ABSTRACT
Over the course of several weeks following the first diagnosed case of COVID-19 In the U.S., the virus rapidly spread across our communities. It became evident that the pandemic was going to place a severe strain on all components of the U.S. healthcare system, and we needed to adapt our daily practices, training and education. In the present paper we discuss four pillars to face a pandemic: surgical and outpatients service, tele-medicine and tele-education. In the face of unprecedented risks in providing adequate health care to our patients during this current, evolving public health crisis of COVID-19, alternative patient management tools such as telemedicine services, allow clinicians to maintain necessary patient rapport with their healthcare provider when required. As a subspecialty, urology should take full advantage of telehealth and teleeducation at this juncture. As tele-urology and tele-education can obviate the potential drawbacks of “social distancing” as it pertains to healthcare, the platform can also reduce the risk of COVID-19 spread, without compromising quality urological care and educational efforts. Telehealth can bring urologists and their patients together, perhaps closer than ever.
Keywords: COVID-19 diagnostic testing [Supplementary Concept]; Telemedicine; Surgical Procedures, Operative; Urology
INTRODUCTION
The novel coronavirus known as severe acute respiratory syndrome corona virus-2 (SARS-CoV-2) has rapidly spread across the globe causing a pandemic known as the Coronavirus Disease 2019 (COVID-19) (1). On March 11, 2020, the World Health Organization (WHO) defined COVID-19 as a pandemic, and two days later, the President of the United States (U.S.) declared the COVID-19 outbreak a national emergency.
Since the first reported case in the U.S. (2), the healthcare community had been bracing for possible community spread of COVID-19 and its potential impact on the U.S. healthcare system. The U.S. was warned of what to expect by our healthcare colleagues across the globe, especially in Italy, where the virus' impact had been felt several weeks earlier than the U.S. (3). As in Asia and in some European countries, widespread transmission of COVID-19 in the U.S. was likely to occur with the majority of the U.S. population becoming exposed to the virus and potentially contracting COVID-19.
Over the course of several weeks following the first diagnosed case of COVID-19 in the U.S., the virus rapidly spread across our communities. It became evident that the pandemic was going to place a severe strain on all components of the U.S. healthcare system, and we needed to adapt our practices quickly to allow us to care for a surging number of COVID-19 positive patients. According to the Centers for Disease Control and Prevention (CDC), more cases of COVID-19 are likely to be identified in the U.S. in the next weeks, requiring stricter measures to reduce community spread. Moreover, the pandemic is placing a heavy demand on resources such as personal protective equipment (PPE), intensive care unit (ICU) beds, ventilators, medical supplies, as well as appropriately trained health care professionals. It became obvious that healthcare systems needed to reorganize to avoid being overwhelmed.
Impact of COVID-19 on the surgical service
On March 18th, 2020 the Centers for Medicare εt Medicaid Services (CMS), a federal agency within the U.S. Department of Health and Human Services, formally released recommendations to delay all elective surgeries and non-essential procedures. In response, professional bodies began to make recommendations to help in re-prioritizing surgical cases and healthcare systems began to create an individualized plan for their institution to prepare for a surge in COVID-19 cases and how they would meet the challenges (4).
Urologists across the U.S. began deferring elective procedures and triaged their surgical cases (5, 6). Publications addressing management of genitourinary cancer care as well as kidney stone patients during the COVID-19 pandemic have helped guide our care of the urologic patient (3, 7). It is important to delay non-urgent cases not only to conserve medical resources but also to protect our patients as well as healthcare workers from potentially being exposed to COVID-19. In the worst hit regions of the U.S. such as New York, urologists were redeployed to assist with care of COVID-19 patients (8, 9). But even for those who are not redeployed to the emergency room and ICU, there are several additional preoperative considerations when operating during the COVID-19 era. The surgeon must weigh the risks to the patient from their underlying disease necessitating surgery versus the risk from possible COVID-19 exposure. A significant population of urologic patients are older with multiple comorbidities, placing them at a greater risk of worse outcomes if they were to contract the novel coronavirus (10). Those patients with genitourinary malignancies face even greater risk than their age matched cohort, as cancer patients are noted to have higher risk and more severe outcomes in a study from China (11). There is a national shortage of blood products during this pandemic and one must be judicious with transfusing their patients as well as weight the need for blood products during the perioperative period when considering proceeding with a surgery (12). As studies have indicated, a significant portion, up to 60% of patients whom are infected with COVID-19, may display minimal to no symptoms, yet be contagious and further spread the virus (13). It is prudent to screen every patient scheduled for a surgical procedure with not only with a comprehensive history and physical exam, but also with COVID-19 screening 1-3 days preoperatively to identify potential asymptomatic carriers and consequently delay their procedure as these patients are shown to have a 20% mortality rate if undiagnosed and undergo surgery during the incubation period (14).
