Abstract
Background
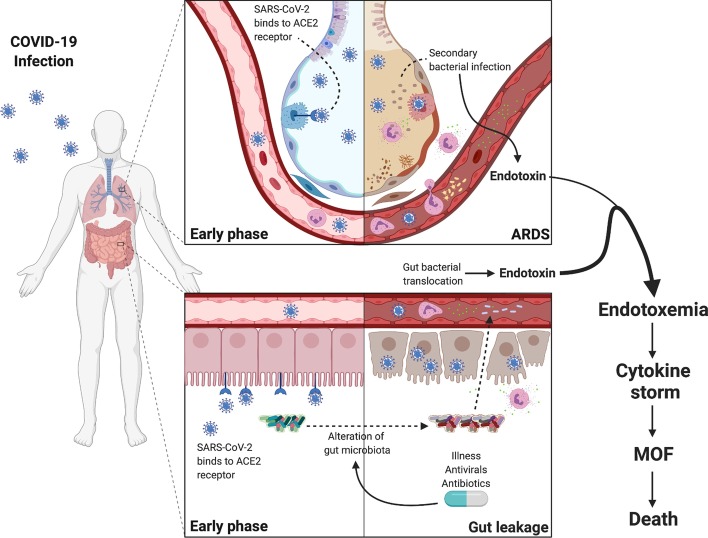
When severe, COVID-19 shares many clinical features with bacterial sepsis. Yet, secondary bacterial infection is uncommon. However, as epithelium is injured and barrier function is lost, bacterial products entering the circulation might contribute to the pathophysiology of COVID-19.
Methods
We studied 19 adults, severely ill patients with COVID-19 infection, who were admitted to King Chulalongkorn Memorial Hospital, Bangkok, Thailand, between 13th March and 17th April 2020. Blood samples on days 1, 3, and 7 of enrollment were analyzed for endotoxin activity assay (EAA), (1 → 3)-β-d-glucan (BG), and 16S rRNA gene sequencing to determine the circulating bacteriome.
Results
Of the 19 patients, 13 were in intensive care and 10 patients received mechanical ventilation. We found 8 patients with high EAA (≥ 0.6) and about half of the patients had high serum BG levels which tended to be higher in later in the illness. Although only 1 patient had a positive blood culture, 18 of 19 patients were positive for 16S rRNA gene amplification. Proteobacteria was the most abundant phylum. The diversity of bacterial genera was decreased overtime.
Conclusions
Bacterial DNA and toxins were discovered in virtually all severely ill COVID-19 pneumonia patients. This raises a previously unrecognized concern for significant contribution of bacterial products in the pathogenesis of this disease.
Keywords: COVID-19, Critically ill, Endotoxemia, Circulating bacteriome, Acute respiratory distress syndrome, Sepsis
Background
While most cases coronavirus disease 2019 (COVID-19) are mild, severe COVID-19 pneumonia can occur with a mortality rate as high as 50% [1]. It is unclear why some patients develop clinical features of sepsis/septic shock with multiple organ dysfunction [2]. The majority of bacterial cultures from severe COVID-19 patients are negative [3], and although empiric antibiotics are commonly used [3–5], they are not recommended [6]. However, while the respiratory tract is the principle site of infection for COVID-19, the disease has been shown to involve the GI tract as well and symptoms such as diarrhea are reported in about a third of cases [7]. Enterocytes in ileum and colon express the ACE2 receptor and virus has been detected in stool. Thus, there is a possibility that bacterial translocation from the GI tract might complicate severe COVID-19 disease [8].
Endotoxin, a part of the cell wall of Gram-negative bacteria, has been extensively investigated and acknowledged as one of the key triggers of lethal shock during severe sepsis and also one of the primary drivers of the cytokine storm [9–11]. Serum (1→ 3)-b-d-glucan (BG) has been evaluated as a potential marker of intestinal barrier dysfunction. Serum BG was tested in several mouse models of gut leakage, including dextran sulfate solution administration, endotoxin injection, and cecal ligation and puncture sepsis [12]. However, the presence of endotoxemia and serum BG in severe COVID-19 has never been examined. Not only bacterial toxin, but also direct bacterial invasion might play role in severe COVID-19. Exploring circulating bacteriome in severe COVID-19 may allow us to test the presence of any bacterial invasion during critical illness.
Thus, we designed this investigation to determine whether bacterial products were present in the blood of severe COVID-19 pneumonia patients and whether their source was likely to be the gut as evidenced by serum BG. We also sought to characterize the circulating bacteriome in COVID-19 pneumonia.
Methods
Study population, setting, and data collection
This was a prospective observational study in COVID-19 pneumonia patients admitted to King Chulalongkorn Memorial Hospital, Bangkok, Thailand, between 13th March and 17th April 2020. Our inclusion criteria included (1) age > 18 years, (2) confirmed COVID-19 pneumonia, and (3) had leftover blood samples. The first day of enrollment was the day that patients fulfilled inclusion criteria. The study was reviewed and approved by Faculty of Medicine, Chulalongkorn University ethics committee (IRB no. 336/63). The informed consent was waived due to the observational nature of the study. The study was designed and conducted according to the STROBE guideline [13].
We obtained demographic data, information on clinical presentations, laboratory investigations, and radiography at the time of presentation, and during intensive care unit (ICU) admission. We collected blood samples that were left over on day 1, day 3, and day 7 after enrollment. All laboratory tests and radiologic assessments, including standard chest radiographs and chest computed tomography, were performed at the discretion of the treating physician. Endotoxin activity assay (EAA), cytokines, and serum BG were measured on day 1, 3, and 7 of enrollment. We assessed clinical outcomes on day 28 after enrollment, including mechanical ventilation, ventilator-free day, vasopressor, prone position, extracorporeal membrane oxygenation (ECMO), acute kidney injury (AKI), renal replacement therapy (RRT), and successful extubation.
Study definitions
A confirmed case of COVID-19 was defined by a positive result of a reverse transcriptase-polymerase chain reaction (RT-PCR) assay of a specimen collected from a nasopharyngeal swab. We defined COVID-19 pneumonia as a COVID-19 case who showed the evidence of pulmonary infiltration from chest radiography or chest computer tomography. We defined severe COVID-19 as a COVID-19 case who was admitted in ICU. Acute kidney injury was defined based on serum creatinine and urine output criteria according to the Kidney Disease Improving Global Outcome 2012 guideline [14]. We defined patient with high endotoxin by EAA ≥ 0.6 on day 1.
