ABSTRACT
Snake-bite is a well-known but fairly ignored medical problem in India. Lack of precise first aid knowledge for snake-bite is a substantial reason for its severe fatality in human beings. The present study is comprised of a pilot survey that assesses and evaluates the knowledge of people of different occupations (teachers, students, farmers, medical residents, and miscellaneous) about snakes and snake-bite management. The pilot survey was conducted through a well-structured open-ended questionnaire about experiences with snakes and snake-bites and first aid measures for accidental snake-bites. Proper knowledge of snakes and snake-bite management was either diminutive or absent in the majority of the subjects, especially amongst teachers. Even the medical professionals were not well acquainted with knowledge about snakes and snake-bite management. Only 13% knew about ‘big four’, 18% knew ‘dry bite’, and 21% of subjects knew about anti-snake venom (ASV) used in India. 39% of subjects knew about the whereabouts of traditional healer. Only 12% of subjects, mostly medical residents, knew of any bedside test for diagnosis of snake-bite, and 11% of respondents also knew of LD50 of Indian cobra. A well-timed first aid treatment is always decisive in the management of life-threatening snake-bite cases but the present survey has found that most of the study groups had inadequate and little misleading fundamental knowledge comprising regional snakes, first aid measures for accidental snake-bite, and welfare schemes for snake-bite victims. Therefore, the present study proposes to conduct more such appraisals and strengthening of education curricula on snake-bite that would surely inculcate an adequate level of primary skill in ignorant societies.
Key Words: snake-bite, first aid, anti-snake venom, dry bite, big four
INTRODUCTION
Snakes are distributed in several parts of the world. The real burden of snake-bite is mostly reported from middle and low-income tropical countries in the form of a huge number of mortalities and morbidities, particularly in agriculture occupants.1-3 India contributes maximum to the snake envenomation caused morbidity and mortality with approx 46,000 deaths and even more morbidities every year.4,5 Epidemiological profile of snake-bite in Haryana suggests annually around thousand snake-bites admissions in hospitals.6 Going by the burden of snake envenomation, there is a need to assess the public about general knowledge about snakes, preventive, and first aid measures for accidental snake-bites which might decrease the incidences of fatal snake envenomation. The role of appropriate first aid knowledge in public and medical professionals definitely matters a lot. Even a minor mistake at the early treatment stage in snake-bite can prove to be detrimental in saving human life. The present study was carried out to assess the knowledge of snakes and snake-bite management in the Rohtak region of Haryana in India. Rohtak district hospitals have reported the maximum number of snake-bites in the past,6 but issues of knowledge on snakes, snake-bite, and government-sponsored welfare schemes for financial assistance of snake-bite victims have not got much attention in this region. Some studies assessing the basic knowledge about snakes and snake-bite management were conducted from different states of India7-9 and from across the world including Australia,10 Hong Kong11 and Laos.12 Few imperative reports have emphasized on integrated multifocal approach to reduce the burden of snake-bite problem by getting hold of reliable statistics of snake-bite incidences, innovative research and developing effective anti-snake venom (ASV) in low-income countries, and disseminating training and education programs for doctors and paramedics at community levels.12,13
MATERIALS AND METHODS
The present pilot survey assessed the knowledge of 100 subjects, 20 each from five different occupations of teachers (faculties from schools and university), students (postgraduate students and Ph.D. scholars), medical residents (junior/senior residents from various medical and dental departments), farmers, and miscellaneous (housewives, daily wage laborers, shopkeepers, and clerks) from Rohtak Region of Haryana. Table 1 contains details of age (median and range) and the gender of subjects from each group. The overall male to female ratio and range of age of the subjects was 3.3:1 and 50 (70–20) years, respectively. Rohtak district of Haryana, a northern state of India (Fig. 1) having a population of over one million was selected as a study site due to records of maximum reporting of snake-bite incidences in hospitals of this district.6 The selection of the subjects was made by a random sampling approach and including the first twenty subjects from each occupation group. Exclusion criteria were not extensive, but those who denied being included and those with less than twenty years of age were excluded from the current study. All the subjects were made aware in advance about the purpose of the present study; therefore, demographic details of the subjects were collected with their consent prior to answering the questionnaire. The structured questionnaire consisted of fifteen questions of general as well as specific queries on snakes. Questions covered a wide range of queries: from subject’s personal experience of snake-bite/snake encounter to descriptions of snake-bite cases seen/heard and information about local traditional snake-bite healers followed by scrupulous queries testing their awareness about first aid measures, venomous snake species of India, ‘big four’, ‘dry bite’ terminology, lethal dose (LD50) of Indian cobra, ASV used to treat snake-bite in India, diagnostic tests for snake-bites, and government welfare schemes for victims of accidental snake-bite in Haryana. All the questions were open-ended which allowed the participants to give descriptive answers. The whole questionnaire was made available in English and translated to native language Hindi (whenever required). Door to door visits were made in the month of April 2018 to complete the survey. Subjects were forbidden for using any kind of external source (book/internet/discussion) during the questionnaire.