Patients that need urgent surgeries are brought to the operating room (OR) with stringent rules and restrictions in place to mitigate the spread of COVID-19. Specific PPE guidelines have been adopted across U.S. hospitals to appropriately resource the insufficiently available masks and gowns while protecting their clinicians and staff. Aerosolizing procedures such as intubation require N95 masks with face shields for all non-COVID positive patients, while a Powered Air-Purifying Respirator (PAPR) is required for all COVID-19 positive patients (15). All staff except for the anesthesia team are asked to step outside the OR for intubation as well as extubation to minimize exposure risk. In addition, for those patients whom are suspect or have tested positive, staff should remain outside the room for at least 18 minutes to remove 99% of aerosolized virus in a negative pressure room (assumes ACH 15/hr) (16). Urologists must be aware that the virus is shed not only during aerosolizing procedures, but can also be shed in blood, urine and feces (17). During laparoscopic and robotic procedures, there is a theoretical risk of aerosolizing the virus therefore caution must be taken to suction gases into a closed system during de-sufflation of pneumo-peritoneum, and the OR staff must wear N95 masks throughout the case to limit possible exposure (18). For those performing robotic surgeries, surgeons should consider donning masks and gloves at the surgical console to minimize the exposure to COVID-19. It is critical for teaching institutions to protect their trainees and limit exposure during this COVID-19 pandemic. Academic institutions have modified and restructured their training programs to minimize exposure to their residents and fellows, as well as avoid any non-essential personnel such as visiting urologists, medical students, and researchers in the OR (19).
Post-operative care of our patients is also different during the COVID-19 era as entire hospital wards have been transformed to care for COVID patients. Urology patients are placed on non-COVID floors, but in some cases, this can lead to ancillary care provided by nurses not familiar with the management of a post-operative urology patient. Hospitals across the U.S. have adopted stern policies limiting any patient visitors per CDC recommendations and this has led to our surgical patients unable to have visitors during their hospital stay (20). Further, the patient care team must carefully weigh the need for post-hospitalization rehabilitation for our patients as placement to nursing homes and long-term care facilities can subsequently place them at a higher risk of contracting COVID-19. Additionally, it is critical to inquire about our patients after discharge regularly either via phone call or telemedicine to confirm an uneventful recovery while convalescing at home to help minimize possible readmissions.
Impact of COVID-19 on the outpatient service
No facet of the U.S. healthcare system has been spared by the COVID-19 pandemic and outpatient services are no different. As we continue to make every effort to mitigate the spread of the virus, it is important to maintain social distancing, even within the hospital and outpatient clinics. As healthcare systems began to restructure and organize their resources and personnel to prepare for a surge in COVID-19 patients, outpatient visits were reduced to only those deemed absolutely necessary while all others were switched over to the rapidly adopted telemedicine platform. On March 17, 2020 CMS announced it had lifted restrictions on billing for telemedicine visits facilitating the wide adoption of telehealth during the pandemic (21). Minimizing traffic at the outpatient clinics allowed for appropriate social distancing, medical resource conservation, and limiting exposure risks to patients and staff alike. Based on CDC guidelines, patients checking in for in-person visits were screened for any symptoms of COVID-19 over the phone at the time of scheduling their appointment as well as upon arrival to the facility and are provided with a mask at check-in to mitigate the spread of the infection (22). All front and back office staff should wear masks and PPE as indicated by CDC guidelines to minimize any exposure. While most office visits were changed to telemedicine visits, there are patients still requiring clinic procedures and in-person visits. Recommendations for triaging office procedures have been made by Katz et. al as well as Howard et. al. to help guide the efforts to limit any non-urgent procedures (5, 23). While this transition away from in-person clinic visits has presented new challenges for the provider and the patient, the U.S. healthcare community has risen to meet these demands with some changes likely to stay in place beyond the COVID era.