Standard of care treatment
Treating physicians performed thorough evaluations and managed COVID-19 patients with standard care including volume status assessment, hemodynamic and respiratory support according to Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19) [6]. Although, currently, there is no specific antiviral treatment for COVID-19, antiviral therapy was given to all patients with confirmed COVID-19 pneumonia as recommended by the Department of Medical Service, Ministry of Public Health of Thailand. The treatment consists of a combination of (1) favipiravir, (2) lopinavir/ritonavir or darunavir, (3) hydroxychloroquine, and (4) azithromycin. Other treatments including intravenous fluid administration and supportive medication were given in discretion of attending physicians.
Laboratory procedures
COVID-19 test confirmation
COVID-19 tests were performed by qRT-PCR technique using cobas® SARS-CoV-2 qualitative test with the cobas®6800 platform (Roche Diagnostics, Indianapolis, IN). We followed the manufacturer’s instructions for testing. The samples were obtained by nasopharyngeal swab and preserved in viral transport cases before sending to analysis. The qRT-PCR tests provided cycle threshold (Ct) value for each test. These values represent the number of cycles required for the positive fluorescent signal. Therefore, the lower Ct values correlated with the higher viral load. The assay is designed to detect ORF1 genes and N genes of SARS-CoV-2. The result was considered positive when the Ct values of both target genes were < 40, negative when they were both > 40. If only one of the target genes had a Ct value < 40, the tests were confirmed by another RT-PCR machine, CFX96 Touch qPCR Detection System (Bio-Rad, Hercules, CA) with detection of 3 genes (ORF1 gene, ORF3 gene, and N gene). All procedures were performed in a biosafety level 2 laboratory.
Endotoxin activity assay
We performed the chemiluminescent-based endotoxin activity assay (EAA; Spectral Diagnostics, Ontario, Canada) as described elsewhere [15]. This assay is based on the detection of enhanced respiratory burst activity in neutrophils following their priming by complexes of endotoxin and a specific anti-endotoxin antibody. Briefly, 40 μL of whole blood were incubated with zymosan and anti-endotoxin antibody. The endotoxin activity level of ≥ 0.60 was considered as high activity level (Additional file 1).
Serum (1 → 3)-b-d-glucan (BG)
We analyzed serum for BG with Fungitell® assay (Associates of Cape Cod, Falmouth, MA) following manufacturer instructions. Briefly, 5 mL of serum was mixed with an alkaline pretreatment reagent (0.125 M KOK/0.6 M KCl) and incubated at 37 °C for 10 min. One hundred microliters of the reconstituted Fungitell reagent was added to each well and the reaction monitored at A405nm–A490nm for 40 min. The Fungitell assay detects BG through the activation of factor G, a protease zymogen which activates a second protease zymogen, pro-clotting enzyme, that cleaves a chromophore from a chromogenic peptide resulting in light absorbance at 405 nm. Serum BG > 60 pg/mL was used as positive cut-off [16]. BG values at < 7.8 pg/mL and > 523.4 pg/mL were recorded as 0 and 523 pg/mL, respectively (Additional file 2).
Cytokines
We measured a panel of cytokines including interleukin-1 beta (IL-1β), interferon-alpha-2 (IFN-α2), interferon gamma (IFN-γ), tumor necrosis factor-α (TNF-α), monocyte chemoattractant protein-1 (MCP-1), interleukin-6 (IL-6), interleukin-8 (IL-8), interleukin-10 (IL-10), interleukin-12, p70 (IL-12 p70), interleukin-17A (IL-17A, interleukin-18 (IL-18), interleukin-23 (IL-23), and interleukin-33 (IL-33) at the same time points using LEGENDplex™ Human Th Cytokine Panel (BioLegend, San Diego, CA, USA) according to manufacturer’s protocol.
16S rDNA high-throughput sequencing
Genomic DNA was extracted from 300 µl of whole blood using the GenUp™ gDNA kit (Biotechrabbit, Germany). The amplification of the bacterial 16S rDNA was performed in total volume 25 µl consisting of Taq DNA polymerase (0.5U) (Biotechrabbit, Germany), 1.5 mM MgCl2, 0.2 mM dNTPs, 0.2 mM forward primer 5′-ACTCCTACGGRAGGCAGCAG-3′ and 0.2 mM reverse primer 5′-CCGTCAATTYYTTTRAGTTT-3′. The PCR product was re-amplified within V4 region of 16S rDNA by using phasing adaptor primers following from [17]. Amplified PCR products (~ 430 bp) were purified by using the QIAquick PCR Purification Kit (QIAGEN, Germany) and quantified by KAPA library quantification kits for Illumina platforms (Kapa Biosystems, USA). The DNA libraries were pooled at equal amount and paired-end (2 × 250 cycles) sequenced on an Illumina MiSeq platform with a MiSeq Reagent Kit V2 (Illumina, USA).
Statistical analyses
Raw sequencing data were demultiplexed by MiSeq reporter software (version 2.6.2.3). The FASTQ files were analyzed by QIIME2 pipeline (version 2019.7) [18]. The paired-end sequences were merged and trimmed based on quality score (< Q30). Then, merged reads were deduplicated and clustered with 99% similarity by using VSEARCH [19]. UCHIME algorithm was used for filtering out the chimeric sequences [20]. The filtered reads were classified based on 16S Greengene database [21] using VSEARCH algorithm. The alpha diversity was analyzed by implemented function in QIIME2. Differential abundance analysis was conducted by linear discriminant analysis effect size (LEfSe) [22]. Wilcoxon matched pairs test were analyzed using GraphPad Prism version 6.01.
Statistical comparisons for continuous and categorical data were performed using Chi-square/Fisher exact test and Mann–Whitney U test/Kruskal–Wallis test. Data are reported as counts (percentages) for categorical and median with interquartile range for continuous data. No imputation was performed on missing data. All statistical analyses were performed using Stata version 15.1 (STATA Corp, TX). P value of less than 0.05 was considered as statistical significance for all tests performed.
Results
A total of 147 patients were recruited. Of these, 53 (34.6%) patients were diagnosed COVID-19 pneumonia. Among patients with COVID-19 pneumonia, only 19 patients fulfilled the inclusion criteria and 13 (68.4%) patients were admitted in the ICU (Fig. 1). Male sex was predominant in our cohort. Markers of inflammations including ferritin, C-reactive protein (CRP), and IL-6 were markedly high (Table 1). Detailed clinical data and the outcomes of 19 patients are shown in Table 2 and Additional file 3: Table S1.
Fig. 1.
