Abstract
Background: The COVID-19 pandemic is an emerging concern regarding the potential adverse effects during pregnancy. This study reviews knowledge on the impact of COVID-19 on pregnancy and describes the outcome of published cases of pregnant women diagnosed with COVID-19.
Methods: Searches were conducted in PubMed®, Scopus®, Web of Science®, and MedRxiv® up to 26th June 2020, using PRISMA standards, to identify original published studies describing pregnant women at any gestational age diagnosed COVID-19. There were no date or language restrictions on the search. All identified studies were included irrespective of assumptions on study quality.
Results: We identified 161 original studies reporting 3,985 cases of pregnant women with COVID-19 (1,007 discharged while pregnant). The 2,059 published cases with pregnancy outcomes resulted in 42 abortions, 21 stillbirths, and 2,015 live births. Preterm birth occurred in 23% of cases. Around 6% of pregnant women required admission to an intensive care unit and 28 died. There were 10 neonatal deaths. From the 163 cases with amniotic fluid, placenta, and/or cord blood analyzed for the SARS-CoV-2 virus, 10 were positive. Sixty-one newborns were positive for SARS-CoV-2. Four breast milk samples from 92 cases showed evidence of SARS-CoV-2.
Conclusion: Emerging evidence suggests that vertical transmission is possible, however, there is still a limited number of reported cases with intrapartum samples. Information, counseling and adequate monitoring are essential to prevent and manage adverse effects of SARS-CoV-2 infection during pregnancy.
Keywords: COVID-19, pregnancy, vertical transmission, perinatal outcomes, breastfeeding
Introduction
The disease resulting from infection with the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-COV-2) and designated COVID-19 by the World Health Organization (WHO) was first identified in humans in December 2019, in the city of Wuhan, China (1), and can present from asymptomatic to a severe acute respiratory infection requiring intensive care (2, 3). The infection can occur at any age, but COVID-19 is proportionally uncommon in children (<1% of the total cases). The infection fatality rate is around 1% but much higher in older people or those with pre-existing medical conditions (such as heart disease, diabetes, chronic obstructive pulmonary disease) (2, 4).
Person-to-person transmission of COVID-19 is well-established and can occur when an infected person coughs, sneezes, or speaks and scattered droplets are inhaled or reach the mucous membranes of the mouth, nose, or eyes of susceptible. COVID-19 can also be transmitted through direct hand contact with surfaces or objects contaminated with SARS-CoV-2 followed by contact with the mouth, nose, or eyes (2).
Pregnant women and newborns receive special attention and there is an emerging concern with the potential risk of SARS-COV-2 vertical transmission (from mother to fetus) or associated malformations, and contagion during delivery and breastfeeding; likewise, it is important to determine the potential adverse effects of COVID-19 in pregnant women (5–7). Considering the rapidly evolving of the COVID-19 pandemic, which is reflected in the current lack of high-quality evidence, we aimed to review the published cases of pregnant women diagnosed with COVID-19.
Methods
The review follows the Preferred Reporting of Systematic Reviews and Meta-Analysis (PRISMA) guidelines (8, 9). This review was not registered with PROSPERO. We searched PubMed®, Scopus®, Web of Science®, and MedRxiv® electronic databases up to 26th June 2020 to identify original published studies describing pregnant women at any gestational age diagnosed with COVID-19 [confirmed by clinical/radiological evidence of pneumonia compatible with SARS-CoV-2 and/or by quantitative real-time polymerase chain reaction (PCR) or dual fluorescence PCR of SARS-CoV-2 infection]. The following search expression was used [(COVID-19 OR 2019-nCoV OR “novel coronavirus” OR SARS-CoV-2 OR “coronavirus 2”) AND (pregnancy OR delivery OR pregnant OR obstetric* OR maternal OR perinatal OR breastfeeding)]. Also, reference tracking was carried out to identify other potential studies to be included.
The PECO (Population, Exposure, Comparison, Outcome) structure design was used to define exposure, outcome, as well as inclusion and exclusion criteria for the review (Table 1). The question was “What are the main obstetric, maternal, and neonatal outcomes of SARS-CoV-2 infection during pregnancy and the potential risk of vertical transmission?”
Table 1.
PECO criteria for inclusion and exclusion of studies.
| Parameter | Inclusion criteria | Data extraction |
|---|---|---|
| Population (P) | Pregnant women at any gestational age | Country, maternal age, gestational age at birth (or at admission), comorbidities |
| Exposure (E) | COVID-19 diagnose | SARS-CoV-2 infection |
| Comparison (C) | None | |
| Outcome (O) | Pregnancy, maternal, and neonatal outcomes | Pregnancy complications, type of delivery, indication for cesarean section, maternal admission to intensive care unit, maternal death, birth weight, neonatal complications, breastfeeding, intrauterine, and/or neonatal samples collected for detection of SARS-CoV-2 |
Each reference retrieved was screened independently by two researchers following predefined criteria to determine eligibility for the systematic review. Studies were excluded if: (1) did not involve humans (e.g., in vitro or animal research); (2) non-original articles (e.g., book chapters, review articles, guidelines); (3) data not reporting pregnant women diagnosed with COVID-19; (4) only indicate prevalence estimations among pregnant women, with no description of perinatal outcomes; and (5) reporting breastfeeding after puerperium period, with no information about pregnancy. There were no date or language restrictions on the search.
Two researchers independently reviewed the included studies and extracted the following data: type of study, data collection period, maternal age, comorbidities and pregnancy complications, type of delivery, indication for cesarean section, gestational age at birth (or at admission or diagnosis), pregnancy outcome, maternal admission to intensive care unit (including mechanical ventilation), maternal death, neonatal outcomes (birth weight, neonatal complications, neonatal death, breastfeeding), intrauterine and/or neonatal samples collected for detection of SARS-CoV-2 (such as amniotic fluid, umbilical cord blood, placenta, breast milk, nasopharyngeal, and anal swabs), and their results (negative/positive and/or reactive/non-reactive).
All identified original observational studies reporting cases of pregnant women at any gestational age diagnosed with COVID-19 were included irrespective of study quality (preprints preliminary reports were also included). The research design of the studies was described based on the authors' classification, except for case reports which were considered when the manuscript described only one case.
Doubts on possible duplicates and/or differences in the data extraction were discussed and resolved by consensus, involving a third researcher whenever necessary.
Cases reported in more than one study, and for which it was possible to identify duplicates, were described only once, presenting the more detailed data. We identified duplicates based on author names and hospital location, publication date, participant admission date, maternal and neonatal characteristics, and outcomes. We did not contact the corresponding authors because of the time constraints and the importance to have immediate results.
Considering the heterogeneity observed across the studies, we decided to perform a narrative synthesis using the Synthesis Without Meta-analysis (SWiM) reporting guideline (intended to complement the PRISMA guidelines) (10). Descriptive statistics were presented (frequency and proportions) based on the total cases with available information.
Results
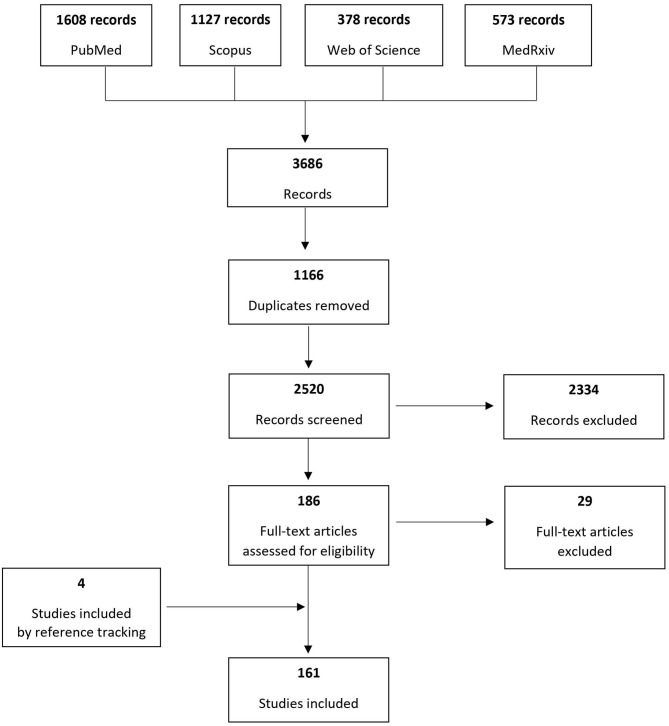
Based on the search of the four electronic databases, 3,686 records were identified and after removing duplicates 2,520 were screened to assess their eligibility for inclusion. One hundred sixty-one original studies published until June 26th, 2020 were included, reporting cases of pregnant women at any gestational age diagnosed with COVID-19. Figure 1 presents the process of study inclusion in the systematic review.
Figure 1.
Systematic review flowchart.
From the 161 studies included, 66 were case series reports (48% from China and 23% from USA) (11–76), 59 case reports (27% from China and 25% from USA) (77–135), 20 cohort studies (30% from China, 30% from USA, 15% from Spain) (136–155), 13 cross-sectional (62% China and 15% USA) (156–168), and 3 case-control studies (2 from China and 1 from Italy) (169–171). Table 2 shows the distribution of studies according to the study design.
Table 2.
Distribution of references included in the review by study design and country.
| Designa | Country | Number of reports (n = 161) |
|---|---|---|
| Case report (n = 59) | ||
| Australia | 1 | |
| Belgium | 1 | |
| Canada | 1 | |
| China | 16 | |
| France | 1 | |
| Germany | 1 | |
| Honduras | 1 | |
| India | 1 | |
| Iran | 2 | |
| Italy | 3 | |
| Jordan | 1 | |
| Korea | 1 | |
| Netherlands | 2 | |
| Peru | 1 | |
| Portugal | 2 | |
| Spain | 1 | |
| Sweden | 1 | |
| Switzerland | 1 | |
| Thailand | 1 | |
| Turkey | 2 | |
| UK | 3 | |
| USA | 15 | |
| Case series reports (n = 66) | ||
| Brazil | 1 | |
| Canada | 1 | |
| China | 32 | |
| France | 2 | |
| India | 1 | |
| Iran | 1 | |
| Italy | 5 | |
| Mexico | 1 | |
| Portugal | 1 | |
| Spain | 3 | |
| Turkey | 1 | |
| UK | 2 | |
| USA | 15 | |
| Case-control (n = 3) | ||
| China | 2 | |
| Italy | 1 | |
| Cross-sectional (n = 13) | ||
| China | 8 | |
| Italy | 1 | |
| Japan | 1 | |
| Sweden | 1 | |
| USA | 2 | |
| Cohort (n = 20) | ||
| China | 6 | |
| Denmark | 1 | |
| Israel | 1 | |
| Italy | 2 | |
| Spain | 3 | |
| UK | 1 | |
| USA | 6 |
The studies' design was reported according to the authors' classification, except for case reports which were considered only when the paper described 1 case.