Impact of COVID-19 on Telemedicine
Following the concept and step-wise restrictions of #Stayathome mandates, millions of Americans have had to restrict their daily activities, avoiding public areas, public transportation, and reduce physical contact to limit the risk of person-to-person transmission. Under these circumstances, telehealth represents the venue for reaching these goals without limiting access to healthcare or compromising patients' health unduly. The concept of the tele-visit employs telecommunication tools to share healthcare information between patients and providers. Several communication tools have been described for two-way audio-video platforms such as computers, touchpads, and smartphones (24).
According to a 2019 survey, only 10% of Americans have used telehealth for a virtual consultation with lack of access (34.6%) and poor awareness (39.7%) of telehealth options as the primary hurdles to adoption (25). The COVID-19 outbreaks and the restrictions suggested by the CDC with stepwise implementation by government agencies for containing the spread of contagion would ultimately bring telehealth into the mainstream of practices, thereby reshaping the future of access to healthcare. In this setting, tele-urology could provide an alternative setting to evaluate post-operative patients. The tele-visit would make it easier for patients and providers to connect, while reducing person-to-person contact with public transportation, in various waiting rooms, hospitals, and clinics, including the urologist and their staff.
Patient acceptance and perceptions of telehealth for new patient visits, follow-up visits, clinic, and hospital consultations have been previously explored, showing potential for improving the urologic continuum of care. Younger patients (mean 62 vs. 65 years), higher education level (77% vs. 65%), previous exposure to video-conference tools (57% vs. 38%), those travelling longer distances (>90 min; 69% vs. 58%), and days missed from work (>1 day; 39% vs. 29%), have been found to prefer the tele-visit setting for sharing new symptoms and sensitive information (26). Viers et al. reported the use of tele-visits for patients following prostatectomy. No significant differences were found in patient perception of the quality of care nor satisfaction with the visit, with similar patient-to-provider face time (14.5 min vs. 14.3 min), patient wait time (18.4 min vs. 13.0 min), and total time devoted to care (17.9 min vs. 17.8 min). Likewise, there were no differences with the urologists' perspective. Further, overall costs to patients have been found to be lower with the tele-visit (27).
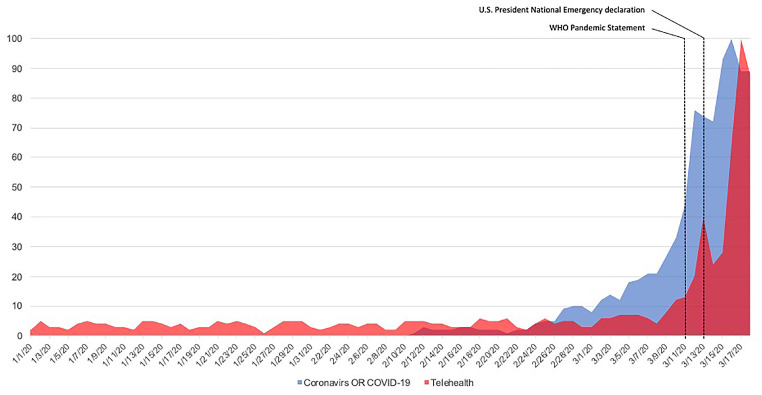
While tele-urology showed encouraging results, up until now it had only been offered as an option. In our current pandemic setting with increasing spread of the COVID virus and mobility restrictions, it might be necessary to employ telehealth to maintain patient access to healthcare. As regulatory barriers for the use of telehealth systems have been tabled for now, urologists should take the opportunity to attest to the viability and benefit of telehealth. Web-engine queries for “telehealth” have increased in the past months, paralleled with the increasing searches for Coronavirus information (Figure-1), these trends cannot be ignored as they are beneficial in promoting a new age of productive healthcare delivery options. At the USC Institute of Urology, we started our telehealth program in 2017. Details of the tele-visit flowchart are reported in Table-1.
