Abstract
Affordable virtual reality technology is now widely available. Billions of dollars are currently being invested into improving and mass producing virtual reality and augmented reality products. Consumer ready immersive virtual reality and augmented reality technologies may help maximize the medical outcome of patients undergoing hand therapy. Being in VR helps reduce the patients’ pain, making it less painful for patients to move their hand/fingers during hand therapy, and gamified virtual reality can help motivate the patient to perform therapeutic hand exercises, and make hand therapy more fun. In addition, VR may be used to help monitor how well patients are doing their hand therapy exercises, and to quantify whether adherence to treatment increases long term functionality. Additional research and development into using virtual reality as a tool for hand therapist is recommended for both acute pain and persistent pain patient populations.
Introduction
Excessive pain during medical procedures is a world wide medical problem.1,2,3 For example, preventing infection via frequent wound cleaning is crucial for surviving a severe burn injury. Unfortunately, most children with large severe burn injuries report severe to excruciating pain during these crucial burn wound debridement/scrubbing sessions in the ICU tankroom, despite treatment with powerful analgesics shortly before the wound care.4 Excessive pain during medical procedures increases patients’ risk of developing expensive long-term medical issues such as persistent/chronic pain and/or PostTraumatic Stress Disorder (PTSD). In addition to traumatic memories for the original burn injury accident/event (e.g., a fire), memories for traumatic wound cleaning sessions can form pathological memory “hot spots” needing future psychotherapy for PTSD. There is a growing urgency to develop effective non-pharmacologic analgesics.7,8
The current brief review explores the potential of immersive virtual reality to enhance analgesia for hand therapy, to make physical therapy (PT)/occupational therapy (OT) more fun, and to help motivate patients to cooperate with their hand therapist. As discussed below, VR hand therapy has potential for a wide range of patient populations needing hand therapy, including acute pain and potentially chronic pain patients.
Psychological influences on pain perception
Pain is a subjective experience of the patient, and pain has a strong psychological component. Unhelpful psychological influences work against the pain medications. Fear, anxiety, depression,9 and expectations of pain,10 memories for previous painful experiences,11,12,13 the direction patients look/focus their attention,14 and other psychological factors can unhelpfully increase how much pain patients experience during painful medical procedures.15 Fortunately, the opposite is also true. Psychological treatments such as attention distraction can help reduce how much acute procedural pain patients experience during medical procedures such as wound cleaning, physical therapy, or occupational therapy for a wide range of medical problems. Therefore, psychological and pharmacologic approaches are often combined. Psychological treatments (and medications) that reduce depression, fear, anxiety, patients’ expectations of pain, and/or catastrophizing, can help reduce the patient’s pain and may increase the effectiveness of the pharmacologic analgesics. For example, reducing patients’ expectations of how much pain they are about to experience has been shown to helpfully reduce the intensity of nociceptive pain signals entering the brain.10
Attention distraction
Attention distraction is one of the simplest psychological treatments for acute pain. However, the most widely used conventional distraction, listening to music during wound care, is a step in the right direction but has limited analgesic effectiveness.16-19 Adjunctive immersive virtual reality is emerging as an unusually effective high tech distraction that takes distraction to a whole new level and can result in large, clinically meaningful reductions in acute pain. During virtual reality, patients look into a pair of VR goggles, and interact with virtual objects in a computer-generated virtual reality world during painful medical procedures. The essence of immersive virtual reality is the user’s illusion of “being there” in the 3D computer generated world, as if the virtual world is a place they are visiting, an illusion known as ‘presence” or “feeling present” in virtual reality.20
The logic of how virtual reality analgesia works
Although more research is needed to investigate the mechanism of how VR works to reduce acute pain, researchers propose that VR reduces pain via an attentional mechanism.21-29 The logic is as follows. Pain requires attention.30,31 During medical procedures with No VR, burn patients typically watch the nurse clean their burn wound during their wound care sessions, and much of the patient’s attention is directed towards the painful procedure and pain-related stimuli in the hospital room. The patient sees objects, nurses and their own unbandaged burn wounds in the wound care room that patients have learned to associate with pain, via aversive conditioning from previous painful experiences in the same wound care room. During No VR, patients are both physically and mentally in the hospital wound care room. In contrast, virtual reality takes the patient’s mind to a different place. Virtual reality puts the brain into “divided attention” mode. Instead of all of their attention being directed towards pain, now a considerable portion of the patients limited attentional resources are diverted into the VR goggles and focused on the computer-generated virtual world, flooding the brain with pleasant sensory input. Researchers propose that VR uses up so much attention, that the patient’s brain has fewer attentional resources available to process incoming nociceptive signals.21,22,23 fMRI brain scan studies show significant reductions in subjective pain ratings, and significant reductions in pain-related brain activity during virtual reality vs. during No VR.32-33 See Figure 1. In one fMRI study, the reduction of pain-related brain activity during VR was comparable to a moderate dose of hydromorphone.33
Figure 1.
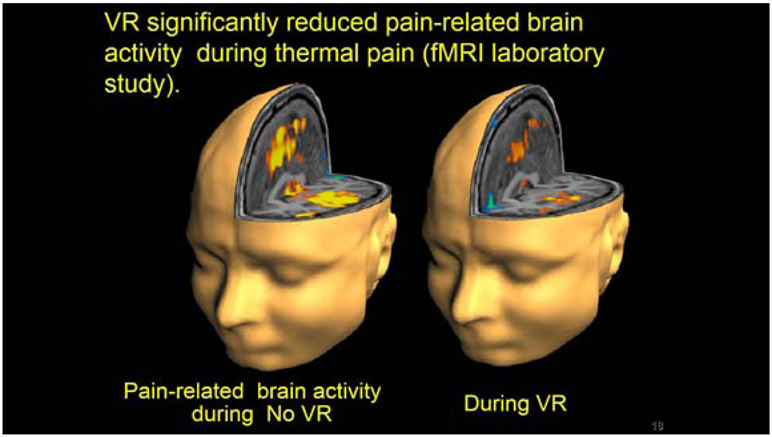
fMRI brain scans showed large reductions in pain related brain activity during virtual reality. Image copyrighted, used with permission.
Clinical studies show growing clinical evidence that virtual reality reduces acute procedural pain during hand therapy.
A number of studies have explored the use of VR to distract burn patients from their acute pain during PT/OT skin stretching exercises.23 See Figures 2 and 3. Burned skin has a natural inclination to contract and harden (hyperossification) during the healing process. Skin contraction has the consequence of reducing skin elasticity, and reducing limb range of motion, which can lead to weakening muscles, and reduced ability to use the injured limb, and can eventually lead to permanent disability. Passive range of motion during the rehabilitation process can be painful, especially for children with large severe burn injuries who are already receiving several painful medical procedures on a daily basis. Virtual reality helps reduce the amount of pain experienced by the burn patients during therapy sessions.23
Figure 2.