Table 1.
Sex ratio (male and female) and age (median and range) of each subject group
| S. No. | Teachers | Students | Medical Residents | Farmers | Others | |||||
| AGE | SEX | AGE | SEX | AGE | SEX | AGE | SEX | AGE | SEX | |
| 1 | 54 | F | 23 | F | 29 | M | 38 | M | 32 | F |
| 2 | 32 | F | 25 | M | 30 | M | 45 | M | 55 | F |
| 3 | 57 | F | 28 | M | 30 | M | 32 | M | 45 | F |
| 4 | 36 | F | 30 | F | 30 | M | 36 | M | 45 | F |
| 5 | 49 | F | 23 | M | 29 | M | 46 | F | 32 | F |
| 6 | 37 | F | 30 | M | 33 | M | 36 | M | 45 | F |
| 7 | 48 | F | 28 | M | 30 | M | 70 | M | 56 | F |
| 8 | 39 | F | 28 | F | 25 | F | 50 | M | 55 | F |
| 9 | 42 | F | 21 | M | 41 | M | 54 | M | 52 | M |
| 10 | 55 | F | 21 | M | 27 | M | 45 | M | 37 | M |
| 11 | 26 | M | 23 | M | 33 | M | 36 | M | 48 | M |
| 12 | 47 | M | 20 | M | 32 | F | 38 | M | 24 | M |
| 13 | 38 | M | 25 | F | 30 | M | 29 | M | 52 | M |
| 14 | 36 | M | 27 | F | 30 | M | 40 | M | 28 | M |
| 15 | 37 | M | 28 | F | 26 | M | 58 | M | 34 | M |
| 16 | 40 | M | 28 | M | 32 | M | 27 | M | 40 | M |
| 17 | 60 | M | 23 | M | 29 | M | 30 | M | 36 | M |
| 18 | 31 | M | 23 | M | 26 | M | 28 | M | 32 | M |
| 19 | 37 | M | 27 | F | 29 | M | 28 | M | 43 | M |
| 20 | 52 | M | 22 | F | 30 | F | 30 | M | 35 | M |
|
Sex Ratio
(M:F) |
-- | 1:1 | - | 1.5:1 | -- | 5.6:1 | -- | 19:1 | -- | 1.5:1 |
|
Median age
(Years) |
39.5 | -- | 25 | -- | 30 | -- | 37 | -- | 41.5 | -- |
|
Age Range
(Years) |
34 | -- | 10 | -- | 16 | -- | 43 | -- | 32 | -- |
Fig. 1.
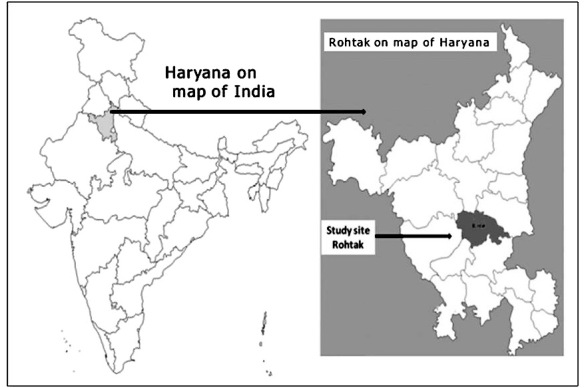
Map of India highlighting the study region.