The studies reported 3,985 pregnant women diagnosed with COVID-19 and the main characteristics are summarized in the Table 3. A detailed description of reported cases is presented in Supplementary Table 1.
Table 3.
Characteristics of pregnant women diagnosed with COVID-19 described in the literature (n = 3985).
| Characteristics | n/N (%) |
|---|---|
| Maternal characteristics | |
| Age, years (min-max) | 15–49 |
| Country of hospital admission | |
| United States of America | 1206/3985 (30.26) |
| China | 823/3985 (20.65) |
| France | 672/3985 (16.86) |
| UK | 440/3985 (11.04) |
| Mexico | 308/3985 (7.73) |
| Spain | 241/3985 (6.05) |
| Italy | 202/3985 (5.07) |
| Portugal | 14/3985 (0.35) |
| Sweden | 14/3985 (0.35) |
| Denmark | 13/3985 (0.33) |
| Israel | 11/3985 (0.28) |
| Iran | 11/3985 (0.28) |
| Turkey | 10/3985 (0.25) |
| India | 3/3985 (0.08) |
| Brazil | 2/3985 (0.05) |
| Canada | 2/3985 (0.05) |
| Japan | 2/3985 (0.05) |
| Netherlands | 2/3985 (0.05) |
| Australia | 1/3985 (0.03) |
| Belgium | 1/3985 (0.03) |
| Germany | 1/3985 (0.03) |
| Honduras | 1/3985 (0.03) |
| South Korea | 1/3985 (0.03) |
| Jordan | 1/3985 (0.03) |
| Peru | 1/3985 (0.03) |
| Switzerland | 1/3985 (0.03) |
| Thailand | 1/3985 (0.03) |
| Pregnancy complications | |
| Gestational diabetes | 179/3985 (4.49) |
| PROM/PPROM | 108/3985 (2.71) |
| Preeclampsia/Eclampsia/ HELLP Syndrome | 68/3985 (1.71) |
| Fetal distress | 44/3985 (1.10) |
| Gestational hypertension | 23/3985 (0.58) |
| Fetal growth restriction | 17/3985 (0.43) |
| Placenta previa/ placental abruption/ placenta accreta | 15/3985 (0.38) |
| Oligohydramnios/Polyhydramnios | 7/3985 (0.18) |
| Chronic diseases of pregnant women | |
| Obesity | 530/3985 (13.30) |
| Asthma | 117/3985 (2.94) |
| Chronic hypertension | 73/3985 (1.83) |
| Diabetes mellitus | 68/3985 (1.71) |
| Hypothyroidism | 26/3985 (0.65) |
| Pregnancy status | |
| Still pregnant at discharge | 1007/3985 (25.27) |
| Pregnancy outcome available (delivered and/or abortion) | 2090/3985 (52.45) |
| No information about pregnancy status | 888/3985 (22.28) |
| Pregnancy outcomes (number of fetus/pregnant women) | |
| No information | 31/2090 (1.48) |
| Voluntary termination of pregnancy | 16/2059 (0.78) |
| Medical termination of pregnancy | 5/2059 (0.24) |
| Spontaneous abortion/fetal demise/ectopic pregnancy (<20 weeks of gestation) |
42/2059 (2.04) |
| Stillbirth (≥20 weeks of gestation; including 1 twin pregnancy) | 21/2059 (1.02) |
| Live birth (including 38 twin pregnancies and 1 triple) | 2015/2059 (97.86) |
| Cesarean section (among delivered pregnant women) | 1127/2090 (53.92) |
| Preterm birth (<37 weeks of gestation) (among live birth delivered) | 455/1975 (23.04) |
| Maternal outcomes | |
| Maternal deaths | 28/3803 (0.74) |
| Maternal admission to Intensive/Critical Care Unit | 215/3365 (6.39) |
| Maternal mechanical ventilation (invasive and/or non-invasive) | 160/2972 (5.38) |
| ECMO | 5/2972 (0.50) |
| Neonatal outcomes (live births, n = 2015) | |
| Neonatal deaths | 10/1755 (0.57) |
| Any neonatal positive sample for SARS-CoV-2 confirmed by RT-PCR (newborns with at least one sample positive) |
61/2015 (3.03) |
| High levels of SARS-CoV-2 IgM antibodies in neonatal blood | 4/2015 (0.20) |
The majority of cases occurred in the USA (n = 1,206, 30%), China (n = 823, 21%), France (n = 672, 17%), UK (n = 440, 11%), Mexico (n = 308, 8%), Spain (n = 241, 6%), and Italy (n = 202, 5%). Maternal age ranged from 15 to 49 years.
From the 3,985 pregnant women described, 2090 (52.4%) had a pregnancy outcome, 1007 (25.3%) were discharged during pregnancy (undelivered) and 888 (22.3%) had no information. From those with available information on gestational age (n = 1,896), 89% of women were in the third trimester of pregnancy (n = 1,685) and only 5% in the first trimester (n = 101).
Vertical Transmission of COVID-19
Among the intrauterine samples analyzed, 11.9% of placentas (n = 8/67), 1.8% of amniotic fluid (n = 1/54), and 2.4% umbilical cord blood (n = 1/42) were positive for SARS-CoV-2 virus (Table 4).
Table 4.
Type of intrauterine/ neonatal samples collected and results.
| Type of samples | n/N* (%) |
|---|---|
| Intrauterine samples | |
| Placenta | 67 |
| Positive results | 8 (11.94) |
| Amniotic fluid | 54 |
| Positive results | 1 (1.85) |
| Umbilical cord blood | 42 |
| Positive results | 1 (2.38) |
| Measurement of SARS-CoV-2 IgM and IgG antibody in umbilical cord blood | 2 |
| Reactive IgM | 0 (0.0) |
| Reactive IgG | 1 (50.0) |
| Neonatal samples | |
| RT-PCR newborn's samples (not specified) | 648 |
| Positive results | 19 (2.93) |
| RT-PCR newborn's oral swabs | 1045 |
| Positive results | 36 (3.44) |
| RT-PCR newborn's anal swabs | 38 |
| Positive results | 5 (13.16) |
| RT-PCR newborn's blood | 20 |
| Positive results | 1 (5.00) |
| Measurement of SARS-CoV-2 IgM and IgG antibody in newborn's blood | 71 |
| Reactive IgM | 4 (5.63) |
| Reactive IgG | 7 (9.86) |
| RT-PCR breast milk | 92 |
| Positive results | 4 (4.35) |
| Measurement of SARS-CoV-2 IgM and IgG antibody in breast milk | 7 |
| Reactive IgM | 5 (71.43) |
| Reactive IgG | 0 (0.0) |
Newborns with at least one sample tested.
We identified 61 (3.0%) newborns with at least one positive sample for SARS-CoV-2 confirmed by real-time reverse transcription-polymerase chain reaction (RT-PCR) (Table 3). Most studies detected the SARS-CoV-2 RNA by RT-PCR using samples from the newborn's nasopharyngeal or throat (n = 1,045), sample collection varying from immediately to 17 days after birth. Neonatal serum samples were tested in 71 newborns, being four reactive for IgM and seven for IgG (Table 4).
From the 92 newborns with at least one breast milk sample tested (sample collection varying from immediately after birth to 15 days after), 4 were positive for SARS-CoV-2 virus by RT-PCR and 5 reactive for IgM antibodies (Table 4). One study reported 3 out of 5 positive breast milk samples collected during the first 5 days after birth, neonatal nasopharyngeal samples were negative on day 1 and 5 and the newborn received expressed breast milk (15).
Maternal and Neonatal Outcomes
The obstetric conditions most frequently reported were gestational diabetes (4.5%), premature rupture of membranes (PROM/PPROM) (2.7%), pre-eclampsia/eclampsia/HELLP syndrome (1.7%), fetal distress (1.1%), gestational hypertension (0.6%), fetal growth restriction (0.4%), placenta previa/placental abruption/ placenta accreta (0.4%), and oligohydramnios/polyhydramnios (0.2%) (Table 3). The included studies reported 13.3% of obesity among pregnant women with COVID-19, 2.9% of asthma, 1.8% of chronic hypertension, and 1.7% of diabetes mellitus (Table 3).
Two hundred and fifteen pregnant women required admission to an intensive care unit (6.4%), 5.4% were mechanically ventilated (n = 160), and 0.5% required ECMO (n = 15). Twenty-eight maternal deaths with COVID-19 were reported (0.7%).
Among 2,059 pregnant women with pregnancy outcomes available, 16 (0.8%) resulted in termination of pregnancy due to maternal concerns regarding COVID-19 and 5 (0.2%) by medical reasons; 42 (2.0%) were spontaneous abortions/fetal demise (<20 weeks of gestation), 21 (1.0%) stillbirths (≥20 weeks of gestation, including one twin pregnancy); and 2015 (97.9%) live births (including 38 twin pregnancies and one triple pregnancy). Cesarean section was the most common type of delivery: 53.9% among 2,090 delivered pregnant women. Preterm birth occurred in 23.0% (455/1975) among live birth delivered and with available information on gestational age. Most of preterm births were iatrogenic for maternal and/or fetal compromise. There were 10 neonatal deaths (0.6%).
Although most of breast milk samples from COVID-19 infected mothers have tested negative for the SARS-CoV-2 virus, most infants did not receive any breast milk, considering those with available information (59.9%, n = 227/379).