A pediatric burn patient using virtual reality during occupational therapy range of motion exercises. Photo copyrighted, used with permission.
Figure 3:
A pediatric burn patient using virtual reality pain distraction during physical/occupational therapy. Photo copyrighted, used with permission.
In a study by Carrougher et al., 2009,34 burn patients rated their pain during physical therapy range of motion exercises on two different days. Patients received their usual pain medications on both days. On one day they performed range of motion exercises while “in” virtual reality, and on the other day, they performed their range of motion exercises during No Virtual Reality (treatment order randomized). Patients reported large and significant reductions in pain when they received VR during physical therapy while achieving equal range of motion angle in VR vs. No VR (i.e., patients stretched as far during VR as during no VR).34 See also Schmitt et al., 2001 and Soltani et al., 2018.35,36
The improvements in range of motion achieved during hospitalization can be quickly lost after discharge if the patient does not continue to perform their PT/OT exercises at home. Although home exercise programs are an important predictor of treatment outcomes,37 non-compliance rates can be high,38,39 thus impacting results. In the future, patients may be more willing to perform their hand therapy homework exercises using gamified virtual reality systems customized by the hand therapist to encourage and motivate patients to make repetitious prescribed therapeutic motions (to score points in a custom virtual reality game, and gradually work their way up to more difficult levels of game play, etc.).
VR analgesia during burn wound cleaning procedures
In the first study to test whether immersive VR can act as an adjunctive non-pharmacologic analgesic,22 two male adolescent patients rated how much pain they felt during burn wound care. Each patient received their usual pain medications before wound care. Each patient had several staples removed from a healing skin grafted burn wound by the wound care nurse while the patient 1) played a conventional PlayStation Nintendo video game (the “No VR” plausible control condition). The patients then had an equal number of staples removed while 2) wearing a VR helmet and “going into” an immersive computer-generated virtual reality (within subjects, within-wound care design, treatment order randomized). Each of the two patients reported large reductions in pain during wound care during staple removal while in virtual reality, compared to their pain during staple removal during the non-immersive Nintendo video game (a plausible No VR control condition) during the same wound care procedure.22 In other words, VR reduced how much pain the adolescents experienced during burn wound care, and in a subsequent study, patients even reported having more fun during burn wound care during VR.4
SnowWorld (www.vrpain.com; see Figure 4), is the first immersive VR world specifically designed for pain reduction.23,40 In SnowWorld, patients float slowly through a 3D computer generated snowy canyon, where they interact with virtual snowmen, penguins and igloos. Virtual objects freeze and shatter when hit by snowballs, with sound effects, and music (e.g., by Paul Simon) playing in the background.
Figure 4.
SnowWorld: A screenshot. Patients float slowly through a 3D computer generated virtual world, during painful medical procedures. Image copyrighted, used with permission.
In a military study conducted at Brooke Army Medical Center Institutes of Surgical Research in San Antonio Texas, soldiers with combat-related burn injuries reported large reductions in pain during wound care using VR (SnowWorld) vs. standard of care, (usual pain medications with no VR).41,42,43 See Figures 5 and 6.
Figure 5.
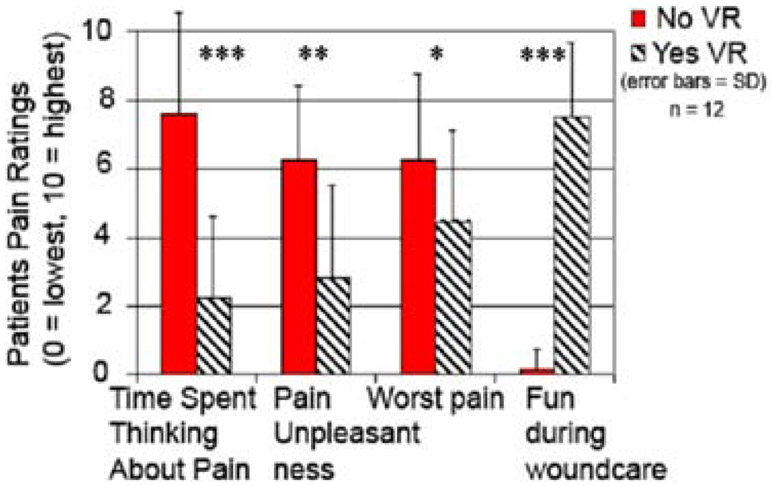
Soldiers with combat-related burn injuries reported significant reductions in worst pain intensity during VR, and significantly more fun during VR. (Image copyrighted, used with permission).
Figure 6.

A soldier with combat-related burn injuries at Brooke Army Medical Center Institutes of Surgical Research in San Antonio Texas. The custom robot-like arm goggle holder holds the VR goggles near the patient with little or no contact with the patient, so the patient does not have to wear a VR helmet (image copyrighted, used with permission).
In a clinical pediatric VR analgesia study by Hoffman et al., 2019,4 using SnowWorld, 48 children with very large severe burn injuries (burns on 40% of their bodies, on average), received standard of care pain medications with No VR for some portions of their burn wound debridement (burn wound scrubbing) session and the children “went into” VR for other portions of the same burn wound care session (treatment order randomized). During VR, these pediatric burn patients reported significant reductions in worst pain intensity, significant reductions in pain unpleasantness, patients spent significantly less time thinking about their pain during wound care, and wound care was significantly more fun.4 Encouragingly, VR continued to be effective at reducing patients’ pain and increasing how much fun patients experienced during wound care, even when used during several different wound care sessions per patient on different days.4
Many patients have burns on their heads or face that make it difficult for them to wear conventional VR helmets on their heads. To address this problem, Hoffman et al., 2019, Maani et al., 2011a, Maani et al, 2011b, and Hoffman et al., 20144, 40-44 used a custom made robot-like goggle holder to hold the VR goggles near the patient’s eyes, with little or no contact between the patient and the VR system, so patients did not have to wear a VR helmet.
VR analgesia has now been shown to reduce pain for a wide range of patient populations.45-51 A VR analgesia study at the University of Montreal found significant reductions in pain during burn wound care in young children (average age 2 years old).45
Hoxhallari et al., 201951 explored using VR during hand surgery during wide awake local anesthesia. VR significantly reduced patients’ anxiety and increased fun during the injection and during the hand surgery.
Recent Major Advances in VR technology, and future directions for using VR and other emerging technologies to help patients needing hand therapy.