RESULTS AND DISCUSSION
Responses to the queries of the survey by participants of different groups are presented in Table 2–5 and in Fig. 2–3. The findings of the present study construe the problem of snake-bite in Haryana. It is evident from Table 2 that a total of 5 subjects including 1 farmer from the rural area and 4 miscellaneous group subjects declared to be bitten by a snake at least once in life. All of these bites took place during day time while working on the farm or houses. All these subjects got treatment in hospitals. One of these victims still had on his face severe surgical sequelae. A total of 181 cases of snake-bites were notified in the survey; 150 cases were witnessed by 43% of respondents and 31 cases were heard/hearsay by 26% respondents. Medical residents witnessed 78% of these cases during medical treatment in hospitals. Twenty four (24) fatal cases of snake-bite particularly from rural areas were notified. Morbidities in form of permanent scarring at the bite site, loss of vision, loss of fingers after surgical intervention were notified in 17 victims. An earlier study on snake-bite epidemiology of this region also reported a similar magnitude of snake-bite in this study region.6 This must be kept in mind that around 80% geographical area of the study region (Rohtak) is under cultivation. About 65% of the population live in rural areas; the majority of these are farmers. Sighting of venomous snakes is quite common in the fields, and even more often during monsoon season. Generally, the habit of walking barefoot at night without torchlight or lamp and sleeping on the floor by the villagers adds to the quantum of this problem. Observations revealed 39% of subjects including 60% of the farmers accepted acquaintance with at least one traditional healer (Table 2). Total of thirteen villages were notified in neighbourhood areas where at least one traditional healer was residing and treating snake-bite victims. The rationale was to know the frequency and interest of the subjects in traditional remedies for snake-bites. Earlier studies have reported of many unhygienic measures such as incision, and sucking of the wound to cease the flow of venom in the body by such traditional healers.14
Table 2.
Responses of survey participants on personal experience of snake-bites and general queries regarding snakes
| Queries from questionnaire | Subject Groups | |||||
| Teachers | Students | Medical Residents | Farmers | Others | % | |
| 1. Self encountered cases of snake-bite | Nil | Nil | Nil | 01 | 04 | 5% |
| 2. Seen and heard cases of snake-bite | 07 | 16 | 118 | 14 | 27 | N.A. |
| 3. Whereabouts of local traditional healer/quack for treatment of snake-bite | 03 | 09 | 01 | 15 | 11 | 39% |
| 4. Number of venomous snake of India | Nil | Nil | 05 | 04 | 03 | 12% |
| 5. Knowledge about ‘Big four’ | Nil | 03 | 10 | Nil | Nil | 13% |
Table 3.
Participants’ responses for first aid measures for snake-bites and sources of knowledge (subjects were allowed to opt for more than one option)
| Subject Group |
Positive claim for
rudimentary and expert first aid knowledge |
Book/School |
TV
(media) |
Internet
(digital) |
Family/Friend |
Hospital
Doctor |
| Teachers | 13 | 01 | 08 | 01 | 08 | 02 |
| Students | 19 | 08 | 03 | 04 | 08 | 02 |
| Medical Residents | 20 | 11 | 05 | 07 | 04 | 14 |
| Farmers | 20 | 01 | Nil | Nil | 19 | Nil |
| Others | 17 | 04 | 02 | 02 | 13 | 01 |
Table 4.
Most preferred methods of first aid for snake-bite by participants of survey
| Subject Group | Assurance & ABC | Tourniquet |
Bandaging/
Immobilization |
Incision |
Venom sucking
with mouth |
Ointments/
Herbs/stones |
Icing/
washing |
| Teachers | Nil | 06 | 03 | Nil | 02 | 01 | 01 |
| Students | Nil | 12 | 02 | 01 | 04 | Nil | Nil |
| Medical residents | 06 | 11 | 03 | Nil | Nil | Nil | Nil |
| Farmers | Nil | 06 | 12 | Nil | Nil | 02 | Nil |
| Miscellaneous | Nil | 14 | 03 | Nil | Nil | Nil | Nil |
Table 5.
