Abstract
Objective:
To summarize the available evidence on the use of elastography in the assessment of the masseter muscle in healthy individuals and patients with masseter muscle disorders.
Methods:
Systematic literature review has been performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines.
Results:
16 of 142 studies identified were analyzed. Elastography was used in seven studies. Heterogeneity was observed in terms of study protocols, devices, patients, units of measure, and results. Elasticity values showed a correlation between the left and right masseter muscle side in healthy people, but not in patients with temporomandibular disorders (TMDs). Elasticity values increased in TMD and were correlated with the severity of TMD symptoms. Phantom studies proved the high reliability of elastography.
Conclusion:
Elastography is a promising tool for the assessment of the masseter muscle elasticity, but the evidence is insufficient. Studies on larger groups are needed to determine the accuracy of elastography to characterize masticatory muscle disorders.
Keywords: elastography, elasticity, temporomandibular disorders, masseter muscle, systematic literature review
Introduction
The masseter muscle, being a part of the masticatory apparatus, helps to perform an important physiological function of mastication, which is an initial activity for appropriate digestion. Pathologies of the masseter muscle result in impaired bite force and occlusal morphology, speech disorders, and acute or chronic pain.1,2 The assessment of the masticatory muscle is particularly useful for diagnosing and monitoring muscle-related temporomandibular disorders (TMDs), which are frequent orofacial problems. The prevalence of TMD varies greatly across studies. Prevalence of myofascial TMD was estimated to be 10.5% in United States community females.3 In the Northern Finland Birth Cohort 1966, the prevalence of TMD symptoms reached 34.2% in 46-year-old people and dominated in females.4 A Brazilian study conducted in adolescents between the age of 10 and 17 years showed a 33.2% prevalence irrespective of age and economic status.5 Studies conducted on the Polish population found that approximately 54% of students presented with TMD symptoms.6,7 Some other studies suggest that TMD symptoms may be present in up to 40–90% of the population, but without the need for active treatment.8 Some reports from the literature link the increase in TMD symptoms to abuse of active substances and poor emotional health status; TMD is diagnosed in over half of the prisoners.9,10
The clinical presentation of TMD includes acute and chronic masticatory muscles and/or temporomandibular joint pain, sounds in temporomandibular joints (clicking and popping), and abnormal jaw movements. The main symptoms may be associated with headache, otolaryngological disorders, and pain within muscles of the neck and shoulder girdle. Physical examination sometimes shows an increased stiffness and tension of the masseter muscles, which is often associated with their hypertrophy, soreness, and pain during palpation. Diagnostic criteria are based on the recommendations of the International Network for Orofacial Pain and Related Disorders Methodology (Diagnostic Criteria for Temporomandibular Disorders; DC-TMD).11,12
Clinical symptoms perceived by patients and the mechanics of the temporomandibular joints are important for the diagnosis of TMD, but they constitute only a part of the picture of the disorders. Novel approaches to evaluate the condition of masticatory muscles may facilitate the diagnosis and enable precise monitoring of the management. One of such techniques is shear wave elastography used for noninvasive assessment of soft tissue hardness. In this method, shear waves generated by pressure are detected by longitudinal ultrasonography waves that propagate in tissues much faster than shear waves. The quantitative measurement of tissue hardness is expressed in kilopascals. The advantages of this method include low dependence on the operator, high repeatability and the possibility of quantitative evaluation of tested parameters.13–16 The main disadvantage is that every organ has its unique characteristics, and hence, normative values must be determined for each muscle independently.17,18 Currently, although there has been a growing body of evidence, little is known about elasticity values of the masseter muscle as well as the optimal examination protocol that would enable to obtain repetitive and reliable results.
The goal of this systematic review was to summarize the available evidence on the use of elastography in the assessment of the masseter muscle in healthy individuals and patients with TMD. Authors focused on the techniques and devices used for the assessment of the masseter muscle. Furthermore, the authors aimed at determining the ranges of the masseter muscle elasticity and factors that contribute to its change.
Methods and materials
Evidence acquisition
The databases PubMed, Ovid MEDLINE, Web of Science, and ClinicalTrials.gov were searched for relevant literature on February 19, 2019. The present systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.19 The search in databases was supplemented with a Google search of grey literature and hand search of the bibliographies of retrieved articles. No restrictions regarding timeframe and geographical scope were applied, but papers published only in English were considered. Electronic search strategies employed the following keywords elastography, shear-wave elastography, sonoelastography, TMD, masticatory, masseter as well as combinations and variations of them and are shown in Supplementary Table 1 to S3. Inclusion and exclusion criteria were defined according to the PICOS (Population, Intervention, Comparison, Outcomes and Study Design) approach (Table 1). Three reviewers performed the literature search. Two reviewers screened records and abstracts and recommended papers for qualitative analysis. The following data were extracted from selected papers: author and year of publication, characteristics of the population under study, examination protocol, the device used, and elasticity values of the normal and diseased masseter muscle.
Table 1.