The early VR systems were very heavy (8 lb VR helmets in the early 1990s, 50 lbs for the VR computer), and very expensive (e.g., $90,000 for the VR system researchers used in the first VR analgesia studies in the 1990s).21-22 Most VR analgesia studies conducted before 2016 have been conducted in hospital and University settings, using expensive pre-Oculus VR technology.
The cost of a highly immersive VR system dropped very dramatically in 2016 (Oculus and HTC VIVE, SONY and other new high quality, low cost, mass produced VR helmets became available to mainstream consumers). Historically, high tech computer companies make conventional video game hardware (e.g., Xbox) very inexpensive, often selling the video game station hardware at a loss. But they later make huge profits on the software (e.g., video games). Following this same pattern as conventional video game marketing, major tech companies have begun mass marketing millions of VR helmets per year. VR hardware is inexpensive, and is continuing to get less expensive each year, while the quality of VR technology (e.g., VR goggles) is rapidly improving.
Virtual reality goggles
With the naked eye, the human visual field is approximately 220 degrees horizontal. VR goggles do a reasonably good job of presenting visual stimuli to the fovea of the human eye, but VR helmets partially limit peripheral vision (limited field of view). Because of the small size of the VR eyepieces/optics, patients essentially see the virtual world while wearing blinders that partially block peripheral vision. Early laboratory studies have shown that 60 degree field of view VR goggles were significantly more effective at reducing pain compared to 35 degree field of view VR goggles.52 In 2013, the price of a 90 degree field of view VR helmet was $35,600. Only three years later, in 2016, the price of a 90 degree FOV helmet dropped from $35,600 to $600. So in other words, in 2016, a 90 degree field of view VR helmet became $35,000 less expensive, per helmet. footnote 1 Affordable VR hand therapy technology is now possible.
Eye tracking
Burn patients with large severe burn injuries often have burned hands, making it challenging for the patients to use their hands to control a computer mouse during burn wound cleaning sessions. One new option recently became commercially available: immersive virtual reality goggles with eye tracking technology. Miniature video cameras mounted inside the VR goggles track the patients eye movements and can tell the VR system which virtual objects the patient is looking at in VR. Thus patients can use their eye movements to interact with the virtual world. For example, in SnowCanyon (www.bigenvironments.com, www.vrpain.com), burn patients can aim snowballs at virtual snowmen, by simply looking at the snowman they want to hit with a Snowball.53 Hands free interactivity with VR via eye tracking could be especially valuable for patients with limited hand mobility, e.g., double amputees, stroke patients, and paralyzed or partially paralyzed patients.
Optical Hand Tracking
Thanks to recent improvements in very low cost optical tracking, (e.g., LEAP motion, https://www.leapmotion.com/) and related tracking technologies, camera based hand tracking can be used as input to the VR computer. In the future, patients will be able to perform therapeutic hand movements, wrist movements, and/or movement gestures to interact with virtual reality as part of their rehabilitation. While in virtual reality, hand movements in the real world (e.g., patients clinching and unclinching a fist) can be captured by video cameras attached to the VR helmet, and communicated to the virtual reality software.54 The patient does not have to hold any controllers in their hands, and does not have to wear gloves. The patient wearing virtual reality goggles sees his/her cyberhand clinching and unclinching, and the patient can use these movements of their virtual hand to interact with virtual objects in the computer generated world (see Figure 7 and Figure 8). Being in VR helps reduce the patients’ pain, making it less painful for patients to move their hand/fingers during hand therapy, and gamified virtual reality can be programmed to help motivate the patient to perform therapeutic hand exercises, to make hand therapy more fun. According to one study55 PT/OT involving VR with a LEAP Motion control optical hand tracking system (40 min OT = 20 min VR on four treatments) increased finger ROM, reduced scar thickening, and improved hand functioning compared to patients who received 60 minutes of OT + No VR, on multiple treatments.
Figure 7.
Using optical camera hand tracking technology mounted on their virtual reality helmet (e.g., VRgineering.com XTAL as shown above) allows hand therapy patients to use their real hand gestures to control their cyberhand gestures allowing patients to interact with virtual objects in the virtual world. (copyrighted image, used with permission). Haptic feedback using sound waves can further enhance the illlusion, www.ultraleap.com/haptics/
Figure 8.
At the higher end of the new VR market, a new highly immersive VR helmet named XTAL is available at VRgineering.com, allowing high realism in VR. This helmet has 180 degrees field of view, and comes with magic leap optical hand tracking/cyberhand technology already integrated.
Using VR to measure dynamic range of motion during performance of daily tasks
As described by Shefer-Eini et al.,54 clinicians have traditionally used a goniometer to measure range of motion during extension and flexion motions of the wrist, fingers and other joints as the “gold standard” measurement of joint range of motion. However, the goniometer only gives “snapshots” whereas VR optical tracking technology can measure wrist and hand movements in real time, as the patient performs various real world tasks. VR camera tracking allows measurement of more complex and ecologically valid movements of the wrist and fingers during performance of daily tasks. The first few generations of camera based tracking were initially too expensive and required a technician, and even today the measurements still need further validation.54 However, due in part to recent multi-billion dollar investments in VR and related technologies, camera tracking is undergoing rapid improvements for immersive virtual reality applications, at a fraction of the previous cost, and these technologies have a number of potential near future medical applications for hand and wrist therapy and beyond, that may quickly disseminate to hand therapy applications during the next few years. In the near future, camera based hand, finger and wrist “motion capture” will also become commercially available with untethered (no wires) VR helmets for VR, and for some helmet models no laptop will be required. VR technology is quickly becoming easier for novice VR users to set up and use, and less expensive (e.g., allowing home use).
Tech experts predict that medical applications of virtual reality will emerge as the second largest application of virtual reality (second only to using virtual reality for entertainment).
Virtual reality works for acute pain, what about for chronic pain?
As describe above, there is growing evidence that immersive virtual reality distraction can help reduce acute pain, e.g., during painful medical procedures.4, 44, 50 Immersive virtual reality distraction is a perfect match for reducing acute pain for 20 minutes or less, while the person is wearing the VR goggles and/or looking into the VR goggles, and interacting with the virtual world, (although longer VR sessions with occasional breaks are becoming more feasible thanks to less nauseogenic VR technology and calm VR worlds).