Numbers of positive responses received for technical queries related to snakes and snake-bites
| Queries from questionnaire | Subject Groups | |||||
| Teachers | Students | Medical Residents | Farmers | Miscellaneous | % | |
| 1. Knowledge of ‘Dry bite’ | 01 | 04 | 10 | 01 | 02 | 18% |
| 2. Knowledge of LD50 of Indian cobra | 02 | 03 | 05 | 01 | Nil | 11% |
| 3. Knowledge of ASV used in India | 02 | 03 | 15 | 01 | Nil | 21% |
| 4. Knowledge of bedside test for snake-bite diagnosis | Nil | Nil | 05 | 04 | 03 | 12% |
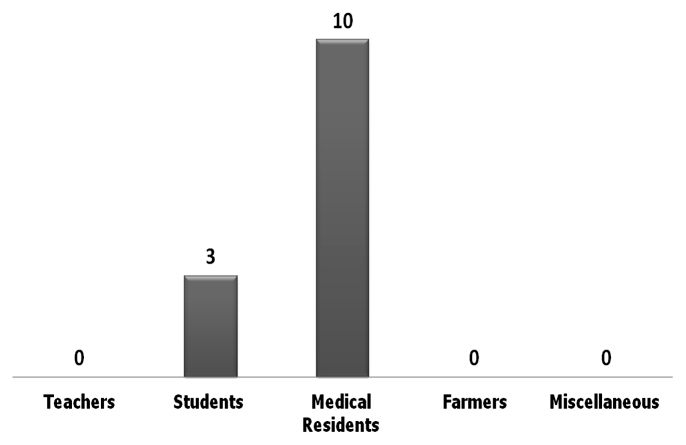
Fig. 2.
Survey participants claims for having knowledge of term ‘big four’
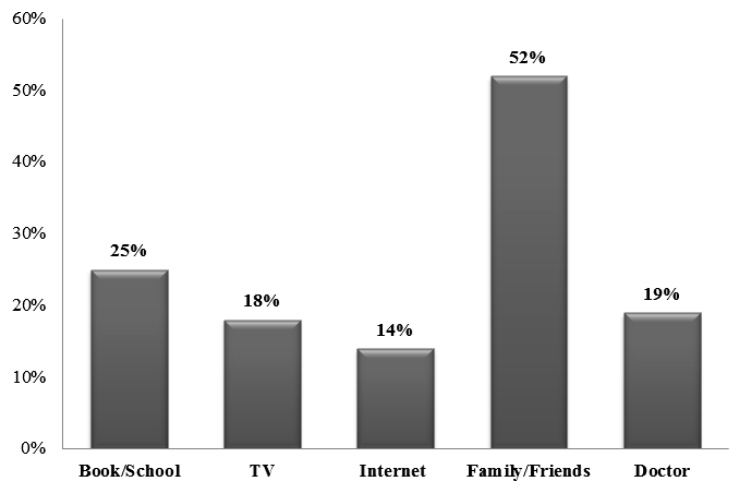
Fig. 3.
Sources of first aid measures as per survey participants
India is abode to several venomous snakes, but ‘big four’ are the most significant medically relevant; therefore, the survey enquired the knowledge about ‘big four’ jargon. Table 2 also reveals that only 13% of participants, mainly medical residents, were familiar with ‘big four’ term and associated snakes. This study has noticed unawareness of the ‘big four’ term among the majority of subjects. Lack of knowledge about ‘big four’ in 100% of the teachers and farmers is distressing (Fig. 2). The ‘big four’; Common Cobra (Naja naja), Russell’s Viper (Daboia russelii), Common Krait (Bungarus caeruleus), and Saw-scaled Viper (Echic carinatus) are called so because these four species contribute maximum to the fatalities caused by envenomation in India. Lack of interest and ignorance is the reasons behind unawareness about this slang.
It could be discerned from Table 2 that only 13% of subjects particularly from medical and agriculture professionals reached nearest to the true figures (50 to 60 species) of venomous species found in India. About 279 species belonging to 28 different families of snakes are found quite commonly across India, 52 to 60 venomous species particularly from Elapidae and Viperidae families are found in India.15,16 But 75% of subjects of the present study were familiar with only one snake, cobra. The familiarity of subjects with Indian cobra is traditional, because of its symbolic association Hindu folklore. Although Indian cobra (Naja naja) is a commonly found snake across India four other species of cobras, eight species of kraits and one subspecies of saw-scaled viper and 20 species of pit viper are also found in India.17-20 Confusion in the identification and differentiation of Common Cobra with Assamese mountain (mock cobra) and Pseudoxenodon macrops (Big-eyed mountain keelback) is quite common. Therefore, it is equally important to be vigilant of other venomous snake species, which can also lead to human fatalities but usually go unnoticed. The present study found that venomous snake meant ‘cobra’ (snake with hood) for most of the subjects.