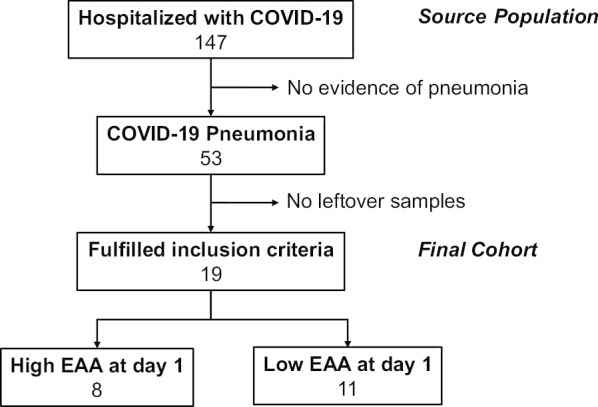
Study cohort
Table 1.
Clinical characteristics of COVID-19 pneumonia at enrollment
| Characteristic | Total (N = 19) |
EAA ≥ 0.6 (N = 8) |
EAA < 0.6 (N = 11) |
|---|---|---|---|
| Age, years | 54 (43, 59) | 49 (40, 59) | 57 (48, 58) |
| Male | 15 (79%) | 6 (75) | 9 (82) |
| APACHE II score |
8 (4, 11) N = 13 |
9 (5, 10) N = 5 |
7.5 (4.0, 11.5) N = 8 |
| SOFA score | 6 (3, 10) |
5 (3, 11) N = 5 |
6 (3.5, 9) N = 8 |
| PaO2/FiO2 ratio at enrollment |
233 (186, 261) N = 13 |
246 (186, 293) N = 5 |
223 (187, 254) N = 8 |
| Underlying disease | |||
| Hypertension | 6 (32) | 1 (13) | 5 (45) |
| Diabetes | 8 (42) | 2 (25) | 6 (55) |
| Chronic kidney disease | 2 (11) | 0 | 2 (18) |
| Time from onset of fever to hospital admission (days) | 5 (3, 7) | 3.5 (2, 5) | 7 (5, 8) |
| Time from onset of fever to 1st EAA measurement (days) | 9 (9, 11) | 9 (6, 12.5) | 9 (9, 11) |
| ICU admission (%) | 13 (68.4) | 5 (62.5) | 8 (72.7) |
| Serum creatinine, mg/dL | 0.90 (0.80, 1.16) | 0.82 (0.69, 1.07) | 0.91 (0.86, 1.28) |
| EAA level | 0.57 (0.47, 0.86) | 0.86 (0.80, 0.90) | 0.48 (0.42, 0.57) |
| Cycle threshold | 23.9 (18.3, 27.7) | 23.7 (15.8, 27.0) | 24.9 (18.3, 30.1) |
| Ferritin | 872 (638, 2409) | 740 (417, 2047) | 1057 (750, 2771) |
| CRP | 127 (27.5, 1457) | 38 (27.5, 130) | 137 (70, 175) |
| Procalcitonin | 0.16 (0.07, 0.55) | 0.11 (0.03, 2.34) | 0.24 (0.09, 0.43) |
| Treatment | |||
| Darunavir | 9 (47) | 6 (75) | 3 (27) |
| Ritonavir | 9 (47) | 6 (75) | 3 (27) |
| Favipiravir | 18 (95) | 7 (88) | 11 (100) |
| Antimalarial drug | 18 (95) | 8 (100) | 10 (91) |
| Azithromycin | 13 (68) | 6 (75) | 7 (64) |
| Corticosteroid | 4 (21) | 3 (38) | 1 (9) |
| Antibiotic | 13 (68) | 5 (63) | 8 (73) |
Data shown as counts (%) or median (IQR)
APACHE II Acute Physiology and Chronic Health Evaluation II, CRP C-reactive protein, EAA endotoxin activity assay, FiO2 fractional inspired oxygen, IL-6 interleukin-6, PaO2 partial pressure of arterial oxygen, SOFA Sequential Organ Failure Assessment
Table 2.
Outcomes at 28 days after enrollment
| Characteristic | Total (N = 19) |
EAA ≥ 0.6 (N = 8) |
EAA < 0.6 (N = 11) |
|---|---|---|---|
| Subsequent bacterial infection | 5 (26%) | 3 (38%) | 2 (18%) |
| Total mechanical ventilation | 10 (52.6) | 5 (62.5) | 5 (45.5) |
| Successful extubation | 8/10 (80%) | 4/5 (80%) | 4/5 (80%) |
| Ventilator-free day (days) | 24 (20, 28) | 23.5 (15, 28) | 28 (21.5, 28) |
| Vasopressor | 7 (36.8) | 2 (25.0) | 5 (45.5) |
| Prone position | 2 (10.5) | 2 (25.0) | 0 |
| ECMO | 1 (5.3) | 1 (12.5) | 0 |
| AKI | 8 (42.1) | 2 (25.0) | 6 (54.5) |
| RRT | 3 (15.8) | 2 (25.0) | 1 (9.1) |
| Mortality | 0 | 0 | 0 |
Data shown as counts (%) or median (IQR)
AKI acute kidney injury, EAA endotoxin activity assay, ECMO extracorporeal membrane oxygenation, RRT renal replacement therapy
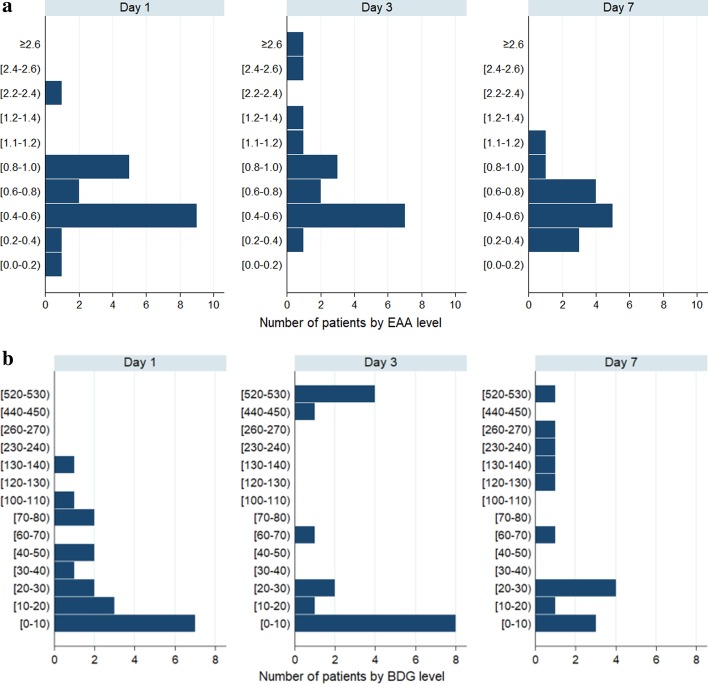
Endotoxin activity and BG
Overall median (IQR) EAA on day 1, day 3, and day 7 were 0.57 (0.47, 0.86), 0.65 (0.49, 0.96), and 0.57 (0.43, 0.74), respectively. There were 8 (42.1%) patients with day 1 EAA ≥ 0.60 (Table 1). Distributions of EAA on day 1, day 3, and day 7 are shown in Fig. 2a.