There is much less research (but growing interest) on whether immersive virtual reality can reduce chronic persistent pain. Encouragingly, preliminary unpublished evidence suggests that virtual reality distraction can temporarily reduce some types of chronic pain, at least during the time that the patient is in virtual reality (while they are wearing the VR helmet and interacting with the virtual world. For example, PBS reporter Miles O’Brien, an amputee with phantom limb pain, reported reductions in his own phantom limb pain during virtual reality, see the third story at https://www.pbs.org/newshour/show/understanding-science-pain-help-virtual-reality. Presumably, when used simply for pain distraction, when the patient takes off the VR helmet, their chronic pain may return. However, beyond distraction, as discussed next, new VR worlds specifically designed to help reduce persistent pain, could in theory permanently change/improve the way patients perceive pain, even after the patient takes off their VR helmet.7,8,50,56
Virtual reality has previously been used to enhance the effectiveness of conventional cognitive behavioral clinical therapy (e.g., Virtual Reality exposure therapy to treat phobias,57-59 post-traumatic stress disorder,60-62 for training VR mindfulness skills,63-66 and patient education).67 Educating patients about the neuroscience of pain (e.g., pre-surgically), can help change how patients interprete their pain,68 and can improve patients satisfaction, reduce healthcare costs, and communicate to patients that it is important for them to stay as active as possible.69 Chronic pain health care professionals can also benefit from pain neuroscience education.67 Researchers have begun to explore pain neuroscience education delivered via virtual reality.70 Similarly, mindfulness skills training can teach patients new pain coping skills (e.g., mindfulness skills) that they can use later when they are no longer in VR. This could help reduce anxiety64 and could potentially help reduce chronic pain, and/or improve patients attitudes and behavior towards persistent pain (e.g., to become less fearful and more acceptant of pain). As discussed below, VR may help permanently reduce pathological phantom limb pain in amputees (an early example of VR therapy for chronic pain).
Traditional Low Tech Mirror therapy for phantom limb pain.
After amputation, amputees often report pain sensations in the missing limb, a phenomenon known as “phantom limb pain”. For example, one patient had a severe injury to their hand, which included severe cramps and pain in their hand. The doctors amputated the patient’s hand, and yet the amputee continued to experience sensations of cramping and pain in their “phantom limb”, even though they no longer had a hand. Although the phantom limb pain-related disease mechanism is not well understood,71,72,73 it may be the result of maladaptive brain plasticity… “mainly caused by reorganisation in the primary somatosensory cortex, presumably characterised by functional degradation of the missing hand representation and remapping of other body part representations.”73, p. 174 In the 1990s, Ramachandran and Rogers-Ramachandran74 experimented with an unusual technique of treating phantom limb patients using “mirror therapy”, using a simple low tech store-bought mirror (not immersive virtual reality). Ramachandran describes the mirror therapy setup as follows: “A mirror is placed vertically on the table, so that the mirror reflection of the patient’s intact hand is ‘superimposed’ on the felt position of the phantom.”74, p. 377 The idea of mirror therapy was to give patients the illusion of moving their phantom limb. Instead of seeing a stump with the hand missing, during mirror therapy, patients have the illusion that their hand has not been amputated, and they have the illusion of control over their missing (phantom) hand and fingers again. In other words, Ramanchandran74 used an illusion (mirror therapy) to treat an illusion (phantom limb pain). Ramachandran74 speculated that the brain was still sending signals down to the amputated limb, but the missing limb was no longer sending signals to the brain, and somehow the patient’s mental representation of their body had not adjusted to the new reality that the patient no longer had a (e.g., right) hand.
In a case series of ten patients, after a number of mirror therapy sessions, Ramachandran’s patients’ phantom limb disappeared for several of the ten patients studied.74 When the phantom limb disappeared, in many cases the phantom limb pain also disappeared.
Although Ramachandran’s74 results are intriguing as a case series, subsequent small studies exploring whether mirror therapy works have reported encouraging but somewhat mixed results.75-79 Some patients appear to benefit from mirror therapy,80 but many patients with phantom limb pain show little or no long term improvement after low tech “simple mirror” therapy. Plasticity-based approaches such as traditional mirror therapy suffer from technological limitations that hinder their effectiveness.75 Low tech mirror-based limb visualization is simple and widely available, but it can be difficult for patients to self-administer correctly, and compliance is poor because it is difficult, repetitive, and not engaging.75 Researchers are currently developing/exploring the use of high tech immersive virtual reality to create a more compelling illusion, to help treat phantom limb pain more effectively.
Immersive virtual reality embodiment therapy for phantom limb (chronic) pain.
Using head mounted VR goggles, what people see in virtual reality changes as the user moves their head to view the environment and their avatar body. This results in a first-person visual experience of the virtual limb attached to the virtual body. This is key to providing potent illusions of ownership/embodiment of the virtual depiction of the body81 (i.e., being the avatar, “the avatar body I control in virtual reality is my body”.
As reviewed by Matamala-Gomez et al., 2019,82 researchers are exploring whether embodiment can be used to help relieve pain (e.g., phantom limb pain or even other types of persistent chronic pain).
Patients wearing a VR helmet look down and see two virtual arms and two virtual hands. They are able to use their virtual body/hand to interact with objects in the virtual world. This can be used for amputees, or even for non-amputees.82
A study of home therapy using traditional low tech mirror therapy (not VR) for people with upper limb hemiparesis suggests that compliance is a major factor for improvement.83 Gamification of embodiment therapy (using immersive VR) has the potential to capture the patient’s attention and encourage active engagement with the task, increasing compliance. In the future, augmented reality may allow patients to see mixtures of virtual images while still in the real world (www.magicleap.com).
Conclusion
Immersive virtual reality technology is proving to be effective as an adjunctive non-pharmacologic analgesic for reducing acute procedural pain during wound care and physical and occupational therapy, including hand therapy. Billions of dollars84 are currently being invested into mass producing virtual reality and augmented reality products to sell to the general public (e.g., primarily for entertainment). Consumer ready immersive virtual reality and augmented reality technologies can likely be harnessed by physical and occupational therapists to help improve the medical and psychological outcome of patients undergoing hand therapy, improve patient satisfaction, and thus reduce healthcare costs. In the future, VR may increase patients’ compliance with hand therapy homework exercises, by making the hand therapy exercises less painful and more fun, during home use. In addition, VR can be used to help monitor whether, when, and how well patients are doing their hand therapy exercises, and to quantify whether adherence to treatment increases long term functionality. Additional research and development into using virtual reality as a tool for hand therapist, is recommended.
Footnotes
The authors do not have any conflicts of interest. The first author has joined the Scientific Advisory Board of BehaVR.com.
Although one author works for Johnson and Johnson and one works for GlaxoSmithKline (GSK), no products or funding from these sources were involved in the conduct of any of the studies in the current manuscript, and these are not considered competing interests.
The 2019 luxury high resolution VR custom helmet named “XTAL” with 180 degrees field of view www.VRgineers.com, is also a fraction of the price of a 2013 90 degree FOV helmet.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Hunter G. Hoffman, Virtual Reality Research Center at the Human Photonics Lab, University of Washington, Seattle.