Abysmal first aid knowledge on snake-bite can enhance the burden of snake-bite mortalities. Data presented in Table 3 revealed affirmations by 89% of subjects to have first aid knowledge on snake-bite. It was important and satisfying to see all the farmers, medical residents, and 95% of students claiming to have basic first aid knowledge in contrast to lack of such knowledge by 65% of educated teachers. Table 3 also illustrated the source of first aid knowledge as responded by the different subject groups. As the questions were open-ended, this allowed participants to answer more than one measure as per their preference. The survey revealed that for farmers, the source of first aid knowledge was almost exclusively family and friends, while medical residents and students have gained such knowledge from books and internet, and television remained the most common source of first aid knowledge for teachers. Overall evaluation of the survey revealed that ‘family/friends’ are most commonly (52%) sought after for information on first aid of snake-bite, while the internet still remained a source of information for only 14% of subjects. However there are great efforts made by the Indian Snake-bite Initiative program for awareness of people at large about snakes and snake-bites, but people of this region remained unaware of such initiatives (http://www.indiansnakes.org/content/india-snake-bite-initiative). Fig. 3 shows details of the percentile of various sources used to gain the first aid knowledge by the different subject groups. Lack of books as the source of first aid information by the majority of subjects also shows that curricula of schools/colleges don’t emphasize much on this grave matter, which again proves the neglected condition of snake envenomation.
The participants were further tested for their first aid knowledge for snake-bites. They were asked their method of choice from amongst various precise and redundant methods of first aid measures. These methods included psychological reassurance with airway, breath, and circulation (ABC) monitoring, use of tourniquet, bandaging/immobilization, incision, sucking out the venom with the mouth, ointments/herbs/stones, and icing/washing of the wound. Methods opted by different groups of subjects are listed in Table 4. Few participants denied having any knowledge about first aid for snake-bites. From amongst the remaining 89% participants, a tourniquet was the most suggested (49%) method, followed by bandaging/immobilization (23%) to restrict the flow of snake venom inside the body. Subjects were not familiar with the benefits of psychological reassurance along with ABC monitoring with exception to a few medical professionals. It was astonishing to note that a few participants believed in using perilous methods like incising the wound and the use of ointment/home remedies/stones for treating the snake-bite victims. For the proper treatment of snake-bite, only recommended method is RIGHT (R-Reassure the patient, I-Immobilize in the same way as a fractured limb, GH-Get to Hospital Immediately, T- Tell the Doctor of any systemic symptoms that manifest on the way of the hospital) without squandering precious time.21
Studies assessing and evaluating the knowledge of people of Haryana on snakes and snake-bite management have never been reported in the past. The present study revealed tourniquet and bandaging as highly preferred first aid methods to prevent the flow of venom inside the body but previous studies have reported local swelling and severity of local envenomation with a tourniquet and incisions of the wound in comparison to snake-bite victims receiving no such first aid treatments.22 The present study also revealed the influence of cinema on few subjects who suggested sucking of venom by mouth but a study compared the effect of suction of bitten wound, and found no significant difference in the occurrence of death or disability, compared to no such first aid.23 In addition, there is a potential threat for the person sucking out the venom of getting poisoned while performing oral suction. The use of some endemic plants and herbs as a remedy for snake-bite poisoning has scientifically been proven to provide relief,24 but the methods like use of stone to extract venom from the wound, or indigenously formulated ointments by traditional healers or quacks may play with the lives of victims. Such unproven and risky methods have been discouraged for snake-bite treatment.25 The present study also found that medical professionals had affirmative thoughts on the subject matter but educated teachers seemed bungled at number of queries regarding snake-bites. Obviously, the regular academic syllabi of school and colleges don’t cover extensive information on snake-bite problem in India.