Fig. 2.
a EAA distribution of COVID-19 pneumonia. b Serum BG distribution of COVID-19 pneumonia
Figure 2b demonstrates the distributions of serum BG following day of enrollment. During 7 days of observation, 8 patients (42.1%) had high BG levels (defined as BG > 60 pg/mL), and 37.5% of patients with high BG also had EAA > 0.6. The level of BG increased following the day of enrollment (Fig. 2b). The median BG levels were higher in patients with high EAA compared those with low EAA [day1 (25 VS 12 pg/mL), day 3 (42 vs 10 pg/mL), and day 7 (75 vs 26 pg/mL)].
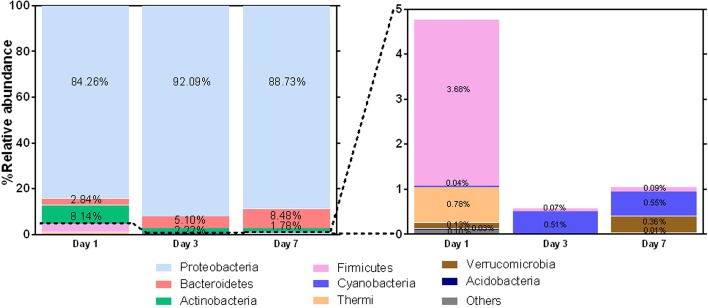
Circulating bacteriome
Forty-nine of 50 samples (98.3%) from 19 COVID-19 pneumonia patients had presence of bacterial DNA in serum. Rarefaction curves are shown in Additional file 4: Figure S1. Bacterial classification revealed that the relative abundances of bacteria were different among patients and days of illness (Additional file 4: Figure S2). Taxonomy composition phyla abundances revealed that the Proteobacteria phylum was the predominant phylum at every time point (Fig. 3, Additional file 4: Figure S3). Interestingly, Gram-negative bacterial genera including Sphingomonas, Bradyrhizobium, Enhydrobacter, Phyllobacterium, Agrobacterium, Comamonas, Sediminibacterium, Acinetobacter, and Pseudomonas were most likely found in different days of illness (Additional file 4: Figure S2). Biodiversity of bacteria, demonstrated by the Chao1 richness, on day 1 was significantly higher than on day 3 (Additional file 4: Figures S4, S5). The bacterial genera including Sphingomonas and Sediminibacterium were significantly (P < 0.05) higher on day 3 compared to day 1; whereas Comamonas, Acinetobacter, and Pseudomonas were significantly (P < 0.05) decreased on day 3 (Additional file 4: Figure S6).
Fig. 3.
Overall summary of dynamic bacterial community profiles in COVID-19 patients on day 1, 3, and 7. Proteobacteria were observed to be the dominant bacterial phyla followed by Bacteroidetes, Actinobacteria and Firmicutes
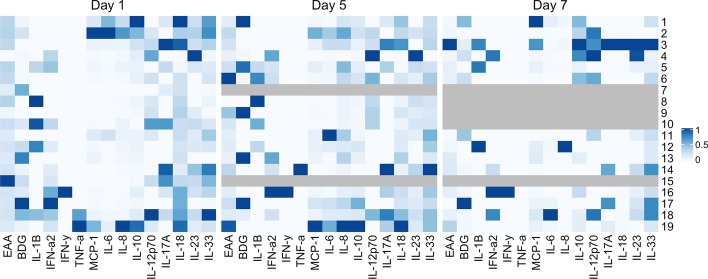
Cytokines
A heat map of cytokine levels on day 1, 3, and 7 is depicted in Fig. 4. Most of COVID-19 pneumonia had elevated of cytokines. On day 1, MCP-1, IL-6, IL-8, IL-10 in COVID-19 pneumonia who were admitted in ICU were significantly higher than COVID-19 pneumonia who were not admitted in ICU [(848 (410, 1782) vs 285 (215, 300), P = 0.003; 45 (16, 334) vs 12 (7, 25), P = 0.023; 73 (47, 128) vs 24 (20, 41), P = 0.009; 23 (19, 56) vs 8 (2, 13), P = 0.022.] (Additional file 3: Table S2).
Fig. 4.
Cytokine heat map on day 1, day 3, and day 7
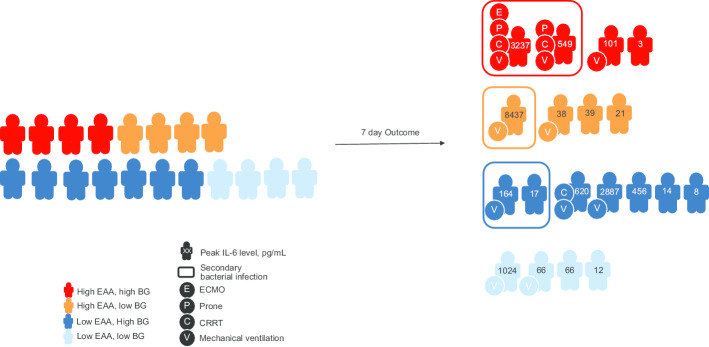
Clinical characteristics at baseline and outcomes
Comparing clinical features between patients with high (≥ 0.6 on day 1) and low EAA (< 0.6 on day 1) revealed that those with high EAA had lower median age, and higher severity scores (Table 1). Patients with high EAA levels sought medical attention earlier than patients with low EAA levels [median time from onset of fever to hospital admission [3.5 (2, 5) vs 7 (5, 8)].
Regarding clinical outcomes, there were five patients who had subsequent infection. All of them had positive bacterial culture from endotracheal suctions or sputum. Three patients had Acinetobacter baumanmii pneumonia around 7 days after ICU admission. One patient had Pseudomonas pneumonia 3 days after admission. One patient had Klebsiella pneumoniae pneumonia 3 days after admission. Patients with high EAA were more likely to develop subsequent bacterial infection within 28 days after enrollment (38% vs 18%). Patients with high EAA tended to need more mechanical ventilation support than the low-EAA group (62.5% vs 45.5%). The proportion of patients requiring vasopressors, prone position, and ECMO did not differ between EAA groups (Table 2).
The 28-day outcomes are shown in Fig. 5. The overall rate of AKI (any stage) in our study was 42.1%. Three (15.8%) patients required renal replacement therapy (RRT). When compared to patients with low EAA, patients with high EAA tended to have lower ventilator-free days [23.5 (15, 28) vs 28 (21.5, 28)] and successful extubation rate (20% vs 60%). No patient died within 28 days after enrollment.
Fig. 5.