Discussion
Worldwide, the incidence of infection in pregnant women at any gestational age is still unclear, as universal screening tests are not generally used, except in the presence of symptoms or at admission for delivery. In a New York's hospital that implemented SARS-CoV-2 testing in all pregnant women admitted for delivery, 15.4% of them were positive for SARS-CoV-2, but 87.9% were asymptomatic (172).
The clinical characteristics of COVID-19 were similar to those described in non-pregnant women, presenting mild or moderate symptoms (11, 19, 21, 32, 76, 160). A systematic review summarized the clinical manifestations of 108 pregnant women with confirmed COVID-19 and most of them presented fever (68%) and coughing (34%), and lymphocytopenia (59%) with elevated C-reactive protein (70%) (173).
Furthermore, pregnant women do not appear to be at increased risk of severe illness of SARS-CoV-2 infection compared with non-pregnant women in the general population (6, 145, 174). However, a study from Sweden suggests that the risk of being admitted to an intensive care unit may be higher in pregnant and postpartum women (n = 13) compared with non-pregnant women of similar age (n = 40) (156). Recently, the Centers for Disease Control and Prevention (CDC) COVID-19 surveillance indicates an increased risk of intensive care unit admissions (1 in 68 of pregnant vs. 1 in 110 non-pregnant women, crude risk ratio 1.6, 95% CI 1.3–1.9) and mechanical ventilation (1 in 195 of pregnant vs. 1 in 370 non-pregnant women, crude risk ratio 1.9, 95% CI 1.4–2.6), but no increase was observed in the rate of mortality (1 in 513 of pregnant vs. 1 in 400 of non-pregnant women, crude risk ratio 0.8, 95% CI 0.5–1.3) (175). However, a more severe presentation of COVID-19 is commonly described in pregnant women with chronic conditions, such as obesity, asthma, and diabetes (174).
Although most of the published cases confirm the absence of transmission of the SARS-CoV-2 virus antenatally or intrapartum, emerging evidence suggests that vertical transmission is possible (28, 30, 75, 77, 82, 151). However, this is still controversial due to a reduced number of reported cases with intrapartum samples (placenta, amniotic fluid, umbilical cord blood), large variability in the type of biological material analyzed and the time of its collection. Results from our review reveal that only 7.8% of women with pregnancy outcome had at least one intrauterine sample analyzed (n = 163/2090). If vertical transmission occurred in all the positive cases reported, the proportion of neonatal infection would be around 6.1% (n = 10/163). It is important to highlight that only two studies (one from Italy and another from Canada) reported three cases with positive RT-PCR for SARS-CoV-2 simultaneously on placenta and neonatal nasopharyngeal swabs samples (51, 97). Two of these neonates had positive samples collected at birth. Additionally, one termination of pregnancy and one miscarriage presented positive placental samples, without evidence of fetal SARS-CoV-2 infection (106, 121). Two studies also used maternal and neonatal serum samples to test for immunoglobulins M (IgM) and G (IgG) antibodies (30, 77). In a series of six cases that had blood collected after delivery evaluated, two of the newborns had high levels of IgG and IgM antibodies (>10 AU/mL) and three had high values of IgG antibodies with normal levels of IgM, but in none SARS-CoV-2 virus was detected by RT-PCR in the neonatal oropharyngeal exudate (30). A case study also reported high values of IgM and IgG antibodies in the newborn's blood at days 1 and 15 after delivery, but with RT-PCR for SARS-CoV-2 negative in five samples of nasopharyngeal exudates collected between the first 2 h and the 16th day of life (77).
Regarding the effect of the SARS-CoV-2 virus on the fetus, no congenital malformation has been reported so far associated to COVID-19. Higher risk of preterm birth has been reported as we observed 23% of preterm birth in our review compared to the estimated global preterm birth rate that is around 10–15% (176). In one study that compared groups of pregnant women with and without COVID-19, there were no significant differences in the occurrence of gestational diabetes, severe pre-eclampsia, PROM, fetal distress, meconium-stained amniotic fluid, premature delivery, neonatal asphyxia, and procedures for severe post-partum bleeding (31).
The maternal and neonatal outcomes observed so far are quite different from the two most serious coronavirus-related previous epidemics (6, 177–190). The first also appeared in China, in 2002-03, and was characterized by severe respiratory infections caused by the Severe Acute Respiratory Syndrome-Coronavirus (SARS-CoV) . The second occurred in 2012, initially in the Middle East, the Middle East Respiratory Syndrome—Coronavirus (MERS-CoV) (6, 177). These epidemics have demonstrated the ability of coronavirus to cause serious complications during pregnancy (179, 190), with worse prognosis in pregnant women than non-pregnant women (181, 191).
In the 2002 epidemic, 12 pregnant women were infected with SARS-CoV, with a fatality rate of 25% (190). Among the seven pregnant women infected in the first trimester, four had a miscarriage (190). Two of the five pregnant women infected during the second or third trimester had fetal growth restriction and four had a preterm delivery (one spontaneous; three induced by the maternal condition) (190). In a review of the pregnancy outcomes of 11 women infected with MERS-CoV, seven pregnant women required admission to the intensive care unit and three died, of which only one had one comorbidity (asthma). Two fetal deaths occurred, and three of nine newborns were preterm (179).
However, considering that SARS-CoV-2 has genetic homology and some clinical similarities to SARS-CoV and MERS-CoV, and the immunological and physiological changes that occur during pregnancy, such as in cell-mediated immunity or lung function, that affect both the susceptibility and the clinical severity of pneumonia, it is important to pay particular attention to the monitoring of pregnant women with COVID-19, because maternal and perinatal adverse outcomes are potentially relevant (6, 177). One study reported two asymptomatic pregnant women at admission for delivery that rapidly evolved to severe COVID-19 disease requiring admission to an intensive care unit (14). Also, we identified 28 maternal deaths, with an infection fatality rate less than 1%, being similar to the other general populations (4). One article from Iran reported seven maternal deaths among nine pregnant women with severe COVID-19, of which three resulted in four stillbirths (1 twin pregnancy) and one in two neonatal deaths (1 twin pregnancy) (41). After concluding our search on the electronic databases, a paper from Brazil reporting 124 maternal deaths of pregnant or postpartum women was published, describing 22.6% admissions to the intensive care unit, of whom 64% had invasive ventilation (192). This raises awareness for questions related to access to healthcare services which may impact on the natural history of disease and reflect worldwide disparities on maternal outcomes.
Thus, it is essential to prevent the infection of COVID-19 and any other viral respiratory infection, as these infections represent an increased risk for the pregnant woman and for the pregnancy itself (6, 193, 194). It is therefore extremely important that pregnant women adopt preventive actions for COVID-19 with great intensity (174). For managing suspected or confirmed SARS-CoV-2 infection in pregnant women, recommendations for health professionals and services have already been published (174, 193, 195–197).
Most women in this review had a cesarean section, many of them without a clear medical indication. The decision on the type of delivery in pregnant women with suspected or confirmed infection with COVID-19 should consider maternal and fetal clinical characteristics, as in normal practice, and not the diagnosis of COVID-19 infection per se. Thus, there is no obstetric contraindication to any mode of delivery, unless the pregnant woman's clinical condition implies an emergent decision (174).
Regarding breast milk samples, the reviewed studies described four cases with evidence of SARS-CoV-2, from the 92 reported (15, 74, 97, 148). Despite that, there is not enough scientific evidence to unequivocally state that there is possibility that mothers with COVID-19 can transmit the virus through breast milk. Therefore, recommendations should be based on the available data and the analogy with past circumstances and predictable costs and benefits. Breastfeeding is recognized as the best form of child feeding due to the countless benefits for both the mother and the newborn, including the protection against gastrointestinal and respiratory infections (198). Thus, considering the benefits of breastfeeding and the fact that the transmission of other respiratory viruses is insignificant through breast milk, there is no indication to stop breastfeeding. According to the recommendations of WHO/UNICEF (199) and the Center for Disease Control and Prevention (CDC) of the United States (193), women with suspected or confirmed infection with COVID-19 can initiate or continue breastfeeding as long as clinical conditions permit. The CDC indicates that the decision to initiate or continue breastfeeding must be determined by the mother with COVID-19, together with family members and health professionals (193).
The major strength of this review is the inclusion of all study designs, including case reports and case series. To the best of our knowledge, this is the first review presenting a detailed description of clinical outcomes of each case identified (Supplementary Table 1). Limitations of this systematic review should be acknowledged. Considerable heterogeneity was observed across the studies, which did not allow us to conduct a meta-analysis. On the other hand, we cannot guarantee that we were able to identify all the cases of pregnant women described in the literature. Possibly there were additional cases currently presented in other types of publications, such as reports. Also, considering the importance of summarizing all existing cases, we did not assess the quality of the studies included in this review. Several studies had missing outcome data and selective reporting bias could not be excluded. Additionally, there may be some cases which could be duplicated, namely the studies which did not describe clinical characteristics case by case.
Conclusion
According to this review, preterm delivery seems to be more frequent among pregnant women with COVID-19. There is emerging evidence on possible vertical transmission (three positive results simultaneously in the placental samples and neonatal oral swabs for SARS-CoV-2 were reported), but the clinical relevance of the fetal infection is unclear. So far, there is not enough scientific evidence to unequivocally state that there is possibility that mothers with COVID-19 can transmit the virus through breast milk.
The maternal fatality rate was below 1% among the reported cases and hospitalizations in intensive care were less than 7%. Although the complications appear to be similar to those of non-pregnant women, services must be prepared to attend to complications, especially in pregnant women with comorbidities. Information, counseling and adequate monitoring are essential to prevent and manage adverse effects of SARS-CoV-2 infection during pregnancy.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author/s.
Author Contributions
CR and HB: conceptualization, methodology, data curation, and original draft preparation. IB and RD: methodology, data curation, writing-reviewing, and editing. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This manuscript has been released as a preprint at MedRxiv Rodrigues et al. (200). The authors acknowledge the contribution of Ana Alfredo, Anzhela Sorokina, and Pedro Pimenta to data extraction.