Inclusion and exclusion criteria
| PICOS | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Population | Healthy patients, phantoms, humans and animals, patients suffering from TMD | Pathologies other than TMD including malignant lesions, benign tumors, injuries |
| Intervention | Shear-wave elastography or sonoelastography of masseter muscle | - |
| Comparator | None or any | - |
| Outcome | Muscle hardness and elasticity | - |
| Study | RCTs, cohort studies, experimental models, animal models, case reports | Review papers, letters, commentaries, articles not in English |
PICOS, Population, Intervention, Comparison, Outcomes and Study Design; RCT, randomized controlled trials;TMD, temporomandibular disorders.
Results
Evidence synthesis
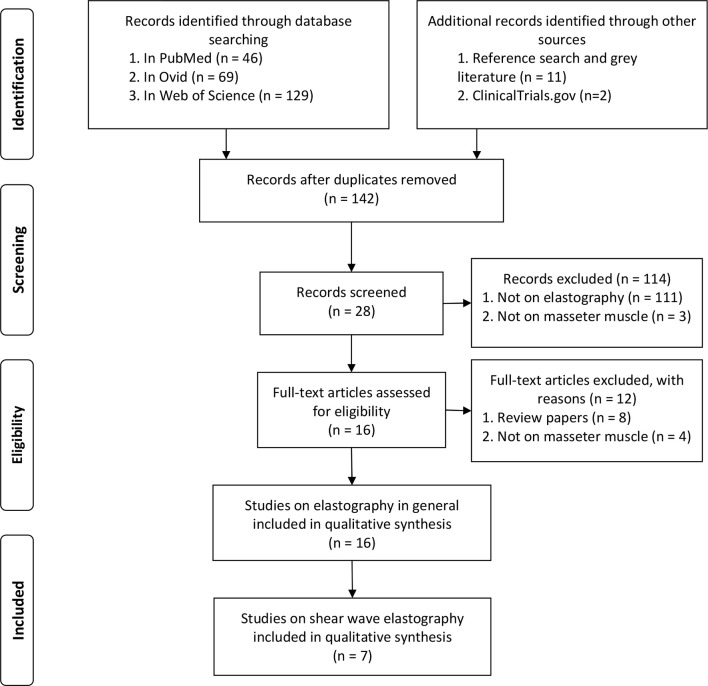
A total of 142 studies were identified, out of which 16 met PICOS criteria and were included in a qualitative analysis of the use of elastography for the assessment of the masseter muscle. For the evaluation of the shear wave elastography values, seven publications were considered. Additionally, two ongoing studies were identified from the Clinical Trials Database. The selection process is shown in the PRISMA flow diagram in Figure 1.
Figure 1.
PRISMA flow diagram of the systematic review protocol. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Study populations
A total of 16 studies on 573 subjects were analyzed. These studies included 486 healthy volunteers, 73 patients with TMD, 13 patients who underwent radiotherapy for nasopharyngeal carcinoma (this subgroup was compared to the healthy control group which was of interest in this review; for this reason, the whole study population was included), 1 patient with unilateral temporal myositis, 6 cadavers, and 2 phantoms. Only in two studies, the study groups comprised over 100 participants. Study cohorts were small with a mean number of subjects of 47.7 (median 33.5; range 10–176). The qualitative evaluation of elasticity values focused on studies using shear wave elastography. These studies included 436 (76% of the pooled number of all studies included) subjects with the mean sample size of 72.6 (median 46.5; range 10–176). The characteristics of the 16 studies included are presented in Table 2. The details of studies on shear wave elastography are depicted in Table 3.
Table 2.
Characteristics of the studies included in the systematic review
| Author | Technique | Study population | Results |
|---|---|---|---|
| Arda, 201120 | Shear wave elastography | 127 healthy volunteers (89 females, 38 males) with a mean age of 37.7 ± 9.11 years; range, 17–63 years) | The mean elasticity values were 10.4 ± 3.7 kPa for the masseter muscle. The same values in the longitudinal and transverse planes. Values in the longitudinal place were greater in males 10.8 ± 3.9 (range 4–20) than in females 10.3 ± 3.6 (range 2–23) with p value of 0.3. There was no correlation between age and elasticity of the muscle (p = 0.50). |
| Ariji, 200921 | Real-time sonographic elastography | 14 healthy volunteers (10 males and six females) and two female patients with TMD | The mean MSI of the right and left muscles in the healthy volunteers were 0.85 ± 0.44 and 0.74 ± 0.35. There was a significant correlation between the right and left MSI (R = 0.67, p < 0.001). The mean MSI was lower in males and in females (0.64 ± 0.34 and 1.05 ± 0.35; p = 0.008). MSI values of a 29-year-old female with TMD of the right masseter muscle were 2.06 for the right and 0.43 for the left masseter muscle. MSI values of a 46-year-old female with bilateral TMD were right 3.71 for the right and 0.22 for the left masseter muscle. |
| Ariji, 2012 | Strain sonoelastography | 35 healthy volunteers (20 males and 15 females) with a mean age of 41.4 ± 12.4 years; range, 25–65 years) | MEI was comparable for both masseter muscles with values of 0.79 ± 0.43 for the right side-and 0.74 ± 0.37 for the left side (p = 0.5737). A strong correlation was observed between the two sides (R = 0.7739; p < 0.001). |
| 8 TMD patients (2 males and six females) with unilateral myofascial pain with a mean age of 44.1 ± 9.6 years; range, 32–60 years) | MEI was higher for the symptomatic side-than for the contralateral side (1.13 ± 0.43 vs 0.77 ± 0.31; p = 0.03). The correlation between the two sides was insignificant (R = 0.4741; p = 0.2050). | ||
| Ariji, 201322 | Strain sonoelastography | ten healthy volunteers (8 males and two females) with a mean age of 40.9 ± 12.4 years; range, 26–54 years | MEI was comparable for both masseter muscles with values of 0.84 ± 0.21 for the right side-and 0.85 ± 0.21 for the left side. MEI increased significantly after exercise. |