Specific queries on the biting mechanism and its management in hospitals received a dull response from almost all participants (Table 5). Only 18% of the participants were aware of the mechanism of dry bite. Most of them were medical professionals and researchers. Only 5% of the farmers and teachers were aware of dry bite. The mechanism of the dry bite is simple to understand. It is a bite by the snake in which the fangs pierce the skin but envenoming doesn’t occur.26 The explanation for dry bites is either mechanical inefficiency of the venom apparatus due to striking at an unnatural angle or due to clothing or perhaps voluntary retention of venom by the snake for the sake of not wasting this precious arsenal on anything other than actual prey. The concept of dry bite can’t be ruled out in order to attain true knowledge of snakes and snake-bite management. A study has reported that the risk of envenomation after bites by venomous snakes varies from 25–50%.26
Knowledge of dry bite is also necessary to differentiate between a non-symptomatic venomous bite and a real non-hazardous non-venomous bite. Several reports have suggested that sometimes the crucial symptoms may not appear even in case of a bite by a venomous snake.27,28 It is always important to know the toxicity level of venom so that threat of snake-bite could be categorized but knowledge of LD50 of Indian cobra was very poor in the subjects. Only 11% of subjects knew about the approximate value of LD50 of Indian cobra. Only 5% of farmers and 10% of teachers knew about the LD50 of Indian cobra. Even medical professionals have limited knowledge about LD50 of Indian cobra, only 25% could tell the exact lethal dose (0.13 mg/kg) of Indian/spectacled cobra (Naja naja) (www.snakebitedatabase.org). Subjects from the miscellaneous group which mainly included housewives, mechanics, and vendors didn’t have knowledge on these specific queries like ‘big four’, LD50 of Indian cobra, and anti-snake venom (ASV). Around 21% of the total subjects knew about the type of ASV used in India for the treatment of venomous snake-bites. Precisely 75% of medical professionals in comparison to just 5% of farmers were aware of the ASV. Knowledge of ASV biochemistry is however crucial for only those who are involved either in the medical profession or in research, but we evaluated all subjects for their general knowledge about life-saving ASV. There is a great diversity of venomous snakes in India but polyvalent ASV is raised against the ‘big four’ snakes.29 Lack of widespread literature and point of interest may be the prime reasons behind unawareness of technical knowledge on snake biting mechanism and its management among teachers, farmers, students, and others.
This pilot survey also enquired the subjects’ awareness on government-sponsored welfare schemes which covers for snake-bites and do provide financial help to victims of accidental snake-bite. It was a huge disappointment to know the unawareness about such schemes even in the highly educated group categories. Only 12% of subjects claimed to have knowledge about such schemes and unexpectedly all educated teachers and students were not conversant about any of such schemes. Five medical residents, four farmers and three subjects from miscellaneous group claimed to have knowledge about such schemes. Only two participants could name these schemes. It was an important query regarding snake-bite as Government is considerate towards high fatalities due to accidental snake-bite amongst poor people, therefore; schemes namely ‘Rajiv Gandhi Parivar Bima Yojna’ and ‘Mukhyamantri Kishan Evam Khetihar Mazdoor Jiwan Suraksha Yojna’ have been implemented to provide financial compensation to farmers and plantation workers in cases of snake-bite associated mortality as well as morbidity.30 The reason for lack of knowledge on such welfare schemes is lack of proper advertisement of such schemes, the lack of internet savvy people, and lack of knowledge about the procedure to apply for such benefits.
India being the ‘snake-bite capital’ of the world needs this type of study for better understanding and implementation of policies. But, India alone is not suffering from a snake-bite problem. A pilot study like this could portray a picture of huge negligence towards such a gross problem. Likewise, such results should be published because South Asia is the epi-center of snake envenomation that needs more extensive studies on this aspect. This study is just a pilot study, surveying only 100 random participants that too without well-defined inclusion and exclusion criteria. So, the results might not be an exact representation of the whole population. Also, Rohtak is just one district of a comparatively smaller state of vast and diverse India, which is not too burdened with snake-bite problems, so this might be an underestimation of real problems. The categorization of participants should also have been more inclusive.