Clinical outcomes in study cohort
We have compared EAA and BG level of our COVID-19 patients with the data from our previous study in 136 severe sepsis or septic shock patients (Additional file 2: Figure S7a and S7b) [23, 24]. This demonstrated that COVID-19 patients had EAA and BG levels comparable to severe sepsis patients.
Discussion
In this cohort of COVID-19 pneumonia, we show that nearly 90% and 40% of patients had endotoxemia (defined as a moderate to high level of EAA), and high levels of BG, a measure of gut permeability (Fig. 2). Using next-generation sequencing (NGS), we could also demonstrate the dominant bacterial DNA came from Proteobacteria, a phylum of Gram-negative bacteria which includes several pathogens that can cause sepsis (Fig. 3).
In animals, high endotoxin activity in viral infection has been demonstrated to be associated with poor outcome. Inoculation of lipopolysaccharides (LPS) in mice with influenza infection resulted in the activation of local pulmonary inflammatory responses and may lead to secondary bacterial pneumonia [25]. LPS binds with toll-like receptor 4 (TLR4) and activates transcription factors activating protein-1 (AP-1), nuclear factor kappa B (NF-kB) and interferon regulatory factor 3 (IRF3) through myeloid differentiation factor 88 (MyD88) and TIR-domain-containing adapter-inducing interferon-β (TRIF)-dependent pathways. This leads to the induction of proinflammatory cytokines and interferons [26].
BG is a key structural polysaccharide of the cell wall of most fungi including Candida spp., and has been used in the diagnosis of invasive fungal infection [16, 27]. Leelahavanichkul et al. reported the use of serum BG as a biomarker of gut permeability in human sepsis [12]. In our study, the increase of serum BG level later in the course of illness (Fig. 2b) might reflect overgrowth of Candida spp. in the gastrointestinal tract from antibiotics exposure [28]. Intestinal Candida overgrowth alone did not increase serum BG. Hence, the detection of BG in serum implied gut-permeability defect in these patients. In addition, BG also induced proinflammatory responses through Dectin-1 signaling [12].
With NGS, a highly sensitive technology, we could detect bacteria which were unable to grow using standard culture methods. From previous reports, bacterial DNA and RNA were discovered between 4 and 100% in blood of healthy individual [29–33]. Our data agree with Gosiewski et al. which showed increased abundance of proteobacteria in sepsis patients compared to the healthy population (60.1% vs 16.4%) [34]. This raises the possibility that COVID-19 could cause a sepsis-like syndrome with the same dominant bacteria phylum as in sepsis patients. This phylum contains many genera of bacteria. The most predominant bacteria were Sphingomonas, Bradyrhizobium, and Enhydrobacter. Sphingomonas paucimobilis is an opportunistic pathogen that can cause hospital-associated infections from environmental exposure [35]. Bradyrhizobium enterica were found in patients with colitis [36]. Enhydrobacter aerosaccus can be detected from a patient with Hemophagocytic lymphohistiocytosis (HLH) with concomitant corticosteroid use [37]. This is particularly of interest due to the growing evidence of HLH syndrome in severe COVID-19 patients [38]. This hypothesis was supported by a recently published study. Arunachalam et al. demonstrated that severe COVID-19 patients had significant increase plasma LPS and bacterial 16S rRNA gene product when compared to healthy adults [39]. From these data, we proposed that both number and diversity of bacteria might contribute to severity of COVID-19 (Additional file 4: Figures S1–S7).
Patients with COVID-19 have been found to have high levels of proinflammatory cytokines such as IL-6, IL-1β, IP10, and MCP-1 [4]. Similar findings were also reported in patients with SARS [40] and MERS-CoV [41]. This has prompted several authors to discuss so-called “Cytokine Storm” in viral respiratory infection that is a cause of multiple organ failure. However, our results suggest that bacterial products might be another possible contributor to the cytokine storm rather than only the virus itself (Additional file 4: Figures S1–S7).
The source of bacterial toxin, and bacterial DNA in the blood of patients with COVID-19 pneumonia is unclear. It is possible that viremia results in capillary leakage syndrome similar to bacterial sepsis which causes interstitial edema and induces dysfunction of the lung and intestinal barrier which may facilitate bacterial toxin and live bacteria translocation into the circulation. These bacterial products then induce the release of proinflammatory cytokines. In our study, many patients (47.3%) ultimately developed subsequent bacterial infection within 28 days. Hanada et al. proposed the mechanism of viral-induced susceptibility of secondary bacterial infection involving local and systemic immune response which results in alterations in respiratory and gut microbiomes and impaired pulmonary immune response [42]. However, the GI tract appears to be another target of COVID-19. Similar to respiratory tract, various cells in the GI tract also express ACE2 and TMPRSS2 which are crucial for fusion of viral particles with host cells [43, 44]. Biopsies from severe cases have revealed involvement of COVID-19 throughout the GI tract from esophagus to colon [45]. Thus, we propose that loss of gut barrier function might be one of the mechanisms that contribute to the presence of bacterial toxin and bacterial DNA in the blood of patients with severe COVID-19 (Fig. 6).
Fig. 6.
Hypothetical pathogenesis of endotoxemia in COVID-19 pneumonia. At early stage, SARS-CoV-2 primarily infects type 2 pneumocytes in the lungs and causes pneumonia which can progress to ARDS and induces susceptibility of secondary bacterial infection by impairing the pulmonary immune response. The virus can enter the bloodstream causing viremia targeting organs with high ACE2 expression including the gut. SARS-CoV-2 infection of enterocytes causes inflammatory response of gastrointestinal tract which results in alteration of the intestinal microenvironment including epithelial hyperpermeability, attenuated local immune system, and dysbiosis of the microbiome. The perturbations of the intestinal microenvironment allow the pathogenic bacteria from the gut lumen to translocate to the bloodstream. Hence, we propose the sources of endotoxin to be majorly from the gut and minorly from the secondary bacterial infection of the lungs. COVID-19, the coronavirus disease 2019; SAR-CoV-2, severe acute respiratory syndrome coronavirus 2; ARDS, acute respiratory distress syndrome; ACE2, angiotensin converting enzyme 2; MOF, multiple organ failure
To our knowledge, this is the first study to demonstrate evidence of bacterial toxins including EAA, and the presence of circulating bacteriome in patients with COVID-19 pneumonia. We also showed the association of high level of EAA and the severity of COVID-19 pneumonia. Both the type of bacteria and the presence of BG in the serum suggest that the gut is the source.