Footnotes
Funding. This study was funded by national funding from the Foundation for Science and Technology - FCT, under the Unidade de Investigação em Epidemiologia - Instituto de Saúde Pública da Universidade do Porto (EPIUnit) (UIDB/04750/2020); the PhD Grant SFRH/BD/111794/2015 (CR) was co-funded by the FCT and the POCH/FSE Program.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.558144/full#supplementary-material
References
- 1.Hui DS, Azhar EI, Madani TA, Ntoumi F, Kock R, Dar O, et al. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health - The latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. (2020) 91:264–6. 10.1016/j.ijid.2020.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caldas J, Tavares M. Epidemiologia da COVID-19 [Online]. Available online at: http://asset.youoncdn.com/ab296ab30c207ac641882479782c6c34/070b44658f5569888804a14826ae273c.pdf (accessed April 13, 2020).
- 3.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. (2020) 395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Russell TW, Hellewell J, Jarvis CI, van Zandvoort K, Abbott S, Ratnayake R, et al. Estimating the infection and case fatality ratio for coronavirus disease (COVID-19) using age-adjusted data from the outbreak on the Diamond Princess cruise ship, February 2020. Euro Surveill. (2020) 25:2000256. 10.2807/1560-7917.ES.2020.25.12.2000256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qiao J. What are the risks of COVID-19 infection in pregnant women? Lancet. (2020) 395:760–2. 10.1016/S0140-6736(20)30365-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rasmussen SA, Smulian JC, Lednicky JA, Wen TS, Jamieson DJ. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol. (2020) 222:415–26. 10.1016/j.ajog.2020.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Favre G, Pomar L, Musso D, Baud D. 2019-nCoV epidemic: what about pregnancies? Lancet. (2020) 395:e40 10.1016/S0140-6736(20)30311-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. (2009) 6:e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. (2015) 4:1. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. (2020) 368:l6890. 10.1136/bmj.l6890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. (2020) 395:809–15. 10.1016/S0140-6736(20)30360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baergen RN, Heller DS. Placental pathology in Covid-19 positive mothers: preliminary findings. Pediatr Dev Pathol. (2020) 23:177–80. 10.1177/1093526620925569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Breslin N, Baptiste C, Gyamfi-Bannerman C, Miller R, Martinez R, Bernstein K, et al. COVID-19 infection among asymptomatic and symptomatic pregnant women: Two weeks of confirmed presentations to an affiliated pair of New York City hospitals. Am J Obstet Gynecol MFM. (2020) 2:100118 10.1016/j.ajogmf.2020.100118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Breslin N, Baptiste C, Miller R, Fuchs K, Goffman D, Gyamfi-Bannerman C, et al. Coronavirus disease 2019 in pregnancy: early lessons. Am J Obstet Gynecol MFM. (2020) 2:100111. 10.1016/j.ajogmf.2020.100111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buonsenso D, Costa S, Sanguinetti M, Cattani P, Posteraro B, Marchetti S, et al. Neonatal late onset infection with severe acute respiratory syndrome coronavirus 2. Am J Perinatol. (2020) 37:869–72. 10.1055/s-0040-1710541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell KH, Tornatore JM, Lawrence KE, Illuzzi JL, Sussman LS, Lipkind HS, et al. Prevalence of SARS-CoV-2 among patients admitted for childbirth in Southern Connecticut. JAMA. (2020) 323:2520–2. 10.1001/jama.2020.8904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cao D, Yin H, Chen J, Tang F, Peng M, Li R, et al. Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: a retrospective study. Int J Infect Dis. (2020) 95:294–300. 10.1016/j.ijid.2020.04.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen L, Li Q, Zheng D, Jiang H, Wei Y, Zou L, et al. Clinical characteristics of pregnant women with Covid-19 in Wuhan, China. N Engl J Med. (2020) 382:e100. 10.1056/NEJMc2009226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen R, Zhang Y, Huang L, Cheng BH, Xia ZY, Meng QT. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can J Anaesth. (2020) 67:655–63. 10.1007/s12630-020-01630-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen S, Huang B, Luo DJ, Li X, Yang F, Zhao Y, et al. [Pregnancy with new coronavirus infection: clinical characteristics and placental pathological analysis of three cases]. Zhonghua Bing Li Xue Za Zhi. (2020) 49:418–23. 10.3760/cma.j.cn112151-20200225-00138 [DOI] [PubMed] [Google Scholar]
- 21.Chen S, Liao E, Cao D, Gao Y, Sun G, Shao Y. Clinical analysis of pregnant women with 2019 novel coronavirus pneumonia. J Med Virol. (2020). 10.1002/jmv.25789. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen X, Li Y, Wang J, Cai H, Cao H, Sheng J. [Pregnant women complicated with COVID-19: a clinical analysis of 3 cases]. Zhejiang Da Xue Xue Bao Yi Xue Ban. (2020) 49:240–4. 10.3785/j.issn.1008-9292.2020.03.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooke WR, Billett A, Gleeson S, Jacques A, Place K, Siddall J, et al. SARS-CoV-2 infection in very preterm pregnancy: experiences from two cases. Eur J Obstet Gynecol Reprod Biol. (2020) 250:259–60. 10.1016/j.ejogrb.2020.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doria M, Peixinho C, Laranjo M, Mesquita Varejao A, Silva PT. Covid-19 during pregnancy: a case series from an universally tested population from the north of Portugal. Eur J Obstet Gynecol Reprod Biol. (2020) 250:261–2. 10.1016/j.ejogrb.2020.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fan C, Lei D, Fang C, Li C, Wang M, Liu Y, et al. Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis. (2020). 10.1093/cid/ciaa226. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fox NS, Melka S. COVID-19 in pregnant women: case series from one large New York City obstetrical practice. Am J Perinatol. (2020) 37:1002–4. 10.1055/s-0040-1712529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu D, Li L, Wu X, Zheng D, Wang J, Yang L, et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. AJR Am J Roentgenol. (2020) 215:127–32. 10.2214/AJR.20.23072 [DOI] [PubMed] [Google Scholar]
- 28.Liu W, Wang Q, Zhang Q, Chen L, Chen J, Zhang B, et al. Coronavirus disease 2019 (COVID-19) during pregnancy: a case series. Preprints. (2020) 2020020373. Available online at: https://www.preprints.org/manuscript/202002.0373/v1
- 29.Luo Y, Yin K. Management of pregnant women infected with COVID-19. Lancet Infect Dis. (2020) 20:513–4. 10.1016/S1473-3099(20)30191-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zeng H, Xu C, Fan J, Tang Y, Deng Q, Zhang W, et al. Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA. (2020) 323:1848–9. 10.1001/jama.2020.4861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang L, Jiang Y, Wei M, Cheng BH, Zhou XC, Li J, et al. [Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province]. Zhonghua Fu Chan Ke Za Zhi. (2020) 55:166–71. 10.3760/cma.j.cn112141-20200218-00111 [DOI] [PubMed] [Google Scholar]
- 32.Zhu H, Wang L, Fang C, Peng S, Zhang L, Chang G, et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr. (2020) 9:51–60. 10.21037/tp.2020.02.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Amorim MMR, Soligo Takemoto ML, Fonseca EBD. Maternal deaths with coronavirus disease 2019: a different outcome from low- to middle-resource countries? Am J Obstet Gynecol. (2020) 223:298–9. 10.1016/j.ajog.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andrikopoulou M, Madden N, Wen T, Aubey JJ, Aziz A, Baptiste CD, et al. Symptoms and critical illness among obstetric patients with coronavirus disease 2019 (COVID-19) infection. Obstet Gynecol. (2020) 136:291–9. 10.1097/AOG.0000000000003996 [DOI] [PubMed] [Google Scholar]
- 35.Blitz MJ, Rochelson B, Minkoff H, Meirowitz N, Prasannan L, London V, et al. Maternal mortality among women with coronavirus disease 2019 admitted to the intensive care unit. Am J Obstet Gynecol. (2020) 223:595–9 e5. 10.1016/j.ajog.2020.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buonsenso D, Raffaelli F, Tamburrini E, Biasucci DG, Salvi S, Smargiassi A, et al. Clinical role of lung ultrasound for diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound Obstet Gynecol. (2020) 56:106–9. 10.1002/uog.22055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen Y, Peng H, Wang L, Zhao Y, Zeng L, Gao H, et al. Infants born to mothers with a new coronavirus (COVID-19). Front Pediatr. (2020) 8:104. 10.3389/fped.2020.00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deng G, Zeng F, Zhang L, Chen H, Chen X, Yin M. Characteristics of pregnant patients with COVID-19 and liver injury. J Hepatol. (2020) 73:989–91. 10.1016/j.jhep.2020.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Giannini A, Mantovani A, Vezzoli C, Franchini D, Finazzi P. Lung ultrasound for pregnant women admitted to ICU for Covid-19 pneumonia. Minerva Anestesiol. (2020) 10.23736/S0375-9393.20.14726-6. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 40.Govind A, Essien S, Karthikeyan A, Fakokunde A, Janga D, Yoong W, et al. Re: novel coronavirus COVID-19 in late pregnancy: outcomes of first nine cases in an inner city London hospital. Eur J Obstet Gynecol Reprod Biol. (2020) 251:272–4. 10.1016/j.ejogrb.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, Seferovic MD, Aski SK, Arian SE, et al. Maternal death due to COVID-19. Am J Obstet Gynecol. (2020) 223:109.e1–e16. 10.1016/j.ajog.2020.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu X, Gao J, Luo X, Feng L, Liu W, Chen J, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Vertical transmission in neonates born to mothers with coronavirus disease 2019 (COVID-19) pneumonia. Obstet Gynecol. (2020) 136:65–7. 10.1097/AOG.0000000000003926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang W, Zhao Z, He Z, Liu S, Wu Q, Zhang X, et al. Unfavorable outcomes in pregnant patients with COVID-19. J Infect. (2020) 81:e99–101. 10.1016/j.jinf.2020.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jain P, Thakur A, Kler N, Garg P. Manifestations in neonates born to COVID-19 positive mothers. Indian J Pediatr. (2020) 87:644. 10.1007/s12098-020-03369-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kayem G, Lecarpentier E, Deruelle P, Bretelle F, Azria E, Blanc J, et al. A snapshot of the Covid-19 pandemic among pregnant women in France. J Gynecol Obstet Hum Reprod. (2020) 49:101826. 10.1016/j.jogoh.2020.101826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Khan S, Jun L, Nawsherwan, Siddique R, Li Y, Han G, et al. Association of COVID-19 with pregnancy outcomes in health-care workers and general women. Clin Microbiol Infect. (2020) 26:788–90. 10.1016/j.cmi.2020.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khan S, Peng L, Siddique R, Nabi G, Nawsherwan, Xue M, et al. Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infect Control Hosp Epidemiol. (2020) 41:748–50. 10.1017/ice.2020.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li L, Liu D, Yang L. Follow-up information about the four pregnant patients with coronavirus disease (COVID-19) pneumonia who were still in the hospital at the end of our study. AJR Am J Roentgenol. (2020) 215:W17–W8. 10.2214/AJR.20.23247 [DOI] [PubMed] [Google Scholar]
