclusion
The lower incidence of cage subsidence, with a better long-term efficacy in maintaining the height of the fused segment, relieving back pain, and improving daily life function indicates that the 3DP-AVB may be a superior alternative for KD with neurological deficits.
Keywords: Kümmell’s disease, 3D printing, artificial vertebral body, spinal reconstruction, vertebral column resection, neurological deficits
Introduction
Kümmell’s disease (KD), first described in 1891, is a clinical scenario that individuals suffer a trivial spinal trauma, eventually develop a progressive, painful, angular kyphosis in the thoracolumbar region after sustaining an asymptomatic period of months to years.1,2 Although a consistent pathomechanism has not yet been reached, the etiopathogenetic hypothesis of ischemic posttraumatic vertebral necrosis is the most supported theory.3,4 KD usually occurs after osteoporotic vertebral compression fractures (OVCFs) of the elderly, which suggests that its occurrence was associated with osteoporosis.5 Intravertebral cleft (IVC), a widely reported radiological sign related to KD,6 is an eventual finding that strongly suggests the presence of osteonecrosis, though it is not the pathognomic sign of KD.7
Due to the lack of a unified standard for the underlying pathogenesis and imaging diagnosis, the most appropriate treatment for KD is still controversial.8 Percutaneous vertebral augmentation (PVA), a minimally invasive procedure, has achieved an outstanding effect for KD after failed conservative treatment.9,10 Owing to the progressive kyphosis and intravertebral instability at the IVC site, patients with advanced KD are prone to nerve injury,11 which is a relative contraindication for cement usage.12 In recent years, a short-segment fixation with polymethylmethacrylate (PMMA) augmentation had been employed for KD complicated by neurological deficits,13–16 however, some scholars realized that this approach might not be sufficient to support the long-term stability.11 Therefore, considering serious comorbidities and severe osteoporosis in elderly patients, one-stage posterior osteotomy and fixation is more suitable for treating KD with neurological deficits compared with anterior or anterior and posterior approaches for a long-term effect.8,17,18
Various techniques, such as titanium mesh cage (TMC), bone grafts, PMMA, or expandable titanium cage, have been used for the anterior column reconstruction (ACR) with advantages of early biomechanical stabilization and high fusion rates, as well as inevitable disadvantages of subsidence and donor-site complications.19,20 For the past few years, 3D-printed artificial vertebral body (3DP-AVB) with good implant fit and osteoinduction implants has gained traction in spine surgery.21,22 As far as we know, no comparative studies have investigated the outcomes of 3D-AVB and TMC for patients with KD complicated by neurological deficits. The present study aimed to comparatively assess the clinical outcomes of 3D-AVB vs TMC for this special condition after single posterior vertebral column resection (PVCR) and provide a basis for selecting the appropriate anterior reconstruction method.
Patients and Methods
Patients
The current study was designed as a retrospective analysis of clinical and radiologic parameters. The report of this retrospective study was in agreement with the Strobe guidelines. From January 2014 to July 2018, 28 consecutive patients confirmed KD complicated by neurological deficits were treated by one-stage PVCR in our department. According to the different ACR implants, they were divided into two groups (12 patients in the 3DP-AVB group and 16 in the TMC group). General data of patients, including age, gender, lesion level, bone mineral density (BMD), fusion segments, and follow-up period are presented in Table 1.
Table 1.
Compare Baseline Characteristics and Surgical Results of the Two Groups
| Patient Characteristics | 3DP-AVB Group (n=12) | TMC Group (n=16) | t/Χ2 | P values |
|---|---|---|---|---|
| Age (year) | 70.75±7.96 | 73.44±8.06 | −0.878 | 0.388 |
| Gender (M/F, n) | 3/9 | 5/11 | 0.131 | 0.717 |
| BMD (T-score) | −3.35±0.64 | −3.11±0.55 | −1.053 | 0.302 |
| Lesion segment (n) | T10 (1),T11 (2),T12 (6),L1 (3) | T10 (2),T11 (2),T12 (5),L1 (7) | 1.483 | 0.686 |
| Fusion levels (n) | 4.67±0.78 | 4.75±0.86 | −0.265 | 0.793 |
| Follow-up (months) | 35.50±8.13 | 32.38±7.33 | 1.066 | 0.296 |
| Operative duration (min) | 164.50±51.19 | 217.63±36.29 | −3.218 | 0.003 |
| Blood loss (mL) | 399.42±107.98 | 530.31±155.68 | −2.492 | 0.019 |
| Complications | 1 | 3 | 0.608 | 0.436 |
The criteria to define the KD includes: (1) delayed post-traumatic osteonecrosis: patients may initially develop low back pain after a minor trauma, and finally local kyphosis even nerve injury may occur after an asymptomatic period of months to years;23 (2) X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) show an IVC sign in the lesion segment.5,11,16 The inclusion criteria were as follows: (1) single-level KD in stage III;24 (2) patients with cord compression and the functional status from B to D (American Spinal Injury Association (ASIA) grade); (3) BMD T-score of all patients was less than −2.5, which was measured by dual-energy X-ray absorptiometry at lumbar spine and hip; and (4) failure of conservative treatment. The exclusion criteria: (1) multiple-level KD; (2) KD patients in stage I or II without neurologic symptoms;24 (3) pathological fracture caused by bone metastasis, multiple myeloma, infection, or tuberculosis.