Figure 1. Google trends analysis for “Tele-Health OR Telehealth” and Corona Virus. Data are reported in relative search volume.
Table 1. Tele-visit flowchart.
|
Impact of COVID-19 on Tele-Education
In the COVID-19 era, there has been an increase demand for educational opportunities as clinical volume has slowed. The American Urological Association (AUA) has previously established an online Core Curriculum, which is updated regularly and available to all AUA members. However, new challenges have risen in medical education with the limits in place due to social distancing. Regional and national conferences have been cancelled, including the AUA Annual Meeting. In response, the AUA has published not only the abstracts from the meeting, but also the surgical videos to enhance virtual learning. A webinar program, AUA Live, is being developed as well.
While virtual learning is being increasingly used in post-graduate medical education, it has been a mainstay of many medical school programs for years, especially during the pre-clinical curriculum (28). Many students have preferred the flexibility of recorded lectures in lieu of large in-person lecture halls. However, post-graduate medical education is more traditionally in-person, with clinical experiences, teaching conferences, grand rounds, and morbidity and mortality conferences (29). Now, conferences and presentations have been shifted to virtual formats. Trainees are often included in telehealth visits to maintain their clinical exposure. Surgical residents cannot replace their operative experience, but some are able to augment their learning with simulators (30). Several surveys have been distributed to assess the impact of COVID-19 in urological training, in particular. A questionnaire sent to all Italian urology residents found that on-call activity was not significantly changed, but there were dramatic reductions in outpatient visits and diagnostic procedures for residents at all levels. Senior residents had compromised volumes of surgical procedures (31). A U.S. based survey from the University of Texas, Houston, is pending publication of these results. A survey of urology residents from 58 countries reported that the preferred educational content included guideline updates and surgical videos. The European Society of Residents in Urology published educational alternatives to compromised activities. For example, to temporarily replace surgical activity, the European Association of Urology education section has online courses, surgery videos, and webinars, and the Surgery in Motion School has videos of surgical demonstrations (32).
To address the demand for high-quality education, a number of programs have started online lecture series. Several institutions have publicized their previously internal lectures, while others have created brand new programs. With the increased usage of tele-conferencing applications, inviting speakers from across the country, and even internationally, has become easier to organize and promote. Moreover, these lectures are readily available to those in practice and not solely limited to trainees within academic institutions. A list of publicly available cost-free lecture series is included in Table-2.
Table 2. List of available free lecture series.
| Institution/Group | Name | Link |
|---|---|---|
| Urology institute at University Hospitals/ Case Western Reserve University and SUNY Upstate | Genitourinary Reconstruction Online Learning Series | https://www.uhhospitals.org/medical-education/urology-medical-education/urology-residency/overview/online-learning-series |
| Educational Multi-institutional Program for instructing REsidents (EMPIRE) | Urology Lecture Series | https://nyaua.com/empire/ |
| Memorial Sloan Kettering Cancer Center | Science Spotlight | https://www.mskcc.org/research/ski/education-training/sciencespotlight |
| National Cancer institute, Urologic Oncology Branch | Urologic Oncology Grand Rounds | https://twitter.com/NCiCCR_UroOnc |
| Society of Women in Urology | TeleURO AFRICA 2020 | https://swiu.org/swiu-news/teleuro-africa-fpmrs.aspx |
| University of California, Irvine | Grand Rounds | http://urology.uci.edu/education_grandrounds.shtml |
| University of California, San Francisco | Urology Collaborative Online Video Didactics (COViD) | https://urologycovid.ucsf.edu/ |
| University of California, San Francisco | Pediatric Urology Fellowship Lectures Online (PedsUroFLO) | https://pedsuroflo.ucsf.edu/ |
| University of Southern California | Urology 60 Minutes | https://www.youtube.com/channel/UCuOf9gTZLObAM7HXHdUSA_Q |
CONCLUSIONS
In the face of unprecedented risks in providing adequate health care to our patients during this current, evolving public health crisis of COVID-19, alternative patient management tools such as telemedicine services, allow clinicians to maintain necessary patient rapport with their healthcare provider when required. As a subspecialty, urology should take full advantage of telehealth and tele-education at this juncture. As tele-urology and tele-education can obviate the potential pitfalls of “social distancing” as it pertains to healthcare, the platform can also reduce the risk of COVID-19 spread, without compromising quality urological care and educational efforts. Telehealth can bring urologists and their patients together, perhaps closer than ever.