David A. Boe, Center for Limb Loss and Mobility, Veterans Hospital, Seattle, WA.
Eric Rombokas, Center for Limb Loss and Mobility, Veterans Hospital, Seattle, WA..
Christelle Khadra, University of Montreal, Montreal, QC, Canada; Research Center, Centre Hospitalier Universitaire (CHU) Sainte-Justine, Montreal, QC, Canada..
Sylvie LeMay, University of Montreal, Montreal, QC, Canada; Research Center, Centre Hospitalier Universitaire (CHU) Sainte-Justine, Montreal, QC, Canada..
Walter J. Meyer, III, Department of Psychiatry and Behavioral Sciences, University of Texas Medical Branch, Galveston, TX, United States, Department of Psychology, Shriners Hospitals for Children—Galveston, Galveston, TX, United States..
Sam Patterson, VR Research Center at HPL, University of Washington, Seattle..
Ann Ballesteros, Emerging Science Innovation & Digital Innovation, GlaxoSmithKline (GSK).
Stephen W. Pitt, Johnson and Johnson JLABS @ US North East (NYC, Boston, & Philadelphia)
REFERENCES
- 1.Melzack R, The tragedy of needless pain. Scientific American, 1990;262:27–33. [DOI] [PubMed] [Google Scholar]
- 2.Goldberg DS, McGee SJ. Pain as a global public health priority. BMC Public Health, 2011;11:770. doi: 10.1186/1471-2458-11-770. PMID: 21978149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clark S, Horton R. Low back pain: a major global challenge. Lancet., 2018;391:2302. doi: 10.1016/S0140-6736(18)30725-6. Epub 2018 Mar 21.PMID: 29573869 [DOI] [PubMed] [Google Scholar]
- 4.Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Peña R, Beck W, Patterson DR, Meyer III WJ. Immersive virtual reality as an adjunctive non-opioid analgesic for predominantly Latin American children with large severe burn wounds during burn wound cleaning in the Intensive Care Unit: A pilot study. Front. Hum. Neurosci, 2019;13:1–11. DOI: 10.3389/fnhum.2019.00262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pavlova M, Kopala-Sibley DC, Nania C, Mychasiuk R, Christensen J, McPeak A, Tomfohr-Madsen L, Katz J, Palermo TM, Noel M. Sleep disturbance underlies the co-occurrence of trauma and pediatric chronic pain: a longitudinal examination. Pain, 2020;. doi: 10.1097/j.pain.0000000000001769. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Noel M, Wilson AC, Holley AL, Durkin L, Patton M, Palermo TM. Posttraumatic stress disorder symptoms in youth with vs without chronic pain. Pain. 2016. October;157(10):2277–84. doi: 10.1097/j.pain.0000000000000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keefe FJ, Huling DA, Coggins MJ, Keefe DF, Zachary Rosenthal M et al. Virtual reality for persistent pain: A new direction for behavioral pain management. Pain. 2012;153:2163–6. doi: 10.1016/j.pain.2012.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keefe FJ, Main CJ, George SZ. Advancing psychologically informed practice for patients with persistent musculoskeletal pain: Promise, pitfalls, and solutions. Phys Ther. 2018;98:398–407. doi: 10.1093/ptj/pzy024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wiech K, Tracey I. The influence of negative emotions on pain: behavioral effects and neural mechanisms. Neuroimage. 2009;47:987–94. doi: 10.1016/j.neuroimage.2009.05.059. [DOI] [PubMed] [Google Scholar]
- 10.Fields HL. How expectations influence pain. Pain. 2018. September;159 Suppl 1:S3–S10. doi: 10.1097/j.pain.0000000000001272. [DOI] [PubMed] [Google Scholar]
- 11.Noel M, Palermo TM, Chambers CT, Taddio A, Hermann C. Remembering the pain of childhood: applying a developmental perspective to the study of pain memories. Pain. 2015;156:31–4. doi: 10.1016/j.pain.0000000000000001. Review [DOI] [PubMed] [Google Scholar]
- 12.Noel M, Rabbitts JA, Tai GG, Palermo TM. Remembering pain after surgery: a longitudinal examination of the role of pain catastrophizing in children's and parents’ recall. Pain. 2015;156:800–8. doi: 10.1097/j.pain.0000000000000102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Noel M, Chambers CT, McGrath PJ, Klein RM, Stewart SH. The influence of children's pain memories on subsequent pain experience. Pain. 2012;153:1563–72. doi: 10.1016/j.pain.2012.02.020. Epub 2012 May 3. [DOI] [PubMed] [Google Scholar]
- 14.Heathcote LC, Lau JY, Mueller SC, Eccleston C, Fox E, Bosmans M, Vervoort T. Child attention to pain and pain tolerance are dependent upon anxiety and attention control: An eye-tracking study. Eur J Pain. 2017;21:250–263. doi: 10.1002/ejp.920. Epub 2016 Jul 27. PMID:27463940 [DOI] [PubMed] [Google Scholar]
- 15.Hemington KS, Cheng JC, Bosma RL, Rogachov A, Kim JA, Davis KD. Beyond Negative Pain-Related Psychological Factors: Resilience Is Related to Lower Pain Affect in Healthy Adults. J Pain. 2017;18:1117–1128. doi: 10.1016/j.jpain.2017.04.009. Epub 2017 May 12. PMID: 28506777 [DOI] [PubMed] [Google Scholar]
- 16.Rohilla L, Agnihotri M, Trehan SK, Sharma RK, and Ghai S. (2018). Effect of music therapy on pain perception, anxiety, and opioid use during dressing change among patients with burns in India: A quasiexperimental, cross-over pilot study. Ostomy Wound Manage. 2018; 64, 40–46. doi: 10.25270/owm.2018.10.4046 [DOI] [PubMed] [Google Scholar]
- 17.Fratianne RB, Prensner JD, Hutson MJ, Super DM, Yowler CJ, and Sandley JM. The effect of music-based imagery and musical alternate engagement on the burn debridement process. J. Burn Care Rehabil. 2001:22, 47–53. doi: 10.1097/00004630-200101000-00010 [DOI] [PubMed] [Google Scholar]
- 18.Bellieni CV, Cioncoloni D, Mazzanti S, Bianchi ME, Morrone I, Becattelli R, Perrone S, Buonocore G. Music provided through a portable media player (iPod) blunts pain during physical therapy. Pain Manag Nurs. 2013;14:e151–e155. doi: 10.1016/j.pmn.2011.09.003. Epub 2011 Nov 16. PMID: 24315267 [DOI] [PubMed] [Google Scholar]