Surgical Procedures
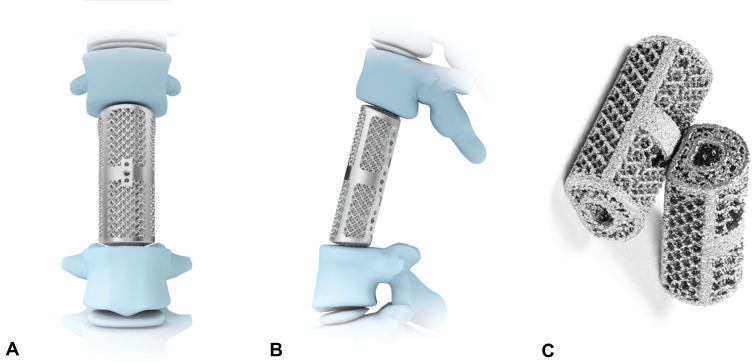
All patients were performed a one-stage PVCR which had been described in detail by previous studies,11,25 and followed by anterior reconstruction with a TMC (Fule Science & Technology Co., Ltd., Beijing, China) or a 3DP-AVB (Beijing AK Medical Co., Ltd., Beijing, China) and posterior reconstruction with 2–3 levels above and below bone cement-augmented pedicle screw fixation (Cox Spinal Screw-Rod System, Fule Science & Technology Co., Ltd., Beijing, China). The 3DP-AVB was approved for clinical use since 2016 by the State Drug and Food Administration of China, and we employed it in 12 consecutive patients since June 2016 in our hospital. The 3DP-AVB, a highly structured and porous simulation of the trabecular structure of vertebral cancellous bone, was made of Ti6-Al4-V titanium alloy using Electron Beam Melting technique. The pore diameter is 800 ± 200 μm, and the porosity is about 80%. The 3DP-AVB is designed to the cylinder with a diameter of 15 mm × 21 mm in thoracic and 18 mm × 24 mm in lumbar. The height of the 3DP-AVB is 25~35 mm, according to the preoperative CT measurement. The angle between the upper and lower endplates of the 3DP-AVB ranges from 0° to 8° (Figure 1).
Figure 1.
3D-printed artificial vertebral body: oblique (A), lateral (B), and superior (C) views.
After general anesthesia, the patients were placed in a prone position with somatosensory-evoked potentials and motor-evoked potentials for spinal cord monitoring. The lesion level was positioned with a C-arm, a posterior midline approach was used to expose the posterior structure of the level involved. Then, bone cement-augmented screws were inserted bilaterally 2–3 segments above and below the target vertebra. After that, a complete laminectomy-facetectomy was performed at the lesion site for decompression. A short rod was used to temporarily stability one side of spine. On the other side, the injured vertebra including adjacent discs was piecemeal resected via a transpedicular approach. Most of the contralateral vertebrae can be removed by crossing the midline in an extremely oblique direction. Then, a TMC or 3DP-AVB filled with autologous or artificial bone was inserted to act as an anterior support. After reducing the kyphosis, two rods were tightened in an alternating manner. Posterolateral fusion was performed over the fixed segments with autografted or artificial bone.
Patients were usually allowed to walk with wearing a brace 5–7 days after the operation. Orthosis was used for at least three months until solid fusion was achieved.
Clinical Parameters Evaluation
Preoperatively and at every routine postoperative clinical follow-up (1-month, 6-month, and final follow-up), visual analog scale (VAS, range 0~10, 0 means no pain, and 10 means maximal pain) score for back pain and the Oswestry Disability Index (ODI, range of 0~50, the higher score indicates more severe disability) were performed. The neurological status was evaluated via the ASIA grading system. Operative time, blood loss, and complications related to anesthesia and operation procedures were also recorded.
Radiographic Parameters Evaluation
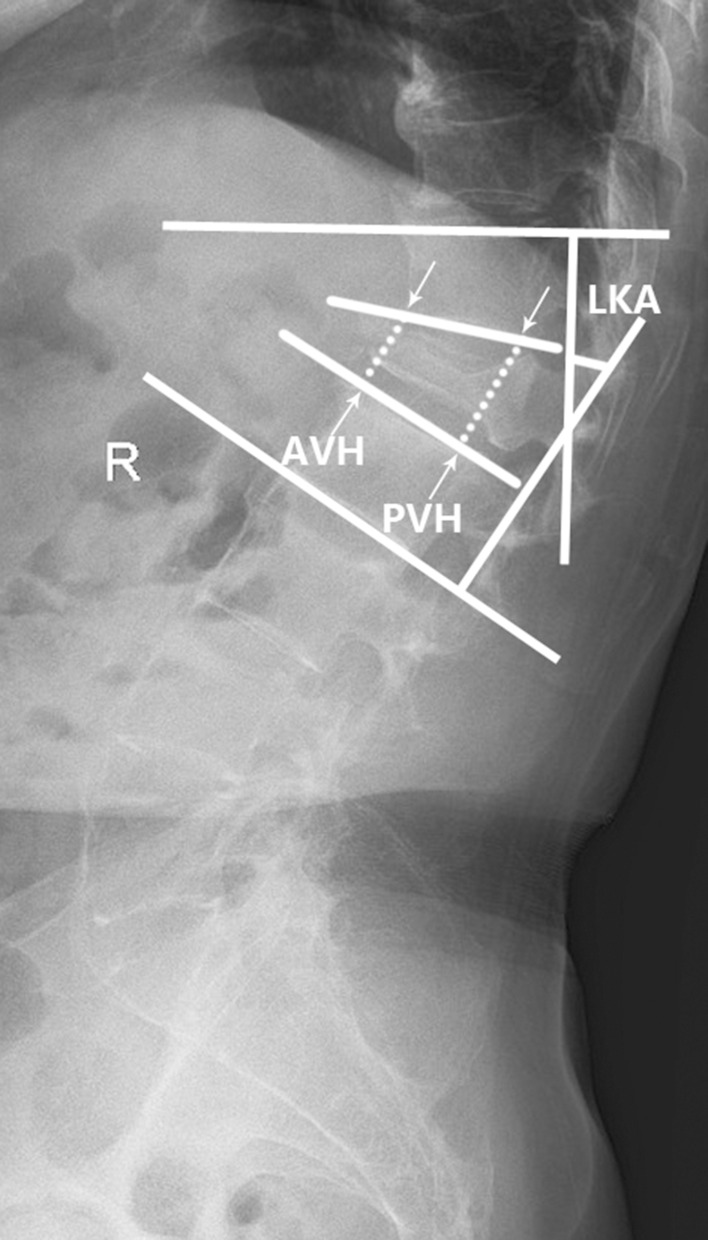
Radiographic data were collected preoperatively, 1- and 6-month postoperatively, and final follow-up. The local kyphotic angle (LKA, Figure 2) was determined by measuring the Cobb angle between upper and lower adjacent segments of diseased vertebrae.11 The intervertebral disc height was measured using standing neutral lateral radiographs, evaluated as an average of the anterior and posterior margins of the intervertebral space (anterior vertebral height (AVH) and posterior vertebral height (PVH), Figure 2).26,27 The loss of intervertebral disc height was defined as cage subsidence (no, ≤2 mm; mild, 2~5 mm; severe, ≥5 mm).28 Graft fusion was evaluated using Bridwell grading criteria.29 All imaging data were measured by the Picture Archiving and Communication Systems (Carestream Health, Inc., Shanghai, China).