REFERENCES
- 1.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]; 1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020; 382:1708-20. [DOI] [PMC free article] [PubMed]
- 2.Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]; 2. Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. First Case of 2019 Novel Coronavirus in the United States. N Engl J Med. 2020; 382:929-36. [DOI] [PMC free article] [PubMed]
- 3.Montorsi F. We Should Not Ignore What Scientific Articles are Telling US: A Lesson from the Italian COVID-19 Experience. J Urol. 2020;204:5–6. doi: 10.1097/JU.0000000000001069. [DOI] [PMC free article] [PubMed] [Google Scholar]; 3. Montorsi F. We Should Not Ignore What Scientific Articles are Telling US: A Lesson from the Italian COVID-19 Experience. J Urol. 2020;204:5-6. [DOI] [PMC free article] [PubMed]
- 4.CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. Centers for Medicare & Medicaid Services; 2020. [No Auhors] [Internet] Available at. < https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental>. [Google Scholar]; 4. [No Auhors]. CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. Centers for Medicare & Medicaid Services 2020. [Internet]. Available at. <https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental>
- 5.Goldman HB, Haber GP. Recommendations for Tiered Stratification of Urological Surgery Urgency in the COVID-19 Era. J Urol. 2020;204:11–13. doi: 10.1097/JU.0000000000001067. [DOI] [PMC free article] [PubMed] [Google Scholar]; 5. Goldman HB, Haber GP. Recommendations for Tiered Stratification of Urological Surgery Urgency in the COVID-19 Era. J Urol. 2020;204:11-3. [DOI] [PMC free article] [PubMed]
- 6.Stensland KD, Morgan TM, Moinzadeh A, Lee CT, Briganti A, Catto JWF, et al. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur Urol. 2020;77:663–666. doi: 10.1016/j.eururo.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]; 6. Stensland KD, Morgan TM, Moinzadeh A, Lee CT, Briganti A, Catto JWF, et al. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur Urol. 2020; 77:663-6. [DOI] [PMC free article] [PubMed]
- 7.Wallis CJD, Novara G, Marandino L, Bex A, Kamat AM, Karnes RJ, et al. Risks from Deferring Treatment for Genitourinary Cancers: A Collaborative Review to Aid Triage and Management During the COVID-19 Pandemic. Eur Urol. 2020:S0302–S2838. doi: 10.1016/j.eururo.2020.04.063. 30331-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; 7. Wallis CJD, Novara G, Marandino L, Bex A, Kamat AM, Karnes RJ, et al. Risks from Deferring Treatment for Genitourinary Cancers: A Collaborative Review to Aid Triage and Management During the COVID-19 Pandemic. Eur Urol. 2020: S0302-2838;30331-6. [DOI] [PMC free article] [PubMed]
- 8.AUA Inside Tract Podcast - Episode 98. Voices of Urology: Lessons from the Front Lines of COVID-19American Urological Association. [No Authors] [Internet] Available at. < https://www.auanet.org/podcast/voices-of-urology-lessons-from-the-front-lines-of-covid-19. [Google Scholar]; 8. [No Authors]. AUA Inside Tract Podcast - Episode 98. Voices of Urology: Lessons from the Front Lines of COVID-19American Urological Association. [Internet]. Available at. <https://www.auanet.org/podcast/voices-of-urology-lessons-from-the-front-lines-of-covid-19