Our study had several limitations. First, our 16s RNA gene amplification technique could not demonstrate the absolute number of bacterial DNA. Therefore, we could not correlate the burden of circulating bacterial DNA to the severity of the patients. However, our study aimed to be a starting point for future investigation. Second, our study did not include respiratory tract or gastrointestinal specimens, so we cannot completely establish the source of bacterial products in our patients. Future study should explore the effect of organ crosstalk between the lung and the intestine during COVID-19 infection. Third, this was a single-center study and all patients had Thai ethnicity. Lastly, we did not use more specific invasive test such as urine sucralose tests for GI leakage due to unstable conditions of the patients. Instead, we used BG which is a non-invasive biomarker to demonstrate GI leakage. From previous study, BG was evaluated as a potential marker of intestinal barrier dysfunction [12].
Conclusions
High levels of endotoxin activity and bacterial DNA can be found in the blood of patients with COVID-19 pneumonia. This previously unrecognized mechanism of hyperinflammation and organ failure in COVID-19 warrants further study.
Supplementary Information
Additional file 1. EAA laboratory specification manual.
Additional file 2. BG laboratory specification manual.
Additional file 3: Table S1. Clinical characteristics of COVID-19 pneumonia. Table S2. Cytokines level on day 1, day 3, and day 7 stratified by ICU admission status.
Additional file 4: Figure S1. Rarefaction curve of pass-filter reads obtained from each sample. Figure S2. Dynamic bacterial community profiles on day 1, day 3, and day 7. Figure S3. Dynamic bacterial community profiles at the phylum level in COVID-19 patients. Figure S4. Shannon diversity index (A) and Chao1 richness (B) representing alpha diversity of bacterial community profiles in COVID-19 patients on day 1, 3, and 7. The Shannon diversity index was not significant differences among the date of onsets whereas the Chao1 richness was significant (P < 0.05) between the first and third date of onsets Figure S5. LEfSe analysis of bacteria on day 1 and day 3. Figure S6. Wilcoxon matched pairs test differential abundant of bacterial genera in each COVID-19 patient between day 1 and day 3. The bacterial genera including Sphingomonas and Sediminibacterium were significantly (P < 0.05) higher in the third date compared to the first of onset whereas Comamonas, Acinetobacter and Pseudomonas were significantly (P < 0.05) decreased during the third date of onsets. Figure S7. Comparison of EAA level (Figure S7a) and BG (Figure S7b) between COVID-19 and other type of infections using data from our previous studies in 136 severe sepsis or septic shock patients.
Acknowledgments
We would like to thank the staff, fellows, nurses, and research coordinators from the Excellence Center for Critical Care Nephrology (EC-CCN) and Emerging Infectious Disease (EID) unit, Faculty of Medicine, Chulalongkorn University. We also thank Miss Pimnara Peerawaranun for statistical analysis and Miss Sasipha Tachaboon medical technologist, for laboratory procedures.
Abbreviations
- AKI
Acute kidney injury
- BG
(1 → 3)-β-D-Glucan
- AP-1
Activates transcription factors activating protein-1
- COVID-19
Coronavirus disease 2019
- Ct
Cycle threshold
- CRP
C-reactive protein
- ECMO
Extracorporeal membrane oxygenation
- EAA
Endotoxin activity assay
- ICU
Intensive care unit
- IFN-α2
Interferon alpha-2
- IFN-γ
Interferon gamma
- HLH
Hemophagocytic lymphohistiocytosis
- IRF3
Interferon regulatory factor 3
- IL-1β
Interleukin-1 beta
- IL-6
Interleukin-6
- IL-8
Interleukin-8
- IL-10
Interleukin-10
- IL-12 p70
Interleukin-12, p70
- IL-17A
Interleukin-17A
- IL-18
Interleukin-18
- IL-23
Interleukin-23
- IL-33
Interleukin-33
- IQR
Interquartile range
- LEfSe
Linear discriminant analysis effect size
- LPS
Lipopolysaccharides
- MCP-1
Monocyte chemoattractant protein-1
- MyD88
Myeloid differentiation factor 88
- NGS
Next-generation sequencing
- NF-kB
Nuclear factor kappa B
- RRT
Renal replacement therapy
- RT-PCR
Reverse transcriptase-polymerase chain reaction
- TLR4
Toll-like receptor 4
- TNF-α
Tumor necrosis factor-α
- TRIF
TIR-domain-containing adapter-inducing interferon-β
Authors’ contributions
PS, WK, and NS were responsible for study concept and design. PS, WK, NS, TP, AC, SP, PP, SC, VS, NW, SK, OP, TT, NL, VP, NP, TS, RS, ST, KT, NLu, AL, TSri, TTa, UT, CC, KP, KTu, SE, JK, and NS were responsible for the acquisition, analysis, or interpretation of data. PS, WK and NS were responsible for drafting the manuscript. PS, WK and NS were responsible for statistical analysis. All authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors interpreted the findings, contributed to writing the manuscript. All authors read and approved the final manuscript.
Funding
The investigator-initiated study was funded by the Excellence Center for Critical Care Nephrology, King Chulalongkorn Memorial Hospital.
Availability of data and materials
On reasonable request, data from this study are available from the corresponding author.
Ethics approval and consent to participate
The study was reviewed and approved by Faculty of Medicine, Chulalongkorn University ethics committee (IRB no. 336/63). The informed consent was waived due to the observational nature of the study.
Consent for publication
Not applicable.
Competing interests
Toray Industries provided endotoxin activity assay kits for use in this study. The company had no influence on the study design or analysis or on the comment of this article. None of the other authors have any disclosures.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Phatadon Sirivongrangson and Win Kulvichit contributed equally to this work
Supplementary Information
Supplementary information accompanies this paper at 10.1186/s40635-020-00362-8.