Figure 2.
Measuring method of local kyphotic angle (LKA), anterior vertebral height (AVH), and posterior vertebral height (PVH).
Statistical Analysis
All statistical analyses were performed using Statistical Package for Social Sciences Computer software (SPSS version 22.0. SPSS Inc., Chicago, IL, USA). Repeated measure analysis of variance and Mann–Whitney U-test were used for intragroup comparisons. The intergroup data were compared using paired t-tests or Fisher’s exact tests. The level of significance was set at 0.05.
Results
Patient Characteristics and Surgical Results
There was no significantly difference in general data of patients between the two groups (P>0.05, Table 1). The mean follow-up period was 35.50±8.13 months (range, 25–49 months) in the 3DP-AVB group and 32.38±7.33 months (range, 22–47 months) in the TMC group (P>0.05, Table 1). The operative duration and blood loss in the 3DP-AVB group were significantly lower than those in the TMC group (164.50±51.19 minutes vs 217.63±36.29 minutes and 399.42±107.98 mL vs 530.31±155.68 mL, respectively; P<0.05, Table 1). No serious intraoperative or postoperative complications were observed. One patient in the 3DP-AVB group had dural tears with cerebrospinal fluid leakage. In the TMC group, one patient had asymptomatic cement leakage, and two patients had delayed wound healing, and they were all cured by conservative treatment. No significant difference regarding complications between the two groups in our study (P>0.05, Table 1). There were no implant-related complications such as screw loosening, screw backout, cage breakage, screw fracture, and rod breakage at the final follow-up.
Clinical Findings
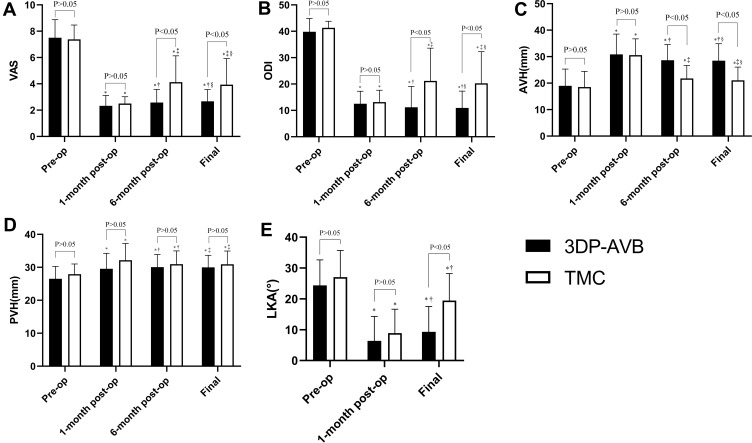
The VAS scores in the 3DP-AVB group and TMC group improved from preoperatively 7.50±1.03 and 7.25±1.07, to 2.33±0.78 and 2.50±0.52 1-month postoperatively, 2.58±1.00 and 4.13±2.00 6-month postoperatively, and 2.67±0.89 and 3.94±1.98 at final follow up (F=125.79, P<0.05; F=33.29, P<0.05; respectively, Figure 3A,,). The follow-up VAS did not significantly change in the 3DP-AVB group (1-month vs 6-month, 1-month vs final; P>0.05, Figure 3A), but significantly increased in the TMC group (1-month vs 6-month, 1-month vs final; P<0.05, Figure 3A). The 6-month postoperative and final VAS in the TMC group were significantly higher than those in the 3DP-AVB group (P<0.05, Figure 3A). As a similar result, the ODI in the 3DP-AVB group and TMC group preoperatively were 39.83±5.06 and 41.31±2.52 and dropped to 12.50±4.76 and 13.13±4.50 1-month postoperatively, 11.17±7.90 and 21.19±10.93 6-month postoperatively, and 10.92±6.40 and 20.25±12.03 at final follow up (F=211.17, P<0.05; F=221.73, P<0.05; respectively, Figure 3B). The follow-up ODI also did not significantly change in the 3DP-AVB group (1-month vs 6-month, 1-month vs final; P>0.05, Figure 3B), but significantly increased in the TMC group (1-month vs 6-month, 1-month vs final; P<0.05, Figure 3B). The 6-month postoperative and final ODI in the TMC group were significantly higher than those in the 3DP-AVB group (P<0.05, Figure 3B). The ASIA in the two groups improved significantly at the final follow-up compared with preoperatively (P<0.05, Table 2), and no significant differences were found during the final follow-up between the two groups (P>0.05, Table 2).
Figure 3.
Clinical and radiographic outcomes. (A–E) *P<0.05 compared with the preoperative data. (A–C) †P>0.05 compared with the 1-month postoperative data, ‡P<0.05 compared with the 1-month postoperative data, §P>0.05 compared with the 6-month postoperative data. (D) †P>0.05 compared with the 1-month postoperative data; ‡P>0.05 compared with the 6-month postoperative data. (E) †P<0.05 compared with the 1-month postoperative data.