| Ariji, 201623 | Strain sonoelastography | 37 TMD patients with myofascial pain (6 males and 31 females) with a median age of 45 years (range 9–83 years) | MEI was calculated at baseline and after 9.5 weeks of massage therapy. Patient were divided by response to the therapy. MEI in the therapy-effective was 1.33 at the baseline, 1.17 after the third treatment session, and 1.00 after the last treatment session. In the therapy-ineffective group, MEI were 1.20, 1.08, and 1.08, respectively. In the first group, values after the treatment were significantly lower in comparison to baseline, while in the second one, the differences were insignificant. |
| Ariji, 201623 | Strain and shear wave elastography | Phantoms and 30 healthy volunteers (21 males and nine females) with the median age of 31.5 years; range, 26–63 years | In healthy subjects, the average hardness on shear-wave sonoelastography was 42.82 ± 5.56 kPa at rest and 53.86 ± 8.26 kPa during jaw clenching. Differences between the left and right hardness values and between males and females were insignificant. |
| Badea, 201424 | Shear wave elastography | 25 healthy controls and 13 patients who had had radiotherapy for nasopharyngeal carcinoma (35 Gy minimum) | Shear waves velocities were measured in m/s. The values for relaxation and contraction in controls and patients presented no differences (1.79 ± 0.52 vs 1.72 ± 0.73; p = 0.72 and 1.70 ± 0.48 vs 1.59 ± 0.77; p = 0.98). Differences between groups were insignificant (1.79 ± 0.52 vs 1.65 ± 0.63; p = 0.78). |
| Damian, 2016 | Strain elastography | One case report of unilateral temporal myositis | Values not available. |
| Ewertsen, 201818 | Shear wave elastography | 10 healthy individuals (5 males and 5 females) with median age of 31 years and range from 22 to 46 years. | The mean shear wave speed in the parallel plane was 2.45 ± 0.25 m/s. The effect of sequence (day-to-day variation) and dominant side-were insignificant. The effect of scan plane in relation to muscle pennation was statistically significant. |
| Gotoh,2013 | Strain elastography | 10 healthy volunteers (8 males and 2 females) before, immediately after, and 10 min after static contraction | The EI ratios of the right and left masseter muscles were 0.84 ± 0.21 and 0.85 ± 0.21, respectively, before exercise, 1.75 ± 0.43 and 1.71 ± 0.43 immediately after exercise, and 0.90 ± 0.38 and 0.87 ± 0.36 10 min after exercise. There were no significant differences between the right and left EI ratios in any of the phases. The EI ratios immediately after exercise were significantly higher than those before exercise and 10 min after exercise on both right and left sides. |
| Herman, 201717 | Shear wave elastography | 176 volunteers with no known history of head and neck disease with a mean age of 48.8 years and range from 21 to 91 years. | The mean stiffness was 10.0 ± 4.3 kPa. A small increase with age was observed. BMI and weight had small effect on stiffness values. |
| Joy, 201525 | Shear wave elastography | 6 Thiel soft-embalmed human cadavers (3 males and 3 females) with a mean age at death of 81.3 ± 13.2 and range from 63 to 97 years. | Masseter 15.0 (95% CI: 6.3–35.5) kPa Sex, age at death and repeated measurements had no effect on elasticity. |
| Nakayama, 201526 | Strain elastography | Phantoms with elasticity of 20, 40 and 60 kPa. 25 healthy volunteers (10 females and 15 males) with a mean age of 30.8 ± 9.8 years and range from 20 to 53 years. |
No differences in EI ratios between males and females as well as between the right and left sides were observed. EI ration increased during clenching. Less variations were observed for the hard coupling agent. The EI ratios increased and showed wide variation with clenching. |
| Takashima, 201727 | Shear wave elastography | 26 females with bilateral masseter muscle pain who were classified as having TMD Ia (myofascial pain; n = 13) or Ib (myofascial pain with limited opening; n = 13) and healthy controls consisted of 24 females. Age range of TMD patients was 15 to 46 years, while controls 23–45 years. |
TMD Ia = 1.96 m/s (12.5 kPa) TMD Ib = 2.00 m/s (13.0 kPa) Healthy females = 1.27 m/s (5.25 kPa) Stiffness was significantly greater in TMD patients (p < 0.05). It was positively correlated with pain (p < 0.05) and negatively with maximum assisted mouth opening (p < 0.05) and painless mouth opening (p < 0.05). |
MEI, masseter muscle elasticity index calculated as the value of (the mean elasticity index of the masseter muscle)/(the mean elasticity index of the subcutaneous fat tissue) and was defined as the total hardness; MSI, masseter stiffness index defined as the ratio of elasticity of the fat tissues and elasticity of the masseter muscle; TMD, temporomandibular disorders; EI, elasticity index defined as the strain values of each area compared with the average strain value of the whole area of interest; EI ratio was calculated as the mean EI of scoring area divided by the mean EI of background.