- 19.van der Heijden MJE, Jeekel J, Rode H, Cox S, van Rosmalen J, Hunink MGM., et al. (2018). Can live music therapy reduce distress and pain in children with burns after wound care procedures? a randomized controlled trial. Burns. 2018;44:823–833. doi: 10.1016/j.burns.2017.12.013 [DOI] [PubMed] [Google Scholar]
- 20.Slater M, Usoh M, Steed A. Depth of presence in immersive virtual environments. Presence Teleoper Virtual Environ 1994; 3:130–144. [Google Scholar]
- 21.Hoffman HG. Virtual Reality: A New Tool for Interdisciplinary Psychology Research. CyberPsychology & Behavior. 1998;1:195–200. [Google Scholar]
- 22.Hoffman HG, Doctor JN, Patterson DR, Carrougher GJ, Furness TA, 3rd: Use of virtual reality as an adjunctive treatment of adolescent burn pain during wound care: A case report. Pain. 2000;85:305–309. [DOI] [PubMed] [Google Scholar]
- 23.Flores H.G. Hoffman, Russell W, Holmes CL, Roberts IK, Polak ME, Serghiou MA, Patterson DR, and Meyer WJ III Virtual Reality Pain Distraction Treatment of Hispanic and Caucasian Children with Large Severe Burns CyberPsychology & Behavior. 2009;12,:92. doi: 10.1089/cpb.2008.9999.abs [DOI] [Google Scholar]
- 24.Birnie KA, Chambers CT, Spellman CM. Mechanisms of distraction in acute pain perception and modulation. Pain. 2017;158:1012–1013. doi: 10.1097/j.pain.0000000000000913. [DOI] [PubMed] [Google Scholar]
- 25.Dahlquist LM, McKenna KD, Jones KK, Dillinger L, Weiss KE, Ackerman CS. Active and passive distraction using a head-mounted display helmet: effects on cold pressor pain in children. Health Psychol. 2007;26:794–801. [DOI] [PubMed] [Google Scholar]
- 26.Gold JI, Kim SH, Kant AJ, Joseph MH, and Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during IV placement. CyberPsychol. Behav 2006;9:207–212. doi: 10.1089/cpb.2006.9.207 [DOI] [PubMed] [Google Scholar]
- 27.Gold JI, Belmont KA, and Thomas DA. The neurobiology of virtual reality pain attenuation. CyberPsychol. Behav 2007;10, 536–544. doi: 10.1089/cpb.2007.9993 [DOI] [PubMed] [Google Scholar]
- 28.Gold JI, and Mahrer NE. Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J. Pediatr. Psychol 2017;43:266–275. doi: 10.1093/jpepsy/jsx129. [DOI] [PubMed] [Google Scholar]
- 29.Zeroth JA, Dahlquist LM, Foxen-Craft EC. The effects of auditory background noise and virtual reality technology on video game distraction analgesia. Scand J Pain. 2019;28;19:207–217. doi: 10.1515/sjpain-2018-0123 [DOI] [PubMed] [Google Scholar]
- 30.Eccleston C Role of psychology in pain management. Br. J. Anaesth 2001:87, 144–152. doi: 10.1093/bja/87.1.144 [DOI] [PubMed] [Google Scholar]
- 31.Eccleston C, and Crombez G. Pain demands attention: a cognitive Affective model of the interruptive function of pain. Psychol. Bull 1999;125, 356–366. doi: 10.1037//0033-2909.125.3.356 [DOI] [PubMed] [Google Scholar]
- 32.Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport. 2004;15:1245–1248. [DOI] [PubMed] [Google Scholar]
- 33.Hoffman HG, Richards TL, Van Oostrom T, Coda BA, Jensen MP, Blough DK, et al. The analgesic effects of opioids and immersive virtual reality distraction: evidence from subjective and functional brain imaging assessments. Anesth Analg. 2007; 105:1776–1783. [DOI] [PubMed] [Google Scholar]
- 34.Carrougher GJ, Hoffman HG, Nakamura D, Lezotte D, Soltani M, Leahy L, Engrav LH, Patterson DR. The effect of virtual reality on pain and range of motion in adults with burn injuries. J Burn Care Res. 2009;30:785–91. doi: 10.1097/BCR.0b013e3181b485d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, Soltani M et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011;37:61–8. doi: 10.1016/j.burns.2010.07.007. Epub 2010 Aug 7. PMID:20692769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Soltani M, Drever SA, Hoffman HG, Sharar SR, Wiechman SA, Jensen MP, Patterson DR. Virtual reality analgesia for burn joint flexibility: A randomized controlled trial. Rehabil Psychol. 2018;63:487–494. doi: 10.1037/rep0000239. Epub 2018 Oct 4. PMID:30284865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peek K, Sanson-Fisher R, Mackenzie L, Carey M. Interventions to aid patient adherence to physiotherapist prescribed self-management strategies: a systematic review. Physiotherapy. 2016;102:127–35. doi: 10.1016/j.physio.2015.10.003. Epub 2015 Oct 22. [DOI] [PubMed] [Google Scholar]
- 38.Pisters MF, Veenhof C, de Bakker DH, Schellevis FG, Dekker J. Behavioural graded activity results in better exercise adherence and more physical activity than usual care in people with osteoarthritis. J Physiother. 2010;56:41–7. [DOI] [PubMed] [Google Scholar]
- 39.Beinart NA, Goodchild CE, Weinman JA, Ayis S, Godfrey EL. Individual and intervention-related factors associated with adherence to home exercise in chronic low back pain: a systematic review. Spine J. 2013;13:1940–50. [DOI] [PubMed] [Google Scholar]
- 40.Hoffman HG: Virtual Reality Therapy. Scientific American. 2004, 291:58–65. [DOI] [PubMed] [Google Scholar]
- 41.Maani C, Hoffman HG, DeSocio PA, Morrow M, Galin C, Magula J, Maiers A and Gaylord K. Pain control during wound care for combat-related burn injuries using custom articulated arm mounted virtual reality goggles. Journal of CyberTherapy and Rehabilitation, 2008;1:193–198. [Google Scholar]