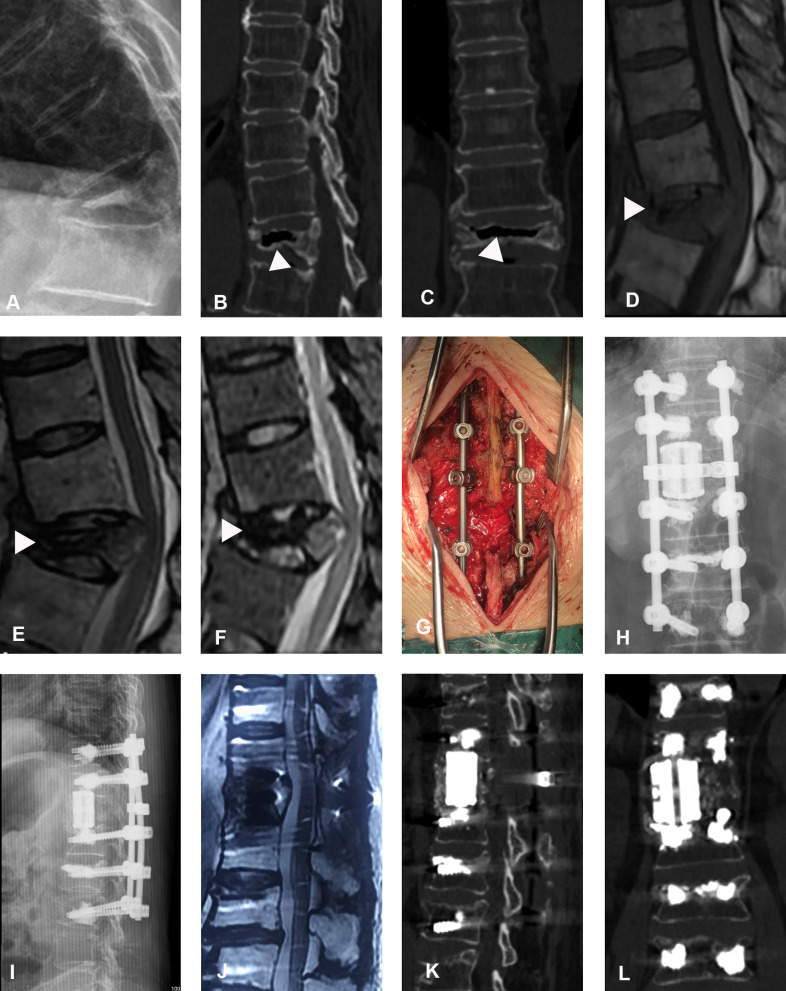
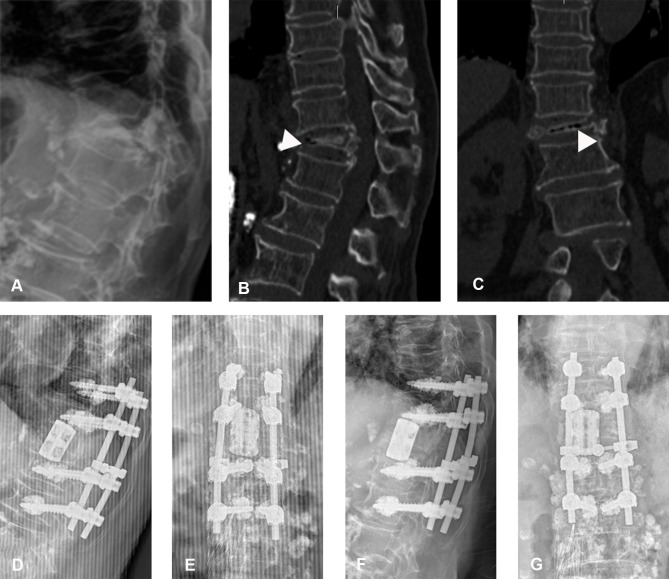
Figure 4.
An 82-year-old female patient experienced Kümmell’s disease complicated by neurological deficits and used a 3D-printed artificial vertebral body (3DP-AVB). (A) T11 collapsed fracture was shown in preoperative X-rays. (B and C) Coronal and sagittal CT showed an intravertebral cleft (IVC) (white triangle). (D–F) MRI showed a decreased signal in IVC (white triangle). (G) Intraoperative images. (H and I) Immediate postoperative X-rays showed that a 3DP-AVB was implanted. (J) Postoperative sagittal T2-weighted MRI showed a sufficient spinal cord decompression. (K and L) Coronal and sagittal CT showed that no subsidence occurred at the final follow-up.
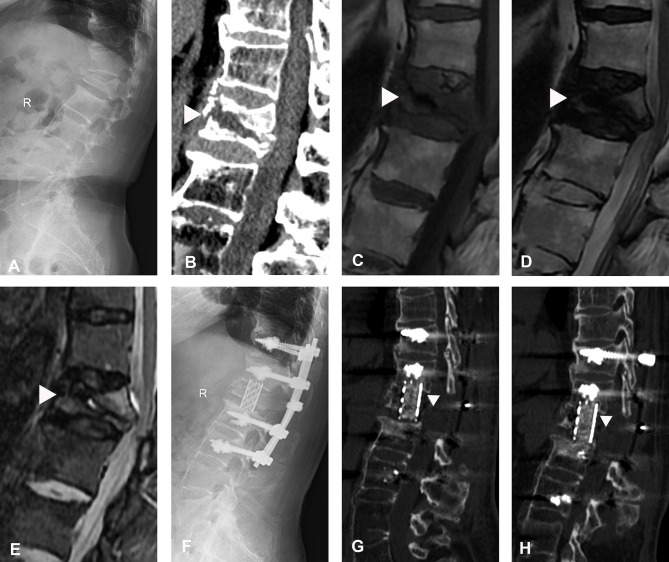
Figure 5.
The 3D-printed artificial vertebral body (3DP-AVB) was used in a 75-year-old female patient with stage III Kümmell’s disease. (A) Preoperative X-rays showed T12 collapsed fracture and thoracolumbar kyphosis. (B and C) An intravertebral cleft sign (white triangle) was shown in preoperative CT scans. (D–G) Postoperative and final follow-up plain radiographs showed no cage subsidence and kyphosis recurrence.
Figure 6.
A titanium mesh cage (TMC) for stage III Kümmell’s disease. (A and B) Preoperative radiographs and CT scans revealed collapsed fracture and kyphosis at L1 with an intravertebral cleft (IVC) sign (white triangle). (C–E) Preoperative MRI showed a decreased signal of IVC (white triangle). (F) No subsidence in immediate postoperative plain radiographs. (G and H) Final follow-up CT scans showed kyphosis recurrence with TMC subsidence (white triangle).
Table 2.
Compare Preoperative and Final Follow-Up ASIA Between the Two Groups
| Group | Preoperative ASIA | Final Follow-Up ASIA | |||||
|---|---|---|---|---|---|---|---|
| B | C | D | B | C | D | E | |
| 3DP-AVB (n=12) | 1 | 6 | 5 | 1 | 1 | 3 | 7* |
| TMC (n=16) | 2 | 7 | 7 | 1 | 1 | 2 | 12* |
| Χ2 | 0.176 | 0.964 | |||||
| P | 0.916 | 0.810 | |||||
Note: *P<0.05 Compare with preoperative and final follow-up.