Table 3.
Characteristics of studies on shear wave elastography
| Author | Device | Patients positioning | Study population | Elasticity values of the masseter muscle |
|---|---|---|---|---|
| Arda, 201 120 | Supersonic with a linear-array transducer with a frequency range of 6–13 MHz (Aix-en-Provence) | Patient in a supine position | 127 healthy volunteers | Total: 10.4 ± 3.7 kPa (range, 2–23) Males: 10.8 ± 3.9 kPa (4-20) Females: 10.3 ± 3.6 kPa (2-23) |
| Ariji, 201623 | Logic E9 with a 9 MHz linear array transducer; the coupling agent with Young’s modulus of 40 kPa was used (GE Healthcare) | Patient in a supine position | 30 healthy volunteers | At rest 42.82 ± 5.56 kPa At jaw clenching 53.86 ± 8.26 kPa |
| Badea, 201424 | ACUSON S2000 with an 8–14 MHz linear transducer; ARFI mode (Siemens) | Patients in a supine position with the head half extended | 25 healthy volunteers and 13 patients after radiotherapy | Central measurement – m/s Healthy at rest; right 1.87 ± 0.52 and left 1.6 ± 0.47 Healthy at contraction right 1.57 ± 0.54 and left 1.47 ± 0.53 Patients at rest; right 1.67 ± 0.6 and left 1.6 ± 0.34 Patients at contraction right 1.41 ± 0.52 and left 1.68 ± 0.9 |
| Ewertsen, 201818 | Logic E9 system with a 9 MHz linear array transducer (GE Healthcare) | Patient in a sitting position | 10 healthy volunteers | 2.45 ± 0.25 m/s |
| Herman, 201717 | Supersonic with a compact linear array transducer SL 15–4 (4–15 MHz) (Aix-en-Provence) |
Patient in a supine position | 176 healthy volunteers | 10.0 ± 4.3 kPa, median 9.85 kPa; |
| Joy, 201525 | Supersonic with a with a frequency range of 4–15 MHz (Aix-en-Provence) |
Cadavers in a supine position | Six cadavers | 15.0 (95% CI: 6.3–35.5) kPa |
| Takashima, 201727 | ACUSON S2001 with an 8–14 MHz linear transducer (Siemens) | Patient in a sitting position | 26 females with TMD and 24 healthy females | TMD Ia = 1.96 m/s (12.5 kPa) TMD Ib = 2.00 m/s (13.0 kPa) Healthy females = 1.27 m/s (5.25 kPa) |
TMD, temporomandibular disorders.
Devices used for the measurement of elasticity
Several devices were used to measure elasticity. For strain elastography, two machines were used. In one study, the EUB-7000 device (Hitachi Medical Systems, Tokyo, Japan) equipped with a 6–13 MHz wide bandwidth linear probe was used,28 while four other studies used LOGIQ E9 (GE Healthcare, Tokyo, Japan) equipped with a 4.5–15 MHz wide bandwidth linear active-matrix transducer (ML6-15-D).22,23,29,30
A wide variety of devices were used for shear wave elastography. Supersonic Imaging System Aixplorer ultrasound machine (Aix-en-Provence, France) was used either with a linear-array transducer with a frequency range of 6–13 MHz or 4–15 MHz.17,20,25 In two studies, a GE Logic E9 system with a 9 MHz linear array transducer was used.18,21 Ariji et al used a coupling agent with Young’s modulus of 40 kPa on the surface of the masseter muscle as the reference and presented the results in kPa.21 Another two studies were conducted using the ACUSON (S2000 or S20001) device (Siemens AG, Munich, Germany) with an 8–14 MHz linear transducer.24,27
The devices used in the studies for shear wave elastography are listed in Table 3.
Techniques used for the measurement of elasticity in masseter muscles
The masseter muscle was examined in two positions: supine or sitting position; the supine position was more frequently used for shear wave elastography, whereas the sitting position was used for strain elastography. Slight differences were noted across the studies when comparing the technique of scanning.