- 49.Lokken EM, Walker CL, Delaney S, Kachikis A, Kretzer NM, Erickson A, et al. Clinical characteristics of 46 pregnant women with a severe acute respiratory syndrome coronavirus 2 infection in Washington State. Am J Obstet Gynecol. (2020). 10.1016/j.ajog.2020.05.031. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lumbreras-Marquez MI, Campos-Zamora M, Lizaola-Diaz de Leon H, Farber MK. Maternal mortality from COVID-19 in Mexico. Int J Gynaecol Obstet. (2020) 150:266–7. 10.1002/ijgo.13250 [DOI] [PubMed] [Google Scholar]
- 51.Patane L, Morotti D, Giunta MR, Sigismondi C, Piccoli MG, Frigerio L, et al. Vertical transmission of coronavirus disease 2019: severe acute respiratory syndrome coronavirus 2 RNA on the fetal side of the placenta in pregnancies with coronavirus disease 2019-positive mothers and neonates at birth. Am J Obstet Gynecol MFM. (2020) 2:100145. 10.1016/j.ajogmf.2020.100145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perrone S, Deolmi M, Giordano M, D'Alvano T, Gambini L, Corradi M, et al. Report of a series of healthy term newborns from convalescent mothers with COVID-19. Acta Biomed. (2020) 91:251–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shanes ED, Mithal LB, Otero S, Azad HA, Miller ES, Goldstein JA. Placental pathology in COVID-19. Am J Clin Pathol. (2020) 154:23–32. 10.1093/ajcp/aqaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sun M, Xu G, Yang Y, Tao Y, Pian-Smith M, Madhavan V, et al. Evidence of mother-to-newborn infection with COVID-19. Br J Anaesth. (2020) 125:e245–e7. 10.1016/j.bja.2020.04.066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vlachodimitropoulou Koumoutsea E, Vivanti AJ, Shehata N, Benachi A, Le Gouez A, Desconclois C, et al. COVID-19 and acute coagulopathy in pregnancy. J Thromb Haemost. (2020) 18:1648–52. 10.1111/jth.14856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Xu L, Yang Q, Shi H, Lei S, Liu X, Zhu Y, et al. Clinical presentations and outcomes of SARS-CoV-2 infected pneumonia in pregnant women and health status of their neonates. Sci Bull. (2020) 65:1537–42. 10.1016/j.scib.2020.04.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yan J, Guo J, Fan C, Juan J, Yu X, Li J, et al. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. (2020) 223:111 e1–e14. 10.1016/j.ajog.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yang P, Wang X, Liu P, Wei C, He B, Zheng J, et al. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J Clin Virol. (2020) 127:104356. 10.1016/j.jcv.2020.104356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yu N, Li W, Kang Q, Zeng W, Feng L, Wu J. No SARS-CoV-2 detected in amniotic fluid in mid-pregnancy. Lancet Infect Dis. (2020). 10.1016/S1473-3099(20)30320-0. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hijona Elosegui JJ, Carballo Garcia AL, Fernandez Risquez AC. [New evidences that discard the possible vertical transmission of SARS-CoV-2 during pregnancy]. Med Clin. (2020) 155:313–4. 10.1016/j.medcle.2020.05.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hijona Elosegui JJ, Carballo Garcia AL, Fernandez Risquez AC, Bermudez Quintana M, Exposito Montes JF. Does the maternal-fetal transmission of SARS-CoV-2 occur during pregnancy? Rev Clin Esp. (2020). 10.1016/j.rce.2020.06.001. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hirshberg A, Kern-Goldberger AR, Levine LD, Pierce-Williams R, Short WR, Parry S, et al. Care of critically ill pregnant patients with coronavirus disease 2019: a case series. Am J Obstet Gynecol. (2020) 223:286–90. 10.1016/j.ajog.2020.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Juusela A, Nazir M, Gimovsky M. Two cases of coronavirus 2019-related cardiomyopathy in pregnancy. Am J Obstet Gynecol MFM. (2020) 2:100113. 10.1016/j.ajogmf.2020.100113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu W, Wang J, Li W, Zhou Z, Liu S, Rong Z. Clinical characteristics of 19 neonates born to mothers with COVID-19. Front Med. (2020) 14:193–8. 10.1007/s11684-020-0772-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lucarelli E, Behn C, Lashley S, Smok D, Benito C, Oyelese Y. Mechanical ventilation in pregnancy due to COVID-19: a cohort of three cases. Am J Perinatol. (2020) 37:1066–9. 10.1055/s-0040-1713664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mulvey JJ, Magro CM, Ma LX, Nuovo GJ, Baergen RN. Analysis of complement deposition and viral RNA in placentas of COVID-19 patients. Ann Diagn Pathol. (2020) 46:151530. 10.1016/j.anndiagpath.2020.151530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nie R, Wang S-S, Yang Q, Fan C-F, Liu Y-L, He W-C, et al. Clinical features and the maternal and neonatal outcomes of pregnant women with coronavirus disease 2019. medRxiv. (2020). 10.1101/2020.03.22.20041061. [Epub ahead of print]. [DOI] [Google Scholar]
- 68.Penfield CA, Brubaker SG, Limaye MA, Lighter J, Ratner AJ, Thomas KM, et al. Detection of severe acute respiratory syndrome coronavirus 2 in placental and fetal membrane samples. Am J Obstet Gynecol MFM. (2020) 2:100133. 10.1016/j.ajogmf.2020.100133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Pereira A, Cruz-Melguizo S, Adrien M, Fuentes L, Marin E, Perez-Medina T. Clinical course of coronavirus disease-2019 in pregnancy. Acta Obstet Gynecol Scand. (2020) 99:839–47. 10.1111/aogs.13921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sentilhes L, De Marcillac F, Jouffrieau C, Kuhn P, Thuet V, Hansmann Y, et al. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol. (2020). 10.1016/j.ajog.2020.06.022. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Silverstein JS, Limaye MA, Brubaker SG, Roman AS, Bautista J, Chervenak J, et al. Acute respiratory decompensation requiring intubation in pregnant women with SARS-CoV-2 (COVID-19). AJP Rep. (2020) 10:e169–e75. 10.1055/s-0040-1712925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wu C, Yang W, Wu X, Zhang T, Zhao Y, Ren W, et al. Clinical manifestation and laboratory characteristics of SARS-CoV-2 infection in pregnant women. Virol Sin. (2020) 35:305–10. 10.1007/s12250-020-00227-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yassa M, Birol P, Mutlu AM, Tekin AB, Sandal K, Tug N. Lung ultrasound can influence the clinical treatment of pregnant women with COVID-19. J Ultrasound Med. (2020). 10.1002/jum.15367. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zhu C, Liu W, Su H, Li S, Shereen MA, Lv Z, et al. Breastfeeding risk from detectable severe acute respiratory syndrome coronavirus 2 in breastmilk. J Infect. (2020) 81:452–82. 10.1016/j.jinf.2020.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yu N, Li W, Kang Q, Xiong Z, Wang S, Lin X, et al. Clinical features and obstetric and neonatal outcomes of pregnant patients with COVID-19 in Wuhan, China: a retrospective, single-centre, descriptive study. Lancet Infect Dis. (2020) 20:559–64. 10.1016/S1473-3099(20)30176-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Liu Y, Chen H, Tang K, Guo Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J Infect. (2020). 10.1016/j.jinf.2020.02.028. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dong L, Tian J, He S, Zhu C, Wang J, Liu C, et al. Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA. (2020) 323:1846–8. 10.1001/jama.2020.4621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Iqbal SN, Overcash R, Mokhtari N, Saeed H, Gold S, Auguste T, et al. An uncomplicated delivery in a patient with Covid-19 in the United States. N Engl J Med. (2020) 382:e34. 10.1056/NEJMc2007605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lee DH, Lee J, Kim E, Woo K, Park HY, An J. Emergency cesarean section performed in a patient with confirmed severe acute respiratory syndrome Coronavirus-2 -a case report. Korean J Anesthesiol. (2020) 73:347–51. 10.4097/kja.20116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Li Y, Zhao R, Zheng S, Chen X, Wang J, Sheng X, et al. Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2, China. Emerg Infect Dis. (2020) 26:1335–6. 10.3201/eid2606.200287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liao X, Yang H, Kong J, Yang H. Chest CT Findings in a pregnant patient with 2019 novel coronavirus disease. Balkan Med J. (2020) 37:226–8. 10.4274/balkanmedj.galenos.2020.2020.3.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang S, Guo L, Chen L, Liu W, Cao Y, Zhang J, et al. A case report of neonatal 2019 coronavirus disease in China. Clin Infect Dis. (2020) 71:853–7. 10.1093/cid/ciaa225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang X, Zhou Z, Zhang J, Zhu F, Tang Y, Shen X. A case of 2019 novel coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. (2020) 71:844–6. 