- 9.Khusid JA, Sullivan JF, Esdaille AR, Khargi R, Shields JM, SUNY Downstate Health Sciences University Urology Team Role of the Urologist During a Pandemic: Early Experience in Practicing on the Front Lines in Brooklyn, New York. Eur Urol. 2020:S0302–S2838. doi: 10.1016/j.eururo.2020.04.024. 30256-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; 9. Khusid JA, Sullivan JF, Esdaille AR, Khargi R, Shields JM; SUNY Downstate Health Sciences University Urology Team. Role of the Urologist During a Pandemic: Early Experience in Practicing on the Front Lines in Brooklyn, New York. Eur Urol. 2020: S0302-2838;30256-6. [DOI] [PMC free article] [PubMed]
- 10.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]; 10. Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020; 323:1574-81. [DOI] [PMC free article] [PubMed]
- 11.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]; 11. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21:335-7. [DOI] [PMC free article] [PubMed]
- 12.Marks P. Coronavirus (COVID-19) Update: Blood Donations. FDA Statement. [Internet] Available at. < https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-blood-donations>. [Google Scholar]; 12. Marks P. Coronavirus (COVID-19) Update: Blood Donations. FDA Statement. [Internet]. Available at. <https://www.fda.gov/news-events/press-announcements/coronavirus-covid-19-update-blood-donations>
- 13.Zhang J, Wu S, Xu L. Asymptomatic carriers of COVID-19 as a concern for disease prevention and control: more testing, more follow-up. Biosci Trends. 2020 doi: 10.5582/bst.2020.03069. Epub ahead of print. [DOI] [PubMed] [Google Scholar]; 13. Zhang J, Wu S, Xu L. Asymptomatic carriers of COVID-19 as a concern for disease prevention and control: more testing, more follow-up. Biosci Trends. 2020. Epub ahead of print. [DOI] [PubMed]
- 14.Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. Version 2. EClinicalMedicine. 2020;21:100331–100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]; 14. Lei S, Jiang F, Su W, Chen C, Chen J, Mei W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. Version 2. EClinicalMedicine. 2020; 21:100331. [DOI] [PMC free article] [PubMed]
- 15.COVID-19: Considerations for Optimum Surgeon Protection Before, During, and After Operation. American College of Surgeons; 2020. [Accessed April 1, 2020]. [No Authors] [Internet] Available at. < https://www.facs.org/covid-19/clinical-guidance/surgeon-protection>. [Google Scholar]; 15. [No Authors]. COVID-19: Considerations for Optimum Surgeon Protection Before, During, and After Operation. American College of Surgeons 2020. [Internet]. Available at. <https://www.facs.org/covid-19/clinical-guidance/surgeon-protection>. Accessed April 1, 2020.
- 16.Procedures, Bedside Procedures. BMH Brigham Health Women's Hospital; [Accessed May 28, 2020]. [No Authors] [Internet] Available at. < https://covidprotocols.org/protocols/procedures/>. [Google Scholar]; 16. [No Authors]. Procedures, Bedside Procedures. BMH Brigham Health Women's Hospital. [Internet]. Available at. <https://covidprotocols.org/protocols/procedures/>. Accessed May 28, 2020.