In the early study on masseter muscle elasticity conducted by a team from Japan, the patient was seated in an upright position with the head in the natural position. The measurements were acquired parallel to the anterior border of the muscle. The probe was placed 15 mm, or 20 mm in more recent studies, above the lower margin of the mandible. In patients with tender points in the masseter muscle, the points were included in the area scanned.22,28 In the study conducted by Ewerstsen et al, the patient was examined when sitting on a chair while the sonographer was sitting behind the patient. The recordings were performed after light pre-compression of the skin.18 Takashima et al who used the sitting position during examination evaluated three points (anterior border, center, and posterior border) of the masseter muscle body.27 Gotoh et al examined their patients in an upright position with the head in the natural position. They used a multiple focus technique with a focal range of 0.5–2.0 cm and image depth of 4.0 cm. Elasticity was measured 15 mm above the edge of the mandible.30
In both studies from 2016 performed by Ariji’s group, the patient lied in the supine position, but the head of the transducer was applied in the same manner. For better accuracy, each of the measurements was performed twice, and the results were averaged.21,23 The supine position dominated in studies using shear wave elastography.17,20,24–26 Additionally, Badea et al examined patients in a supine position with the head half extended and advised to refrain from swallowing during the examination. Nakayama et al instructed the patients to turn the head so that the side to be examined faced upwards and to relax the masseter muscle.26 Regarding contraction during the examination, Nakayama et al asked the patients to clench the mandible with the maximum force, while Badea et al asked the patients to make a moderate contraction.24,26
Most studies used some ultrasound gel on the skin over the muscle and carried out scanning without compressing the tissue.17,20,25,27
Elasticity values of the masseter muscle
Two studies showed that the elasticity of the masseter muscle differs significantly not only from that of different organs but also from that of different muscles. Arda et al20 compared elasticity values in different locations of the body and found a significant difference between them in healthy people. The lowest values were recorded in the spleen (2.9 ± 1.8 kPa) and the highest in the Achilles tendons (51.5 ± 25.1 kPa). Moreover, considerable differences were noted between the same tissues, but with different locations and functions, e.g. elasticity for the masseter muscle was 10.4 ± 3.7 kPa, while for the supraspinatus muscle, it was three times higher and reached 31.2 ± 13 kPa.20 Herman et al reported a difference in elasticity across different organs; however, the difference between the sternocleidomastoid muscle (9.89 ± 4.1 kPa) and the masseter muscle (10.04 ± 4.3 kPa) was small.17
Overall, in studies on humans, four studies expressed elasticity values of the normal masseter muscle in kPa17,20,21,27 while three studies used velocity (m/s) to report elasticity.15,20,25 Additionally, one study on cadavers reported elasticity in kPa.25
For kPa, the values at rest in healthy people ranged from 5.25 kPa in the study by Takashima et al27 to 42.82 ± 5.56 kPa in the study by Ariji et al.21 It is worth noting that the studies were conducted using different devices and coupling agents. The study by Arda et al20 and Herman et al17 showed similar results (10.4 ± 3.7 and 10.0 ± 4.3 kPa). Both research teams used the Supersonic device. Only one study reported values of 12.5–13 kPa for patients with TMD.27
For m/s, the values at rest in healthy people ranged from 1.27 m/s in the study by Takashima et al27 to 2.45 m/s in the study by Ewertsen et al.18 Of these studies, two were conducted using ACUSON Siemens devices but with different models, and one study used Logic E9 from GE Healthcare.
The values of elasticity of the masseter muscle are presented in Table 2.
Factors affecting elasticity values of the masseter muscle
The impact of age remains unclear. One study found no correlation between age and elasticity of the muscle,20 while another study noted a small increase in elasticity with age.17 Regarding sex, three studies reported no differences in elasticity between males and females.20,25,26 Only one study reported significantly lower values of the masseter stiffness index in males than in females.28 Some studies investigated whether there are differences between both masseter muscles. In most cases, a significant correlation between the right and left masseter stiffness index in healthy volunteers was observed, indicating that elasticity of both normal muscles is similar.21,22,26,28–30 Differences between the sides of masseter muscles appeared for pathologies. In patients with TMD, the masseter muscle elasticity index was higher for the symptomatic side than for the contralateral side.22,28 More detailed report by Takashima et al showed significantly increased stiffness in patients with TMD as well as a positive correlation of stiffness with pain and a negative correlation with maximum assisted mouth opening and painless mouth opening.27 The history of radiotherapy did not affect elasticity values. Exercise increased the masseter muscle elasticity index.29 The effect of contraction or clenching is not clear because of conflicting results.21,24,26
Discussion
The present systematic review shows small evidence for the use of elastography to assess the masseter muscle. Reports available in the literature are heterogeneous because the studies were conducted using different devices, protocols, and health conditions of patients. Additionally, they report results of elastography with different units, which cannot be compared directly.
The main limitation of this review is the small number of studies included in the qualitative evaluation of elastography of the masseter muscle. Large heterogeneity across the studies precluded not only determining normative values but also comparing elasticity values in different pathologies. Because of the sparsity of data, also studies on cadavers and phantoms were included to show the background of the use of elastography as well as to capture all possible evidence in this scope. Joy et al25 used Thiel embalmed cadavers which are used for medical research as this method preserves greater flexibility compared to formalin-embalmed cadavers. In the phantom study, a muscle phantom of known elasticity was used and compared to sonographic results obtained from the measurement of healthy volunteers.26 This study proved that on one hand, measurements are reliable and on the other, that can be used to measure tissue hardness in humans. Due to the heterogeneity of the studies, authors were unable to conduct a meta-analysis on the change in the masseter muscle elasticity between healthy people and patients with TMD.
Different measures of elasticity were used across studies. Masseter muscle elasticity index and elasticity index as well as masseter stiffness index (MSI) are defined in Table 2; they were used for strain sonoelastography and real-time sonographic elastography. The results of shear wave elastography were presented in two units m/s and kPa. These two units represent a different approach to measurement; m/s shows the shear wave speed with which the waves propagate in a given tissue, while kPa is calculated from the velocity of the shear waves using Young’s elastic modulus. Because the retrospective calculation of kPa from m/s and vice versa31 is not feasible, authors recommend providing results using either kPa or both units.