Radiographic Findings
All radiographic parameters, including AVH, PVH, and LKA, were evaluated preoperatively, 1-month and 6-month postoperatively, and at the final follow-up. The AVH, PVH, and LKA of the two groups significantly improved during postoperative follow-up (P<0.05, Figure 3C–E), and no significant differences existed between the two groups 1-month postoperatively (P>0.05, Figure 3C–E). The follow-up AVH, PVH in the 3DP-AVB group, and PVH in the TMC group did not significantly change (1-month vs 6-month, 1-month vs final; P>0.05, Figure 3C and D). However, the AVH in the TMC group significantly decreased in the TMC group (1-month vs 6-month, 1-month vs final; P<0.05, Figure 3C) and the 6-month postoperative and final AVH in the TMC group were significantly lower than those in the 3DP-AVB group (P<0.05, Figure 3C). At the final follow-up, the loss of LKA in the TMC group was significantly greater than in the 3DP-AVB group (10.57° vs 2.96°, P<0.05, Figure 3E). All the subsidence occurred before 6 months after the operation because there were no significant differences existed between the 6 months after the operation and final follow-up in the two groups (P>0.05, Table 3). The subsidence was less in the 3DP-AVB group compared with the TMC group (0.97 mm vs 5.39 mm, P<0.05, Table 3), and the risk of subsidence in the 3DP-AVB group was lower than that in the TMC group (41.6% vs 87.5%, P<0.05, Table 3). The final VAS, ODI and loss of LKA in the severe-subsidence group were significantly higher than those in the non- and mild-subsidence groups (P<0.05, Table 4) and there was no significant difference in the no- and mild-subsidence groups (P>0.05, Table 4). Three cases were shown in Figures 4–6.
Table 3.
Compare the Subsidence Outcomes and Subsidence Grade Between the Two Groups
| Group | Subsidence Outcomes (mm) | Subsidence Grade | |||
|---|---|---|---|---|---|
| 6 Months After Operation | Final Follow-Up | No | Mild | Severe | |
| 3DP-AVB (n=12) | 0.86±2.20 | 0.97±2.23* | 7 | 4 | 1 |
| TMC (n=16) | 5.00±2.23 | 5.39±2.50* | 2 | 6 | 8 |
| t/Χ2 | 4.894 | 4.839 | 8.219 | ||
| P values | 0.000 | 0.000 | 0.016 | ||
Note: *P>0.05 compare the 6 months after operation and final follow-up subsidence.
Table 4.
Radiographic and Clinical Outcomes According to Different Subsidence Grades
| No Subsidence (n= 9) |
Mild Subsidence (n= 10) |
Severe Subsidence (n=9) |
|
|---|---|---|---|
| Final VAS | 2.67±0.71 | 2.40±1.26a | 5.22±1.39bc |
| Final ODI | 9.44±2.46 | 9.30±2.11a | 30.78±6.44bc |
| Loss of LKA (°) | 3.31±3.44 | 4.62±3.06a | 14.29±6.62bc |
Notes: aP>0.05 compare mild subsidence and no subsidence; bP<0.05 compare severe subsidence and no subsidence; cP<0.05 compare severe subsidence and mild subsidence.
Discussion
Although KD is not fully defined yet, it has been widely regarded as delayed post-traumatic vertebral collapse with a unique imaging feature of IVC.2–5,23,24 In 2004, Li et al24 divided the course of KD into 3 stages: Stage I, patients may suffer from back pain due to a minor trauma, while some patients may be symptom-free; Stage II, a mild vertebral collapse may occur with intact posterior cortical wall because of dynamic instability in the IVC; Stage III, radiographs show a severe vertebral collapse with posterior cortical breakage and patients usually experience a serious kyphosis deformity even neural deficits.
Minimally invasive procedure such as PVA has been widely used for KD patients at stage I or II; however, the results reported in the literature are inconsistent.30,31 Several studies32,33 have revealed that IVC might be an independent risk factor for recollapse of the augmented vertebrae after PVA. For stage III KD with neurologic deficits, PVP and PKP are no longer suitable attributed to unable relieve spinal cord compression and reconstruct spinal stability.8,23 Therefore, open surgeries, including anterior, posterior, and a combination of anterior and posterior approaches, have been proposed for this condition.18 Theoretically, the anterior approach may be the most appropriate treatment via providing directly resecting the lesions and reconstructing the stability of the anterior column.34 However, this method, especially combined with a posterior approach, is inappropriate for KD patients with serious comorbidities and severe osteoporosis.34 A less-invasive procedure, short-segment fusion with vertebroplasty, has become an alternative therapy for KD patients in poor general condition,13,14,16,17 however, with the potential for insufficient anterior column support and increasing loss of kyphosis correction.11,34,35 Due to the IVC, a solid cement often forms during vertebroplasty, resulting in less mechanical interlock between the PMMA and cancellous bone, therefore, increase the potential for recollapse of the augmented vertebrae, leading to further kyphosis even PMMA cement dislodgment.11,35 Our previous study showed that PVCR had better long-term clinical and radiographic results compared with posterior short-segment fusion with vertebroplasty.11 Thus, PVCR is still the most secure method for treating KD with neurological deficits.