- 17.Wu ZS, Zhang ZQ, Wu S. Focus on the Crosstalk Between COVID-19 and Urogenital Systems. J Urol. 2020;204:7–8. doi: 10.1097/JU.0000000000001068. [DOI] [PMC free article] [PubMed] [Google Scholar]; 17. Wu ZS, Zhang ZQ, Wu S. Focus on the Crosstalk Between COVID-19 and Urogenital Systems. J Urol. 2020;204:7-8. [DOI] [PMC free article] [PubMed]
- 18.Novara G, Giannarini G, De Nunzio C, Porpiglia F, Ficarra V. Risk of SARS-CoV-2 Diffusion when Performing Minimally Invasive Surgery During the COVID-19 Pandemic. Eur Urol. 2020:S0302–S2838. doi: 10.1016/j.eururo.2020.04.015. 30247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]; 18. Novara G, Giannarini G, De Nunzio C, Porpiglia F, Ficarra V. Risk of SARS-CoV-2 Diffusion when Performing Minimally Invasive Surgery During the COVID-19 Pandemic. Eur Urol. 2020: S0302-2838;30247-5. [DOI] [PMC free article] [PubMed]
- 19.Nassar AH, Zern NK, McIntyre LK, Lynge D, Smith CA, Petersen RP, et al. Emergency Restructuring of a General Surgery Residency Program During the Coronavirus Disease 2019 Pandemic: The University of Washington Experience. JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.1219. Epub ahead of print. [DOI] [PubMed] [Google Scholar]; 19. Nassar AH, Zern NK, McIntyre LK, Lynge D, Smith CA, Petersen RP, et al. Emergency Restructuring of a General Surgery Residency Program During the Coronavirus Disease 2019 Pandemic: The University of Washington Experience. JAMA Surg. 2020. Epub ahead of print. [DOI] [PubMed]
- 20.Outpatient and Ambulatory Care Settings Responding to Community Transmission of COVID-19 in the United States. HHSgov TRACIE. [Updated May 26, 2020];Healthcare emergency preparedness information gateway. [No Authors] [Internet] Available at. < https://asprtracie.hhs.gov/technical-resources/resource/8487/outpatient-and-ambulatory-care-settings-responding-to-community-transmission-of-covid-19-in%20-los%20Estados%20Unidos>. [Google Scholar]; 20. [No Authors]. Outpatient and Ambulatory Care Settings Responding to Community Transmission of COVID-19 in the United States. HHSgov TRACIE. Healthcare emergency preparedness information gateway. Updated May 26, 2020. [Internet]. Available at. <https://asprtracie.hhs.gov/technical-resources/resource/8487/outpatient-and-ambulatory-care-settings-responding-to-community-transmission-of-covid-19-in%20-los%20Estados%20Unidos>.
- 21.Medicare Telemedicine health care provider fact sheet. [Accessed Mar 17, 2020];Centers for Medicare & Medicaid Services. [No Authors] [Internet] available at. < https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet>. [Google Scholar]; 21. [No Authors]. Medicare Telemedicine health care provider fact sheet. Centers for Medicare & Medicaid Services. [Internet]. available at. <https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet>. Accessed Mar 17, 2020.
- 22.Management of Visitors to Healthcare Facilities in the Context of COVID-19: Non-US Healthcare Settings. CDC; https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html [No Authors] [Internet] Available at. <. >. [Google Scholar]; 22. [No Authors]. Management of Visitors to Healthcare Facilities in the Context of COVID-19: Non-US Healthcare Settings. CDC. [Internet]. Available at. <https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/hcf-visitors.html>.
- 23.Katz EG, Stensland KS, Mandeville JA, MacLachlan LS, Moinzadeh A, Sorcini A, et al. Triaging Office-Based UrologY Procedures During the COVID-19 Pandemic. J Urol. 2020;204:9–10. doi: 10.1097/JU.0000000000001034. [DOI] [PMC free article] [PubMed] [Google Scholar]; 23. Katz EG, Stensland KS, Mandeville JA, MacLachlan LS, Moinzadeh A, Sorcini A, et al. Triaging Office-Based UrologY Procedures During the COVID-19 Pandemic. J Urol. 2020;204:9-10. [DOI] [PMC free article] [PubMed]
- 24.Gettman M, Rhee E, Spitz A. AUA Telemedicine Workgroup. Telemedicine in Urology. American Urological Association; [Internet] Available at. < https://www.auanet.org/guidelines/telemedicine-in-urology>. [Google Scholar]; 24. Gettman M, Rhee E, Spitz A. AUA Telemedicine Workgroup. Telemedicine in Urology. American Urological Association. [Internet]. Available at. <https://www.auanet.org/guidelines/telemedicine-in-urology>.