The studies included in the present review analyzed several factors that were important for the assessment of masseter muscles in patients diagnosed with TMD. First, a correlation between the left and right sides of the masseter muscle was confirmed for healthy people. Second, the masseter muscle affected by TMD presented with increased values of elasticity. Furthermore, elasticity values correlated with the severity of TMD symptoms. Finally, a strong correlation between actual and measured hardness confirmed by phantom studies proves the high reliability of elastography. The noninvasive nature of this examination and real-time display of results increase its potential to be accepted by patients. All these features suggest that elastography has the potential of being a valuable tool for the assessment of muscle-related TMD and monitoring the results of the management.
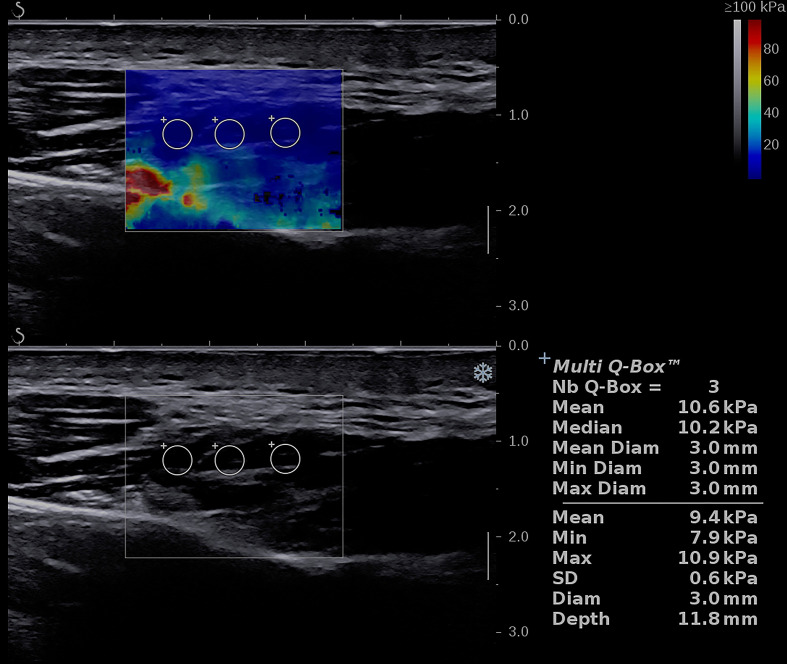
The European Society of Radiology highlights the need for the development of new imaging biomarkers that have sufficiently high accuracy and reproducibility in detecting pathological processes.32 From the European Society of Radiology perspective, elastography still requires to be standardized and validated by gathering evidence from large studies. Currently, two ongoing studies are in progress and have been registered at ClinicalTrials.gov. Both studies aim to assess shear wave elastography. The first study will enroll 20 participants,31 while the second will enroll 150 participants33 and is focused on determining elasticity values in patients with TMD and healthy subjects. In authors institution, attempts have been made to gain experience in using shear wave elastography to examine the masseter muscle. An example of a shear wave image of the masseter muscle of a healthy person is shown in Figure 2. New studies are showing a growing interest in this modality with the aim to improve oral health in patients with TMD.
Figure 2.
Image shows shear wave elastography of the masseter muscle of healthy volunteer (33-year-old male). Ultrasound linear probe was placed longitudinally to the long axis of the muscle and the presented image was obtained. Three ROIs of 3 mm in diameter each were placed in the central aspect of the muscle belly and provided three independent measurements. The mean elasticity of the masseter muscle calculated from 3 measurements was 9.4 kPa.
Currently, there is no reliable method for the assessment of the masseter muscle in patients with TMD. However, several attempts have been made and investigated in clinical trials. The use of diffusion-weighted MRI showed that it could be useful to evaluate myalgia of the masticatory muscles.34 Electromyography is another method which can help to make a proper diagnosis, exclude other pathologies and measure the severity of pain.34 It is worth noting that TMD is a complex condition in which an interplay of several factors and overlap of other conditions can be observed. Complete assessment of the patient requires checking the conditions of temporomandibular joint which can be done with ultrasound35 or magnetic resonance.36
Conclusion
Elastography is a promising tool for the assessment of the masseter muscle elasticity for improved diagnosis of TMD and for monitoring the effects of management; however, the evidence is insufficient. Studies on larger groups are needed to properly determine the accuracy of shear wave elastography for the characterization of masticatory muscle disorders.
Footnotes
Funding: This study is a part of the research project titled “Shear Wave Sonoelastography in the Diagnosis and Management of the Masseter Muscles Disorders” funded by the National Science Centre, Poland (Funding ID: PREL.B160.18.007).
Contributor Information
Anna Olchowy, Email: ania.olchowy@gmail.com.
Mieszko Wieckiewicz, Email: m.wieckiewicz@onet.pl.
Efraim Winocur, Email: winocur@tauex.tau.ac.il.
Marzena Dominiak, Email: marzena.dominiak@umed.wroc.pl.
Ilona Dekkers, Email: I.A.Dekkers@lumc.nl.
Mateusz Łasecki, Email: m.c.lasecki@wp.pl.
Cyprian Olchowy, Email: cyprian.olchowy@gmail.com.