- 42.Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K, McGhee LL, et al. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J Trauma. 2011b;71(1 Suppl):S125–30. doi: 10.1097/TA.0b013e31822192e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Maani CV, Hoffman HG, Fowler M, Maiers AJ, Gaylord KM, Desocio PA. Combining ketamine and virtual reality pain control during severe burn wound care: one military and one civilian patient. Pain Med. 2011a;12:673–8. doi: 10.1111/j.1526-4637.2011.01091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hoffman HG, Meyer WJ 3rd, Ramirez M, Roberts L, Seibel EJ, Atzori B, Sharar SR, Patterson DR. Feasibility of articulated arm mounted Oculus Rift Virtual Reality goggles for adjunctive pain control during occupational therapy in pediatric burn patients. Cyberpsychol Behav Soc Netw. 2014. June;17(6):397–401. doi: 10.1089/cyber.2014.0058. PMID: 24892204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Khadra C, Ballard A, Déry J, Paquin D, Fortin JS, Perreault I, Labbe DR, Hoffman HG, Bouchard S, LeMay S. Projector-based virtual reality dome environment for procedural pain and anxiety in young children with bum injuries: a pilot study. J Pain Res. 2018. February 14;11:343–353. doi: 10.2147/JPR.S151084. eCollection 2018. PMID: 29491717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Atzori B, Lauro Grotto R, Giugni A, Calabrò M, Alhalabi W, Hoffman HG. Virtual Reality Analgesia for Pediatric Dental Patients. Front. Psychol 2018a;9:2265. doi: 10.3389/fpsyg.2018.02265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Atzori B, Hoffman HG, Vagnoli L, Patterson DR, Alhalabi W, Messeri A, Lauro Grotto R. Virtual Reality Analgesia During Venipuncture in Pediatric Patients With Onco-Hematological Diseases. Front Psychol. 2018b;20;9:2508. doi: 10.3389/fpsyg.2018.02508. eCollection 2018. PMID: 30618938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Indovina P, Barone D, Gallo L, Chirico A, De Pietro G, Antonio G Virtual Reality as a Distraction Intervention to Relieve Pain and Distress During Medical Procedures: A Comprehensive Literature Review. Clin J Pain. 2018;34:858–877. 10.1097/AJP.0000000000000599. [DOI] [PubMed] [Google Scholar]
- 49.McSherry T, Atterbury M, Gartner S, Helmold E, Searles DM, Schulman C. Randomized, Crossover Study of Immersive Virtual Reality to Decrease Opioid Use During Painful Wound Care Procedures in Adults. J Burn Care Res. 2018; 20;39:278–285. doi: 10.1097/BCR.0000000000000589. [DOI] [PubMed] [Google Scholar]
- 50.Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain. 2014;30:1089–98. doi: 10.2196/medinform.7271. Review. [DOI] [PubMed] [Google Scholar]
- 51.Hoxhallari E, Behr IJ, Bradshaw JS, Morkos MS, Haan PS, Schaefer MC, Clarkson JHW. Virtual Reality Improves the Patient Experience during Wide-Awake Local Anesthesia No Tourniquet Hand Surgery: A Single-Blind, Randomized, Prospective Study. Plast Reconstr Surg. 2019;144:408–414. doi: 10.1097/PRS.0000000000005831 [DOI] [PubMed] [Google Scholar]
- 52.Hoffman HG, Seibel EJ, Richards TL, Furness TA, Patterson DR, Sharar SR. Virtual reality helmet display quality influences the magnitude of virtual reality analgesia. J Pain. 2006;7:843–850. [DOI] [PubMed] [Google Scholar]
- 53.Al-Ghamdi NA, Meyer WJ 3rd, Atzori B, Alhalabi W, Seibel CC, Ullman D, Hoffman HG. Virtual Reality Analgesia With Interactive Eye Tracking During Brief Thermal Pain Stimuli: A Randomized Controlled Trial (Crossover Design). Front Hum Neurosci. 2020. January 23;13:467, 1–11. doi: 10.3389/fnhum.2019.00467. eCollection 2019. PMID:32038200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Shefer-Eini D, Ratzon NZ, Rizzo AA, Yeh SC, Lange B, Yaffe B et al. Camera-tracking gaming control device for evaluation of active wrist flexion and extension. J Hand Ther. 2017;30:89–96. doi: 10.1016/j.jht.2016.07.002. Epub 2016 Nov 26. [DOI] [PubMed] [Google Scholar]
- 55.Tarakci E, Arman N, Tarakci D, Kasapcopur O. Leap Motion Controller-based training for upper extremity rehabilitation in children and adolescents with physical disabilities: A randomized controlled trial. J Hand Ther. 2019;1–8. doi: 10.1016/j.jht.2019.03.012. [Epub ahead of print] PMID:31010703 [DOI] [PubMed] [Google Scholar]
- 56.Garcia-Palacios A, Herrero R, Vizcaíno Y, Belmonte MA, Castilla D, Molinari G, Baños RM, Botella C. Integrating virtual reality with activity management for the treatment of fibromyalgia: acceptability and preliminary efficacy. Clin J Pain. 2015;31:564–72. doi: 10.1097/AJP.0000000000000196. PMID: 25551475 [DOI] [PubMed] [Google Scholar]
- 57.Carlin AS, Hoffman HG & Weghorst S. Virtual reality and tactile augmentation in the treatment of spider phobia: A case study. Behav Res Ther. 1997;35:153–158. [DOI] [PubMed] [Google Scholar]
- 58.Garcia-Palacios A, Hoffman H G, Carlin C, Furness TA III, Botella-Arbona C. Virtual reality in the treatment of spider phobia: A controlled study. Behaviour Research and Therapy. 2002;40:9;983–993. [DOI] [PubMed] [Google Scholar]
- 59.Hoffman HG, Garcia-Palacios A, Carlin A, Furness TA III & Botella-Arbona C Interfaces That Heal: Coupling Real and Virtual Objects to Treat Spider Phobia, International Journal of Human–Computer Interaction. 2003;16:2, 283–300. [Google Scholar]
- 60.Difede J, & Hoffman HG. Virtual reality exposure therapy for World Trade Center Post Traumatic Stress Disorder: A case report. Cyberpsychol Behav. 2002;5:529–536. [DOI] [PubMed] [Google Scholar]
- 61.Difede J, Cukor J, Wyka K, Olden M, Hoffman H, Lee FS, Altemus M.D-Cycloserine Augmentation of Exposure Therapy for Post-Traumatic Stress Disorder: A Pilot Randomized Clinical Trial. Neuropsychopharmacology. 2014;39:1052–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Freedman SA, Hoffman HG, Garcia-Palacios A, Tamar Weiss PL, Avitzour S, Josman N. Prolonged exposure and virtual reality-enhanced imaginal exposure for PTSD following a terrorist bulldozer attack: a case study. Cyberpsychol Behav Soc Netw. 2010;13:95–101. PMID: 20528299 [DOI] [PubMed] [Google Scholar]