10.1093/cid/ciaa200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wen R, Sun Y, Xing QS. A patient with SARS-CoV-2 infection during pregnancy in Qingdao, China. J Microbiol Immunol Infect. (2020) 53:499–500. 10.1016/j.jmii.2020.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xia H, Zhao S, Wu Z, Luo H, Zhou C, Chen X. Emergency Caesarean delivery in a patient with confirmed COVID-19 under spinal anaesthesia. Br J Anaesth. (2020) 124:e216–8. 10.1016/j.bja.2020.02.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Zambrano LI, Fuentes-Barahona IC, Bejarano-Torres DA, Bustillo C, Gonzales G, Vallecillo-Chinchilla G, et al. A pregnant woman with COVID-19 in Central America. Travel Med Infect Dis. (2020) 36:101639. 10.1016/j.tmaid.2020.101639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zhang B, Liu S, Tan T, Huang W, Dong Y, Chen L, et al. Treatment with convalescent plasma for critically ill patients with severe acute respiratory syndrome coronavirus 2 infection. Chest. (2020) 158:e9–13. 10.1016/j.chest.2020.03.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ahmed I, Azhar A, Eltaweel N, Tan BK. First COVID-19 maternal mortality in the UK associated with thrombotic complications. Br J Haematol. (2020) 190:e37–8. 10.1111/bjh.16849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Algarroba GN, Rekawek P, Vahanian SA, Khullar P, Palaia T, Peltier MR, et al. Visualization of severe acute respiratory syndrome coronavirus 2 invading the human placenta using electron microscopy. Am J Obstet Gynecol. (2020) 223:275–8. 10.1016/j.ajog.2020.05.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alzamora MC, Paredes T, Caceres D, Webb CM, Valdez LM, La Rosa M. Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol. (2020) 37:861–5. 10.1055/s-0040-1710050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bani Hani DA, Alsharaydeh I, Bataineh AM, Al Athamneh M, Qamileh I, Al-Baik A, et al. Successful anesthetic management in cesarean section for pregnant woman with COVID-19. Am J Case Rep. (2020) 21:e925512. 10.12659/AJCR.925512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Blauvelt CA, Chiu C, Donovan AL, Prahl M, Shimotake TK, George RB, et al. Acute respiratory distress syndrome in a preterm pregnant patient with coronavirus disease 2019 (COVID-19). Obstet Gynecol. (2020) 136:46–51. 10.1097/AOG.0000000000003949 [DOI] [PubMed] [Google Scholar]
- 93.Du Y, Wang L, Wu G, Lei X, Li W, Lv J. Anesthesia and protection in an emergency cesarean section for pregnant woman infected with a novel coronavirus: case report and literature review. J Anesth. (2020) 34:613–8. 10.1007/s00540-020-02796-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gidlof S, Savchenko J, Brune T, Josefsson H. COVID-19 in pregnancy with comorbidities: more liberal testing strategy is needed. Acta Obstet Gynecol Scand. (2020) 99:948–9. 10.1111/aogs.13862 [DOI] [PubMed] [Google Scholar]
- 95.Hong L, Smith N, Keerthy M, Lee-Griffith M, Garcia R, Shaman M, et al. Severe COVID-19 infection in pregnancy requiring intubation without preterm delivery: a case report. Case Rep Womens Health. (2020) 27:e00217. 10.1016/j.crwh.2020.e00217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kalafat E, Yaprak E, Cinar G, Varli B, Ozisik S, Uzun C, et al. Lung ultrasound and computed tomographic findings in pregnant woman with COVID-19. Ultrasound Obstet Gynecol. (2020) 55:835–7. 10.1002/uog.22034 [DOI] [PubMed] [Google Scholar]
- 97.Kirtsman M, Diambomba Y, Poutanen SM, Malinowski AK, Vlachodimitropoulou E, Parks WT, et al. Probable congenital SARS-CoV-2 infection in a neonate born to a woman with active SARS-CoV-2 infection. CMAJ. (2020) 192:E647–50. 10.1503/cmaj.200821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kuhrt K, McMicking J, Nanda S, Nelson-Piercy C, Shennan A. Placental abruption in a twin pregnancy at 32 weeks' gestation complicated by coronavirus disease 2019 without vertical transmission to the babies. Am J Obstet Gynecol MFM. (2020) 2:100135. 10.1016/j.ajogmf.2020.100135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Li J, Wang Y, Zeng Y, Song T, Pan X, Jia M, et al. Critically ill pregnant patient with COVID-19 and neonatal death within two hours of birth. Int J Gynaecol Obstet. (2020) 150:126–8. 10.1002/ijgo.13189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lowe B, Bopp B. COVID-19 vaginal delivery - A case report. Aust N Z J Obstet Gynaecol. (2020) 60:465–6. 10.1111/ajo.13173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lu D, Sang L, Du S, Li T, Chang Y, Yang XA. Asymptomatic COVID-19 infection in late pregnancy indicated no vertical transmission. J Med Virol. (2020) 92:1660–4. 10.1002/jmv.25927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lyra J, Valente R, Rosario M, Guimaraes M. Cesarean section in a pregnant woman with COVID-19: first case in Portugal. Acta Med Port. (2020) 33:429–31. 10.20344/amp.13883 [DOI] [PubMed] [Google Scholar]
- 103.Nesr G, Garnett C, Bailey C, Koshy R, Arami S. Immune thrombocytopenia flare with mild COVID-19 infection in pregnancy: a case report. Br J Haematol. (2020) 190:e146–8. 10.1111/bjh.16928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Peng Z, Wang J, Mo Y, Duan W, Xiang G, Yi M, et al. Unlikely SARS-CoV-2 vertical transmission from mother to child: a case report. J Infect Public Health. (2020) 13:818–20. 10.1016/j.jiph.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Piersigilli F, Carkeek K, Hocq C, van Grambezen B, Hubinont C, Chatzis O, et al. COVID-19 in a 26-week preterm neonate. Lancet Child Adolesc Health. (2020) 4:476–8. 10.1016/S2352-4642(20)30140-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Baud D, Greub G, Favre G, Gengler C, Jaton K, Dubruc E, et al. Second-trimester miscarriage in a pregnant woman with SARS-CoV-2 infection. JAMA. (2020) 323:2198–200. 10.1001/jama.2020.7233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mehta H, Ivanovic S, Cronin A, VanBrunt L, Mistry N, Miller R, et al. Novel coronavirus-related acute respiratory distress syndrome in a patient with twin pregnancy: a case report. Case Rep Womens Health. (2020) 27:e00220. 10.1016/j.crwh.2020.e00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Polonia-Valente R, Moucho M, Tavares M, Vilan A, Montenegro N, Rodrigues T. Vaginal delivery in a woman infected with SARS-CoV-2 - The first case reported in Portugal. Eur J Obstet Gynecol Reprod Biol. (2020) 250:253–4. 10.1016/j.ejogrb.2020.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Schnettler WT, Al Ahwel Y, Suhag A. Severe acute respiratory distress syndrome in coronavirus disease 2019-infected pregnancy: obstetric and intensive care considerations. Am J Obstet Gynecol MFM. (2020) 2:100120. 10.1016/j.ajogmf.2020.100120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sharma KA, Kumari R, Kachhawa G, Chhabra A, Agarwal R, Sharma A, et al. Management of the first patient with confirmed COVID-19 in pregnancy in India: from guidelines to frontlines. Int J Gynaecol Obstet. (2020) 150:116–8. 10.1002/ijgo.13179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Taghizadieh A, Mikaeili H, Ahmadi M, Valizadeh H. Acute kidney injury in pregnant women following SARS-CoV-2 infection: a case report from Iran. Respir Med Case Rep. (2020) 30:101090. 10.1016/j.rmcr.2020.101090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Vallejo V, Ilagan JG. A Postpartum death due to coronavirus disease 2019 (COVID-19) in the United States. Obstet Gynecol. (2020) 136:52–5. 10.1097/AOG.0000000000003950 [DOI] [PubMed] [Google Scholar]
- 113.Xiong X, Wei H, Zhang Z, Chang J, Ma X, Gao X, et al. Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID-19. J Med Virol. (2020). 10.1002/jmv.25857. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yu Y, Fan C, Bian J, YinShen. Severe COVID-19 in a pregnant patient admitted to hospital in Wuhan. Int J Gynaecol Obstet. (2020) 150:262–3. 10.1002/ijgo.13232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zamaniyan M, Ebadi A, Aghajanpoor S, Rahmani Z, Haghshenas M, Azizi S. Preterm delivery, maternal death, and vertical transmission in a pregnant woman with COVID-19 infection. Prenat Diagn. (2020). 10.1002/pd.5713. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Anderson J, Schauer J, Bryant S, Graves CR. The use of convalescent plasma therapy and remdesivir in the successful management of a critically ill obstetric patient with novel coronavirus 2019 infection: a case report. Case Rep Womens Health. (2020) 27:e00221. 10.1016/j.crwh.2020.e00221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Browne PC, Linfert JB, Perez-Jorge E. Successful treatment of preterm labor in association with acute COVID-19 infection. Am J Perinatol. (2020) 37:866–8. 10.1055/s-0040-1709993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Carosso A, Cosma S, Borella F, Marozio L, Coscia A, Ghisetti V, et al. Pre-labor anorectal swab for SARS-CoV-2 in COVID-19 pregnant patients: is it time to think about it? Eur J Obstet Gynecol Reprod Biol. (2020) 249:98–9. 10.1016/j.ejogrb.2020.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.González Romero D, Ocampo Pérez J, González Bautista L, Santana-Cabrera L. Pronóstico perinatal y de la paciente embarazada con infección por COVID-19. Rev Clin Esp. (2020) 220:533–4. 10.1016/j.rce.2020.04.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hansen KA, Stovall DW. Ectopic pregnancy during coronavirus disease 2019 (COVID-19): To operate, or not to operate. Obstet Gynecol. (2020) 136:288–90. 10.1097/AOG.0000000000003995 [DOI] [PubMed] [Google Scholar]