REFERENCES
- 1.Sciote JJ, Raoul G, Ferri J, Close J, Horton MJ, Rowlerson A. Masseter function and skeletal malocclusion. Rev Stomatol Chir Maxillofac Chir Orale 2013; 114: 79–85. doi: 10.1016/j.revsto.2013.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Widmer CG, English AW, Morris-Wiman J. Developmental and functional considerations of masseter muscle partitioning. Arch Oral Biol 2007; 52: 305–8. doi: 10.1016/j.archoralbio.2006.09.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Janal MN, Raphael KG, Nayak S, Klausner J. Prevalence of myofascial temporomandibular disorder in US community women. J Oral Rehabil 2008; 35: 801–9. doi: 10.1111/j.1365-2842.2008.01854.x [DOI] [PubMed] [Google Scholar]
- 4.Jussila P, Kiviahde H, Näpänkangas R, Päkkilä J, Pesonen P, Sipilä K, et al. . Prevalence of temporomandibular disorders in the Northern Finland birth cohort 1966. J Oral Facial Pain Headache 2017; 31: 159–64. doi: 10.11607/ofph.1773 [DOI] [PubMed] [Google Scholar]
- 5.de Melo Júnior PC, Aroucha JMCNL, Arnaud M, Lima MGdeS, Gomes SGF, Ximenes R, et al. . Prevalence of TMD and level of chronic pain in a group of Brazilian adolescents. PLoS One 2019; 14: e0205874.. doi: 10.1371/journal.pone.0205874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wieckiewicz M, Grychowska N, Wojciechowski K, Pelc A, Augustyniak M, Sleboda A, et al. . Prevalence and correlation between TMD based on RDC/TMD diagnoses, oral parafunctions and psychoemotional stress in Polish university students. Biomed Res Int 2014; 2014: 1–7. doi: 10.1155/2014/472346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Osiewicz MA, Lobbezoo F, Loster BW, Loster JE, Manfredini D. Frequency of temporomandibular disorders diagnoses based on RDC/TMD in a Polish patient population. Cranio 2018; 36: 304–10. doi: 10.1080/08869634.2017.1361052 [DOI] [PubMed] [Google Scholar]
- 8.Al-Jundi MA, John MT, Setz JM, Szentpétery A, Kuss O. Meta-Analysis of treatment need for temporomandibular disorders in adult nonpatients. J Orofac Pain 2008; 22: 97–107. [PubMed] [Google Scholar]
- 9.Vainionpää R, Kinnunen T, Pesonen P, Laitala M-L, Anttonen V, Sipilä K. Prevalence of temporomandibular disorders (TMD) among Finnish prisoners: cross-sectional clinical study. Acta Odontol Scand 2019; 77: 264–8. doi: 10.1080/00016357.2018.1535660 [DOI] [PubMed] [Google Scholar]
- 10.Hamamoto DT, Rhodus NL. Methamphetamine abuse and dentistry. Oral Dis 2009; 15: 27–37. doi: 10.1111/j.1601-0825.2008.01459.x [DOI] [PubMed] [Google Scholar]
- 11.Schiffman E, Ohrbach R. Executive summary of the diagnostic criteria for temporomandibular disorders for clinical and research applications. J Am Dent Assoc 2016; 147: 438–45. doi: 10.1016/j.adaj.2016.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peck CC, Goulet J-P, Lobbezoo F, Schiffman EL, Alstergren P, Anderson GC, et al. . Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J Oral Rehabil 2014; 41: 2–23. doi: 10.1111/joor.12132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Creze M, Nordez A, Soubeyrand M, Rocher L, Maître X, Bellin M-F. Shear wave sonoelastography of skeletal muscle: basic principles, biomechanical concepts, clinical applications, and future perspectives. Skeletal Radiol 2018; 47: 457–71. doi: 10.1007/s00256-017-2843-y [DOI] [PubMed] [Google Scholar]
- 14.Nenadic I, Urban MW, Greenleaf JF, Gennisson JL, Bernal M, Tanter M. Ultrasound elastography for biomedical applications and medicine: Wiley; 2016. [Google Scholar]
- 15.Hirsch S, Braun J, Sack I. Magnetic Resonance Elastography: Physical Background and Medical Applications: Wiley; 2017. [Google Scholar]
- 16.Magnetic Resonance Elastography New York Heidelberg Dordrecht London. Springer, 2014;. [Google Scholar]
- 17.Herman J, Sedlackova Z, Vachutka J, Furst T, Salzman R, Vomacka J. Shear wave elastography parameters of normal soft tissues of the neck. Biomedical Papers 2017; 161: 320–5. doi: 10.5507/bp.2017.024 [DOI] [PubMed] [Google Scholar]
- 18.Ewertsen C, Carlsen J, Perveez MA, Schytz H. Reference values for shear wave elastography of neck and shoulder muscles in healthy individuals. Ultrasound Int Open 2018; 04: E23–9. doi: 10.1055/s-0044-102013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moher D, Liberati A, Tetzlaff J, Altman DG, .PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006–12. doi: 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 20.Arda K, Ciledag N, Aktas E, Arıbas BK, Köse K. Quantitative assessment of normal soft-tissue elasticity using shear-wave ultrasound elastography. AJR Am J Roentgenol 2011; 197: 532–6. doi: 10.2214/AJR.10.5449 [DOI] [PubMed] [Google Scholar]