- 63.Navarro-Haro MV, Hoffman HG, Garcia-Palacios A, Sampaio M, Alhalabi W, Hall K, Linehan M. The Use of Virtual Reality to Facilitate Mindfulness Skills Training in Dialectical Behavioral Therapy for Borderline Personality Disorder: A Case Study. Front. Psychol 2016;7:1–9 10.3389/fpsyg.2016.01573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Navarro-Haro MV, Modrego-Alarcón M, Hoffman HG, et al. Evaluation of a Mindfulness-Based Intervention With and Without Virtual Reality Dialectical Behavior Therapy® Mindfulness Skills Training for the Treatment of Generalized Anxiety Disorder in Primary Care: A Pilot Study. Front Psychol. 2019;28;10:55. doi: 10.3389/fpsyg.2019.00055. eCollection 2019. PMID: 30745888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gomez J, Hoffman HG, Bistricky SL, Gonzalez M, Rosenberg L, Sampaio M, Garcia-Palacios A, Navarro-Haro MV, Alhalabi W, Rosenberg M, Meyer WJ 3rd, Linehan MM. The Use of Virtual Reality Facilitates Dialectical Behavior Therapy® "Observing Sounds and Visuals" Mindfulness Skills Training Exercises for a Latino Patient with Severe Burns: A Case Study. Front Psychol. 2017. 8:1611, p 1–8. doi: 10.3389/fpsyg.2017.01611. eCollection 2017. PMID 28993747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Flores A, Linehan MM, Todd SR, Hoffman HG. The Use of Virtual Reality to Facilitate Mindfulness Skills Training in Dialectical Behavioral Therapy for Spinal Cord Injury: A Case Study. Front Psychol. 2018;9:531, 1–7. doi: 10.3389/fpsyg.2018.00531. eCollection 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Louw A, Vogsland R, Marth L, Marshall P, Cox T, Landers M. Interdisciplinary Pain Neuroscience Continuing Education in the Veterans Affairs: Live Training and Live-Stream With 1-Year Follow-up. Clin J Pain. 2019;35:901–907. doi: 10.1097/AJP.0000000000000756. PMID:31433321 [DOI] [PubMed] [Google Scholar]
- 68.Nkhata LA, Brink Y, Ernstzen D, Louw QA. A systematic review on self-management education campaigns for back pain. S Afr J Physiother. 2019;13;75:1314. doi: 10.4102/sajp.v75i1.1314. eCollection 2019. Review. PMID: 31535051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Louw A, Diener I, Landers MR, Zimney K, Puentedura EJ. Three-year follow-up of a randomized controlled trial comparing preoperative neuroscience education for patients undergoing surgery for lumbar radiculopathy. J Spine Surg. 2016;2:289–298. doi: 10.21037/jss.2016.12.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Louw A, Louw C, Flynn T. Case Report: Pain Neuroscience Education using Virtual Reality. Pain and Rehab. 2019;2019:pp. 4–7. [Google Scholar]
- 71.Kikkert S, Mezue M, O'Shea J, Henderson Slater D, Johansen-Berg H, Tracey I, Makin TR. Neural basis of induced phantom limb pain relief. Ann Neurol. 2019;85:59–73. doi: 10.1002/ana.25371. Epub 2019 Jan 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Flor H, Diers M, Andoh J. The neural basis of phantom limb pain. Trends Cogn Sci. 2013;17:307–8. doi: 10.1016/j.tics.2013.04.007. Epub 2013 Apr 19. PMID:23608362 [DOI] [PubMed] [Google Scholar]
- 73.Kikkert S, Johansen-Berg H, Tracey I, Makin TR. Reaffirming the link between chronic phantom limb pain and maintained missing hand representation. Cortex. 2018;106:174–184. doi: 10.1016/j.cortex.2018.05.013. Epub 2018 May 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ramachandran VS, Rogers-Ramachandran D. Synaesthesia in phantom limbs induced with mirrors. Proc Biol Sci. 1996;22;263:377–86. PMID: 8637922 [DOI] [PubMed] [Google Scholar]
- 75.Moseley GL, Gallace A, Spence C. Is mirror therapy all it is cracked up to be? Current evidence and future directions. Pain. 2008;15;138:7–10. doi: 10.1016/j.pain.2008.06.026. Epub. [DOI] [PubMed] [Google Scholar]
- 76.Moseley GL, Flor H. Targeting cortical representations in the treatment of chronic pain: a review. Neurorehabil Neural Repair. 2012;26:646–52. doi: 10.1177/1545968311433209. Epub 2012 Feb 13. Review. PMID: 22331213 [DOI] [PubMed] [Google Scholar]
- 77.Thøgersen M, Hansen J, Arendt-Nielsen L, Flor H, Petrini L. Removing own-limb visual input using mixed reality (MR) produces a "telescoping" illusion in healthy individuals. Behav Brain Res. 2018;16;347:263–271. doi: 10.1016/j.bbr.2018.03.024. Epub 2018 Mar 15. [DOI] [PubMed] [Google Scholar]
- 78.Seidel S, Kasprian G, Sycha T, Auff E. Mirror therapy for phantom limb pain--a systematic review. Wien Klin Wochenschr. 2009;121:440–4. doi: 10.1007/s00508-009-1212-9. Review. German. PMID: 19657605 [DOI] [PubMed] [Google Scholar]
- 79.Barbin J, Seetha V, Casillas JM, Paysant J, Pérennou D. The effects of mirror therapy on pain and motor control of phantom limb in amputees: A systematic review. Ann Phys Rehabil Med. 2016;59:270–5. doi: 10.1016/j.rehab.2016.04.001. Epub 2016 May 30. [DOI] [PubMed] [Google Scholar]
- 80.Chan BL, Witt R, Charrow AP, Magee A, Howard R, Pasquina PF, Heilman KM, Tsao JW. Mirror therapy for phantom limb pain. N Engl J Med. 2007. November 22;357:2206–7. [DOI] [PubMed] [Google Scholar]
- 81.Serino A, Alsmith A, Costantini M, Mandrigin A, Tajadura-Jimenez A, Lopez C. Bodily ownership and self-location: components of bodily self-consciousness. Conscious Cogn. 2013;22:1239–52. doi: 10.1016/j.concog.2013.08.013. Epub 2013 Sep 13. [DOI] [PubMed] [Google Scholar]
- 82.Matamala-Gomez M, Diaz Gonzalez AM, Slater M, Sanchez-Vives MV. Decreasing Pain Ratings in Chronic Arm Pain Through Changing a Virtual Body: Different Strategies for Different Pain Types. J Pain. 2019;20:685–697. doi: 10.1016/j.jpain.2018.12.001. Epub 2018 Dec 16. PMID: 30562584 [DOI] [PubMed] [Google Scholar]
- 83.Kuys SS, Edwards T, and Morris NR, Effects of adherence of mirror therapy in people with chronic upper limb hemiparesis: A preliminary study. ISRN Rehabil, 2012. [Google Scholar]
- 84. https://www.forbes.com/sites/billfrist/2018/07/10/virtual-reality-isnt-just-for-gamers-anymore-it-will-change-your-health/#6d4cb4364c0a.