CONCLUSION
Findings of the present study depict the current scenario on lack of knowledge of the public on snakes, snake-bites, and first aid measures for snake envenomation. It also provides a complete unawareness about the Government’s welfare schemes for snake-bite victims. It is also accentuated through this study to conduct more extensive and systematic surveillance on the points unveiling snake-bite problem at root level from every part of the world, wherever notable snake-bite prevalence is reported. Such assessments would properly inculcate basic knowledge on snake-bite prevention and management in learned and laymen. It is further suggested to execute human welfare ideas at the root level by conducting educational and awareness programs at the village/town level especially for populations at higher risk rather than implementing policies on websites only.
ACKNOWLEDGEMENTS
First author acknowledges the University Grants Commission (UGC) for being recipient of fellowship. A hearty thank to all the participants of pilot survey who voluntarily and eagerly shared their knowledge on study topic.
CONFLICT OF INTEREST
Authors declare no conflict of interest.
REFERENCES
- 1.Arnold C. Vipers, mambas and taipans: the escalating health crisis over snakebites. Nature. 2016; 537(7618):26–28. [DOI] [PubMed]
- 2.Chippaux J-P. Snakebite envenomation turns again into a neglected tropical disease! J Venom Anim Toxins Incl Trop Dis. 2017;23(1):38. doi: 10.1186/s40409-017-0127-6 [DOI] [PMC free article] [PubMed]
- 3.Warrell DA. Snake bite. The Lancet. 2010;375(9708):77–88. doi: 10.1016/S0140-6736(09)61754-2 [DOI] [PubMed]
- 4.Mohapatra B, Warrell DA, Suraweera W, et al. Snakebite Mortality in India: A Nationally Representative Mortality Survey. PLoS Negl Trop Dis. 2011;5(4):e1018. doi: 10.1371/journal.pntd.0001018 [DOI] [PMC free article] [PubMed]
- 5.Snakebites under-reported in India - Nature India. https://www.natureasia.com/en/nindia/article/10.1038/nindia.2012.69. Accessed January 29, 2020.
- 6.Bhargava S, Kaur R, Singh R. Epidemiological profile of snake-bite cases from Haryana: A five year (2011–2015) retrospective study. J Forensic Leg Med. 2018;54:9–13. doi: 10.1016/j.jflm.2017.12.004 [DOI] [PubMed]
- 7.Karthick P, Varalakshimi E. Assess the knowledge on prevention and first aid measures of snake bite among farmer’s. Int J Dev Res. 2017;7(10):15975–15977.
- 8.Naskar S, Das D, Mukherjee A, Chowdhury R, Mitra M, MajumderDB. Knowledge on Snake Bite diagnosis & Management among Internees in a Government Medical College of Kolkata. J Dent Med Sci. 2015;14(11):52–55. doi: 10.9790/0853-141135255 [DOI]
- 9.Pandve HT, Makan A, Kulkarni TA. Assessment of Awareness Regarding Snakebites and its Related Issues among Rural Communities. SF J Pub Health. 2017;1(1): 1000002.
- 10.Sutherland SK, Coulter AR, Harris RD. Rationalisation of First-Aid Measures for Elapid Snakebite. Wilderness Environ Med. 2005;16(3):164–167. doi:10.1580/1080-6032(2005)16[164:rofmfe]2.0.co;2 [DOI] [PubMed]
- 11.Fung HTJ, Lam SKT, Lam KK, Kam CW, Simpson ID. A Survey of Snakebite Management Knowledge Amongst Select Physicians in Hong Kong and the Implications for Snakebite Training. Wilderness Environ Med. 2009;20(4):364–370. doi: 10.1580/1080-6032-020.004.0364 [DOI] [PubMed]
- 12.Inthanomchanh V, Reyer JA, Blessmen J, Phrasisombath K, Yamamoto E, Hamajima N. Assessment of knowledge about snakebite management amongst healthcare providers in the provincial and two district hospitals in Savannakhet Province, Lao PDR. Nagoya J Med Sci. 2017;79(3):299–311. doi: 10.18999/nagjms.79.3.299 [DOI] [PMC free article] [PubMed]
- 13.Gutiérrez JM, Williams D, Fan HW, Warrell DA. Snakebite envenoming from a global perspective: Towards an integrated approach. Toxicon. 2010;56(7):1223–1235. doi: 10.1016/j.toxicon.2009.11.020 [DOI] [PubMed]
- 14.Rao VD, Bickram P, Ramyatha RP, Sumalatha N. Analysis of Snake Bite Victims in a Tertiary Care Center. Health Renaiss. 2014;12(1):24–28. doi: 10.3126/hren.v12i1.11981 [DOI]
- 15.Aengals R, Kumar SVM, Palot MJ. Updated Checklist of Indian Reptiles. Zoological Survey of India, 2011. www.zsi.gov.in/checklist/Reptiles .