- 21.Ariji Y, Nakayama M, Nishiyama W, Nozawa M, Ariji E. Shear-Wave sonoelastography for assessing masseter muscle hardness in comparison with strain sonoelastography: study with phantoms and healthy volunteers. Dentomaxillofac Radiol 2016; 45: 20150251. doi: 10.1259/dmfr.20150251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ariji Y, Gotoh A, Hiraiwa Y, Kise Y, Nakayama M, Nishiyama W, et al. . Sonographic elastography for evaluation of masseter muscle hardness. Oral Radiol 2013; 29: 64–9. doi: 10.1007/s11282-012-0111-3 [DOI] [Google Scholar]
- 23.Ariji Y, Nakayama M, Nishiyama W, Ogi N, Sakuma S, Katsumata A, et al. . Can sonographic features be efficacy predictors of robotic massage treatment for masseter and temporal muscle in patients with temporomandibular disorder with myofascial pain? Cranio 2016; 34: 13–19. doi: 10.1179/2151090314Y.0000000037 [DOI] [PubMed] [Google Scholar]
- 24.Badea I, Tamas-Szora A, Chiorean I, Fildan F, Ciulea E, Badea M. Quantitative assessment of the masseter muscle's elasticity using acoustic radiation force impulse. Med Ultrason 2014; 16: 89–94. doi: 10.11152/mu.201.3.2066.162.ib1asz2 [DOI] [PubMed] [Google Scholar]
- 25.Joy J, McLeod G, Lee N, Munirama S, Corner G, Eisma R, et al. . Quantitative assessment of Thiel soft-embalmed human cadavers using shear wave elastography. Ann Anat 2015; 202: 52–6. doi: 10.1016/j.aanat.2015.06.007 [DOI] [PubMed] [Google Scholar]
- 26.Nakayama M, Ariji Y, Nishiyama W, Ariji E. Evaluation of the masseter muscle elasticity with the use of acoustic coupling agents as references in strain sonoelastography. Dentomaxillofac Radiol 2015; 44: 20140258. doi: 10.1259/dmfr.20140258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takashima M, Arai Y, Kawamura A, Hayashi T, Takagi R. Quantitative evaluation of masseter muscle stiffness in patients with temporomandibular disorders using shear wave elastography. J Prosthodont Res 2017; 61: 432–8. doi: 10.1016/j.jpor.2017.01.003 [DOI] [PubMed] [Google Scholar]
- 28.Ariji Y, Katsumata A, Hiraiwa Y, Izumi M, Iida Y, Goto M, et al. . Use of sonographic elastography of the masseter muscles for optimizing massage pressure: a preliminary study. J Oral Rehabil 2009; 36: 627–35. doi: 10.1111/j.1365-2842.2009.01977.x [DOI] [PubMed] [Google Scholar]
- 29.Ariji Y, Nakayama M, Taguchi A, Gotoh A, Kise Y, Katsumata A, et al. . Intramuscular changes of soft and hard areas after low-level static contraction of the masseter muscle and the correlations with muscle hardness and increase in water content: evaluations with sonographic elastography and magnetic resonance imaging. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: 354–61. doi: 10.1016/j.oooo.2013.05.017 [DOI] [PubMed] [Google Scholar]
- 30.Gotoh A, Ariji Y, Hasegawa T, Nakayama M, Kise Y, Matsuoka M, et al. . Sonographic elastography for assessing changes in masseter muscle elasticity after low-level static contraction. Oral Radiol 2013; 29: 140–5. doi: 10.1007/s11282-012-0119-8 [DOI] [Google Scholar]
- 31. NCT02425839 Assessment of correlation between changes of shear wave elastography and surface electromyogram of the masseter (Everest. 2015;.
- 32.Heller CG, Myers GB. The male climacteric, its symptomatology, diagnosis and treatment: use of urinary gonadotropins, therapeutic test with testosterone proprionate and testicular biopsies in delineating the male climacteric from psychoneurosis and psychocenic impotence. Journal of the American Medical Association 1944; 126: 472–7. [Google Scholar]
- 33. NCT03844854 Shear wave sonoelastography in the diagnosis and management of the masseter muscles disorders. 2019;.
- 34.Sawada E, Kaneda T, Sakai O, Kawashima Y, Ito K, Hirahara N, et al. . Increased apparent diffusion coefficient values of masticatory muscles on diffusion-weighted magnetic resonance imaging in patients with temporomandibular joint disorder and unilateral pain. J Oral Maxillofac Surg 2019; 77: 2223–9. doi: 10.1016/j.joms.2019.04.031 [DOI] [PubMed] [Google Scholar]
- 35.Razek AAKA, Al Mahdy Al Belasy F, Ahmed WMS, Haggag MA. Assessment of articular disc displacement of temporomandibular joint with ultrasound. J Ultrasound 2015; 18: 159–63. doi: 10.1007/s40477-014-0133-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rao VM, Liem MD, Farole A, Razek AA. Elusive "stuck" disk in the temporomandibular joint: diagnosis with MR imaging. Radiology 1993; 189: 823–7. doi: 10.1148/radiology.189.3.8234710 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.