Providing a robust spinal reconstruction after PVCR for KD patients is a challenge for surgeons. Currently, TMC is the most commonly used for ACR, however, with the incidence of implant-related complications from 14.3% to 21.6%.18 Previous studies have shown that server TMC subsidence (≥5 mm) is an important risk factor related to instrumentation failure.28,36 The subsidence has been proven to correlate with osteoporosis, progressive resection of the endplate, a sharp edge of mesh, or over intervertebral distraction.37–40 From June 2016, 12 consecutive patients with KD underwent anterior reconstruction with the 3D-AVB were involved in our center and compared with the previous 16 consecutive patients who restoration with the TMC. Our study showed that the subsidence was less with the group of 3DP-AVB than the TMC group (average, 0.97 mm vs 5.39 mm) and a lower risk of severe subsidence in the 3DP-AVB group (8.3% vs 50%, P<0.05). Although both groups achieved similar short-term effects, including VAS, ODI, AVH, PVH, and LKA (P>0.05), the long-term outcomes were different; the TMC group had significant loss of AVH and LKA due to the subsidence compared to the 3DP-AVB group (P<0.05). These observations suggest that the 3DP-AVB provides more excellent stability than the TMC. We attribute this result to the following aspects: (1) a larger diameter endcap of 3DP-AVB allows for an expansion of the bone-implant interface, which distributes point-loading and loads the periphery of the endplates where there is thicker cortical bone, and eventually reduces the risk of subsidence;22,41,42 (2) withYoung’s modulus more similar to native human bone (0.5–20 GPa), 3DP-AVB may reduce subsidence and “stress shadowing effect” compared with traditional implants;43 (3) the porosity of 3DP-AVB made by Ti6-Al4-V titanium alloy in our study can enhance the delivery of osteoinductive factors as well as facilitate osteoconduction, thus potentially improving bony ingrowth.21,42 An additional screw fixation system attached to the 3DP-AVB that can connect to the pedicle screws and rods system also can be designed to further strengthen the support between the anterior column and posterior column.44
A patient-specific/individualized 3DP-AVB has been explored to fit the unique spinal pathoanatomy of complex congenital, traumatic and neoplastic pathologies.45 Previous studies have indicated that operative time can be significantly reduced by the use of custom 3DP-AVB.45 At the same time, the individualized prosthesis does require extensive design and manufacturing processes prior to production, which spends a lot of money and time.22 In our study, the lesion segments of all patients were located in the thoracolumbar segment with less adjacent segment degeneration, so there was no need to use a custom prosthesis. The “off-the-shelf” 3DP-AVB produced by Beijing AK Medical Co., Ltd. could provide sufficient angle and height to fit with adjacent vertebrae based on the preoperative CT measurement. Compared with TMC, there is no need to cut 3DP-AVB during the operation, which significantly reduced intraoperative time and blood loss in our series (P<0.05).
Although the clinical consequence relevance of cage subsidence among the literature was quite different,37,41,46,47 several studies proposed that loss of intervertebral height due to the subsidence could lead to buckling of the yellow ligament, foraminal stenosis, and eventually cause second nerve injury.41,48 Different from previous researches,48 the loss of height of the anterior border was much larger than that of the posterior because employment of posterior pedicle internal fixation system was to improve posterior column structural rigidity and prevent subsidence occurring at the posterior rim of the TMC, which leads to the great loss of kyphosis correction in our series. Therefore, it will not cause nerve injury due to buckling of the yellow ligament and stenosis of the neural foramen and there was no significant difference in ASIA during the last follow-up between the two groups (P>0.05). Our study showed that mild subsidence did not produce significant clinical results, while severe subsidence was correlated with recurrence of back pain and bad daily life function, owing to the more substantial loss of kyphosis correction. As is widely understood, improper sagittal alignment of the spine results in inefficient energy use, maximizing muscle tension caused by exhaustive bracing and spine instability, and may contribute to low back pain.48 As kyphosis was aggravated related to the subsidence, patients in the TMC group complained of more severe back pain and restrictions on activities than those in the 3D-AVB group (P<0.05). Cage subsidence occurred in 67.9% (19/28) and appeared before 6 months after the operation, while all patients achieved solid fusion at final follow-up, which is consistent with the results of previous studies.37,47,48 Although internal fixation failure is common in cage subsidence with osteoporosis, it did not occur in our research. The outstanding result may be related to the use of a long segmental bone cement screw technique.
The present study has several limitations. First, the cases included in this study were single vertebral lesions, and the effect of the 3DP-AVB in multiple remains to be further discussed. Second, because of the limited sample size, we did not establish a control group for other implants, whether the 3DP-AVB is the best choice is open to question. Third, a prospective randomized controlled trial with a large sample size is needed to verify the reliability of the results in our study.
Conclusions
This retrospective study demonstrated that both the 3DP-AVB and TMC resulted in effective clinical and radiographic outcomes when used to treat KD with neurological deficits for anterior column reconstruction after PVCR. Compared with TMC, 3DP-AVB with less blood loss and operation time, lower incidence of cage subsidence, and better long-term efficacy in maintaining the height of the fused segment, reducing the loss of kyphosis correction, relieving back pain, and improving daily life function may be a better alternative.
Funding Statement
There is no funding to report.
Data Sharing Statement
The data supporting this study are available from the corresponding author for a reasonable request.
Ethics Approval
Our study was approved by the institutional ethics committee of the Beijing Hospital of Traditional Chinese Medicine, Capital Medical University.
Consent to Participate
Written informed consent was obtained from patients included in the study.
Disclosure
The authors declare that there are no conflicts of interest in this work.