- 25.U.S. Telehealth Satisfaction Study. J.D.Power. [Internet] [No Authors] Available at. < https://www.jdpower.com/business/healthcare/us-telehealth-satisfaction-study>. [Google Scholar]; 25. [No Authors]. U.S. Telehealth Satisfaction Study. J.D.Power. [Internet]. Available at. <https://www.jdpower.com/business/healthcare/us-telehealth-satisfaction-study>
- 26.Viers BR, Pruthi S, Rivera ME, O'Neil DA, Gardner MR, Jenkins SM, et al. Are Patients Willing to Engage in Telemedicine for Their Care: A Survey of Preuse Perceptions and Acceptance of Remote Video Visits in a Urological Patient Population. Urology. 2015;85:1233–1239. doi: 10.1016/j.urology.2014.12.064. [DOI] [PubMed] [Google Scholar]; 26. Viers BR, Pruthi S, Rivera ME, O'Neil DA, Gardner MR, Jenkins SM, et al. Are Patients Willing to Engage in Telemedicine for Their Care: A Survey of Preuse Perceptions and Acceptance of Remote Video Visits in a Urological Patient Population. Urology. 2015; 85:1233-9. [DOI] [PubMed]
- 27.Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015;68:729–735. doi: 10.1016/j.eururo.2015.04.002. [DOI] [PubMed] [Google Scholar]; 27. Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: a randomized controlled trial. Eur Urol. 2015; 68:729-35. [DOI] [PubMed]
- 28.Rose S. Medical Student Education in the Time of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.5227. Epub ahead of print. [DOI] [PubMed] [Google Scholar]; 28. Rose S. Medical Student Education in the Time of COVID-19. JAMA. 2020. Epub ahead of print. [DOI] [PubMed]
- 29.Newman NA, Lattouf OM. Coalition for medical education-A call to action: A proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID-19. J Card Surg. 2020;35:1174–1175. doi: 10.1111/jocs.14590. [DOI] [PMC free article] [PubMed] [Google Scholar]; 29. Newman NA, Lattouf OM. Coalition for medical education-A call to action: A proposition to adapt clinical medical education to meet the needs of students and other healthcare learners during COVID-19. J Card Surg. 2020;35:1174-5. [DOI] [PMC free article] [PubMed]
- 30.Chick RC, Clifton GT, Peace KM, Propper BW, Hale DF, Alseidi AA, et al. Using Technology to Maintain the Education of Residents During the COVID-19 Pandemic. J Surg Educ. 2020:S1931–S7204. doi: 10.1016/j.jsurg.2020.03.018. 30084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]; 30. 30 Chick RC, Clifton GT, Peace KM, Propper BW, Hale DF, Alseidi AA, et al. Using Technology to Maintain the Education of Residents During the COVID-19 Pandemic. J Surg Educ. 2020: S1931-7204;30084-2. [DOI] [PMC free article] [PubMed]
- 31.Amparore D, Claps F, Cacciamani GE, Esperto F, Fiori C, Liguori G, et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. 2020 doi: 10.23736/S0393-2249.20.03868-0. Epub ahead of print. [DOI] [PubMed] [Google Scholar]; 31. Amparore D, Claps F, Cacciamani GE, Esperto F, Fiori C, Liguori G, et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. 2020. Epub ahead of print. [DOI] [PubMed]
- 32.Pang KH, Carrion DM, Rivas JG, Mantica G, Mattigk A, Pradere B, et al. The Impact of COVID-19 on European Health Care and Urology Trainees. Eur Urol. 2020:S0302–S2838. doi: 10.1016/j.eururo.2020.04.042. 30305-5. [DOI] [PMC free article] [PubMed] [Google Scholar]; 32. Pang KH, Carrion DM, Rivas JG, Mantica G, Mattigk A, Pradere B, et al. The Impact of COVID-19 on European Health Care and Urology Trainees. Eur Urol. 2020: S0302-2838;30305-5. [DOI] [PMC free article] [PubMed]