- 121.Hosier H, Farhadian SF, Morotti RA, Deshmukh U, Lu-Culligan A, Campbell KH, et al. SARS-CoV-2 infection of the placenta. J Clin Invest. (2020) 130:4947–53. 10.1101/2020.04.30.20083907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Inchingolo R, Smargiassi A, Moro F, Buonsenso D, Salvi S, Del Giacomo P, et al. The diagnosis of pneumonia in a pregnant woman with coronavirus disease 2019 using maternal lung ultrasound. Am J Obstet Gynecol. (2020) 223:9–11. 10.1016/j.ajog.2020.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Indraccolo U. A pregnant woman and the SARS-CoV-2 infection: how are barriers easily crossed? Recenti Prog Med. (2020) 111:259–60. 10.1701/3347.33190 [DOI] [PubMed] [Google Scholar]
- 124.Joudi N, Henkel A, Lock WS, Lyell D. Preeclampsia treatment in severe acute respiratory syndrome coronavirus 2. Am J Obstet Gynecol MFM. (2020) 2:100146. 10.1016/j.ajogmf.2020.100146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Kang X, Zhang R, He H, Yao Y, Zheng Y, Wen X, et al. [Anesthesia management in cesarean section for a patient with coronavirus disease 2019]. Zhejiang Da Xue Xue Bao Yi Xue Ban. (2020) 49:249–52. 10.3785/j.issn.1008-9292.2020.03.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kelly JC, Dombrowksi M, O'Neil-Callahan M, Kernberg AS, Frolova AI, Stout MJ. False-negative testing for severe acute respiratory syndrome coronavirus 2: consideration in obstetrical care. Am J Obstet Gynecol MFM. (2020) 2:100130. 10.1016/j.ajogmf.2020.100130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kleinwechter H, Laubner K. Coronaviruserkrankung 2019 (COVID-19) und Schwangerschaft. Der Diabetologe. (2020) 16:242–6. 10.1007/s11428-020-00611-0 [DOI] [Google Scholar]
- 128.Lang GJ, Zhao H. Can SARS-CoV-2-infected women breastfeed after viral clearance? J Zhejiang Univ Sci B. (2020) 21:405–7. 10.1631/jzus.B2000095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Panichaya P, Thaweerat W, Uthaisan J. Prolonged viral persistence in COVID-19 second trimester pregnant patient. Eur J Obstet Gynecol Reprod Biol. (2020) 250:263. 10.1016/j.ejogrb.2020.05.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Rabice SR, Altshuler PC, Bovet C, Sullivan C, Gagnon AJ. COVID-19 infection presenting as pancreatitis in a pregnant woman: a case report. Case Rep Womens Health. (2020) 27:e00228. 10.1016/j.crwh.2020.e00228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Rosen MH, Axelrad J, Hudesman D, Rubin DT, Chang S. Management of acute severe ulcerative colitis in a pregnant woman with COVID-19 infection: a case report and review of the literature. Inflamm Bowel Dis. (2020) 26:971–3. 10.1093/ibd/izaa109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Schoenmakers S, Snijder P, Verdijk R, Kuiken T, Kamphuis S, Koopman L, et al. SARS-CoV-2 placental infection and inflammation leading to fetal distress and neonatal multi-organ failure in an asymptomatic woman. medRxiv. (2020). 10.1101/2020.06.08.20110437. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tang MW, Nur E, Biemond BJ. Immune thrombocytopenia due to COVID-19 during pregnancy. Am J Hematol. (2020) 95:E191–2. 10.1002/ajh.25877 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Vibert F, Kretz M, Thuet V, Barthel F, De Marcillac F, Deruelle P, et al. Prone positioning and high-flow oxygen improved respiratory function in a 25-week pregnant woman with COVID-19. Eur J Obstet Gynecol Reprod Biol. (2020) 250:257–8. 10.1016/j.ejogrb.2020.05.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yilmaz R, Kilic F, Arican S, Hacibeyoglu G, Suslu H, Koyuncu M, et al. Anesthetic management for cesarean birth in pregnancy with the novel coronavirus (COVID-19). J Clin Anesth. (2020) 66:109921. 10.1016/j.jclinane.2020.109921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ferrazzi E, Frigerio L, Savasi V, Vergani P, Prefumo F, Barresi S, et al. Vaginal delivery in SARS-CoV-2-infected pregnant women in Northern Italy: a retrospective analysis. Bjog. (2020) 127:1116–21. 10.1111/1471-0528.16278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Griffin I, Benarba F, Peters C, Oyelese Y, Murphy T, Contreras D, et al. The impact of COVID-19 infection on labor and delivery, newborn nursery, and neonatal intensive care unit: prospective observational data from a single hospital system. Am J Perinatol. (2020) 37:1022–30. 10.1055/s-0040-1713416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Khoury R, Bernstein PS, Debolt C, Stone J, Sutton DM, Simpson LL, et al. Characteristics and outcomes of 241 births to women with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection at five New York City medical centers. Obstet Gynecol. (2020) 136:273–82. 10.1097/AOG.0000000000004025 [DOI] [PubMed] [Google Scholar]
- 139.Knight M, Bunch K, Vousden N, Morris E, Simpson N, Gale C, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. (2020) 369:m2107. 10.1136/bmj.m2107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.la Cour Freiesleben N, Egerup P, Hviid KVR, Severinsen ER, Kolte AM, Westergaard D, et al. SARS-CoV-2 in first trimester pregnancy - does it affect the fetus? medRxiv. (2020). 10.1101/2020.06.08.20125195. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.London V, McLaren R, Jr, Atallah F, Cepeda C, McCalla S, Fisher N, et al. The relationship between status at presentation and outcomes among pregnant women with COVID-19. Am J Perinatol. (2020) 37:991–4. 10.1055/s-0040-1712164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Luo Q, Chen L, Yao D, Zhu J, Zeng X, Xia L, et al. Safety of breastfeeding in mothers with SARS-CoV-2 infection. medRxiv. (2020). 10.1101/2020.05.30.20033407. [Epub ahead of print]. [DOI] [Google Scholar]
- 143.Martinez-Perez O, Vouga M, Cruz Melguizo S, Forcen Acebal L, Panchaud A, Munoz-Chapuli M, et al. Association between mode of delivery among pregnant women with COVID-19 and maternal and neonatal outcomes in Spain. JAMA. (2020) 324:296–9. 10.1001/jama.2020.10125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mendoza M, Garcia-Ruiz I, Maiz N, Rodo C, Garcia-Manau P, Serrano B, et al. Pre-eclampsia-like syndrome induced by severe COVID-19: a prospective observational study. BJOG. (2020) 127:1374–80. 10.1111/1471-0528.16339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mohr-Sasson A, Chayo J, Bart Y, Meyer R, Sivan E, Mazaki-Tovi S, et al. Laboratory characteristics of pregnant compared to non-pregnant women infected with SARS-CoV-2. Arch Gynecol Obstet. (2020) 302:629–34. 10.1007/s00404-020-05655-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Pierce-Williams RAM, Burd J, Felder L, Khoury R, Bernstein PS, Avila K, et al. Clinical course of severe and critical coronavirus disease 2019 in hospitalized pregnancies: a United States cohort study. Am J Obstet Gynecol MFM. (2020) 2:100134. 10.1016/j.ajogmf.2020.100134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Savasi VM, Parisi F, Patane L, Ferrazzi E, Frigerio L, Pellegrino A, et al. Clinical findings and disease severity in hospitalized pregnant women with coronavirus disease 2019 (COVID-19). Obstet Gynecol. (2020) 136:252–8. 10.1097/AOG.0000000000003979 [DOI] [PubMed] [Google Scholar]
- 148.Wu Y, Liu C, Dong L, Zhang C, Chen Y, Liu J, et al. Coronavirus disease 2019 among pregnant Chinese women: case series data on the safety of vaginal birth and breastfeeding. BJOG. (2020) 127:1109–15. 10.1111/1471-0528.16276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Yang H, Hu B, Zhan S, Yang LY, Xiong G. Effects of severe acute respiratory syndrome coronavirus 2 infection on pregnant women and their infants. Arch Pathol Lab Med. (2020) 144:1217–22. 10.5858/arpa.2020-0232-SA [DOI] [PubMed] [Google Scholar]
- 150.Yin M, Zhang L, Deng G, Han C, Shen M, Sun H, et al. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection during pregnancy in China: a retrospective cohort study. medRxiv. (2020). 10.1101/2020.04.07.20053744. [Epub ahead of print]. [DOI] [Google Scholar]
- 151.Zeng L, Xia S, Yuan W, Yan K, Xiao F, Shao J, et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. (2020) 174:722–5. 10.1001/jamapediatrics.2020.0878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Blitz MJ, Grunebaum A, Tekbali A, Bornstein E, Rochelson B, Nimaroff M, et al. Intensive care unit admissions for pregnant and nonpregnant women with coronavirus disease 2019. Am J Obstet Gynecol. (2020) 223:290–1. 10.1016/j.ajog.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.San-Juan R, Barbero P, Fernandez-Ruiz M, Lopez-Medrano F, Lizasoain M, Hernandez-Jimenez P, et al. Incidence and clinical profiles of COVID-19 pneumonia in pregnant women: a single-centre cohort study from Spain. EClinicalMedicine. (2020) 23:100407. 10.1016/j.eclinm.2020.100407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Vintzileos WS, Muscat J, Hoffmann E, John NS, Vertichio R, Vintzileos AM, et al. Screening all pregnant women admitted to labor and delivery for the virus responsible for coronavirus disease 2019. Am J Obstet Gynecol. (2020) 223:284–6. 10.1016/j.ajog.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zeng Y, Lin L, Yan Q, Wei W, Xiang Yang B, Huang R, et al. Update on clinical outcomes of women with COVID-19 during pregnancy. Int J Gynaecol Obstet. (2020) 150:264–6. 10.1002/ijgo.13236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Collin J, Byström E, Carnahan A, Ahrne M. Public health agency of Sweden's brief report: pregnant and postpartum women with severe acute respiratory syndrome coronavirus 2 infection in intensive care in Sweden. Acta Obstet Gynecol Scand. (2020) 99:819–22. 10.1111/aogs.13901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Ferrazzi EM, Frigerio L, Cetin I, Vergani P, Spinillo A, Prefumo F, et al. COVID-19 Obstetrics Task Force, Lombardy, Italy: executive management summary and short report of outcome. Int J Gynaecol Obstet. (2020) 149:377–8. 10.1002/ijgo.13162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gulersen M, Blitz MJ, Rochelson B, Nimaroff M, Shan W, Bornstein E. Clinical implications of SARS-CoV-2 infection in the viable preterm period. Am J Perinatol. (2020) 37:1077–83. 10.1055/s-0040-1713851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Liao J, He X, Gong Q, Yang L, Zhou C, Li J. Analysis of vaginal delivery outcomes among pregnant women in Wuhan, China during the COVID-19 pandemic. Int J Gynaecol Obstet. (2020) 150:53–7. 