References
- 1.Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Greninger AL, Pipavath S, Wurfel MM, Evans L, Kritek PA, West TE, Luks A, Gerbino A, Dale CR, Goldman JD, O'Mahony S, Mikacenic C. Covid-19 in Critically Ill patients in the seattle region - case series. N Engl J Med. 2020 doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan China. Lancet. 2020;395(10223):497–506. doi: 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS, China Medical Treatment Expert Group for C clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, Laundy M, Morgan JS, Kesecioglu J, McGeer A, Mermel L, Mammen MJ, Alexander PE, Arrington A, Centofanti J, Citerio G, Baw B, Memish ZA, Hammond N, Hayden FG, Evans L (2020) Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). ESICM
- 7.Luo S, Zhang X, Xu H. Don't overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19) Clin Gastroenterol Hepatol. 2020 doi: 10.1016/j.cgh.2020.03.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, Cui X, Xiao J, Meng T, Zhou W, Liu J, Xu H. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. BioRxiv. 2020 doi: 10.1101/2020.01.30.927806. [DOI] [Google Scholar]
- 9.Opal SM. The host response to endotoxin, antilipopolysaccharide strategies, and the management of severe sepsis. Int J Med Microbiol. 2007;297(5):365–377. doi: 10.1016/j.ijmm.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 10.Munford RS. Sensing gram-negative bacterial lipopolysaccharides: a human disease determinant? Infect Immun. 2008;76(2):454–465. doi: 10.1128/IAI.00939-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danner RL, Elin RJ, Hosseini JM, Wesley RA, Reilly JM, Parillo JE. Endotoxemia in human septic shock. Chest. 1991;99(1):169–175. doi: 10.1378/chest.99.1.169. [DOI] [PubMed] [Google Scholar]
- 12.Leelahavanichkul A, Worasilchai N, Wannalerdsakun S, Jutivorakool K, Somparn P, Issara-Amphorn J, Tachaboon S, Srisawat N, Finkelman M, Chindamporn A. Gastrointestinal leakage detected by serum (1–>3)-beta-d-glucan in mouse models and a pilot study in patients with sepsis. Shock. 2016;46(5):506–518. doi: 10.1097/SHK.0000000000000645. [DOI] [PubMed] [Google Scholar]
- 13.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, Initiative S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 14.KDIGO Clinical Practice Guideline for Acute Kidney Injury (2012). Kidney Int 2:1–138
- 15.Romaschin AD, Harris DM, Ribeiro MB, Paice J, Foster DM, Walker PM, Marshall JC. A rapid assay of endotoxin in whole blood using autologous neutrophil dependent chemiluminescence. J Immunol Methods. 1998;212(2):169–185. doi: 10.1016/S0022-1759(98)00003-9. [DOI] [PubMed] [Google Scholar]
- 16.Worasilchai N, Leelahavanichkul A, Kanjanabuch T, Thongbor N, Lorvinitnun P, Sukhontasing K, Finkelman M, Chindamporn A. (1–>3)-beta-D-glucan and galactomannan testing for the diagnosis of fungal peritonitis in peritoneal dialysis patients, a pilot study. Med Mycol. 2015;53(4):338–346. doi: 10.1093/mmy/myv007. [DOI] [PubMed] [Google Scholar]
- 17.Wu L, Wen C, Qin Y, Yin H, Tu Q, Van Nostrand JD, Yuan T, Yuan M, Deng Y, Zhou J. Phasing amplicon sequencing on Illumina Miseq for robust environmental microbial community analysis. BMC Microbiol. 2015;15:125. doi: 10.1186/s12866-015-0450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bolyen E, Rideout JR, Dillon MR, Bokulich NA, Abnet C, Al-Ghalith GA, Alexander H, Alm EJ, Arumugam M, Asnicar F (2018) QIIME 2: Reproducible, interactive, scalable, and extensible microbiome data science. Peer J Preprints, [DOI] [PMC free article] [PubMed]
- 19.Rognes T, Flouri T, Nichols B, Quince C, Mahé F. VSEARCH: a versatile open source tool for metagenomics. PeerJ. 2016;4:e2584. doi: 10.7717/peerj.2584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edgar RC, Haas BJ, Clemente JC, Quince C, Knight R. UCHIME improves sensitivity and speed of chimera detection. Bioinformatics. 2011;27(16):2194–2200. doi: 10.1093/bioinformatics/btr381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeSantis TZ, Hugenholtz P, Larsen N, Rojas M, Brodie EL, Keller K, Huber T, Dalevi D, Hu P, Andersen GL. Greengenes, a chimera-checked 16S rRNA gene database and workbench compatible with ARB. Appl Environ Microbiol. 2006;72(7):5069–5072. doi: 10.1128/AEM.03006-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, Huttenhower C. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12(6):R60. doi: 10.1186/gb-2011-12-6-r60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Srisawat N, Kulvichit W, Tungsanga S, Peerapornratana S, Vorasitchai S, Tangkanakul C, Lumlertgul N, Komaenthammasophon C, Praditpornsilpa K, Tungsanga K, Eiam-Ong S. The role of neutrophil chemotaxis activity as an immunologic biomarker to predict mortality in critically-ill patients with severe sepsis. J Crit Care. 2020;56:215–221. doi: 10.1016/j.jcrc.2020.01.020. [DOI] [PubMed] [Google Scholar]
- 24.Srisawat N, Tungsanga S, Lumlertgul N, Komaenthammasophon C, Peerapornratana S, Thamrongsat N, Tiranathanagul K, Praditpornsilpa K, Eiam-Ong S, Tungsanga K, Kellum JA. The effect of polymyxin B hemoperfusion on modulation of human leukocyte antigen DR in severe sepsis patients. Crit Care. 2018;22(1):279–279. doi: 10.1186/s13054-018-2077-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koch RM, Diavatopoulos DA, Ferwerda G, Pickkers P, de Jonge MI, Kox M. The endotoxin-induced pulmonary inflammatory response is enhanced during the acute phase of influenza infection. Intensive Care Med Exp. 2018;6(1):15. doi: 10.1186/s40635-018-0182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lin E, Lowry SF. The human response to endotoxin. Sepsis. 1998;2:255–262. doi: 10.1023/A:1009890031293. [DOI] [Google Scholar]
- 27.Ruhnke M, Bohme A, Buchheidt D, Cornely O, Donhuijsen K, Einsele H, Enzensberger R, Hebart H, Heussel CP, Horger M, Hof H, Karthaus M, Kruger W, Maschmeyer G, Penack O, Ritter J, Schwartz S, Infectious Diseases Working Party in H, Oncology of the German Society for H, Oncology Diagnosis of invasive fungal infections in hematology and oncology–guidelines from the Infectious Diseases Working Party in Haematology and Oncology of the German Society for Haematology and Oncology (AGIHO) Ann Oncol. 2012;23(4):823–833. doi: 10.1093/annonc/mdr407. [DOI] [PubMed] [Google Scholar]
- 28.Netea MG, Joosten LA, van der Meer JW, Kullberg BJ, van de Veerdonk FL. Immune defence against Candida fungal infections. Nat Rev Immunol. 2015;15(10):630–642. doi: 10.1038/nri3897. [DOI] [PubMed] [Google Scholar]