References
- 1.Steel HH. Kümmell’s disease. Am J Surg. 1951;81(2):161–167. doi: 10.1016/0002-9610(51)90206-1 [DOI] [PubMed] [Google Scholar]
- 2.Swartz K, Fee D. Kümmell’s disease: a case report and literature review. Spine (Phila Pa 1976). 2008;33(5):152–155. doi: 10.1097/BRS.0b013e3181657f31 [DOI] [PubMed] [Google Scholar]
- 3.He D, Yu W, Chen Z, Li L, Zhu K, Fan S. Pathogenesis of the intravertebral vacuum of Kümmell’s disease. Exp Ther Med. 2016;12(2):879–882. doi: 10.3892/etm.2016.3369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ma R, Chow R, Shen FH. Kummell’s disease: delayed post-traumatic osteonecrosis of the vertebral body. Eur Spine J. 2010;19(7):1065–1070. doi: 10.1007/s00586-009-1205-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lim J, Choi SW, Youm JY, Kwon HJ, Kim SH, Koh HS. Posttraumatic delayed vertebral collapse: Kummell’s disease. J Korean Neurosurg Soc. 2018;61(1):1–9. doi: 10.3340/jkns.2017.0505.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Formica M, Basso M, Cavagnaro L, Formica C, Zanirato A, Felli L. Kümmell disease: illustrative case for definition criteria. Spine J. 2016;16(10):e707–e708. doi: 10.1016/j.spinee.2016.03.035 [DOI] [PubMed] [Google Scholar]
- 7.Maldague BE, Noel HM, Malghem JJ. The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology. 1978;129(1):23–29. doi: 10.1148/129.1.23 [DOI] [PubMed] [Google Scholar]
- 8.Zhang X, Hu W, Yu J, Wang Z, Wang Y. An effective treatment option for Kümmell disease with neurological deficits. Spine (Phila Pa 1976). 2016;41(15):E923–E930. doi: 10.1097/BRS.0000000000001467 [DOI] [PubMed] [Google Scholar]
- 9.Chang J-Z, Bei M-J, Shu D-P, Sun C-J, Chen J-B, Xiao Y-P. Comparison of the clinical outcomes of percutaneous vertebroplasty vs. kyphoplasty for the treatment of osteoporotic Kümmell’s disease: a prospective cohort study. BMC Musculoskelet Disord. 2020;21(1):238. doi: 10.1186/s12891-020-03271-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jiang J, Gu F, Li Z, Zhou Y. The clinical efficacy and experience of bipedicular percutaneous vertebroplasty combined with postural reduction in the treatment of Kümmell’s disease. BMC Musculoskelet Disord. 2020;21(1):82. doi: 10.1186/s12891-020-3113-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei H, Dong C, Zhu Y. Posterior fixation combined with vertebroplasty or vertebral column resection for the treatment of osteoporotic vertebral compression fractures with intravertebral cleft complicated by neurological deficits. Biomed Res Int. 2019;2019. doi: 10.1155/2019/4126818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li KC, Li AFY, Hsieh CH, Liao TH, Chen CH. Another option to treat Kümmell’s disease with cord compression. Eur Spine J. 2007;16(9):1479–1487. doi: 10.1007/s00586-006-0094-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee SH, Kim ES, Eoh W. Cement augmented anterior reconstruction with short posterior instrumentation: a less invasive surgical option for Kummell’s disease with cord compression. J Clin Neurosci. 2011;18(4):509–514. doi: 10.1016/j.jocn.2010.07.139 [DOI] [PubMed] [Google Scholar]
- 14.Zhang GQ, Gao YZ, Zheng J, et al. Posterior decompression and short segmental pedicle screw fixation combined with vertebroplasty for Kümmell’s disease with neurological deficits. Exp Ther Med. 2013;5(2):517–522. doi: 10.3892/etm.2012.833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen L, Dong R, Gu Y, Feng Y. Comparison between balloon kyphoplasty and short segmental fixation combined with vertebroplasty in the treatment of Kümmell’s disease. Pain Physician. 2015;18(4):373–381. doi: 10.1097/BRS.0b013e318238f29a [DOI] [PubMed] [Google Scholar]
- 16.Kim HS, Heo DH. Percutaneous pedicle screw fixation with polymethylmethacrylate augmentation for the treatment of thoracolumbar intravertebral pseudoarthrosis associated with Kummell’s osteonecrosis. Biomed Res Int. 2016;2016. doi: 10.1155/2016/3878063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cho Y. Posterior vertebrectomy and circumferential fusion for the treatment of advanced thoracolumbar Kümmell disease with neurologic deficit. Asian Spine J. 2017;11(4):634–640. doi: 10.4184/asj.2017.11.4.634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu F, Chen Z, Lou C, et al. Anterior reconstruction versus posterior osteotomy in treating Kümmell’s disease with neurological deficits: a systematic review. Acta Orthop Traumatol Turc. 2018;52(4):283–288. doi: 10.1016/j.aott.2018.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y, Quan Z, Zhao Z, et al. Evaluation of anterior cervical reconstruction with titanium mesh cages versus nano-hydroxyapatite/polyamide66 cages after 1- or 2-level corpectomy for multilevel cervical spondylotic myelopathy: a retrospective study of 117 patients. PLoS One. 2014;9(5):e96265. doi: 10.1371/journal.pone.0096265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ganau M, Cebula H, Fricia M, et al. Surgical preference regarding different materials for custom-made allograft cranioplasty in patients with calvarial defects: results from an internal audit covering the last 20 years. J Clin Neurosci. 2020;74:98–103. doi: 10.1016/j.jocn.2020.01.087 [DOI] [PubMed] [Google Scholar]
- 21.Tong Y, Kaplan DJ, Spivak JM, Bendo JA. Three-dimensional printing in spine surgery: a review of current applications. Spine J. 2020;20(6):833–846. doi: 10.1016/j.spinee.2019.11.004 [DOI] [PubMed] [Google Scholar]
- 22.Burnard JL, Parr WCH, Choy WJ, Walsh WR, Mobbs RJ. 3D-printed spine surgery implants: a systematic review of the efficacy and clinical safety profile of patient-specific and off-the-shelf devices. Eur Spine J. 2020;29(6):1248–1260. doi: 10.1007/s00586-019-06236-2 [DOI] [PubMed] [Google Scholar]
- 23.Huang YS, Hao DJ, Wang XD, et al. Long-segment or bone cement–augmented short-segment fixation for Kummell disease with neurologic deficits? A comparative cohort study. World Neurosurg. 2018;116:e1079–e1086. doi: 10.1016/j.wneu.2018.05.171 [DOI] [PubMed] [Google Scholar]
- 24.Li K-C, Wong T, Kung F, Li A, Hsieh C. Staging of Kümmell’s disease. J Musculoskelet Res. 2004;08(01):43–55. doi: 10.1142/S0218957704001181 [DOI] [Google Scholar]