10.1002/ijgo.13188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Liu H, Liu F, Li J, Zhang T, Wang D, Lan W. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J Infect. (2020) 80:e7–13. 10.1016/j.jinf.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Liu P, Zheng J, Yang P, Wang X, Wei C, Zhang S, et al. The immunologic status of newborns born to SARS-CoV-2-infected mothers in Wuhan, China. J Allergy Clin Immunol. (2020) 146:101–9.e1. 10.1016/j.jaci.2020.04.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Ochiai D, Kasuga Y, Iida M, Ikenoue S, Tanaka M. Universal screening for SARS-CoV-2 in asymptomatic obstetric patients in Tokyo, Japan. Int J Gynaecol Obstet. (2020) 150:268–9. 10.1002/ijgo.13252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Qadri F, Mariona F. Pregnancy affected by SARS-CoV-2 infection: a flash report from Michigan. J Matern Fetal Neonatal Med. (2020). 10.1080/14767058.2020.1765334. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 164.Qiancheng X, Jian S, Lingling P, Lei H, Xiaogan J, Weihua L, et al. Coronavirus disease 2019 in pregnancy. Int J Infect Dis. (2020) 95:376–83. 10.1016/j.ijid.2020.04.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang Z, Wang Z, Xiong G. Clinical characteristics and laboratory results of pregnant women with COVID-19 in Wuhan, China. Int J Gynaecol Obstet. (2020). 10.1002/ijgo.13265. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wu X, Sun R, Chen J, Xie Y, Zhang S, Wang X. Radiological findings and clinical characteristics of pregnant women with COVID-19 pneumonia. Int J Gynaecol Obstet. (2020) 150:58–63. 10.1002/ijgo.13165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Zeng QL, Li GM, Ji F, Ma SH, Zhang GF, Xu JH, et al. Clinical course and treatment efficacy of COVID-19 near Hubei Province, China: a multicentre, retrospective study. Transbound Emerg Dis. (2020). 10.1111/tbed.13674. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zhang ZJ, Yu XJ, Fu T, Liu Y, Jiang Y, Yang BX, et al. Novel coronavirus infection in newborn babies aged <28 days in China. Eur Respir J. (2020) 55:2000697. 10.1183/13993003.00697-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Cosma S, Carosso A, Cusato J, Borella F, Carosso M, Bovetti M, et al. COVID-19 and first trimester spontaneous abortion: a case-control study of 225 pregnant patients. medRxiv. (2020). 10.1101/2020.06.19.20135749. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Li N, Han L, Peng M, Lv Y, Ouyang Y, Liu K, et al. Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clin Infect Dis. (2020). 10.1093/cid/ciaa352. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yang H, Sun G, Tang F, Peng M, Gao Y, Peng J, et al. Clinical features and outcomes of pregnant women suspected of coronavirus disease 2019. J Infect. (2020) 81:e40–4. 10.1016/j.jinf.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sutton D, Fuchs K, D'Alton M, Goffman D. Universal screening for SARS-CoV-2 in women admitted for delivery. N Engl J Med. (2020) 382:2163–4. 10.1056/NEJMc2009316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID-19: a systematic review of 108 pregnancies. Acta Obstet Gynecol Scand. (2020) 99:823–9. 10.1111/aogs.13867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Royal College of Obstetricians and Gynaecologists Royal College of Midwives Royal College of Paediatrics and Child Health Public Health England and Health Protection Scotland Coronavirus (COVID-19) Infection in Pregnancy: Information for Healthcare Professionals (Version 11, July 24th 2020). [Online]. Available online at: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/coronavirus-pregnancy/ (accessed August 1, 2020).
- 175.Ellington S, Strid P, Tong VT, Woodworth K, Galang RR, Zambrano LD, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:769–75. 10.15585/mmwr.mm6925a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chawanpaiboon S, Vogel JP, Moller A-B, Lumbiganon P, Petzold M, Hogan D, et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Global Health. (2019) 7:e37–46. 10.1016/S2214-109X(18)30451-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Schwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. (2020) 12:194. 10.3390/v12020194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Stockman LJ, Lowther SA, Coy K, Saw J, Parashar UD. SARS during pregnancy, United States. Emerg Infect Dis. (2004) 10:1689–90. 10.3201/eid1009.040244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Alfaraj SH, Al-Tawfiq JA, Memish ZA. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: report of two cases & review of the literature. J Microbiol Immunol Infect. (2019) 52:501–3. 10.1016/j.jmii.2018.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Alserehi H, Wali G, Alshukairi A, Alraddadi B. Impact of Middle East Respiratory Syndrome coronavirus (MERS-CoV) on pregnancy and perinatal outcome. BMC Infect Dis. (2016) 16:105. 10.1186/s12879-016-1437-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Maxwell C, McGeer A, Tai KFY, Sermer M. No. 225-Management guidelines for obstetric patients and neonates born to mothers with suspected or probable severe acute respiratory syndrome (SARS). J Obstet Gynaecol Can. (2017) 39:e130–7. 10.1016/j.jogc.2017.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Assiri A, Abedi GR, Al Masri M, Bin Saeed A, Gerber SI, Watson JT. Middle east respiratory syndrome coronavirus infection during pregnancy: a report of 5 cases from Saudi Arabia. Clin Infect Dis. (2016) 63:951–3. 10.1093/cid/ciw412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Haines CJ, Chu YW, Chung TK. The effect of Severe Acute Respiratory Syndrome on a hospital obstetrics and gynaecology service. Bjog. (2003) 110:643–5. 10.1046/j.1471-0528.2003.03007.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Jeong SY, Sung SI, Sung JH, Ahn SY, Kang ES, Chang YS, et al. MERS-CoV infection in a pregnant woman in Korea. J Korean Med Sci. (2017) 32:1717–20. 10.3346/jkms.2017.32.10.1717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Jiang X, Gao X, Zheng H, Yan M, Liang W, Shao Z, et al. Specific immunoglobulin g antibody detected in umbilical blood and amniotic fluid from a pregnant woman infected by the coronavirus associated with severe acute respiratory syndrome. Clin Diagn Lab Immunol. (2004) 11:1182–4. 10.1128/CDLI.11.6.1182-1184.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Malik A, El Masry KM, Ravi M, Sayed F. Middle east respiratory syndrome coronavirus during pregnancy, Abu Dhabi, United Arab Emirates, 2013. Emerg Infect Dis. (2016) 22:515–7. 10.3201/eid2203.151049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Owolabi T, Kwolek S. Managing obstetrical patients during severe acute respiratory syndrome outbreak. J Obstet Gynaecol Can. (2004) 26:35–41. 10.1016/S1701-2163(16)30694-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Payne DC, Iblan I, Alqasrawi S, Al Nsour M, Rha B, Tohme RA, et al. Stillbirth during infection with Middle East respiratory syndrome coronavirus. J Infect Dis. (2014) 209:1870–2. 10.1093/infdis/jiu068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Robertson CA, Lowther SA, Birch T, Tan C, Sorhage F, Stockman L, et al. SARS and pregnancy: a case report. Emerg Infect Dis. (2004) 10:345–8. 10.3201/eid1002.030736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gynecol. (2004) 191:292–7. 10.1016/j.ajog.2003.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Lam CM, Wong SF, Leung TN, Chow KM, Yu WC, Wong TY, et al. A case-controlled study comparing clinical course and outcomes of pregnant and non-pregnant women with severe acute respiratory syndrome. BJOG. (2004) 111:771–4. 10.1111/j.1471-0528.2004.00199.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Takemoto MLS, Menezes MO, Andreucci CB, Nakamura-Pereira M, Amorim MMR, Katz L, et al. The tragedy of COVID-19 in Brazil: 124 maternal deaths and counting. Int J Gynaecol Obstet. (2020). 10.1002/ijgo.13300. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Centers for Disease Control and Prevention (CDC) If You Are Pregnant, Breastfeeding, or Caring for Young Children. [Online]. Available online at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/pregnancy-breastfeeding.html (accessed July 29, 2020).
- 194.Yang H, Wang C, Poon LC. Novel coronavirus infection and pregnancy. Ultrasound Obstet Gynecol. (2020) 55:435–7. 10.1002/uog.22006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Favre G, Pomar L, Qi X, Nielsen-Saines K, Musso D, Baud D. Guidelines for pregnant women with suspected SARS-CoV-2 infection. Lancet Infect Dis. (2020) 20:652–3. 10.1016/S1473-3099(20)30157-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Liang H, Acharya G. Novel corona virus disease (COVID-19) in pregnancy: what clinical recommendations to follow? Acta Obstet Gynecol Scand. (2020) 99:439–42. 10.1111/aogs.13836 [DOI] [PubMed] [Google Scholar]
- 197.Poon LC, Yang H, Lee JCS, Copel JA, Leung TY, Zhang Y, et al. ISUOG Interim guidance on 2019 novel coronavirus infection during pregnancy and puerperium: information for healthcare professionals. Ultrasound Obstet Gynecol. (2020) 55:700–8. 10.1002/uog.22013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Victora CG, Bahl R, Barros AJ, Franca GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. (2016) 387:475–90. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- 199.UNICEF/World Health Organization Coronavirus Disease (COVID-19): What Parents Should Know. [Online]. Available online at: https://www.unicef.org/stories/novel-coronavirus-outbreak-what-parents-should-know (accessed July 29, 2020).
- 200.Rodrigues C, Baia I, Domingues R, Barros H. Pregnancy and breastfeeding during COVID-19 pandemic: a systematic review of published pregnancy cases. medRxiv. (2020). 10.1101/2020.04.25.20079509. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author/s.