- 16.Asokan JR. Snakes An Introduction. First Edition, Madras Commissioner of Museums Government Museum, Madras, India, 1996.
- 17.Whitaker R, Captain A, Ahmed F. Snakes of India: The Field Guide. Chennai: Draco Books; 2004.
- 18.Joseph JK, Simpson ID, Menon NCS, et al. First authenticated cases of life-threatening envenoming by the hump-nosed pit viper (Hypnale hypnale) in India. Trans R Soc Trop Med Hyg. 2007;101(1):85–90. doi: 10.1016/j.trstmh.2006.03.008 [DOI] [PubMed]
- 19.Kochar DK, Tanwar PD, Norris RL, et al. Rediscovery of severe saw-scaled viper (Echis sochureki) envenoming in the Thar desert region of Rajasthan, India. Wilderness Environ Med. 2007;18(2):75–85. doi: 10.1580/06-WEME-OR-078R.1. [DOI] [PubMed]
- 20.Simpson ID, Norris RL. Snakes of medical importance in India: is the concept of the “Big 4” still relevant and useful? Wilderness Environ Med. 2007;18(1):2–9. doi: 10.1580/06-weme-co-023r1.1. [DOI] [PubMed]
- 21.Ghosh S, Mukhopadhyay P, Chatterjee T. Management of Snake Bite in India. J Assoc Physicians India. 2016;64(8):11–14. [PubMed]
- 22.Michael GC, Thacher TD, Shehu MIL. The effect of pre-hospital care for venomous snake bite on outcome in Nigeria. Trans R Soc Trop Med Hyg. 2011;105(2):95–101. doi: 10.1016/j.trstmh.2010.09.005. [DOI] [PubMed]
- 23.Wang W, Chen Q-F, Yin R-X, et al. Clinical features and treatment experience: a review of 292 Chinese cobra snakebites. Environ Toxicol Pharmacol. 2014;37(2):648–655. doi: 10.1016/j.etap.2013.12.018. [DOI] [PubMed]
- 24.Samy RP, Thwin MM, Gopalakrishnakone P, Ignacimuthu S. Ethnobotanical survey of folk plants for the treatment of snakebites in Southern part of Tamilnadu, India. J Ethnopharmacol. 2008;115(2):302–312. doi: 10.1016/j.jep.2007.10.006. [DOI] [PubMed]
- 25.Madaki JKA, Obilom RE, Mandong BM. Pattern of First-Aid Measures Used by Snake-bite Patients and Clinical Outcome at Zamko Comprehensive Health Centre, Langtang, Plateau State. Niger Med Pract. 2005;48(1):10–13–13.
- 26.Warrell DA. Guidelines for the management of snake-bites. World Health Organization South-East Asia Regional Office, New Delhi. (2010). http://apps.searo.who.int/PDS_DOCS/B4508.pdf
- 27.Silveria PV, Nishioka S de A. Non-venomous snake bite and snake bite without envenoming in a Brazilian teaching hospital. Analysis of 91 cases. Rev Inst Med Trop Sao Paulo. 1992;34(6):499–503. doi: 10.1590/s0036-46651992000600002. [DOI] [PubMed]
- 28.Silveira PV, Nishioka S de A. Venomous snake bite without clinical envenoming (‘dry-bite’). A neglected problem in Brazil. Trop Geogr Med. 1995;47(2):82–85. [PubMed]
- 29.Whitaker R, Whitaker S. Venom, antivenom production and the medically important snakes of India. Curr Sci. 2012;103(6):635–643.
- 30.Bhargava S, Sarin RK, Singh R. The medico-legal issues of snake envenomations in India. J Forensic Med Toxicol. 2019;36(1):78–82. doi: 10.5958/0974-4568.2019.00020.6. [DOI]