- 25.Wang H, Ding W. Posterior vertebral column resection through unilateral osteotomy approach for old lumbar fracture combined with Kummell disease. World Neurosurg. 2018;109:147–151. doi: 10.1016/j.wneu.2017.09.148 [DOI] [PubMed] [Google Scholar]
- 26.Okano I, Jones C, Salzmann SN, et al. Endplate volumetric bone mineral density measured by quantitative computed tomography as a novel predictive measure of severe cage subsidence after standalone lateral lumbar fusion. Eur Spine J. 2020;29(5):1131–1140. doi: 10.1007/s00586-020-06348-0 [DOI] [PubMed] [Google Scholar]
- 27.Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013;19(1):110–118. doi: 10.3171/2013.4.SPINE12319 [DOI] [PubMed] [Google Scholar]
- 28.Wang H, Guo J, Wang S, et al. Instrumentation failure after posterior vertebral column resection in adult spinal deformity. Spine (Phila Pa 1976). 2017;42(7):471–478. doi: 10.1097/BRS.0000000000001844 [DOI] [PubMed] [Google Scholar]
- 29.Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Spine (Phila Pa 1976). 1995;20(12):1410–1418. doi: 10.1097/00007632-199506020-00014 [DOI] [PubMed] [Google Scholar]
- 30.Tsai -T-T, Chen W-J, Lai P-L, et al. Polymethylmethacrylate cement dislodgment following percutaneous vertebroplasty: a case report. Spine (Phila Pa 1976). 2003;28(22):E457–E460. doi: 10.1097/01.brs.0000096668.54378.25 [DOI] [PubMed] [Google Scholar]
- 31.Li X, Lou X, Lin X, Du J. Refracture of osteoporotic vertebral body concurrent with cement fragmentation at the previously treated vertebral level after balloon kyphoplasty: a case report. Osteoporos Int. 2014;25(5):1647–1650. doi: 10.1007/s00198-014-2626-4 [DOI] [PubMed] [Google Scholar]
- 32.Yu WB, Jiang XB, Liang D, Xu WX, Ye LQ, Wang J. Risk factors and score for recollapse of the augmented vertebrae after percutaneous vertebroplasty in osteoporotic vertebral compression fractures. Osteoporos Int. 2019;30(2):423–430. doi: 10.1007/s00198-018-4754-8 [DOI] [PubMed] [Google Scholar]
- 33.Yu W, Xu W, Jiang X, Liang D, Jian W. Risk factors for recollapse of the augmented vertebrae after percutaneous vertebral augmentation: a systematic review and meta-analysis. World Neurosurg. 2018;111(August2017):119–129. doi: 10.1016/j.wneu.2017.12.019 [DOI] [PubMed] [Google Scholar]
- 34.Kashii M, Yamazaki R, Yamashita T, et al. Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures - Anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J. 2013;22(7):1633–1642. doi: 10.1007/s00586-013-2759-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang SC, Chen WJ, Yu SW, Tu YK, Kao YH, Chung KC. Revision strategies for complications and failure of vertebroplasties. Eur Spine J. 2008;17(7):982–988. doi: 10.1007/s00586-008-0680-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matsumoto M, Watanabe K, Tsuji T, et al. Late instrumentation failure after total en bloc spondylectomy. J Neurosurg Spine. 2011;15(3):320–327. doi: 10.3171/2011.5.SPINE10813 [DOI] [PubMed] [Google Scholar]
- 37.Ji C, Yu S, Yan N, et al. Risk factors for subsidence of titanium mesh cage following single-level anterior cervical corpectomy and fusion. BMC Musculoskelet Disord. 2020;21(1):32. doi: 10.1186/s12891-019-3036-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Daubs MD. Early failures following cervical corpectomy reconstruction with titanium mesh cages and anterior plating. Spine (Phila Pa 1976). 2005;30(12):1402–1406. doi: 10.1097/01.brs.0000166526.78058.3c [DOI] [PubMed] [Google Scholar]
- 39.Wu J, Luo D, Ye X, Luo X, Yan L, Qian H. Anatomy-related risk factors for the subsidence of titanium mesh cage in cervical reconstruction after one-level corpectomy. Int J Clin Exp Med. 2015;8(5):7405–7411. [PMC free article] [PubMed] [Google Scholar]
- 40.Oh KW, Lee JH, Lee J-H, Lee D-Y, Shim HJ. The correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clin Spine Surg. 2017;30(6):E683–E689. doi: 10.1097/BSD.0000000000000315 [DOI] [PubMed] [Google Scholar]
- 41.Fengbin Y, Jinhao M, Xinyuan L, Xinwei W, Yu C, Deyu C. Evaluation of a new type of titanium mesh cage versus the traditional titanium mesh cage for single-level, anterior cervical corpectomy and fusion. Eur Spine J. 2013;22(12):2891–2896. doi: 10.1007/s00586-013-2976-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Xu N, Wei F, Liu X, et al. Reconstruction of the upper cervical spine using a personalized 3d-printed vertebral body in an adolescent with ewing sarcoma. Spine (Phila Pa 1976). 2016;41(1):E50–E54. doi: 10.1097/BRS.0000000000001179 [DOI] [PubMed] [Google Scholar]
- 43.Li P, Jiang W, Yan J, et al. A novel 3D printed cage with microporous structure and in vivo fusion function. J Biomed Mater Res Part A. 2019;107(7):1386–1392. doi: 10.1002/jbm.a.36652 [DOI] [PubMed] [Google Scholar]
- 44.Chung KS, Shin DA, Kim KN, Ha Y, Yoon DH, Yi S. Vertebral reconstruction with customized 3-dimensional−printed spine implant replacing large vertebral defect with 3-year follow-up. World Neurosurg. 2019;126:90–95. doi: 10.1016/j.wneu.2019.02.020 [DOI] [PubMed] [Google Scholar]
- 45.Mobbs RJ, Choy WJ, Wilson P, McEvoy A, Phan K, Parr WCH. L5 en-bloc vertebrectomy with customized reconstructive implant: comparison of patient-specific versus off-the-shelf implant. World Neurosurg. 2018;112:94–100. doi: 10.1016/j.wneu.2018.01.078 [DOI] [PubMed] [Google Scholar]
- 46.Liu X, Chen Y, Yang H, et al. The application of a new type of titanium mesh cage in hybrid anterior decompression and fusion technique for the treatment of continuously three-level cervical spondylotic myelopathy. Eur Spine J. 2017;26(1):122–130. doi: 10.1007/s00586-016-4888-3 [DOI] [PubMed] [Google Scholar]
- 47.Wu WJ, Jiang LS, Liang Y, Dai LY. Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J. 2012;21(7):1374–1382. doi: 10.1007/s00586-011-2131-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen Y, Chen D, Guo Y, et al. Subsidence of titanium mesh cage: a study based on 300 cases. J Spinal Disord Tech. 2008;21(7):489–492. doi: 10.1097/BSD.0b013e318158de22 [DOI] [PubMed] [Google Scholar]