- 29.Whittle E, Leonard MO, Harrison R, Gant TW, Tonge DP. Multi-Method Characterization of the Human Circulating Microbiome. Front Microbiol. 2018;9:3266. doi: 10.3389/fmicb.2018.03266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qiu J, Zhou H, Jing Y, Dong C. Association between blood microbiome and type 2 diabetes mellitus: a nested case-control study. J Clin Lab Anal. 2019;33(4):e22842. doi: 10.1002/jcla.22842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li Q, Wang C, Tang C, Zhao X, He Q, Li J. Identification and characterization of blood and neutrophil-associated microbiomes in patients with severe acute pancreatitis using next-generation sequencing. Front Cell Infect Microbiol. 2018;8:5. doi: 10.3389/fcimb.2018.00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sato J, Kanazawa A, Ikeda F, Yoshihara T, Goto H, Abe H, Komiya K, Kawaguchi M, Shimizu T, Ogihara T, Tamura Y, Sakurai Y, Yamamoto R, Mita T, Fujitani Y, Fukuda H, Nomoto K, Takahashi T, Asahara T, Hirose T, Nagata S, Yamashiro Y, Watada H. Gut dysbiosis and detection of "live gut bacteria" in blood of Japanese patients with type 2 diabetes. Diabetes Care. 2014;37(8):2343–2350. doi: 10.2337/dc13-2817. [DOI] [PubMed] [Google Scholar]
- 33.Panaiotov S, Filevski G, Equestre M, Nikolova E, Kalfin R. Cultural isolation and characteristics of the blood microbiome of healthy individuals. Adv Microbiol. 2018 doi: 10.4236/aim.2018.85027. [DOI] [Google Scholar]
- 34.Gosiewski T, Ludwig-Galezowska AH, Huminska K, Sroka-Oleksiak A, Radkowski P, Salamon D, Wojciechowicz J, Kus-Slowinska M, Bulanda M, Wolkow PP. Comprehensive detection and identification of bacterial DNA in the blood of patients with sepsis and healthy volunteers using next-generation sequencing method—the observation of DNAemia. Eur J Clin Microbiol Infect Dis. 2017;36(2):329–336. doi: 10.1007/s10096-016-2805-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wasiura J, Segal BH, Mullin KM. Cluster of Sphingomonas paucimobilis Bacteremias Linked to Diversion of Intravenous Hydromorphone. N Engl J Med. 2019;381(6):584–585. doi: 10.1056/NEJMc1902973. [DOI] [PubMed] [Google Scholar]
- 36.Bhatt AS, Marty FM, Meyerson M. Bradyrhizobium enterica in cord colitis syndrome. N Engl J Med. 2013;369(19):1867. doi: 10.1056/NEJMc1311318. [DOI] [PubMed] [Google Scholar]
- 37.Mishra D, Satpathy G, Wig N, Fazal F, Ahmed NH, Panda SK. Evaluation of 16S rRNA broad range PCR assay for microbial detection in serum specimens in sepsis patients. J Infect Public Health. 2020 doi: 10.1016/j.jiph.2020.01.007. [DOI] [PubMed] [Google Scholar]
- 38.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ, Collaboration HAS, UK, COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Arunachalam PS, Wimmers F, Mok CKP, Perera R, Scott M, Hagan T, Sigal N, Feng Y, Bristow L, Tak-Yin Tsang O, Wagh D, Coller J, Pellegrini KL, Kazmin D, Alaaeddine G, Leung WS, Chan JMC, Chik TSH, Choi CYC, Huerta C, Paine McCullough M, Lv H, Anderson E, Edupuganti S, Upadhyay AA, Bosinger SE, Maecker HT, Khatri P, Rouphael N, Peiris M, Pulendran B. Systems biological assessment of immunity to mild versus severe COVID-19 infection in humans. Science. 2020 doi: 10.1126/science.abc6261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong CK, Lam CW, Wu AK, Ip WK, Lee NL, Chan IH, Lit LC, Hui DS, Chan MH, Chung SS, Sung JJ. Plasma inflammatory cytokines and chemokines in severe acute respiratory syndrome. Clin Exp Immunol. 2004;136(1):95–103. doi: 10.1111/j.1365-2249.2004.02415.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mahallawi WH, Khabour OF, Zhang Q, Makhdoum HM, Suliman BA. MERS-CoV infection in humans is associated with a pro-inflammatory Th1 and Th17 cytokine profile. Cytokine. 2018;104:8–13. doi: 10.1016/j.cyto.2018.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hanada S, Pirzadeh M, Carver KY, Deng JC. Respiratory Viral Infection-Induced Microbiome Alterations and Secondary Bacterial Pneumonia. Front Immunol. 2018;9:2640. doi: 10.3389/fimmu.2018.02640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jin X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, Hao SR, Jia HY, Cai H, Zhang XL, Yu GD, Xu KJ, Wang XY, Gu JQ, Zhang SY, Ye CY, Jin CL, Lu YF, Yu X, Yu XP, Huang JR, Xu KL, Ni Q, Yu CB, Zhu B, Li YT, Liu J, Zhao H, Zhang X, Yu L, Guo YZ, Su JW, Tao JJ, Lang GJ, Wu XX, Wu WR, Qv TT, Xiang DR, Yi P, Shi D, Chen Y, Ren Y, Qiu YQ, Li LJ, Sheng J, Yang Y. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020 doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, Fang Z, Gu Z, Gao L, Shi H, Mai L, Liu Y, Lin X, Lai R, Yan Z, Li X, Shan H. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020 doi: 10.1136/gutjnl-2020-321013. [DOI] [PubMed] [Google Scholar]
- 45.Ng SC, Tilg H. COVID-19 and the gastrointestinal tract: more than meets the eye. Gut. 2020;2020:321195. doi: 10.1136/gutjnl-2020-321195. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. EAA laboratory specification manual.
Additional file 2. BG laboratory specification manual.
Additional file 3: Table S1. Clinical characteristics of COVID-19 pneumonia. Table S2. Cytokines level on day 1, day 3, and day 7 stratified by ICU admission status.
Additional file 4: Figure S1. Rarefaction curve of pass-filter reads obtained from each sample. Figure S2. Dynamic bacterial community profiles on day 1, day 3, and day 7. Figure S3. Dynamic bacterial community profiles at the phylum level in COVID-19 patients. Figure S4. Shannon diversity index (A) and Chao1 richness (B) representing alpha diversity of bacterial community profiles in COVID-19 patients on day 1, 3, and 7. The Shannon diversity index was not significant differences among the date of onsets whereas the Chao1 richness was significant (P < 0.05) between the first and third date of onsets Figure S5. LEfSe analysis of bacteria on day 1 and day 3. Figure S6. Wilcoxon matched pairs test differential abundant of bacterial genera in each COVID-19 patient between day 1 and day 3. The bacterial genera including Sphingomonas and Sediminibacterium were significantly (P < 0.05) higher in the third date compared to the first of onset whereas Comamonas, Acinetobacter and Pseudomonas were significantly (P < 0.05) decreased during the third date of onsets. Figure S7. Comparison of EAA level (Figure S7a) and BG (Figure S7b) between COVID-19 and other type of infections using data from our previous studies in 136 severe sepsis or septic shock patients.
Data Availability Statement
On reasonable request, data from this study are available from the corresponding author.